Clinical signs of inflammation of the pancreas are difficult to distinguish from other diseases of the digestive tract; they all cause similar symptoms: abdominal pain, dyspepsia. In this case, blood tests for pancreatitis play a major role. Other tests, for example, examination of stool, saliva, and urine, determine the form of pancreatitis - acute or chronic. For a doctor treating pancreatitis, you need to know exactly whether you are dealing with an acute form of the disease or an exacerbation of a chronic inflammatory process in the gland.
blood test for pancreatitis
Methods for determining chronic pancreatitis
The pancreas produces enzymes that break down proteins, fats and carbohydrates, and also synthesizes the hormone insulin, which delivers glucose to the body's cells. Diagnosis of pancreatitis involves determining the concentration of digestive enzymes and gland hormones in the bloodstream.
- Amylase – is involved in the processing of carbohydrate foods (breaks down starch); A distinction is made between pancreatic amylase and general α-amylase (diastase).
- Trypsin and elastase – ensure the digestion of proteins.
- Lipase - breaks down fats; its deficiency is detected by an increase in cholesterol in tests.
Lack of insulin leads to increased sugar in the bloodstream.
tests for pancreatitis
Pancreatic enzymes normally become active only in the intestines. If the movement of pancreatic juice through the ducts to the intestines is difficult, some enzymes are activated in the organ itself, “digesting” it - an inflammatory process occurs. It can be sluggish and occur without pain, but is accompanied by degeneration of organ tissues that are deprived of secretory activity. Tests for chronic pancreatitis reveal pathological processes and functional insufficiency of the pancreas. If chronic pancreatitis is suspected, diagnosis includes the following laboratory tests;
- Complete blood count (CBC) – detects inflammation in the body;
- Biochemical analysis - the most important diagnostic test for pancreatitis - provides information on the content of digestive enzymes, as well as glucose and cholesterol in the blood.
- Urine analysis for diastase - may show a slight but prolonged excess of amylase in the urine - a sign of chronic pancreatitis; a decrease in amylase compared to the norm indicates degeneration of the gland tissue.
- Stool analysis: fatty grayish stool with undigested food remains indicates a dysfunction of the pancreas.
- Testing saliva for amylase levels will help differentiate acute from chronic inflammation.
Treatment of the chronic form consists of organizing proper nutrition and taking medications that correct secretory insufficiency of the organ. Sick people quickly understand whether they can eat spicy, fatty, salty foods. As soon as you break your diet for pancreatitis, after a few hours a painful attack begins, which must be distinguished from an acute form of inflammation of the pancreas.
Instrumental diagnostic methods
By and large, all patients with this disease undergo instrumental examination only with an ultrasound examination of the abdominal organs. This is due to the fact that the diagnosis can be easily made after interviewing, examining the patient and obtaining laboratory tests. Ultrasound is a high-quality and reliable first-line study, as it is inexpensive and highly informative. All other studies are of little information and are not highly effective for diagnosis. Their use is justified only when it is not possible to visualize the affected parts using ultrasound examination or when there is a suspicion of the presence of a space-occupying formation in the organ (cancerous tumor, cyst, pseudocyst). In this case, the question arises about the surgical operation and the extent of resection.
Ultrasound examination
"Gold standard" for diagnosis. The doctor will easily see diffuse changes in the tissue of the affected organ, thickening and swelling of the pancreatic capsule. In chronic pancreatitis, calcifications and petrifications, areas of parenchyma destruction, are detected. The advantage of this study is that it makes it possible to assess the condition of other organs (gallbladder, liver and their ducts). This is important when the outflow of secretions is impaired due to stones and the presence of cholecystitis, since in this case all the conditions for the development of the disease are created.
Important! Currently, new methods of ultrasound diagnostics have been developed. In particular, endoscopic ultrasound and intraductal ultrasound of the pancreas. These studies make it possible to insert sensors into the stomach or into the ducts themselves, and the doctor can study in more detail and give an opinion on the condition of the organ. The disadvantage of these studies is their invasiveness, which exacerbates inflammation and organ destruction.
CT scan
Most often, this study is prescribed when complications occur. X-ray examination allows you to study in detail the structure of an organ (including the circulatory system), assess the degree of destruction, and determine the amount of living and healthy tissue.
Endoscopic retrograde cholangiopancreatography (ERCP)
For biliary-dependent pancreatitis, ERCP is performed. A special probe is inserted into the main duct, the opening of which opens on the large duodenal papilla, and a contrast agent is supplied. After this, the patient is given an x-ray. Such an examination allows you to assess the patency of many (even the smallest) ducts, determine the presence or absence of stones and other possible obstacles (strictures, adhesions, kinks). During the examination, small stones can be removed, which will then be removed naturally. This surgical method is minimally invasive, so it is now preferred.
Rarely used instrumental diagnostic methods
- Fibrogastroduodenoscopy (FGDS) - allows you to assess the condition of the major papilla of the duodenum, evaluate the final sections of the duct itself, and evaluate the functionality of the sphincter of Oddi.
- Plain radiography of the abdominal cavity is a study used for differential diagnosis. Often, with this disease, there are no changes in the image, except in cases where petrification (areas of calcification) have already formed in the pancreas. This sign allows us to fully guarantee that the patient has chronic pancreatitis.
- Laparoscopy. More of a therapeutic rather than a diagnostic method. It is used in controversial situations when the above studies could not completely visualize the affected organ. During diagnosis, various surgical procedures can be used for therapeutic purposes.
Diagnosis of acute pancreatitis
In acute inflammation, intensive destruction of the gland tissue by its own enzymes occurs, which is accompanied by poisoning and deterioration of the general condition of the body. Diagnosis of pancreatitis in its acute form begins with taking into account clinical manifestations. The main symptom is pancreatic colic - acute pain in the epigastric region, which can be so severe that the patient loses consciousness.
vomiting attack
The pain syndrome is aggravated by attacks of vomiting that do not bring relief. In such a situation, doctors prescribe tests that are necessary to establish the fact of inflammation in the body and assess the extent of damage to the gland. Standard tests for pancreatitis are marked “cito!”, and should be done as quickly as possible:
- complete blood count (CBC);
- blood biochemistry - characterized by a sharp increase in amylase content in the blood, since with such a pathology it is activated not in the intestines, but in the pancreas itself and enters the bloodstream;
- biochemical analysis of urine shows an increase in diastase sometimes by 200-250 times; to monitor the dynamics of acute inflammation, urine should be taken every three hours;
- A stool analysis in acute pancreatitis may indicate that the process of digesting food is disrupted.
increase in amylase
An increase in amylase in the blood is also characteristic of pathologies such as cholecystitis, diabetes mellitus, and pain syndrome of the “acute abdomen” type may indicate appendicitis, perforation of an ulcer and other diseases of the abdominal cavity. To clarify pancreatitis, differential diagnosis is necessary. Before recognizing acute inflammation, the pancreas is examined by other diagnostic methods. Ultrasound, MRI, radiography - determine the localization of the pathology, its nature (inflammation, cyst, tumor).
Symptoms of the disease
In order to understand in time that problems are starting in the pancreas, you need to be attentive to all signals from the body. At different stages of the development of the disease, characteristic symptoms arise that cause discomfort and health problems:
- Pain. As soon as inflammatory processes begin and blockage of the ducts, a person feels an unpleasant sharp pain under the ribs. Depending on the location of the disease, it may hurt on one side, the side, or immediately along the entire circumference of the ribs. The pain is constant and does not subside even at rest.
- Vomit. The stomach stops digesting the food eaten; without enzyme tablets, vomiting immediately appears. Vomiting occurs with every meal.
- Heat. Inflammatory processes in the body and intoxication provoke a protective reaction of the body and an increase in body temperature to 38–38.5 degrees.
- Jaundice. When the pancreas swells, its body can put pressure on the bile ducts, resulting in obstructive jaundice. A person develops all the signs of jaundice: yellowed eyes, palms and skin.
- Diarrhea or constipation. Problems of the digestive tract immediately make themselves felt; lack of enzymes and intoxication cause difficulties with bowel movements.
Blood tests
Informative tests for pancreatitis are a blood test: blood is taken from a finger for a general analysis; from a vein - for biochemical.
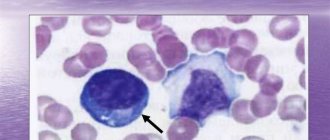
General analysis
Data from a general analysis show the presence of an inflammatory process in the body. In acute pancreatitis, the blood formula changes significantly.
- The number of leukocytes sometimes increases tens of times. Normally, the leukocyte content is no more than 9∙109/l.
- The erythrocyte sedimentation rate (ESR) increases, its normal value is 15-20 mm/h.
- The hematocrit (the ratio of the volume of red blood cells and plasma) increases, the blood becomes thick due to an imbalance of water-salt balance and fluid loss. The normal hematocrit is 46-48%.
complete blood count for pancreatitis
With chronic inflammation of the pancreas, the following changes are noted in a blood test:
- the number of white blood cells sometimes even decreases, but usually there is a slight increase over a long period of time;
- ESR slows down;
- there is a decrease in hemoglobin levels - which indicates developing anemia against the background of exhaustion of the body. Normal hemoglobin level is 120-160 g/l
Blood biochemistry
During a biochemical blood test for pancreatitis, attention is paid to the following data:
blood chemistry
- the level of enzymes produced by the pancreas: diastase, lipase, trypsin;
- glucose content;
- the amount of proteins of the acute phase of inflammation (globulins, C-reactive protein);
- total protein concentration.
Complications in the development of pancreatitis are indicated in a blood test by low calcium levels, the appearance of tumor markers, and an increase in glycosylated hemoglobin.
Pancreatic enzymes
When the pancreas becomes inflamed, its cells are destroyed, the enzymes that were in them enter the blood - their level increases sharply, which indicates the activity of the inflammatory process.
Amylase
The most characteristic sign of pancreatitis is a jump in amylase in the blood. At the very beginning of acute pancreatitis and in the first hours of relapses of a chronic disease, a rapid increase in pancreatic amylase in the bloodstream begins. This indicator reaches its maximum value by the end of the first day, then it decreases, and on the 4th-5th day it gradually normalizes.
amylase in the blood
It should be noted that the value of total amylase (diastase) does not always indicate the development of pancreatitis. This enzyme is produced by both the pancreas (P-type) and the salivary glands (S-type). An increase in α-amylase with normal P-type levels is not a sign of pancreatitis. In the chronic form of the disease, sometimes there is even a decrease in the enzyme in the blood, which may indicate deep damage to the gland cells that produce this secretion.
Lipase
As part of pancreatic juice, lipase enters the intestine, where it promotes the breakdown of dietary fats. Its content in the blood should be 20 thousand times less than in pancreatic juice. An increase in the level of lipase in the bloodstream - hyperlipasemia - means that fatty foods in the intestines are not completely digested, this leads to increased cholesterol in the blood, as well as changes in stool. Both of these signs, combined with an increase in lipase in the blood, make it possible to diagnose pancreatitis and other pathologies of the pancreas. The level of lipase in acute pancreatitis begins to increase on the second day from the onset of inflammation and remains at a height of 1.5-2 weeks, exceeding the norm by 5-10 times.
Currently, a radioimmunological method has been developed for the determination of trypsin and phospholipase in blood serum. With exacerbation of pancreatitis, phospholipase activation increases tens and even hundreds of times (at a norm of 2-7.9 ng/l, it reaches 400 ng/l). A low level of lipase indicates damage to gland cells that synthesize enzymes.
Proteases: trypsin and elastase
Proteases break down protein foods in the intestines; when the pancreatic ducts are disrupted, they enter the bloodstream instead of the digestive tract.
- The content of trypsin in the blood in acute forms of pancreatitis increases compared to the norm by 12-70 times - on the first day of illness, and then quickly decreases to normal levels. The chronic course of the disease is accompanied by a low level of trypsin (2-10 times lower than normal), which is an indicator of the death of gland cells that secrete enzymes.
- Elastase is an enzyme that, in acute pancreatitis, remains at a high level for 7-10 days of the disease. At this time, in many patients, the content of lipase and amylase already returns to normal, but the amount of elastase remains significant in 100% of patients with pancreatitis. The higher the concentration of elastase in the blood, the more iron is affected by inflammation, the larger the area of necrosis and the worse the prognosis of the disease. In chronic pancreatitis, diagnosis is carried out by the elastase content in the stool; its low content indicates a weakened ability of the gland to synthesize digestive enzymes.
Glucose level
If inflammation engulfs the endocrine cells of the gland that synthesize insulin, against the background of its deficiency, an increase in blood sugar occurs. Without insulin, glucose cannot be absorbed by the body's cells. The glucose level is very important, since diabetes is one of the common complications of pancreatitis. A more accurate indicator is glycated (glucose-bound) hemoglobin, which gives an idea of the blood sugar level over three months.
glucose level
Protein content
With pancreatitis, the protein content in the blood changes.
- The amount of acute phase proteins (C-reactive protein, fibrinogen) increases - they appear in the blood during any inflammatory processes. With successful relief of inflammation, their number decreases.
- The concentration of total protein and albumin decreases - this is associated with digestive disorders: food entering the intestines is not completely digested due to a lack of enzymes, is not absorbed into the blood, but leaves the body with fecal residues. This indicator is especially characteristic for chronic pancreatitis.
Other indicators
In some cases, other indicators are used to diagnose pancreatitis.
- With inflammation of the pancreas, the concentration of the enzymes ALT (alanine aminotransferase) and AST (aspartate aminotransferase) increases. Normally, these compounds are inside cells, participating in protein metabolism. With pathological destruction of cells, enzymes enter the bloodstream. An increase in ALT and AST in the blood is a sign not only of pancreatitis, it also accompanies diseases of the liver, heart, and severe muscle injuries. In combination with other symptoms of pancreatic pathology, ALT and AST indicators are used to clarify the diagnosis. In acute pancreatitis, the concentration of AST exceeds the norm by 2-5 times, and the ALT enzyme - by 6-10 times.
- Determination of tumor markers in the blood is prescribed to exclude a serious complication of pancreatitis - pancreatic cancer. Specific proteins for gland pathology are CA 19-9 and CEA (carcinoembryonic antigen), which are produced by degenerated cells. An increase in C 19-9 by three times and CEA by two times is a sign of pancreatitis; if these indicators are exceeded, they indicate the possible development of a malignant tumor in the gland. In some cases, a positive result for tumor markers indicates diseases of the liver, stomach, and not the pancreas.
- An increase in bilirubin is observed in the case of an increase in the size of the inflamed pancreas, which impedes the outflow of enzymes from the gallbladder.
Laboratory stress tests
Sometimes, in addition to the tests that are taken on an empty stomach, you also need to take those that are done after certain substances are introduced into the body. This is called a load test. They are different.
Glycoamylasemic test. First, a test is taken to determine the initial concentration of blood amylase. Then the person is given 50 grams of glucose, which he must take orally. A few hours later, the amylase test is repeated. Then both indicators are compared.
Prosein test. First you need to determine what the initial concentration of diastase in the urine is. Then a drug called Proserin is injected into the body. And for two hours, the level of diastase is measured every 30 minutes.
Iodolipol test. After a person wakes up, he empties his bladder, then takes a drug called Iodolipol. The level of iodine in the urine begins to be determined after an hour, every half hour. Such a diagnosis of pancreatic diseases is based on the activity of the lipase enzyme that this organ produces.
Diagnosis of pancreatic diseases is based on the activity of the lipase enzyme, which is secreted in the bladder.
A glucose tolerance test is necessary to diagnose lesions of the endocrine apparatus of the pancreas. The glucose level is first determined on an empty stomach, then after one hour, and then two hours after the patient has taken the glucose solution. This test can only be prescribed by an endocrinologist. It is he who will interpret the test results, because there is a danger of complications that are associated with an increase in the level of this carbohydrate in the blood.
Ultrasound and MRI. A method such as ultrasound is one of the most important in diagnosis. This is because the doctor has the opportunity to see the structure of the gland and consider the possible presence of a cyst or oncology. Normally, this organ transmits ultrasound, as do the liver and spleen. If there are no pathologies and the pancreas is in order, then the size of its tail is about 35 mm, the head is 32 mm, and the body is about 21 mm. There should be no changes in the tissue of the organ, and the contours of the pancreas should be smooth and clear.
An x-ray method is also used if any pathology of the pancreas is detected.
Magnetic resonance imaging, or MRI, is considered one of the most accurate methods for biopsy of the pancreas. It is with the help of this method that one can determine with great accuracy whether the tissues of an organ have increased or changed. Using layer-by-layer sections, you can more accurately determine the location of the cyst or oncological process.
An x-ray method is also used if any pathology of the pancreas is detected. However, only if it is radiopaque. For example, these are stones or cysts.
All of these methods are basic in diagnosing the pancreas.
If you begin to notice symptoms of a malfunction of the pancreas, you should immediately consult a doctor.
You should get tested. This way you will understand whether everything is okay with this organ or whether you need treatment. The sooner an accurate diagnosis is made, the sooner treatment will begin. As a rule, it all starts with an examination by a regular therapist. However, if you have severe acute pain, the ambulance team should take you to the hospital.
This is where the diagnosis will be carried out. Surgeon intervention may also be required. If you want to undergo an examination of this organ for the sake of prevention, you should not delay it. Go as soon as possible to a laboratory where this can be done. Remember that if the problem is not detected in time, all this will lead to serious complications.
Analysis of urine
Analysis of urine
A biochemical urine test is informative in diagnosing pancreatitis. The color of urine becomes a sign of the disease: the light yellow color changes with inflammation to dark yellow or brown. In urine analysis, an increase in diastase is observed. The more active the inflammatory process, the sharper the level of total amylase in the urine rises. This indicator is characteristic not only of acute pancreatitis; amylase in the urine also increases in diabetes mellitus. Severe inflammation is accompanied by ketone bodies, leukocytes and red blood cells present in the urine. Protein is found in urine when its absorption in the intestine is impaired. In the acute course of the disease, urine must be taken repeatedly to monitor the dynamics of amylase in the body.
Urinalysis in chronic gland disease shows a decrease in the level of α-amylase, which is associated with a weakening of the secretory functions of the gland during long-term pathology.
Laboratory tests of the pancreas
Any disturbances in the functioning of the organ must be treated immediately, because they can cause serious human health problems, including death.
It is to identify the disease at an early stage that laboratory diagnostics of pancreatic diseases is carried out.
Frequently identified signs of inflammation in an organ include deviations in research results. Let's look at them in more detail.
Stool analysis
stool analysis
If you have symptoms of inflammation of the pancreas, you need to submit your stool for examination to clarify the diagnosis. To get reliable results, take tests after a dietary meal. You need to consume 105 g of protein food, 180 g of carbohydrate food, 135 g of fat. Stool analysis for pancreatitis provides information about functional disorders of the pancreas.
- The increased fat content makes the stool shiny, with a pasty consistency and high in fatty acids - evidence of a lack of the lipase enzyme in the intestines.
- Changes in stool also affect its color: with pancreatitis, it acquires a grayish tint.
- The presence of undigested residues indicates a general lack of enzymes in the intestines.
- A decrease in the level of elastase-1 in the feces shows how much the secretory function of the pancreas is reduced. In severe cases, fecal elastase levels drop below 100 mcg/g.
Interpretation of biochemical analysis
The final formulation of the diagnosis is made on the basis of research: laboratory and instrumental. When diagnosing inflammation of the pancreas, the main thing is a blood test for pancreatitis; it gives indicators of abnormalities in pancreatic enzymes:
- the level of pancreatic amylase in the blood should not exceed 54 units; with pancreatitis, it increases sharply on the first day of the disease;
- normal lipase content is up to 1.60 units/l, with acute pancreatitis it increases 5-20 times;
- The normal trypsin content is 10-60 μg/l, an increase indicates acute inflammation, a decrease indicates a chronic process.
- The upper limit of normal elastase in the bloodstream is 4 ng/ml; the higher its excess, the more severe the form of the disease.
Laboratory examination provides other informative indicators.
- The sugar content in the bloodstream should not exceed 5.5 mmol/l; with pancreatitis it increases.
- The total protein content in healthy people is 64 g/l; its decrease indicates pathology of the pancreas, lack of nutrition or intestinal diseases.
- Protein norm CA 19-9 – up to 34 units/l; exceeding the level is a sign of pancreatitis, a significant increase is a suspicion of oncology.
- The normal level of cholesterol in the blood is 6.7 mmol/l; in men its level is higher than in women. With diabetes mellitus and pancreatitis, cholesterol levels increase.
- AST and ALT enzymes are normally up to 41 mmol/l; if the level is elevated, there is reason to diagnose pancreatitis.
With a variety of diagnostic methods and indicators, the value of pancreatic amylase on the first day of the disease and the determination of lipase and elastase in subsequent days are informative for the attending physician.
Table of main blood parameters that change during pancreatitis
| Index | Values for pancreatitis |
| Amylase In blood: In urine (diastasis): | ≥150 units/l ≥320 units |
| Lipase | ≥ 60 IU/l |
| Elastase in 1 g of feces | ≤ 200 µg |
| Blood leukocytes | ≥9x109 |
| ASAT | ≥37 U/l |
| AlAT | ≥45 U/l |
| Total protein | ≥83 g/l |
| C-reactive protein | ≥5 mg/l |
| ESR | ≥20mm/h |
| Direct bilirubin | ≥8 µmol/l |
| Indirect bilirubin | ≥19 µmol/l |