Osteoporosis is one of the most common diseases of the 21st century. Its prevalence is associated with the general aging of the planet's population, as well as a decrease in people's physical activity. The condition can be corrected using modern therapeutic methods, provided it is diagnosed in a timely manner. People who are at risk for this disease should regularly check their bones for osteoporosis.
How to identify osteoporosis
Diagnosing osteoporosis can sometimes be difficult because in most cases the disease is asymptomatic and patients do not seek medical help. The most constant symptom of osteoporosis is pain in the sacral and lumbar spine, in the hip joints. Patients sometimes complain of pain in the ankle joints, pelvic bones, and ribs. Pain syndrome. intensifies with changes in weather and atmospheric pressure, and physical activity.
In the future, the pain becomes constant due to overstrain of the spinal ligaments and back muscles. During the period of a fracture of ribs or vertebrae, acute pain is localized at the site of the fracture. If these symptoms are present, doctors at the Yusupov Hospital conduct an examination for osteoporosis using densitometry.
The clinical picture of osteoporosis is characterized by the following features:
- Feeling of heaviness in the interscapular area, general muscle weakness;
- Decreased growth;
- Pain during palpation and tapping of the spine, tension in the long back muscles;
- Changes in the patient’s posture (appearance of stoop, “petitioner’s posture”, increased lumbar lordosis);
- A decrease in the distance between the lower ribs and the iliac crest and the appearance of small skin folds on the sides of the abdomen.
The most obvious symptom of osteoporosis is bone fracture. In postmenopausal osteoporosis, spongy bone loss occurs predominantly. Fractures of the vertebral bodies are extremely common. Traumatologists make a diagnosis of a vertebral body fracture based on the appearance of acute pain in the corresponding part of the spine, which sharply intensifies with movements and tapping on the spine, and X-ray data of the spine in two projections.
In women over 45 years of age, radial fractures also occur in a typical location. In later stages of osteoporosis, femoral neck fractures occur. Multiple rib fractures often occur with osteoporosis, which has developed as a result of long-term use of glucocorticoids.
Patients with age-related osteoporosis experience loss of both cancellous and cortical bone mass. Cervical fractures associated with cortical osteoporosis and intertrochanteric fractures due to loss of cancellous substance occur. In this case, the diagnosis of osteoporosis is made during X-ray examinations.
Diagnosis of osteoporosis at home
It is impossible to make an accurate diagnosis without visiting a specialist and conducting tests . Therefore, you should not do it yourself and prescribe treatment measures for yourself .
The only thing you can do is to suspect warning signs and see a specialist. These are bone pain, increased general fatigue, the appearance of oral diseases, tachycardia, early gray hair, increased fragility of nails, back pain, decreased height, decreased mobility of the spine and other characteristic signs. If you notice them, get examined as soon as possible.
How to Diagnose Osteoporosis
The initial stage of diagnosing osteoporosis is identifying risk factors based on patient data. The likelihood of developing osteoporosis increases in patients with a low calcium content in the diet, vitamin D deficiency, or suffering from diseases of the gastrointestinal tract (due to decreased calcium absorption). The risk of developing osteoporosis increases if the following factors are present:
- Early menopause;
- Long-term use of thyroid hormones and glucocorticoids;
- Long periods of immobilization;
- Bad habits (alcohol abuse, smoking);
- Low body mass index;
- Insufficient physical activity.
Doctors at the Yusupov Hospital widely use x-ray methods in diagnosing osteoporosis. X-rays can detect the presence of abnormal bone density only when there is a loss of more than 30% of bone mass. Using this method, late signs of osteoporosis are more often detected - fractures of long bones or deformation of the vertebrae.
An informative method of examining for osteoporosis is densitometry - a measurement of bone tissue density based on the determination of calcium. For early diagnosis of osteoporosis, various bone densitometry methods are used. They make it possible to detect as little as 2–5% loss of bone mass, to assess the dynamics of bone tissue density during the development of the disease or the effectiveness of the therapy.
Doctors use isotope research methods (monophoton and two-photon absorptiometry), X-ray (monoenergy and dual-energy absorptiometry, quantitative computed tomography) and ultrasound. Dual-energy X-ray absorptiometry is the gold standard, allowing you to measure the content of bone mineral in any part of the skeleton, determine the content of calcium salts, muscle mass and adipose tissue throughout the body. Using densitometers, the lumbar vertebrae, bones of the forearm, proximal femur and the whole body are examined.
Diagnostic methods
If osteoporosis is suspected, an examination is prescribed to determine the mineral density (calcium saturation level) of the bones. This method is known as densitometry.
Bone density testing is performed using:
If necessary, a biochemical blood test and other examination methods are prescribed.
Ultrasound densitometry is considered the most common method for diagnosing pathology. Its essence boils down to the following: the speed of passage of the ultrasonic wave through the bone structure is determined. The denser the fabric, the higher this indicator.
Ultrasound densitometry is performed using highly sensitive equipment. The method allows you to determine with maximum accuracy the level of bone mass density in any part of the spine. Such an examination allows you to diagnose osteoporosis at the initial stage of development, when the deviation from the norm does not exceed 4%.
Ultrasound densitometry has the following advantages in comparison with other techniques:
- absolute harmlessness;
- high accuracy even at the initial stages of pathology development;
- the results of the examination become known after a few minutes;
- no contraindications to the procedure.
Ultrasound densitometry is allowed to be performed on pregnant and lactating women, children and the elderly.
X-ray
X-ray densitometry is also considered a highly informative and accurate method for diagnosing osteoporosis.
Its main disadvantage is that during the examination the tissues are exposed to harmful radiation. In this regard, the method has many contraindications. The essence of X-ray densitometry comes down to the same principle as ultrasound. Bone mineral density in this case is estimated based on the speed of passage of rays through the vertebral structures.
Biochemical analysis of blood and urine
With osteoporosis, the composition of blood and urine changes. Therefore, if a disease is suspected, the following are prescribed:
- Blood chemistry. Shows the concentration of hormones synthesized by the thyroid, reproductive and parathyroid glands.
- Biochemical urine analysis. Shows the concentration in the body of magnesium, calcium and phosphorus, elements responsible for building bones.
Biochemical analysis makes it possible to identify pathology in the early stages of development. This method is also used to monitor the effectiveness of the treatment.
Other methods
In some cases, densitometry is not able to identify places where thinning of the bone structure occurs. In such circumstances, scintigraphy is used, which involves the introduction of a contrast agent into the body. The latter “highlights” problem areas.
In addition to these methods, an MRI examination is used. It allows you to assess the nature of changes occurring in bone tissue and the functionality of the spine.
In rare cases, the doctor uses genetic testing. This method is used when cases of osteoporosis have been identified among the patient’s closest relatives.
Tests for osteoporosis in women and men
In order to assess bone tissue metabolism, rheumatologists at the Yusupov Hospital use laboratory diagnostic methods. The purpose of laboratory diagnostics is to exclude diseases, the manifestation of which may be osteopenia (osteomalacia, Paget's disease, bone metastases, myeloma), to establish the causes of secondary osteoporosis and the metabolic characteristics of the disease. The latter is important for making a diagnosis and choosing a method of adequate therapy, assessing its effectiveness.
What is the test for osteoporosis called? To assess the intensity of bone turnover, special biochemical markers are used, which are divided into 3 groups. Markers of bone tissue formation include osteocalcin, calcitonin and the bone enzyme alkaline phosphatase - ostase.
Osteocalcin is the major non-collagenous bone matrix protein produced by osteoblasts. The production of osteocalcin is dependent on vitamins K and D. This reduces to some extent the sensitivity and specificity of determining osteocalcin as a marker of bone turnover.
It is the concentration of calcitonin in the blood that reflects the metabolic activity of bone tissue osteoblasts, since this substance is the result of new synthesis, and not its release during bone destruction. In primary osteoporosis, normal or slightly elevated levels of osteocalcin are detected. Its increase in primary osteoporosis occurs in individuals with a high level of bone turnover. An increased level of decarboxylated osteocalcin may be a prognostic parameter for an increased risk of hip fractures in osteoporosis in elderly people.
Calcitonin production occurs in the parafollicular cells of the thyroid gland. Calcitonin has the following effects on bone tissue, calcium and phosphorus metabolism:
- Inhibits the activity of cells that destroy bone tissue;
- Stimulates the activity of osteoblasts, the production of bone matrix and the deposition of calcium in the bones;
- Reduces phosphate levels in the blood and stimulates the absorption of phosphorus by bones;
- Reduces calcium content in the blood, stimulates its entry into bone tissue;
- Increases excretion from the body in urine of calcium, phosphorus, water, magnesium, potassium, sodium, water;
- Stimulates the conversion of the inactive form of vitamin D3 in the kidneys into the biologically active form - calcitriol.
The bone enzyme alkaline phosphatase (ostase) is an indicator of bone health. His study is prescribed for diagnosing metabolic bone diseases and monitoring the effectiveness of treatment for osteoporosis. Ostase activity increases in bone pathology with increased osteoblast activity or bone tissue breakdown, hyperparathyroidism, rickets, osteosarcoma and cancer metastases in the bone, during healing of fractures.
A physiological increase in ostase activity is observed during periods of rapid growth, in women in the last trimester of pregnancy and after menopause. Ostase activity decreases in hypothyroidism, hereditary hypophosphatasemia, impaired bone growth, and lack of magnesium and zinc in food. A marker of bone matrix formation is determined to assess the effectiveness of anabolic and antiresorptive therapy for osteoporosis and other types of bone tissue pathology.
Research Features
Next, we will look in detail at how to determine osteoporosis using a blood test and what indicators should be there. Many people are trying to find out what this diagnostic method is called, but it has no name.
Total calcium indicator
Calcium is a component of bones - an important mineral component: 99% is contained in the skeleton in the form of hydroxyapatite crystals. The measure is determined by the colorimetric method. The concentration of the substance depends on age.
The microelement exists in three varieties:
- Ionized (50% of total mass).
- Protein bound (40%).
- Bound with phosphate or citrate ions (10%).
From a physiological point of view, an important role is played by the fraction of ionized material , the amount of which is consistently controlled by hormones that have a combined effect on the microelement. Such substances are calcitrol, parathyroid hormone and calcitonin .
In blood serum, the rate of ionized calcium ranges from 1.0 to 1.35 mmol/l .
Primary osteoporosis is characterized by a practically unchanged amount of calcium. The exception is hypercalcemia (excess) in disease caused by postmenopause or bone metastases. Increased levels are observed with increased levels of lithium, vitamin D or thiazide diuretics.
The osteopenic stage of pathology is characterized by a deficiency of the element due to malabsorption syndrome, rheumatoid process, impaired intestinal absorption, and long-term use of glucocorticoids.
If osteoporosis is characterized by rapid metabolism in the joints, then hypercalciuria (excess) occurs in the body. Among the causes of the phenomenon are menopause, rheumatism or glucocorticoids. To normalize the indicators, special medications are prescribed.
The normal calcium ratio is as follows (in mmol/l):
- Up to 10 days of life – 1.89–2.59.
- Up to 2 years - 2.26–2.74.
- Up to 12 years - 2.19–2.69.
- Under 18 years old - 2.11–2.54.
- Up to 60 years old - 2.16–2.57.
- From 60 years and older - 2.04–2.56.
Important! Before submitting the material for assessment, you must avoid heavy physical activity, alcohol, and refrain from eating.
Inorganic phosphorus
This mineral is a component of motor organs: it forms skeletal tissue and is involved in cellular energy metabolism. The volume is 600 g. Of these, 85% is distributed in the skeleton in the form of crystals, and 15% in the form of ions and esters.
The material has the following fractions :
- Ionized – 55%.
- With proteins – 10%.
- In the form of complexones (in conjunction with other ions) – 36%.
Primary osteoporosis is characterized by a normal or slightly reduced level of inorganic phosphorus . In diseases caused by glucocorticoids, there is an increased loss of the element, which is excreted in the urine. It is present in the body in the form of magnesium or calcium phosphates .
Normal values are (in mmol/l):
- Up to 10 days of life - 1.44–2.89.
- Up to 2 years - 1.44–2.17.
- Up to 12 years - 1.44–1.77.
- Up to 60 years old - 0.79–1.44.
- From 60 years of age in women - 0.91–1.33.
- From 60 years of age in men - 0.75–1.19.
Osteocalcin
Osteocalcin forms the skeletal structure along with hydroxyapatites and phosphates. This is a non-collagenous protein synthesized by osteoblasts - bone cells. It serves as one of the main markers of metabolism in joints .
The indicators of this protein in pathology are the most informative: they make it clear how active osteoblasts are. The marker reveals the rate of development of osteoporosis .
When diagnosing, it is worth paying attention to the condition of the kidneys , since protein is excreted by these organs. If the level is too high, the kidneys need to be examined due to possible disruption of their function, which develops due to prolonged bed rest.
Reference! For osteocalcin, the required capacity depends on gender and age.
The coefficient is as follows (measured in ng/ml):
- Up to 6 years: men – 39–121, women – 44–130.
- Under 15 years: 66–336 and 73–222.
- Under 50 years: 14–42 and 11–43.
- After 50 years: 14–46 and 15–46.
During the examination, the doctor must take into account the daily fluctuations of the element in the vessels. To obtain objective data, several samples should be taken at different times.
Parathyroid hormone
This is a hormone secreted by the parathyroid glands, regulating the phosphorus-calcium ratio in the circulatory system, designed to increase the concentration of calcium and reduce phosphorus , due to which trace elements are actively absorbed in the gastrointestinal tract.
When there is a deficiency of microelements, parathyroid hormone triggers mechanisms for their extraction from the joints. The maximum quantity occurs at 15–00, the minimum – at 7–00. This fluctuation is associated with the peculiarities of human physiology. Violation of hormone secretion affects the metabolism of the constituent materials of the musculoskeletal system. Calcium is lost through the kidneys in large quantities, washed out of the bones and less absorbed by the intestines.
Excess hormonal substances cause slower bone formation. Due to loss of strength, the risk of fracture increases. An increased amount of phosphorus contributes to the deposition of stones, poor circulation and vascular calcification.
The normal level of parathyroid hormone is determined by the following parameters (measurement in pg/ml):
- Up to 22 years: for men – 12–95, for women – 12–95.
- Up to 70 years: 9.5–75 and 9.5–75.
- From 71: 4.7–117 and 4.7–117.
Deoxypyridinoline (DPID)
This material forms collagen and shows its resorption. Detection requires immunochemiluminescent diagnosis. Information about this hormone is especially valuable at the early stage of the disease.
DPID is involved in the formation of articular fibers. Thanks to the substance, collagen molecules finally bond with each other. Due to pathology occurring in the bones, deoxypyridinoline is released and circulates through the circulatory system and is then excreted in the urine.
The normal amount of DPID is:
- 3.0–7.4 nmol/mmol – for women.
- 40–50 nmol/mmol – for children.
- 2.3–5.4 nmol/mmol – for men.
Test for osteoporosis
In the diagnosis of osteoporosis, metabolic markers are used:
- Parathyroid hormone;
- Calcium;
- Phosphorus;
- Vitamin D general.
Parathyroid hormone is involved in regulating the restoration of bone structure. This marker is examined if there is an increase in calcium levels or a decrease in phosphorus levels in the blood. In postmenopausal osteoporosis, parathyroid hormone levels are often normal or low, and in patients with steroid-induced or age-related osteoporosis, they are slightly elevated.
Indicators of calcium content in the blood in primary osteoporosis do not exceed the physiological norm. Hypercalcemia is determined in patients with senile osteoporosis with prolonged immobilization after a femoral neck fracture. Increased calcium levels in the blood are observed in primary osteoporosis, accompanied by increased bone turnover.
With primary osteoporosis, the level of phosphorus in the blood in most cases does not go beyond normal limits. It decreases in older people when osteoporosis is combined with osteomalacia (softening of the bones). To assess renal reabsorption of phosphorus, the concentration is determined in morning urine.
Total vitamin D is an indicator that reflects the status of vitamin D in the body. Vitamin D levels can vary depending on age (it decreases in older people), the type of food eaten, and the season (higher in late summer, lower in winter). A decrease in vitamin D levels in the blood is observed during pregnancy.
Rules for preparing for testing
The main goal of these tests is to obtain a true picture of a particular process occurring in the human body. To do this you need to prepare in a certain way.
Before donating blood:
- Blood is drawn for the laboratory on an empty stomach - no food is taken 12 hours before the procedure.
- The entire previous day abstain from fatty foods.
- Dinner is allowed, but light and early.
- Fasting for 2 days before the procedure is not allowed.
Before urine testing:
- You cannot drink more or less liquid than usual.
- It is prohibited to take antimicrobial drugs of any mode of action.
- You should abstain from sexual intercourse for at least 12 hours.
- You cannot donate urine during your period.
Osteoporosis can cause aggravation of back problems in the form of poor posture and osteochondrosis
The onset of osteoporosis in the first stages does not have clearly defined signs. When reaching the age of 30 years and above, representatives of both sexes should undergo periodic diagnostics . For women after 40 years and for men after 50 years, this procedure is mandatory once every 1-2 years. Also a reason to get tested are indirect signs of osteoporosis. Early detection of bone tissue demineralization will allow timely treatment measures to be taken and a complete recovery to be guaranteed.
Markers of bone resorption
To assess the effectiveness of osteoporosis treatment, resorption (reabsorption) markers are used. Their reduction under the influence of therapy begins after 2–3 weeks and reaches normal after 3–6 months. Beta-CrossLaps (C-terminal telopeptides) are formed during the degradation of type I collagen, which makes up more than 90% of the organic bone matrix. Its measurement makes it possible to assess the rate of degradation of relatively “old” bone tissue. With a pathological increase in reabsorption in osteoporosis and in old age, type 1 collagen degrades to a large extent. This leads to an increase in the level of its fragments in the blood.
Currently, there is evidence of the effect of gene polymorphism on bone mineral density. Allelic polymorphism of the bone remodeling gene network is being studied to identify osteoporosis susceptibility genotypes. Widely distributed enzymes are acid phosphatases. Their level is analyzed to determine the degree of bone reabsorption and monitor antiresorptive therapy.
To perform a modern and high-quality diagnosis of osteoporosis in the laboratory of the Yusupov Hospital, make an appointment with a rheumatologist by calling the contact center. After the initial examination, the doctor will prescribe those tests for osteoporosis and instrumental research methods that are most informative for establishing an accurate diagnosis for the patient. Examination for osteoporosis using densitometry allows us to detect a decrease in bone tissue mineralization at the preclinical stage of development of the pathological process.
Author
If test results are conflicting
What indicators are they guided by if the results of all studies are slightly below or above the upper limit of normal? In this case, the diagnosis is made based on the T-criterion.
Densitometric study of bone mass allows you to compare:
- Bone mineral density (abbreviated BMD) of a specific patient with the norm (with the same indicators in healthy people).
- By how many units (standard deviations) do these indicators differ from the norm (T-criterion).
For example, T = 3 means that the patient's bone mineral density is 3 units below normal (peak bone mass in a healthy person).
Comparison of bone density (BMD) of a patient with the norm:
| Norm | Osteopenia | Osteoporosis |
| T-criterion >-1 | from -1 to -2.5 | from <-2.5 |
Bone mineral density scale (abbreviated BMD)
Indications for detecting osteoporosis
Every person over 40 years of age, especially when it comes to women, should think about the need to diagnose osteoporosis. It should be regular and held every year.
Diagnosis of the disease is carried out when the T-index deviates from the norm:
- the result obtained is 0..-1 – the bone has normal density;
- indicator -1..-2.5 indicates bone loss;
- a value less than -2.5 indicates the appearance of osteoporosis.
Radiography
Radiography is one of the mandatory tests if osteoporosis is suspected. More often, the study is prescribed if the patient has a fracture or cracked bones.
In the early stages of the disease, X-ray diagnostics are not informative. However, after a loss of 20–30% of bone mass, it can detect changes in:
- thoracic and lumbar spine;
- pelvic bones;
- bones of the skull.
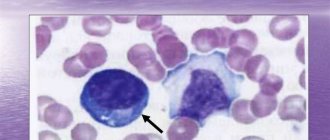
Sparse bone tissue appears on X-rays as light, almost transparent spots.
X-ray of bone tissue affected by osteoporosis