Useful articles / August 31, 2020
A single test is not enough to diagnose iron deficiency anemia. It is necessary to evaluate a set of indicators: ferritin, transferrin, serum iron, hemoglobin, total iron-binding capacity. Iron deficiency can be latent, but the level of hemoglobin in a general blood test (CBC) is not a cause for concern. However, iron reserves in the body are often depleted by that time (read more about ferritin in the article “Ferritin analysis: why is it needed?”). What does a serum iron test show?
What is iron?
A serum iron test is often called an iron test - they are the same test. However, it should not be confused with ferritin or hemoglobin. Iron is a trace element that is part of hemoglobin and other respiratory pigments, which ensure the transfer and delivery of oxygen to tissues. Iron is responsible for hematopoiesis and redox reactions of the body, is involved in collagen synthesis, the functioning of the immune system, and porphyrin metabolism. Fe deficiency leads to disruption of hemoglobin synthesis and oxygen transport in the body.
A person receives iron through food and is absorbed in the intestines. And this is where the transport protein ferritin, which transports and stores iron, is important.
Ferritin and serum iron are different tests,” explains Lyubava Kazakova, general practitioner at ELISA Medical Center. — The level of iron in the body can change depending on nutrition, and ferritin shows the reserve of this substance. For example, serum iron may be one thing today and another tomorrow. It changes after eating or taking iron supplements. Ferretin cannot be changed so dramatically. Ferritin can also increase during inflammatory processes in the body. Thus, sometimes there is a false impression that the supply of a substance is normal, but in fact this is a mistake. Therefore, when diagnosing iron deficiency anemia, a set of tests is needed.
A serum iron test is necessary to assess the amount of iron in the body at the time of the test. As we have already said, the main source of microelements is food. Heme iron comes from meat and fish, non-heme iron comes from vegetables and fruits. It is important to understand that only 1-5% of iron is absorbed by the body from plant foods. For animal products, this figure reaches 35%. The process of absorption of the substance is “controlled” by the intestines. Excess microelement is stored in the body as a reserve. But the level of ferrum in serum changes throughout the day, and also depends on age and gender.
Iron deficiency anemia in children
Iron deficiency is the most common condition in children due to an unbalanced diet. In addition, rapid growth, low birth weight and excessive consumption of cow's milk are common causes of IDA.
During the first six months of a child's life, iron reserves are sufficient to ensure erythropoiesis (the formation of red blood cells). Babies with low birth weight and/or perinatal blood loss deplete their reserves earlier because they are smaller. Children receive the greatest amount of iron from breast milk in the first month, then the level of iron gradually decreases.
Solid foods, which begin 6 months after birth, should be rich in iron, zinc, calcium, phosphorus, magnesium and vitamin B6. According to the World Health Organization (WHO), 98% of the iron requirements of children aged 6 to 23 months should be met from solid foods.
Normal blood iron levels
Fe levels in the blood of men and women are different. For physiological reasons, the rate will be lower in women (menstrual cycle and pregnancy), and higher in men. The average value for men is 14.3–25.1 µmol/l, for women – 10.7–21.5 µmol/l.
Regardless of gender, the older a person is, the lower his iron level in the body.
What reduces the level of ferrum in the blood?
- Age. The older the person, the lower the serum iron concentration.
- Menstruation and pregnancy.
- Chronic fatigue and stress.
- Sleep deficiency.
- Physical overexertion.
Iron deficiency anemia during pregnancy
Any hemoglobin value below 105 g/L (10.5 g/dL) can be considered true anemia, regardless of gestational age.
During pregnancy, the risk of developing iron deficiency anemia increases as the body's need for iron increases. According to WHO estimates, in developing countries, every second pregnant woman and about 40% of preschool children suffer from anemia.
Severe anemia during pregnancy increases the risk of premature birth, low birth weight, and postpartum depression. Anemia is responsible for about 20% of all deaths among women giving birth.
Anemia. How to increase iron levels in the blood?
Impaired intake, absorption or loss of iron can lead to iron deficiency anemia. Anemia is not an independent diagnosis, more often it is a consequence of chronic diseases: tumor formations, polyps, intestinal diverticulosis, uterine fibroids, endometriosis, gastric ulcers... Before treatment, it is necessary to find out the cause of iron deficiency.
Causes of iron deficiency anemia:
- Nutritional deficiency (elderly people are more susceptible, their diet contains more dairy and plant products than animal products).
- Diseases (stomach ulcer, duodenal ulcer, various polyps, tumors. With oncology, hemoglobin decreases, which is associated with increased destruction of iron in the body).
- Menorrhagia in women (heavy menstruation).
Symptoms:
- General weakness.
- Increased fatigue.
- Hair loss and brittle nails.
- Cardiopalmus.
- Increased irritability, anxiety.
- Light sleep.
- Problems with memory and concentration.
- Dysphagia (difficulty swallowing dry food).
Therapy should have an integrated approach: changing the diet plus taking synthetic forms of iron. For some diseases, for example, resection of the small intestine, changing the diet cannot solve the problem of iron deficiency. Parenteral administration of drugs is necessary.
Prevention of iron deficiency anemia in children
To prevent iron deficiency anemia in infants, you should feed your baby breast milk or iron-fortified formula for the first year. Cow's milk is not recommended for children under one year of age. After 6 months, it is necessary to introduce foods rich (enriched) in iron. It is not recommended to give children over 1 year of age more than 500 ml of cow's milk per day.
Interesting fact about iron deficiency anemia
It is unexpected, but true, that with iron deficiency anemia it is easier for the human body to cope with malaria, tuberculosis and a number of respiratory diseases. It may also improve survival rates in patients with HIV and reduce the risk of developing cancer. The reason is very simple - most pathogenic bacteria, thanks to iron, grow stronger and spread throughout the body (like bacteria, cancer cells also need iron to grow). And in people with iron deficiency, the bacteria are more likely to die before they become a dangerous infection. The human body is unique and when an infection is detected, it slows down the production of iron, thus helping itself to cope with the threat that has arisen.
What increases iron levels in the blood?
- Products containing iron.
- Taking iron supplements.
There is a category of people who do not consume animal products and are confident that hemoglobin can be raised with plant foods high in iron,” says Lyubava Kazakova. — Yes, there is iron in buckwheat, green vegetables, and pomegranates. But on average 1-5% of iron is absorbed from plant foods. This is due to the fact that these products contain iron in trivalent form, and when entering the body it must be converted into divalent form.
There is a lot of controversy about pomegranate juice, which increases hemoglobin. But if you drink 3 glasses of juice a day, it will do more harm than good. Pomegranate juice is highly acidic, which can lead to exacerbation of chronic gastritis and other gastrointestinal problems. However, pomegranate contains large amounts of vitamin C and B, which improve the absorption of the microelement. That is, if you have animal products (meat and offal), green vegetables and pomegranates in your diet, this will improve the absorption of iron. As for meat, you don't need to eat it every day! 1-2 times a week will be enough, and on other days replace it with fish and eggs.
Is it possible to increase the level of a microelement in the blood with hematogen? Hematogen is a food supplement, a bar, which contains black food albumin (powder from the blood of cattle). It is important to understand that this is a supplement, not a medicine. It is impossible to cure anemia and increase the level of iron in the blood with hematogen alone. The bar can be considered as a source of useful microelements and vitamins, but not as an alternative to iron-containing preparations.
Why don't your Fe levels increase if you take iron supplements or eat iron-containing foods? This may be due to the fact that substances enter the body that interfere with the absorption of iron: tea, coffee, calcium supplements.
Anemia during pregnancy, tests to detect anemia, high iron levels - read the continuation of the article
Most common clinical manifestations
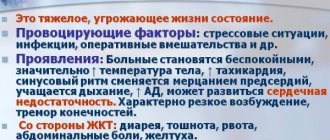
The severity of symptoms in chronic anemia can vary and depends on the rate of blood loss, age and gender of the patient. The severity of the condition is due to tissue iron deficiency. The appearance of anemic syndrome is caused by tissue hypoxia; its manifestation is universal for all types of anemia:
- The occurrence of weakness and fatigue.
- The appearance of pallor of the skin and mucous membranes.
- The occurrence of headache and pulsation in the temples.
- The presence of dizziness and fainting.
- The appearance of shortness of breath and palpitations during habitual physical activity.
- Increased anginal pain due to heart problems.
- Decreased general tolerance to physical activity.
- The emergence of resistance to treatment with vasodilators.
Sideropenic syndrome can be caused by tissue iron deficiency; its main manifestations are the following symptoms:
- The presence of dry skin, cracks on the surface of the arms, and also on the legs and in the corners of the mouth, when the patient is diagnosed with so-called angular stomatitis.
- The presence of glossitis, accompanied by atrophy of the papillae, pain and redness of the tongue.
- The occurrence of brittleness, thinning and splitting of nails.
- The presence of hair loss in combination with early graying.
- The presence of taste perversion when patients eat chalk, clay, minced meat, sand, and the like.
- Presence of addiction to unusual odors, for example, to kerosene, fuel oil, gasoline, acetone, mothballs, car exhaust fumes, which completely disappears after taking iron supplements.
- The presence of dysphagia, that is, difficulty swallowing solid food.
The presence of secondary immunodeficiency syndrome is characterized by a tendency to frequent relapses of infectious and inflammatory diseases. This syndrome includes:
- The presence of damage to the digestive system in the form of glossitis, dysphagia, decreased acid-forming functions of the stomach, atrophic gastritis, bloating, constipation and diarrhea.
- Presence of damage to the hepatobiliary system.
- The presence of pathological changes in the cardiac system, which is manifested by the occurrence of shortness of breath, tachycardia, cardialgia, swelling in the legs, anginal pain, hypotension, expansion of the boundaries of the heart, and so on.
- The presence of damage to the nervous system, which is manifested by a decrease in memory and ability to concentrate.
- The presence of damage to the muscular frame, which is manifested by muscle weakness under normal loads, and in addition, mixed urinary incontinence and the like.
The skin of patients suffering from chronic anemia is usually pale, but not icteric. As for the liver, spleen and peripheral lymph nodes, they are not enlarged. Sometimes the skin may even acquire a bluish tint. Such patients tan very poorly in the sun, and girls, as a rule, are infantile and often have menstrual cycle disorders, ranging from amenorrhea to the presence of heavy menstruation.
Survey
Anemia can develop against the background of chronic inflammation in the body, with diseases such as pneumonia and more. Therefore, when signs of anemia appear, the patient first undergoes a comprehensive examination.
Modern diagnostics make it possible to accurately determine the diagnosis in a short time, identify the causes of anemia of chronic diseases and prescribe optimal treatment.
Diagnosing ACD is not so easy. An integrated approach is required, which includes a whole list of activities and examinations. Let's highlight the most important ones:
- First, the doctor is required to conduct a full interview to draw up an anamnesis. Here it is important to be frank and honest with a specialist, since by hiding some pathologies, disorders or not talking about previous operations, you risk getting the wrong conclusion. Any information about current diseases and diseases that existed several years ago plays a role in data collection.
- Next comes the diagnosis itself. The first test will be a routine general blood test. It is needed to determine the quantitative and qualitative composition of components in the blood.
- Biochemical analysis is often performed. This is a more complex laboratory study of samples that answers a number of important questions.
- Based on chronic pathologies and diseases that provoked ACD, the patient is referred for additional examinations. Usually this is ultrasound, cardiogram, MRI and other diagnostic methods.
Having received all the results, the doctor makes a conclusion, makes an accurate diagnosis and determines the characteristics of the ongoing anemia. Only on the basis of a wide range of information is it possible to select the correct and adequate treatment. Having understood what inflammatory processes or pathologies a person has encountered, one can make a prediction regarding the further development of anemia and its elimination.
Conducting laboratory diagnostics
The main criteria for determining chronic iron deficiency anemia in a patient are:
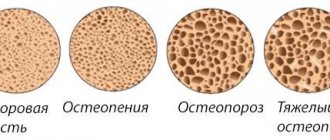
- The presence of a low color index.
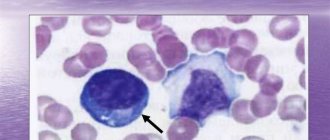
- Presence of erythrocyte hypochromia and microcytosis.
- Decreased serum iron levels.
- Increased serum iron-binding function and decreased ferritin levels.
After determining whether the patient has anemia and the level of its severity, it is necessary to find out the causes and source of bleeding. To do this, a whole series of various studies should be carried out. The main diagnostic methods include:
- Conducting an endoscopic examination of the digestive system. As a rule, as part of such a diagnosis, a colonoscopy is performed, possibly with a biopsy.
- Testing feces for occult blood.
- Conducting gynecological manual and ultrasound examinations in women.
- Carrying out a study of the urinary system. In this case, patients undergo a urine test, ultrasound examination of the kidneys, and in addition, cystoscopy.
- Conducting an X-ray examination of the chest organs.
- Performing a study of sputum and bronchial lavage water.
In the absence of data that would indicate an obvious erosive and ulcerative process, it is necessary to conduct a detailed oncological search.