Markers of hepatitis C are particles of the virus and antibodies to it detected in the blood. Antibodies are represented by immunoglobulins (plasma protein compounds) of the IgG and IgM classes. If they are present in the blood, this means that the person is infected with a viral infection or has suffered from it. Molecular biological diagnostic methods are highly accurate - more than 98%. In combination with serological tests, doctors detect HCV viral particles and determine the stage of the disease.
Who needs to get tested
During complex diagnostics, two types of markers are detected in the body of patients:
- antigens are RNA particles of the virus, to which immunoglobulins of the IgM and IgG types are formed;
- Antibodies (anti-HCV) are protein compounds in the blood plasma whose action is aimed at destroying the virus.
A blood test for markers of a viral disease is carried out when:
- previous hepatitis of unspecified origin;
- increased blood concentrations of liver transaminases (ALT, AST);
- screening examination;
- obvious signs of viral liver damage;
- medical examination of workers of medical institutions;
- examination of people at high risk of HCV infection;
- monitoring the effectiveness of antiviral therapy;
- donor blood transfusion;
- the birth of a child from a sick mother;
- pregnancy planning;
- questionable data from other studies.
Detection of anti-HCV in the blood does not confirm the presence of a viral disease. RNA analysis is of key importance in diagnosis. Its presence indicates a positive test result for markers of HCV infection.
How to get tested for hepatitis markers
To diagnose the hepatitis virus in the body, venous blood is needed. She is taken in a hospital setting on an empty stomach. The study does not require a special preparatory period, however, a few days before the procedure it is recommended to give up alcoholic beverages, smoking, coffee and medications. In addition, physical activity is prohibited. The results of the study will be ready in a few days.
How to prepare for diagnosis
To confirm the diagnosis of HCV infection, laboratory tests are prescribed - analysis for serological and molecular markers of HCV. To carry them out, blood is taken from the ulnar vein. To eliminate errors in the results, the following are trained:
- 2 weeks before the test, refuse any alcohol-containing drinks;
- for 7-10 days follow diet No. 5 according to Pevzner, in which fatty meat, fried and spicy foods are excluded from the diet;
- half a day before blood sampling, do not smoke, try not to worry;
- analysis for HCV markers is done in the morning on an empty stomach.
To avoid false results, you must tell your doctor if you are taking any medications. If possible, they are abandoned 2-4 weeks before the examination.
Decoding
Analysis for hepatitis markers can be both qualitative and quantitative. In the first case, the specialist needs to determine whether a pathogen is present in the blood; in the second, it is possible to determine the type of specific pathogen. This allows you to prescribe an effective and safe treatment regimen that promotes rapid recovery of the body. Please note that decoding must be carried out by a qualified attending physician.
Negative result
If the test result for hepatitis markers is negative, we can conclude that the person is completely healthy. You can be sure of this, since this disease manifests itself immediately after infection. A favorable result is indicated only by a condition in which the research results are below normal.
Positive result
If the test results show a positive result, then two weeks later the patient is sent for a repeat blood test. This allows you to verify the correctness of the research.
Keep in mind that a positive result may indicate an acute form of this disease. If this was not the case, then the specialist concludes that the incubation period has passed or that the person is a carrier of this virus. An individual treatment regimen for the disease is selected for him, which allows him to restore his liver.
© 2020 – 2020, . All rights reserved.
Types of tests for hepatitis C virus
To identify markers for hepatitis C, 2 main types of research are carried out - molecular and serological. Specific immunoglobulins in the blood serum signal that the liver is damaged by infection. These studies are performed for the primary detection of antigens and antibodies to HCV.
For differential diagnosis, additional studies are carried out, the results of which determine the stage of the disease and appropriate treatment tactics.
Serological markers
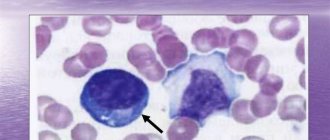
Serological indicators of hepatitis C (antibodies) are protein compounds in the blood that are synthesized by the immune system in response to the penetration of the Hepatitis C Virus (HCV) into the body.
During a serological study, anti-HCV is detected, that is, antibodies to viral particles. Positive results indicate previous disease or active inflammation of the liver.
In most modern clinics, markers of viral hepatitis C are determined during an enzyme-linked immunosorbent assay (ELISA), the essence of which is as follows:
- protein complexes are captured from blood serum;
- they are treated with labeled enzymes;
- The type of antibody is determined from the observed color reaction.
Regardless of the HCV genotype, ELISA can determine the amount of IgG antibodies class G and IgM class M. The specificity of the second generation tests is 95%. The detection period for HVC core IgM markers does not exceed 9-10 weeks after infection.
The third generation enzyme immunoassay was developed based on the NS5 antigen. The advantage of the technique is a significant reduction in the serological window - the presence of HCV markers in the blood can be confirmed 4-6 weeks after infection. Its sensitivity and specificity is 99%. If HCV IgG type markers are detected, this indicates a previous infection or the presence of chronic hepatitis.
Serological screening is a mandatory test for the initial diagnosis of a viral disease. But to confirm the data obtained, they resort to additional research.
Molecular markers
Molecular biological methods are aimed at detecting particles of an infectious agent. Based on the results of the examination, a positive serological test for markers such as anti-HCV and replication, that is, reproduction, of the virus is confirmed.
In virology, two types of research are used:
- Qualitative – performed to test the donor’s blood or confirm hepatitis in persons with detected anti-HCV (the result is positive or negative - there is a virus or there is no virus).
- Quantitative – plays the role of a marker of infectious load. The concentration of virions determines the pathogen RNA carrier and the activity of liver inflammation.
Molecular test systems allow you to perform PCR (polymerase chain reaction) in real time. The degree of viral load on the body depends on the stage of the disease and varies in the range from 10 to 10 million international units in 1 ml of blood.
Quantitative PCR diagnostics serves as a marker of RNA virus replication in low-grade hepatitis. The analysis is performed at 4, 12 and 24 weeks of interferon therapy. A repeat molecular test is performed 24-48 weeks after taking the medication.
Additional Research
After confirming the diagnosis, the genotype of the pathogen is determined. The method of further treatment and the prognosis of complications depend on the data obtained. To do this, analyze the NS5 region of the HCV protein.
Test systems are imperfect, which makes it difficult to diagnose hepatitis with recently identified new genotypes.
Additionally, a puncture biopsy of the liver and histological analysis of the tissue taken are performed. Based on examination under a microscope, the severity of changes in the structure of the organ and the location of the lesions are determined. Structurally, histological markers of hepatitis B and C differ little from each other. The accuracy of predicting viral infection based on tissue examination data exceeds 76%.
Hepatologists identify several histological markers of HVC infection:
- fatty degeneration of hepatocytes (liver cells);
- stellate fibrosis of the parenchyma;
- stepwise necrosis of hepatocytes;
- formation of the connective tissue framework of the liver.
If complications are detected - hepatosis, hepatocellular carcinoma - the treatment tactics are adjusted.
Description of markers
To diagnose the disease, clinical tests or rapid tests are used. They allow us to identify different stages of the disease: infection, recovery, development.
Reference. Antigens are foreign substances to the body, upon the appearance of which antibodies are formed. These are protein molecules or fragments of HBV that appear after the body is infected. Antibodies are protein compounds that prevent the virus from multiplying and neutralize its toxins.
HBV marker table:
| Marker type | Clinical significance |
| HBs-Ag | Hepatitis B virus surface antigen. This component of the HBV envelope identifies the hepatocytes into which the virus will invade. |
| HBe-Ag | A virus protein that indicates its active reproduction. If the diagnostic results are positive, this indicates that the disease has worsened or the likelihood of infection is high. |
| HBcore-Ag | This is a nuclear antigen of HBV (located in cell nuclei), which is detected during a liver biopsy (intravital sampling of tissue fragments). |
| Anti-HBs | Antibodies to HBsAg. When the immune system comes into contact with the protein, immunoglobulins (IG) begin to form, which prevent it from penetrating the liver cells. |
| HBe antigen | Total antibodies to HBe, which are detected at the beginning of recovery. |
| Anti-Hbcor-Ag | General antibodies to HBcore-Ag. It is used to detect hepatitis that has long ended. |
| Immunoglobulins class M to HBcore-Ag | This marker indicates the presence of an acute infection. |
| Antibodies class G to Hbcor-Ag | When they are identified, we are talking about current or completed HBV. |
Hepatitis B virus DNA indicates the presence of an infectious agent. If this marker is present for a long time, the infection becomes chronic. This indicator indicates that HBV is multiplying rapidly and destroying the liver. Hepatitis B virus DNA can be detected in the early stages of pathology.
HBsAg – anti-HBs complex
HBs Ag is an early marker of hepatitis B. It is also called the Australian antigen because it was first identified in the indigenous people of Australia. As mentioned earlier, this is the outer protein coat of the pathogen. This genotype has several subtypes: ayw, aur, adw, adrq, adrq+, which differ slightly in structure.
Sometimes it happens that when interpreting an HBsAg test, a false positive result may be obtained
This marker can be detected during the incubation of hepatitis or within 1 - 1.5 months after the onset of the first symptoms. If this indicator is detected in the bloodstream for more than six months, then the likelihood of developing chronic HBV increases.
Donor blood is recommended to be tested for the presence of HBs Ag. However, many enzyme immunoassays do not accurately detect this marker in patients. Then the likelihood of a false negative or false positive test for hepatitis B increases. A false negative result is obtained if the test is carried out 3 to 4 weeks after possible infection, if the disease has a passive course, the patient has a low concentration of HBs Ag or rare subtypes. A false positive result is caused by various factors: improper sampling of biological material, cancer, etc.
To assess the course of the pathology, as well as predict its outcome, it is important to monitor the HBs Ag – anti-HBs system. Antibodies to the surface antigen of the virus in hepatitis B (acute form) are detected after a long period of time after the disappearance of HBs Ag.
Reference. The period during which the HBsAg–anti-HBs complex is not monitored is the serological “window” phase. The timing of the appearance of antibodies depends on the state of immunity of the infected person. As a rule, the “window” phase lasts from 3 – 4 months to 1 year.
If anti-HBs are detected again, this indicates that post-infectious immunity has formed. That is, the patient recovered from HBV.
If antibodies are detected during an acute infection or immediately after HBsAg has disappeared, then this is a bad sign. Then the risk of severe hepatitis B increases, which is accompanied by signs of hepatic encephalopathy (neuropsychic disorders due to liver dysfunction).
In chronic HBV, both markers may appear simultaneously.
Antibodies to HBs may be present for the rest of life.
Recombinant HBsAg vaccines are used to prevent hepatitis B
Anti-HBsAg are the only components of the immune system that have protective properties. That is, these immunoglobulins protect the body from re-infection with hepatitis B.
Currently, recombinant HBsAg vaccines are used to prevent type B infection. The solution is administered intramuscularly, after which antibodies begin to be released after 14 days. To form full immunity, the vaccine is given 3 times.
Vaccination is considered successful if the antibody level exceeds 100 mIU/ml. After 9–12 years, their concentration may decrease slightly. If the amount of immunoglobulins does not exceed 99 mIU/ml, then such an immune reaction is considered negative or weak.
Reference. The effectiveness of the immune response after administration of the vaccine is reduced if the patient is under 2 or over 60 years of age, suffers from chronic infections, has a weakened immune system, or the dose of the drug is insufficient. Then it is necessary to administer an additional dose of the vaccine after 1 year.
Resistance to the vaccine is observed in patients with HIV or weighing more than 70 kg. According to doctors, in order to achieve adequate results of immunoprophylaxis of hepatitis B, the dose of the drug needs to be increased.
Carefully. It is not recommended to vaccinate people who have had HBV, as this puts an excessive burden on an already weakened immune system. Therefore, before vaccination, it is necessary to conduct tests for the presence of HBsAg, anti-HBs, as well as HB core antibodies. If at least one of the markers is present in the blood, then vaccination is contraindicated.
If the number of antibodies decreases after immunization, it is recommended to carry out revaccination (re-vaccination). Although in most cases, post-vaccination immunity remains, even if the concentration of anti-HBsAg decreases. Only patients with HIV, chronic kidney failure, liver disease, as well as persons prescribed hemodialysis (extrarenal blood purification) need an additional dose of the drug.
Antibodies to HBcore-Ag
This antigen is localized only in the nuclei of the liver cells of an infected person. It can be detected by liver biopsy; HBcore-Ag does not circulate in the bloodstream. Due to the fact that the antigen occupies a core position in the viral particle, it is highly immunogenic. It is for this reason that antibodies to it begin to be released almost from the first days of the disease, when there are still no external symptoms.
Antibodies to HBcore-Ag are divided into 2 types: immunoglobulins class M (IgM) and class G (IgG). IgM is detected during the latent period, when there are no clinical manifestations. This marker indicates acute HBV. It can be observed from 6 months to 1 year, and after treatment it disappears. IgM is detected when a chronic process worsens.
Testing for IgM and IgG helps diagnose hepatitis B in the “seronegative” period, when other HBS markers are absent.
Reference. Sometimes HBcore-IgM and IgG may indicate diseases of the musculoskeletal system.
Interpretation of analyzes
A gastroenterologist or hepatologist can accurately interpret the results of serological, molecular and histological analysis. When interpreting the results, data from additional studies must be taken into account - biochemical blood tests, ultrasound and MRI of the liver, coagulograms.
What do the survey results mean:
- The presence of serological markers in the blood serum does not indicate continued replication of the virus. This often indicates a past infection.
- The absence of anti-HCV markers does not prove that a person is healthy. In the early period, in the acute form of the disease or in immunodeficiencies, it is not possible to detect antibodies to HCV.
- Recipients who have received contaminated blood transfusions often show markers of hepatitis C. But this does not yet signal a viral infection.
- If antibodies and RNA are detected simultaneously, this signals acute hepatitis or a relapse of an indolent infection.
Decoding combinations of HCV serological markers
| RNA-HCV | anti-HCV | Data interpretation |
| — | + | Virus extinction; acute hepatitis with minimal primary spread of RNA virus in the blood |
| — | — | Hepatitis C is absent |
| + | + | Acute form of the disease or relapse of indolent infection |
| + | — | False positive RNA test result; chronic hepatitis due to immunodeficiency; initial stage of acute hepatitis |
Experts warn patients against self-interpretation of data and self-medication. Hepatitis C is a dangerous infection that can only be treated under the supervision of a doctor.
General information about hepatitis
The term "hepatitis" can be described as a collective term. A disease of an infectious nature is caused by viruses of various types that are transmitted to humans in such ways as:
- fecal-oral (acute viral hepatitis A, HEV);
- parenteral (HBV and HCV);
- vertical (from mother to her fetus - HBV and HCV);
- transplacental (HBV and HCV).
Hepatitis B is one of the parenteral forms that provokes negative consequences for the liver (cirrhosis, cancer). In the absence of timely treatment, the disease often becomes chronic.
The mechanism of transmission of infection involves the fact that biological fluids of a sick person enter the blood of a healthy person. This can happen during unprotected sexual intercourse, during medical procedures without a proper disinfection regime, or when using a shared needle with a patient when injecting drugs.
Hepatitis A is the popular name for “jaundice”, “Botkin’s disease” is an intestinal disease. The pathogen enters the body with contaminated products, through household items shared with the patient, infected with his secretions. Having a shorter incubation period than parenteral hepatitis (30-45 days versus six months), HAV provides a real opportunity to identify the source of infection, as well as patients in the initial form of the disease among contacts.
Hepatitis C is a disease caused by the HCV virus. The route of transmission is similar to HBV. An aggressive and difficult to correct form of the disease. According to many experts, there is no effective treatment for advanced forms.
Hepatitis E is the result of exposure to HEV. A special feature is the high level of involvement of the kidneys in the process. The infection is transmitted by the fecal-oral route. It is especially dangerous for pregnant women in the last trimester. The likelihood of recovery from the virus is high, even spontaneously.
Can marker testing be false?
Determining serological markers does not always mean that a person actually has hepatitis. Despite the high accuracy of ELISA, diagnostic results may be affected by:
- severe immunodeficiency conditions;
- pregnancy;
- multiple sclerosis;
- taking medications with heparin;
- exacerbation of respiratory diseases;
- vaccination;
- autoimmune systemic connective tissue diseases;
- hematological malignant tumors;
- systematic hemodialysis.
To avoid false diagnostic results, test systems are now used that are not affected by the presence of C-reactive proteins or rheumatoid factor in the blood. However, such systems are not yet available in all clinics.
What can affect test results?
After listening to the doctors’ recommendations, patients prefer to exclude everything the day before. But fasting can negatively affect the examination results. If this lasts more than two days, then the amount of bilirubin in the blood increases sharply. And this is an important indicator when examining for hepatitis B and C. The amount of bilirubin in the blood gives an assessment of the degree of damage to liver cells (hepatocytes).
Meals before taking tests should not be plentiful, but complete. Raw vegetables and fruits are not prohibited. But yellow, red and orange are best eaten another day. On the eve of the examination, it is advisable to go to bed in a good mood and wake up no later than an hour before the examination.
Physical activity, increased emotional state, and stress cause a sharp jump and then a decrease in indicators. This situation persists for days. Therefore, it is better to exclude this. Different types of massage are not advisable.
Relatives take care of your good mood before taking tests. The patient is afraid of voicing the diagnosis. It is important to reassure him, assuring him that this simply cannot happen. If a person is in a panic state, the level of iron, cholesterol, and glucose in the blood increases. The beach, bathhouse and sauna are contraindicated. These procedures should be canceled at least two days in advance.
This is interesting: The first signs and symptoms of hepatitis B in women
What to do if hepatitis C markers are positive
Even the accidental detection of antibodies to the causative agent of hepatitis requires contacting a doctor. Diagnosis and treatment are carried out by a hepatologist, infectious disease specialist or gastroenterologist. To confirm the diagnosis, the following are additionally prescribed:
- coagulogram;
- fine-needle liver biopsy;
- molecular biological research;
- Ultrasound and MRI of the liver;
- blood chemistry;
- histological analysis.
Once the diagnosis is confirmed, treatment is carried out, which is aimed at destroying the viral infection and maintaining liver function.
In 2011, the old therapy with Ribavirin and Interferon was replaced by direct antiviral drugs (DAAs) - Asunaprevir, Paritaprevir, Voxilaprevir, Ledipasvir, Dasabuvir. The effectiveness of some of them reaches 95-98%.
Why do you need to donate blood for markers of viral hepatitis?
Modern blood testing methods make it possible to make a diagnosis at an early stage. They detect the presence of the virus in the blood with 99% accuracy. Also, such tests are done to determine the form of the disease and its stage. They are needed to select tactics and treatment regimens, to adjust therapy if necessary, and to evaluate its effectiveness.
Therefore, a test for markers of hepatitis is most often prescribed when this disease is suspected, for example, when symptoms appear. The doctor gives a referral for such tests if the patient complains of nausea, vomiting, loss of appetite, pain in the right side, weakness, diarrhea, if he has a change in the color of feces and urine, itching, yellowing of the skin and whites of the eyes.
If the diagnosis is confirmed, it is repeated during treatment to monitor the effectiveness of the therapy, as well as after its completion. Then it is recommended to undergo testing for markers six months after recovery and after 2 years. This will help identify virus carriage or the transition of the disease to a chronic form.
For preventive purposes, it is recommended to undergo this test in the following cases:
- when planning pregnancy;
- preparation for vaccination;
- before surgical interventions;
- during preventive examinations;
- before donating blood;
- if necessary, hemodialysis;
- when elevated levels of liver enzymes are detected;
- if there are symptoms of the disease;
- for people at risk – for drug addiction, frequent change of sexual partners;
- if infection is suspected, for example, after a cut or injection with a suspicious object, or communication with a sick person.
It is imperative that medical workers, especially those who come into contact with blood, regularly conduct such tests. These are nurses, laboratory assistants, gynecologists, dentists. But it is also done to everyone for whom a personal medical record is issued.
Prices for diagnosing hepatitis C in Moscow laboratories
If viral hepatitis is suspected, the doctor prescribes laboratory and instrumental tests, the results of which determine:
- presence of HCV in the blood;
- pathogen genotype;
- severity of inflammation and stage of the disease.
The cost of the examination depends on the type of medical institution, type and number of tests:
| Type of examination | Cost in rubles |
| qualitative PCR for hepatitis C | 1000-1500 |
| Hepatitis C quantitative PCR | 4000-4500 |
| IgM immunoglobulin test | 380-450 |
| IgG immunoglobulin test | 390-470 |
| needle biopsy of the liver | 14000-14500 |
| MRI of the liver | 2500-2700 |
| coagulogram | 1150-1200 |
| biochemical liver tests | 1300-1500 |
With timely detection of markers of viral hepatitis and antiviral treatment, the prognosis is favorable. Ignoring the disease is dangerous due to chronic inflammation, complications - hepatosis, hepatocellular carcinoma, cirrhosis. Therefore, if you suspect an infection, be sure to contact a gastroenterologist.
Explanation of results (table)
Viral hepatitis markers are deciphered by a specialist. Having received the answers from the laboratory test, the patient needs to see a doctor to determine further tactics.
Below is a table with diagnostic results.
| Hepatitis | Index | Characteristic | Decoding the result |
| A/E | anti-HAV/HEVIgM | M class antibodies produced in response to infection are counted | Acute course of pathology |
| Ig Ganti-HAV/ HEV | Class G | Past pathology | |
| IN | HBsAg | Surface antigen is tested | Infection rate |
| HBeAg | Nuclear “e” antigen is detected | Study confirms intensive reproduction | |
| HBcAg | Nuclear “core” antigen is determined | Indicates replication | |
| anti-HBc (total) | Represents total antibodies | Allows you to confirm pathology in case of negative HBsAg | |
| IgManti-HBc | Immunoglobulins to nuclear antigen are determined | Indicates an acute course, and is also an indicator of the rate of replication during chronic pathology | |
| anti-HBe | Same | Beginning of convalescence | |
| anti-HBs | Antibodies to the surface type of antigen are being studied | The result indicates a fulminant course or a previously suffered pathology | |
| HBV-DNA | The genetic material of the pathogen is determined | Indicator of active infectious process | |
| D | IgManti-HDV | Antibodies M are detected | Indicates a past illness |
| IgGanti-HDV | The same, only class G | Acute stage of the disease | |
| HDAg | Examines pathogen antigen | Indicator of presence in the body | |
| HDV-RNA | Genetic material of the viral agent | Active reproduction | |
| WITH | anti-HCVIgG | Class G antibodies are detected | Possible infection or past illness |
| anti-HCVcoreIgM | Type M antibodies against nuclear proteins are detected | Acute process or exacerbation of chronic course | |
| anti-HCVcoreIgG | The same, only class G | Previous pathology or carriage | |
| anti-HCV NS | Antibodies against non-structural proteins are determined | Chronization of the process | |
| HCV-RNA | Part of a pathogenic agent | Active reproduction | |
| G | HGV-RNA | Genetic material of the pathogen | Same |
Hepatitis D and G
Hepatitis D virus is an anthroponotic infection. Infection occurs through any fluids of an infected person, but only those who have hepatitis B are susceptible to it. The symptoms of these diseases are largely similar, but the type D virus often causes ascites and edema. Tests are prescribed primarily for patients with hepatitis B and those who take narcotic drugs.
The disease can be identified by antigens and antibodies to them:
- RNA of this virus. This marker is present in the body during the period of active spread of infection.
- Anti-IOP IgM appears during the acute period.
- HDAg. The presence of antigen in the blood confirms infection.
- Anti-IOP IgG. The person has already suffered the disease in the past, and now he has immunity to this type of virus.
The hepatitis G virus is spread through sexual contact and through repeated use of disposable syringes. Less commonly, transmission of the virus occurs through acupuncture or body piercing. Like type D, this type of disease can only occur in people with hepatitis C, B or D. Long-term absence of symptoms leads to a chronic course and increases the risk of developing cirrhosis of the liver.
Early diagnosis is possible by testing blood to detect markers:
- Virus RNA. In this case, a diagnosis of acute hepatitis G is made.
- Anti-HSG. A sign that the patient has suffered hepatitis and now has immunity to this disease in his body.
Analysis process
Blood for analysis is taken from a vein.
Blood can be taken for analysis at home or in a hospital. The procedure requires sterile instruments and disposable materials. Before it begins, the patient’s forearm is tied with a tourniquet. Thanks to this, the blood vessels become more convex. At the next stage, the injection site is treated with cotton wool soaked in alcohol. The needle is inserted into a vein located in the elbow area.
Blood taken from a vein is drawn into a previously prepared laboratory container. After the required amount of biological material has been collected, the needle is carefully removed. Then all that remains is to press the cotton swab to the injection site. The patient is advised to clench his arm at the elbow. This is done in order to stop the bleeding and prevent the appearance of hematomas.
If the procedure is carried out in full accordance with the correct technique, it will not cause any discomfort. The blood is delivered to the laboratory as soon as possible. In 2 hours it will be too late. If the patient becomes ill during the procedure, the nurse uses ammonia.
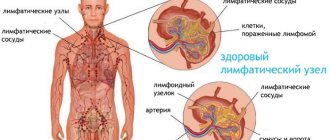
What are markers and what are they for?
The peculiarity of hepatitis C and B is that the early stages of the infection do not have characteristic symptoms, and when the patient comes to the clinic with complaints, his liver is severely affected and its functions are impaired. Early diagnosis will help to avoid such development.
Markers are specific antigens and antibodies to these diseases. Detection of specific antibodies in the blood serum can confirm whether a person has one or another type of hepatitis. An important feature is that markers are detected even at an early stage of the disease in the absence of symptoms.
To identify specific and serological markers for hepatitis, several types of research are used.
- Diagnostics based on immunological research methods.
- Using the immune response to viruses.
- Using a specialized screening study.
- By performing an enzyme immunoassay.
Depending on the methods and purpose of diagnosis, 2 types of tests are performed for hepatitis markers:
- specific;
- nonspecific.
Specific analysis
During such a study, it is possible to determine the type of virus that caused the disease. Specific markers are hepatitis antigens.
Antigen represents individual elements of the virus. When exposed to a favorable environment, these antigens participate in the production of new virus cells. Unused fragments are carried throughout the body by the bloodstream.
Non-specific analysis
This type of marker includes antibodies to existing antigens. This diagnostic method becomes possible due to the ability of the human body to produce antibodies (cells aimed at fighting pathogens). The detection of such antibodies to hepatitis antigens indicates the presence of pathological processes in the liver tissues.
How to test for hepatitis B and C markers?
For the study, 5 ml of venous blood is taken. She can give up at any time of the day. But when conducting repeated studies, it is advisable to donate blood at the same time. Blood is taken from a vein in the elbow. Before the procedure, the patient needs to sit for at least 15 minutes to calm down and restore breathing after walking. You cannot take blood after an X-ray examination or ultrasound. Physiotherapeutic procedures can also affect the results. If a repeat test is required to confirm the diagnosis, it is advisable to take it in the same laboratory as the first. This will make the results more reliable.
In order for this study to be used to prescribe treatment, it must be carried out with confirmation of identity, that is, upon presentation of a passport. Many people try to take such an analysis anonymously, since positive results are necessarily transferred to the State Sanitary and Epidemiological Supervision Authority, but doctors will not take such a study into account. Therefore, it is better to do everything officially.