During various medical commissions and examinations, we take a lot of tests, including blood tests, but to obtain maximum information about a person’s health, a number of other special tests are used. A test that can provide more information is the large platelet count ratio (P-LCR) blood test. It is used to study platelets and their effect on the ability of blood to clot.
Platelet test
Normal indicators
Normal platelet levels are 13-43%; in some cases, this number can be adjusted if autoimmune diseases or chronic diseases occur. The norm differs for people of different age groups and looks like this:
- for adult women and men, the platelet rate is 80-320x109/l;
- newborns and infants have an unstable indicator from 180 to 490 × 109/l;
- in the first year of life, the platelet level in children is 180–400×109/l;
- from 1 to 6 years the norm is 160–390 × 109/l;
- from 7 to 12 years the norm is 16–380 × 109/l;
- in adolescence, the norm is 160–360 × 109/l and gradually approaches the adult level.
If there are differences from the above norms, additional diagnostics are necessary, as this indicates pathological processes in the patient’s body
It is very important to note that different laboratories use different chemical reagents and equipment, so it is likely that the results of the same patient may differ in different laboratories. That is why, next to a person’s current indicators, acceptable normal limits are indicated.
Reasons for the decline
The causes of low platelets may be hidden in chronic kidney disease, malaria and leukemia. Platelets in the blood decrease due to heavy metal poisoning, as well as after chemotherapy procedures. The reasons for decreased indicators may also be hidden in preeclampsia in pregnant women, cardiac surgery, side effects of drug therapy, alcohol abuse, and lack of vitamin B12 and folic acid.
In medicine, a decrease in platelets below normal is called thrombocytopenia. A doctor can make this diagnosis if the platelet count has decreased by more than three times. Like an elevated platelet count, thrombocytopenia has several characteristic signs:
- the presence of blood in urine and feces without urogenital infections that could provoke them;
- pinpoint rash on the skin;
- difficulty stopping bleeding from the nose, gums and bleeding during menstruation in women.
The causes of thrombocytopenia must be eliminated immediately, since even the smallest cut can provoke enormous blood loss and exhaustion of the body, as a result of which the patient dies.
Large platelet ratio value
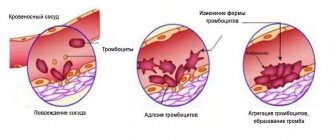
Platelets are a necessary component of human blood, and they perform an important function: they prevent excessive blood loss due to possible damage to the vessel. The coefficient of large platelets has the ability to increase, and this factor can be influenced by certain reasons, which we will consider in this article.
Platelets are cells or platelets of colorless texture that are responsible for the ability of blood to clot. By implementing the so-called grouping, as a result of which a barrier is formed, they help stop bleeding. The optimal platelet level depends on the age category. So, for example, in an adult the quantitative indicator can vary between 200-400 g/l, and in childhood the limits narrow significantly - 150-180. Platelets in the blood can also change their numbers depending on the season of the year or time of day.
The platelet count is determined by taking a general blood test. Often the patient is diagnosed with thrombocytosis, which means the platelet level is elevated. Deviations of this kind require constant monitoring and immediate treatment. Plt analysis - what does it mean? This is a test to detect blood platelets.
Currently, there are several types of thrombocytosis:
- Primary. It occurs as a result of a negative change in the functionality of bone marrow cells. As a rule, it does not manifest itself in any way; only in rare cases does it cause pain in the head and general malaise. The danger in this case is that such deviations can provoke the appearance of malignant neoplasms.
- Secondary. It is a symptomatic sign of certain diseases, as well as the result of surgical treatment or a side effect as a result of taking certain medications.
Regardless of the species, it is necessary to clarify the reason why the platelet count is increased and their further normalization through various therapeutic methods.
As mentioned earlier, the optimal quantitative level of P LCR is 13-43%, and it does not matter which category the patient belongs to. If a patient is diagnosed with a chronic disease or a congenital form of the disease, then in this situation his condition is taken into account. It is possible that an individual treatment will be formed that is fundamentally different from others.
As for the generally accepted meaning, it may change at the age category level.
The table shows the optimal indicators of the total platelet count depending on age and gender:
The large deviations identified indicate that the number of large blood cells increases significantly. Studying the results obtained implies not only counting the total number of platelets and their compliance with normal values, but also the presence of chronic diseases in the patient (it does not matter in what quantity).
It should be noted that elevated platelet counts may be influenced by the equipment used to test the material and reagents. In this case, the norm that can be accepted is written on the result form next to the indicators related to the patient.
What does platelet distribution index mean?
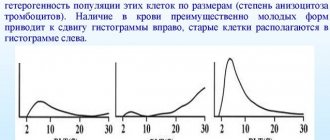
The platelet distribution index (PDW index) is deciphered as the width of the distribution of PLT by volume (the designation PDW index is indicated on the medical form). This indicator reflects the variety and change in size of substances (in %), that is, the PDW index can determine the ratio of microplatelet and macroplatelet in the blood.
In a healthy patient (over 18 years old), the index rate is 15-17%. For minor patients, the optimal level is 10-16%. In this case, a slight deviation of 2-3% is allowed.
A study of the PDW index should be carried out in the following cases:
- Hospitalization.
- Standard medical examination.
- Diagnosis of inflammation or pathologies of the circulatory system.
The PDW index is studied together with MPV and PCT (proportion of blood volume occupied by platelets).
Important! It is worth highlighting such a designation as the calculation of the SD index on PDW, in which PDW-SD means an indicator characterizing the heterogeneity of PLT.
Increase in PDW index
An increase in the PDW index indicates strong volumetric heterogeneity of the PLT. If this index increases by more than 20%, appropriate treatment is required. In this case, the patient may experience weakness, malaise, and decreased performance.
Thus, a significant increase in the platelet index should be observed in the following cases:
- Physical overexertion.
- Anemia, including among pregnant women.
- Oncology.
- Surgery (for example, removal of the spleen), as well as the postoperative period.
- Heavy menstruation.
- Inflammatory process.
- Incorrect blood draw.
- Treatment with corticosteroids.
Lowering the PDW index
When the PDW index decreases, the laboratory technician, when testing the blood, notes a low content of flat blood cells. Moreover, such a deviation is not always associated with the development of pathologies (menstruation, stress, poor diet, bad habits, taking medications).
With a significant decrease in the index, diseases such as: liver cirrhosis may develop; cancer; leukemia; anemia; hepatitis.
Reasons for the increase
If the test determines that platelet levels are elevated, the doctor may diagnose thrombocytosis, which causes problems with blood flow and makes it difficult for cells to move through the veins and arteries. It is known that with the slightest mechanical damage, regardless of the cause, platelets stick together and form a kind of plug, which clogs the damaged area and prevents bleeding.
If the patient’s tests show an increased level of platelets, then there is a risk of a blood clot forming inside the vessels, which can block the access of oxygen to certain organs and provoke their death. If this happens in the pulmonary artery, then access to the heart is blocked and the person may die from a heart attack; if a blood clot forms in the vessels of the brain, then the patient will have a stroke. There are additional reasons that provoke the formation of a blood clot - these are atherosclerosis and varicose veins, which lead to a narrowing of the lumen in the vessels, and the slightest blockage can be fatal for a person.
Most patients suffer from thrombocytosis due to reasons such as a malfunction of the bone marrow, where the process of normal hematopoiesis is disrupted. Diseases such as leukemia, leukemia, as well as metastases that have penetrated into the bone marrow from other organs are a clear provocateur of the fact that there is an increased level of platelets in the body. A high level of these blood cells can also provoke poisoning with poisons and chemicals; in rare cases, high levels of platelets cause the consequences of viral diseases in children.
If we analyze the patient’s condition, then in addition to the cause of the disease, we can identify characteristic symptoms that accompany a violation of platelet levels:
- increased sensitivity of the fingertips on the hands, with a light touch the patient feels pain;
- vegetative-vascular dystonia;
- tachycardia;
- frequent shortness of breath, sometimes even in a calm state;
- formation of subcutaneous hematomas and bruises;
- itching and bluish discoloration of the skin;
- constant lethargy, decreased performance and weakness in the limbs;
- blurred vision;
- regular nosebleeds; female patients may experience heavy menstruation.
As a rule, only two or three symptoms appear at the same time; the appearance of all the listed signs is unlikely.
Large platelet coefficient p lcr
Information about various diseases can be accurately determined by an HGB blood test, the interpretation of which will fully assess the patient’s condition and track the dynamics of recovery.
This is the most common type of clinical examination. Any disease will definitely affect the state of the blood.
Passing through the entire body, its systems and organs, blood will provide detailed information about human health. Basic blood parameters can be determined using modern diagnostic equipment.
Decoding is done using abbreviations in English, which are placed on a special form.
As soon as a patient enters a medical institution, the first thing the doctor prescribes is a blood test.
The fact of the presence of various diseases and their prevention at an early stage depends on timely access to the clinic.
Dizziness, fever, vomiting, upset stomach, various pathologies that are symptoms of many diseases can be determined by doing a blood test and determining whether each indicator is elevated or decreased. The study consists of quantitative determination of blood composition and its deviation from the norm. The studied parameters include:
- RBC count;
- hemoglobin level HGB;
- total white blood cell count WBC;
- platelet count PLT;
- hematocrit HCT;
- erythrocyte sedimentation rate ESR.
Abbreviations in the analysis printout
This test shows the number of platelets, their maturity and size.
The index is called the large platelet ratio. The study indicates changes in particle number and associated pathology. Blood is drawn in the laboratory. For testing, blood can be taken from a finger or from a vein in the case of an advanced analysis. Blood sampling is almost painless and rarely causes discomfort. When taking blood from a vein, the arm is tied with a flagellum, the skin is treated with a disinfectant solution and pricked with a sterile needle. When taking blood from a finger, it is disinfected with an antiseptic and pierced with a medical blade.
https://www.youtube.com/watch?v=o94ikVJc6L0
The material is collected in a test tube and transferred for research, which must be carried out immediately in the first hours, because then a precipitate may form and it will be difficult to determine many indices.
Very often, a printout of the results of a clinical blood test is presented in the form of abbreviations in English. Decoding abbreviations for a general blood test from English into Russian will help the average user navigate the indicators and adequately evaluate the result of a laboratory analysis.
Here is what is included in a clinical blood test (abbreviated in English):
- WBC
- R.B.C.
- HGB
- HCT
- PLT
- MCV (HCT/RBC)
- MCH (HGB/RBC)
- MCHC (HGB/HCT)
- MPV
- PDW
- PCT
- LYM/Lymph (%, #)
- MXD (%, #)
- NEUT (NEU - %, #)
- MON (%, #)
- EO (%, #)
- BA (%, #)
- IMM (%, #)
- ATL (%, #)
- GR (%, #)
- RDW (SD, CV)
- P-LCR
- ESR
Printout of clinical blood test
The use of such abbreviations in the OAC is convenient and practical: it does not take up much space in the analysis printout and complies with international standards for the designation of blood parameters. Hematologists and therapists can decipher them without much difficulty, and for highly specialized doctors and patients, a reminder of the designations of each indicator will be useful.
Causes of elevated platelet count
When an increased level of platelets in the blood is detected, specialists are faced with one of the main tasks: to identify the cause of such deviations. All possible causes of this kind of changes are divided into pathological and physiological. In this case, these include:
- injuries and possible surgical interventions - the body produces a large number of red blood cells, thereby replenishing the lost amount of blood;
- critical days for representatives of the weaker half of humanity - in most cases, such physiological characteristics contribute to the formation of anemia, which in turn provokes the body to actively recover by increasing the number of red blood cells;
- diagnosing atherosclerosis in a patient;
- elevated blood sugar levels (diabetes mellitus).
Another important reason for an increase in platelet levels is the excessive amount of alcohol consumed, since ethyl alcohol can adversely affect the composition of the blood, namely the elimination of platelets
Manifestation of symptoms
If you listen to the so-called “signals” of your body, you can detect the following changes:
- increased sensitivity of the fingertips, which can gradually turn into pain;
- the occurrence of bruises or hemorrhages in the subcutaneous area;
- change in the appearance of the skin (mainly a bluish tint) or a feeling of itching;
- weakness of the whole body, which entails a decrease in overall performance;
- impairment of visual functionality;
- bleeding may be frequent (nasal, intestinal), and women may have heavy periods.
Basically, the above symptoms can appear individually or in pairs, however, individual dysfunctions of the body mean that the patient needs to go to a medical institution to undergo a certain number of relevant tests, identify the cause of platelet level deviations and formulate subsequent therapy.
With elevated P-LCR values, a person physically feels a number of changes in his condition, which are not always clearly manifested against the background of the current illness, but when paying closer attention to his feelings, they can be recorded. In a hospital setting, with regular blood sampling, the attending physician can promptly see a trend toward an increase in the number of large platelets in the blood and take the necessary measures. But the patient should independently monitor the symptoms that may appear with elevated platelet values in the blood:
- excessive sensitivity of the fingertips is possible, such a sensation can even cause pain;
- bruises or bruises may suddenly appear on the body without any reason for their occurrence;
- itching may occur and acquire a bluish tint;
- with a general weakening of the body, lethargy may occur and performance decreases;
- You may experience nosebleeds and periods with heavier bleeding.
Important! All together, the above symptoms do not appear, but if you find at least two or three of them, you should immediately consult a doctor and undergo the necessary tests. Early detection of the problem will allow you to quickly and effectively cope with the disease
Early detection of the problem will allow you to quickly and effectively cope with the disease.
Carrying out treatment
Expert opinion
Cardiologist Grigory Viktorovich
To normalize the platelet values in the blood and bring the number of large platelets to a normal balance, the issue of treating the underlying disease should be addressed. If the treatment issue can be quickly resolved, the P-LCR indicator will drop to the required values on its own. If the norm is seriously exceeded, the doctor can begin treating thrombocytosis directly, in parallel with the treatment of the underlying disease. During treatment, tests must be used to monitor the effect of medications. The most commonly used medications are Interferon and Anagrelide. Small deviations from the norm cannot cause any particular harm to the patient’s health and are treated with special diets. It is necessary to fill the menu with products that stimulate blood thinning, such as fresh onions or fresh garlic. Tomatoes and tomato juice are excellent in reducing platelet levels; it is recommended to season vegetable salads with olive oil. You can take fish oil separately. For any diet, it will be useful to consume about two liters of regular water per day, and add foods high in magnesium.
P-LCR reduced
The P-LCR test result should indicate at least 30 percent large or giant platelets. However, as with any survey, some fluctuations are possible. Here they range from 13 to 43 percent. This test is usually ordered when a doctor needs a detailed image analysis of platelets in the blood. It is very common for normal morphology to indicate an incorrect number. P-LCR should always be done on an empty stomach. Only then is a real assessment of the patient’s condition possible. Just because the P-LCR is low doesn't mean we have cause for concern. This result should always be assessed in conjunction with other parameters. The physician must consider the number of plates as well as the average volume. If the other indicators are normal and only the P-LCR is out of bounds, there is no cause for concern. Sometimes this is a natural feature. Some people, for example, have an elevated platelet count throughout their lives, while others have a very low platelet count but all other parameters are within normal limits. Contrary to appearances, this situation is quite common and does not require detailed diagnosis.
Research parameters
After a general blood test and the presence of certain complaints indicated by the patient when communicating with the doctor, an extended blood test is prescribed. Laboratory specialists can not only count the number of platelet cells, but also significantly expand the information by assessing cell size, quality, maturity and activity. An excess of large platelets may indicate disruptions in the functioning of the body and the presence of diseases.
To obtain information about the number of large platelets in the blood, in comparison with normal-sized platelets, laboratory tests are performed that study the P-LCR value. This indicator is expressed as a percentage.
The large platelet count, or P-LCR, can indicate certain problems in the body if its values are abnormal.
Attention! Only a specialist with experience in conducting this type of research can accurately determine the test results and make the correct diagnosis.
What are platelets
P-LCR increased
It is also possible to obtain a larger P-LCR result. Sometimes this is a natural characteristic of a particular person. Then usually a large average platelet volume appears in the blood test, as well as a large variance. Sometimes an elevated P-LCR can also indicate a disease. The most common is autoimmune purpura. Otherwise it is called immune thrombocytopenia. The result of this disease is the destruction of platelets by the body. As a result, many large and huge platelets are formed. Their functionality can be impaired and very often leads to many unwanted effects. If the interpretation of the results indicates an abnormality, the reason for this will need to be found. It may turn out that this is caused by illness. Never ignore abnormalities found during laboratory tests because they very often report diseases that have not yet developed. Therefore there is a much better chance of curing them. Test results should always be interpreted by a specialist who will also be familiar with the patient's overall clinical picture. An accurate medical history is also important. He will provide your doctor with specific information and help you with ideas. Sometimes abnormalities in the results occur, for example, with systemic diseases. Any disturbance in the production and functioning of platelets can be caused by anemia, inflammation, infection, or alcoholism. Very often, their abnormal amount appears in cancer. It is our blood that can be the first to tell us about the state of our body.
General blood test norms for children under 1 year of age
| Index | Age | |||
| newborn | 7-30 days | 1 – 6 months | 6 -12 months | |
| Hemoglobin | 180-240 | 107 — 171 | 103-141 | 113-140 |
| Red blood cells | 3,9-5,5 | 3,6-6,2 | 2,7-4,5 | 3,7-5,3 |
| Color index | 0,85-1,15 | 0,85-1,15 | 0,85-1,15 | 0,85-1,15 |
| Reticulocytes | 3-15 | 3-15 | 3-12 | 3-12 |
| Leukocytes | 8,5-24,5 | 6,5 -13,8 | 5,5 – 12,5 | 6-12 |
| Rod | 1-17 | 0,5- 4 | 0,5- 5 | 0,5- 5 |
| Segmented | 45-80 | 16-45 | 16-45 | 16-45 |
| Eosinophils | 1 — 6 | 1 — 5 | 1 — 5 | 1 — 5 |
| Basophils | 0 — 1 | 0 — 1 | 0 — 1 | 0 — 1 |
| Lymphocytes | 15 — 35 | 45 — 70 | 45 — 70 | 45 — 70 |
| Platelets | 180-490 | 180-400 | 180-400 | 160-390 |
| ESR | 2-4 | 4-10 | 4-10 | 4-12 |
| Index | Age | ||||
| 1-2 years | 2-3 years | 3-6 years | 6-9 years | 9 -12 years | |
| Hemoglobin | 100 — 140 | 100 — 140 | 100 — 140 | 120 — 150 | 120 — 150 |
| Red blood cells | 3,7-5,3 | 3,9-5,3 | 3,9-5,3 | 4,0-5,2 | 4,0-5,2 |
| Color index | 0,75-0,96 | 0,8-1,0 | 0,8-1,0 | 0,8-1,0 | 0,8-1,0 |
| Reticulocytes | 0,3-1,2 | 0,3-1,2 | 0,3-1,2 | 0,3-1,2 | 0,3-1,2 |
| Leukocytes | 6,0 — 17,0 | 4,9-12,3 | 4,9-12,3 | 4,9-12,2 | 4,5-10 |
| Rod | 1 — 5 | 1 — 5 | 1 — 5 | 1 — 5 | 1 — 5 |
| Segmented | 28 — 48 | 32 — 55 | 32 — 55 | 38 — 58 | 43 — 60 |
| Eosinophils | 1 — 7 | 1 — 6 | 1 — 6 | 1 — 5 | 1 — 5 |
| Basophils | 0 — 1 | 0 — 1 | 0 — 1 | 0 — 1 | 0 — 1 |
| Lymphocytes | 37 — 60 | 33 — 55 | 33 — 55 | 30 — 50 | 30 — 46 |
| Platelets | 160-390 | 160-390 | 160-390 | 160-390 | 160-390 |
| ESR | 4-12 | 4-12 | 4-12 | 4-12 | 4-12 |
Decoding
The meaning of WBC in a general blood test is white blood cells, which translated from English means white blood cells. This is how a blood test identifies leukocytes, which under a microscope look like white cells. The unit of measurement is 109/l.
The meaning of RBC in a blood test is red blood cells. In laboratory analysis, red blood cells are designated as such. Unit of measurement - 1012/l
HGB is a shortened version of the English word Hemoglobin. This is how hemoglobin is indicated on the blood test printout. Unit of measurement - g/l (g/l), g/dl (g/dl).
HCT stands for Hematocrit.
PLT stands for Platelets. This is how platelets are encrypted in the printout of a clinical blood test.
MCV is short for Mean Corpuscular Volume, which means the average volume of a red blood cell. It is measured in µm3 or femtoliters (fl).
| Age | MCV rate (fl) |
| Women | Men |
| Newborn babies | 140 |
| Children from 1 to 12 months | 71-84 |
| 1-5 years | 73-86 |
| 5-10 years | 75-88 |
| 10-18 years | 78-90 |
| Adults 18 and older | 80-100 |
As can be seen from the table, the MCV norm in a general blood test is not very different for adults and all ages of children, with the exception of newborns. Their red blood cell volume is significantly larger, which is associated with a higher content of fetal hemoglobin (HbF) in their structure.
Name of red blood cells depending on size:
- Normal - normocyte
- More than normal - macrocyte
- Less than normal - microcyte
The abbreviation MCH means mean corpuscular hemoglobin. Translated as the average amount of hemoglobin in a red blood cell. Measured in picograms (pg).
| Age | MCH rate (pg) |
| Women | Men |
| Newborn babies | 29-37 |
| 1-2 months | 27-34 |
| 3-6 months | 25-32 |
| 1-3 years | 22-30 |
| 3-18 years | 25-32 |
| Adults 18 and older | 27-35 |
MCH is an analogue of the color indicator, only not in relative numbers, but in picograms.
MCHC — mean corpuscular hemoglobin concentration. This is the average concentration of hemoglobin in red blood cells. The difference between this indicator and total hemoglobin in a blood test is that MCHC takes into account the volume of red blood cells only, and the total hemoglobin level is determined based on the volume of all blood (plasma cells).
| Age | MCHC rate (g/l, g/l) |
| Newborn babies | 280-360 |
| 1-2 months | 280-350 |
| 3-12 months | 300-360 |
| 1-3 years | 320-380 |
| 4-18 years | 320-370 |
| Adults 18 and older | 320-360 |
As can be seen from the table, the MCHC norm in the analysis does not change much with age.
MPV is short for mean platelet volume. Stands for average platelet volume. Platelets stay in the bloodstream for a short time and as they “mature” they decrease in size, so determining their volume (MPV) helps determine the degree of platelet maturity in the blood. The unit of MPV is femtoliter (fl), which is equal to µm2.
| Age | Average platelet volume |
| Women | Men |
| Newborn babies | 7,0-8,0 |
| Children under 1 year | 7,2-8,2 |
| 1-18 years | 7,4-9,0 |
| Adults 18 and older | 7,4-10,0 |
The MPV norm is when the volume of 83-90% of platelets corresponds to the age norm indicated in the table and only 10-17% of large and small (immature and old).
Decoding PDW in a blood test - platelet distribution width. The abbreviation refers to the relative width of the platelet distribution across the volume.
The PDW norm is 10-17%. This figure indicates what percentage of the total platelet count differs in volume from the mean value (MPV).
PCT is the full name in English platelet crit. Translated as thrombocrit. The indicator means how much volume platelets occupy in relation to the volume of whole blood.
The PCT norm in tests for children and adults is 0.15-0.4%.
LYM or Lymph in KLA stands for lymphocyte. This is the abbreviated name for lymphocytes in a blood test. The printout may contain 2 indicators:
- LYM% (LY%) - relative content of lymphocytes
- LYM# (LY#) - absolute lymphocyte content
MXD (MID)
The abbreviation MXD means mixed. An indicator of a mixture of types of leukocytes: monocytes, basophils and eosinophils. The results of the general analysis can be in 2 options:
- MXD% (MID%)—relative cell content
- MXD# (MID#)—absolute cell content
MXD norm: relative to all leukocytes - 5-10%, in absolute numbers - 0.25-0.9*109/l.
NEUT is short for neutrophils. This indicator in the general analysis means blood neutrophils. Determined in the analysis in 2 options:
- NEUT% (NEU%) - relative content of neutrophils
- NEUT# (NEU#) — absolute content of neutrophils
MON is short for Monocyte. This is how the UAC denotes monocytes, the indicator of which in the analysis printout can be of 2 types:
- MON% (MO%) - relative number of monocytes
- MON# (MO#) - absolute number of monocytes
EO can be deciphered from a general blood test as Eosinophils, which means eosinophils in English. The results of a clinical analysis may contain 2 indicators:
- EO% - relative content of eosinophils
- EO# - absolute eosinophil content
BA - Basophils (basophils)
- BA% - relative basophil content
- BA#—absolute basophil content
The abbreviation IMM stands for immature granulocytes.
- IMM% - relative content of immature granulocytes
- IMM# - absolute content of immature granulocytes
ATL is the designation for atypical lymphocytes.
- ATL% - relative content of atypical lymphocytes
- ATL# - absolute content of atypical lymphocytes
GR is the number of granulocytes in the blood. Granulocytes include: basophils, eosinophils and neutrophils.
- GR% is the relative content of granulocytes. The norm in adults is 50-80%
- GR# is the absolute content of granulocytes. The norm for adults is 2.2-8.8*109/l
HCT/RBC
The HCT/RBC ratio refers to the average red blood cell volume. Same as MCV (see above)
HGB/RBC
HGB/RBC - this indicator determines the average hemoglobin content in a red blood cell. Same as MCH (see above).
HGB/HCT
HGB/HCT is the average hemoglobin concentration in red blood cells. Same as MCHC (see above)
RDW is the erythrocyte distribution width in %. Shows what percentage of red blood cells have sizes different from the norm (7-8 microns). The more microcytes (size {amp}lt;7 microns) and macrocytes (size {amp}gt;8 microns) in the blood, the higher the RDW.
- The normal RDW in adults is 11.5–14.5%
- The norm for newborns (up to 1 month) is 14.9–18.7%
In children older than 1 month, the RDW norm is practically no different from adults. In newborn children, the rate is much higher, because Fetal hemoglobin is still present in large quantities in their blood, which affects the size of red blood cells.
Exceeding RDW above the specified values is erythrocyte anisocytosis.
RDW-SD
RDW-SD is a measure that indicates the size gap between the smallest microcyte and the largest macrocyte.
RDW-CV
RDW-CV is the percentage distribution of red blood cells by size: % microcytes, % normocytes and % macrocytes.
P-LCR - large platelet ratio
ESR stands for erythrocyte sedimentation rate, which is translated from English as erythrocyte sedimentation rate. The Russian abbreviation for this value is ESR (in old forms it may be designated ROE).
Having a transcript of the general blood test from English transcription into Russian will be useful not only for the patient, but also for doctors of various specialties, because In everyday practice, it is extremely rare to encounter all the variety of possible UAC indicators.
The decoding is carried out by a specialist who takes into account all the factors influencing the change in the number of cells. The test result is given to the patient the day after blood donation.