Spinal diseases are common, they cause painful symptoms and provoke dangerous complications, including disability. To avoid serious consequences, it is necessary to identify pathological changes in the spinal column in time. For this purpose, various instrumental studies are used, but one of the most informative is MRI of the spine.
Using magnetic resonance imaging, you can obtain very accurate information about the condition of the bone elements of the spine and the surrounding soft tissues. This is a safe and non-invasive diagnostic method that allows you to identify pathological changes in the early stages of the disease. But to get accurate results, you need to know how to prepare for the procedure and behave during it.
Table of contents
- Introduction
- Classification of tomographs
- Indications
- Contraindications
- Preparation
- How does the procedure work?
- Duration of the procedure
- What the results show
- Conclusion, transcript
- What's the difference with and without contrast?
- CT or MRI of the spine, which is better?
- X-ray or MRI of the spine, which is better?
- Ultrasound or MRI, which is better?
- To kid
- Photo
- Video
- Price
- Reviews
- Where to do
Introduction
The spine
is the main part of the human axial skeleton.
Consists of 33-34 vertebrae, sequentially connected to each other in a vertical position. MRI diagnostics of the spine
is a highly informative and safe study. The scan is carried out in the following areas: coccyx, sacrococcygeal region, sacrolumbar or lumbar region, thoracic region, cervical region. Based on the patient’s symptoms and complaints, the doctor can prescribe an MRI of a specific area, several or all departments at once, or a specific area. For example, magnetic resonance imaging of the atlanodental joint.
MRI of the spine allows you to visualize not only the bone structure, but also the adjacent soft tissues, feeding vessels, and cerebrospinal fluid. Scanning is carried out layer by layer. The layer parameters depend on the calibration of the device and can vary from 2 to 10 mm. The shallower the depth of the layer during the study, the greater the opportunity to determine degenerative disorders and pathologies at the stage of primary formation.
| Anatomical structure of the spine | MRI of the spine |
What parts of the spine are examined on MRI?
When examining the spine, MRI makes it possible to study the condition of not only all bone parts (from the cervical to the coccyx), but also other important structures:
- intervertebral discs;
- spinal cord and its membranes;
- vessels and nerves;
- ligaments;
- cartilage tissue;
- intervertebral joints;
- adjacent muscles and fiber.
The structure of the spine using the example of a separate segment
Magnetic resonance imaging accurately determines the localization of herniated protrusions of intervertebral discs, their size, the degree of degenerative changes, and impaired circulation of cerebrospinal fluid. With its help, adhesions in the epidural tissue are differentiated from inflammatory ones, as well as from tumor and vascular neoplasms.
All departments can be studied in detail during magnetic resonance scanning.
Classification of tomographs
To carry out an MRI scan, a special installation is used - a tomograph.
According to their design and technical characteristics, they are divided into the following types:
- closed
- closed with shortened tunnel
- open
- vertical.
The devices differ in the structure of the scanning capsules and the location of the magnets.
1. Closed MRI scanner
- a device with a long cylindrical tunnel, the walls of which limit the space. Magnets to create a working field are installed around the entire perimeter of the chamber.
Equipment advantages:
- The ability to create a magnetic field up to 3 Tesla (T).
- High resolution and detailed images.
- Detects disorders at an early stage and pathologies of the spine with an accuracy of up to 90%.
Weaknesses of a closed type installation:
- The narrow, dark space of the capsule causes psychological discomfort and negatively affects the condition of patients with claustrophobia.
- There are restrictions on the load-carrying capacity of the retractable table.
Closed tomograph
2. Closed tomograph with shortened tunnel
has a scanning capsule reduced to 60-90 cm.
Installation benefits:
- Creates a magnetic field voltage of 1.5 - 2 Tesla.
- Informative high-resolution images.
- Only the part being examined is placed in the scanning tunnel, not the entire body. Very convenient for patients with phobias and anxiety disorders.
- Determines pathologies and disorders with an accuracy of up to 90%.
Flaws:
Not suitable for a comprehensive examination of the spine from the cervical region to the coccyx.
| Closed tomograph with shortened tunnel |
3. Open tomograph
consists of a table where the patient is placed and an upper scanner. The review remains open.
Device capabilities:
- Comfortable examination of infants and active children.
- Large load capacity of the extendable table.
- Lack of anxiety in people with claustrophobia.
Disadvantages of the tomograph:
- Low magnetic field voltage limits the scanner's capabilities.
- Spinal pathologies in the early stages of formation remain unnoticed by the device.
Open tomograph
4. Vertical tomograph
allowed the use of a new algorithm for examining the spinal column. Due to insufficient information about the condition of the vertebrae, experts realized the need to scan the spine in a standing and sitting position. This allows you to make a diagnosis with extreme accuracy.
| Vertical tomograph |
Another parameter that you should pay attention to when choosing a clinic and equipment for examination is the magnetic field strength.
According to the operating voltage power, tomographs are divided into:
- Low-floor installations – up to 0.5 Tesla.
- Mid-field devices – up to 1 Tesla.
- High-field equipment – 1.5 Tesla.
- Ultra-high-field tomographs – from 3 Tesla.
For timely diagnosis of disorders and pathologies, it is enough to undergo a scan on a device with an operating magnetic field voltage of 1.5 Tesla.
| Tomograph power and image resolution |
MRI of the spine - indications and cost
What is MRI? – Magnetic resonance imaging – is a type of diagnostic study that reproduces maximum details about the state of a person’s internal organs. The procedure occurs without internal intervention based on magnetic fields. Such research is completely safe from ionizing radiation.
During the diagnostic process, the MRI machine creates a series of images , based on which the doctor performs an analysis and makes a diagnosis. High diagnostic technologies make it possible to detect the presence of various diseases at an early stage and begin their treatment in time.
Indications
The following specialists can refer you for an MRI of the spine: a neurologist, a traumatologist, a vertebrologist, a surgeon, and in some cases a cardiologist, since pinched nerve endings of the spinal column can provoke tachycardia and pain in the heart area.
Indications for prescribing a magnetic resonance examination are the following symptoms and conditions:
- Intrauterine malformations of the bone structure of the spinal column.
- Old and recent spinal injuries.
- The patient has a history of vegetative-vascular dystonia.
- Age-related changes (violation of the integrity of cartilage tissue, wear of the vertebrae).
- Headache
- Pain syndrome in the neck area.
- Pain in the back and lower back.
- Gait disturbance.
- Suspicion of infectious and inflammatory diseases (arthrosis, rheumatoid arthritis, lumbago, radiculitis).
- Suspicion of neoplasms in the spine or spinal cord.
MRI of the spinal column is also prescribed to monitor the situation in the following cases:
- Assessing the effectiveness of therapeutic treatment.
- Confirmation of the feasibility of surgical intervention.
- Postoperative control.
- Monitoring of oncological pathology in the spine.
MRI diagnostics of the spine: indications and contraindications
Magnetic resonance imaging is used in the diagnosis of almost all spinal pathologies. Researched:
- injuries;
- developmental anomalies;
- inflammatory diseases (spondylitis, osteomyelitis, discitis);
- degenerative processes (osteochondrosis, spondyloarthrosis, protrusion of intervertebral discs);
- malignant neoplasms and metastases.
Spinal tumor on MRI (indicated by arrows)
Osteochondrosis
This is a degenerative-dystrophic chronic disease that begins with the nucleus pulposus of the intervertebral disc and spreads further to all elements of the vertebral motor segment.
It makes sense to do an MRI for any persistent back pain, since making an accurate diagnosis during an initial examination by a neurologist based only on clinical signs is not an easy task. Difficulties may be due to the fact that;
- there are individual differences in the structure of the spine, the level of nerve exit from the spinal cord and the innervation of the lower extremities;
- There are a number of diseases that cause similar symptoms: pathologies of the hip joints, ischemic neuritis of the lower extremities, vascular diseases, abdominal and pelvic organs.
Therefore, a neurological examination can only suggest the localization of the process. To make a final diagnosis, it is necessary to visualize the process on MRI, which will allow you to immediately choose the right treatment tactics.
Spondylitis
An inflammatory disease in which early diagnosis and adequate treatment tactics make it possible to avoid severe disabling consequences.
Most often it is the result of the introduction of microorganisms with the bloodstream into the adjacent space of the spinal disc (there are no vessels in the disc itself). This disease is quite rare and is often mistaken for degenerative, leading to inappropriate treatment. X-rays and CT scans do not detect spondylitis at an early stage. Therefore, in case of persistent back pain that is not amenable to conservative treatment, increased inflammatory markers in the blood or fever, it is necessary to do an MRI of the spine. If the diagnosis of spondylitis is delayed, spinal cord damage and sepsis may develop.
The key signs of spondylitis on MRI are:
- inability to visualize the boundaries of the intervertebral disc and the adjacent vertebral body;
- increased signal intensity from the disc itself and the vertebral body.
MRI with intravenous contrast, in this case, reveals the spread of the inflammatory process and the formation of an epidural abscess. Standard MRI without contrast makes it possible to distinguish spondylitis from degenerative and tumor processes.
Dynamic studies (repeated) are prescribed for patients with a confirmed diagnosis of spondylitis and who have little improvement after conservative treatment. This is due to the fact that changes in inflammatory markers in the blood are not always indicative of assessing the effectiveness of treatment. Repeated MRIs may reveal abscess formation that requires surgical drainage.
Spinal injuries
According to the state of neurovascular formations, they can be:
- uncomplicated (without damage to the spinal cord and spinal nerves);
- complicated (with their damage).
Spinal cord injury occurs:
- acute - directly at the time of injury by foreign bodies or bone fragments;
- early - in the next 10 days, as a result of compression by hematoma, edema, secondary displacement of the vertebrae;
- later - after several weeks, and sometimes even years, due to the scar-adhesive process or the formation of cysts.
MRI makes it possible to establish a diagnosis in 98% of cases, as it visualizes:
- ligaments;
- intervertebral discs;
- membranes of the spinal cord;
- spinal cord and its pathologies (hemorrhages, swelling, ischemia);
- violation of the structure of the vertebral bodies.
MRI of the lumbosacral spine shows a herniated disc at the level of the 5th lumbar and 1st sacral vertebrae, which puts pressure on the spinal cord and nerve roots.
MRI is the main method for diagnosing post-traumatic disc herniations.
In a certain group of patients with spinal trauma in the acute period, there are no signs of vertebral damage on the radiograph. But after 3-8 months. sudden sharp pain occurs at the site of the previous injury. Repeated examination reveals a compression fracture of the spine.
This is explained by the fact that in the acute period hemorrhage occurred in the vertebral body. After its resorption, aseptic inflammation and destruction of bone structures developed. The action of axial load on the weakened vertebral body led to its compression fracture.
MRI allows you to visualize these hemorrhages in the acute period and take timely measures, which significantly affects the patient’s future health.
Metastatic lesions of the spine
The appearance of pain in the spine, an increase in existing pain in the spine and lower extremities in patients with cancer should be the reason for urgent MRI of the entire spinal column with intravenous contrast.
However, the scope of primary diagnostic measures depends on the severity of the patient’s problems at the time of examination. Asymptomatic lesions in the spine of a metastatic nature, identified on CT or scintigraphy, should be confirmed by MRI with contrast.
The appearance of threatening symptoms in the form of weakness in the limbs, dysfunction of the pelvic organs or sensitivity is the reason for performing an emergency MRI of the entire spine with contrast, even if the patient has a history of degenerative disease of the spine.
Magnetic resonance imaging is contraindicated in patients:
- having implants or foreign bodies made of ferromagnets in the body;
- wearing non-removable electronic devices (pacemakers, cochlear implants, insulin pumps and others);
- with vascular clips installed on the arteries of the brain;
- pregnant women in the first trimester;
- if it is impossible to remain still due to claustrophobia, pain or other reasons.
Our clinic does not examine children under 5 years of age or adults with a body weight of more than 130 kg or a waist circumference of more than 150 cm.
Contraindications
Contraindications for magnetic resonance imaging of the spine are the same as for MRI of any other area. Factors limiting or prohibiting the use of this diagnostic method are divided into absolute contraindications, when scanning in a magnetic resonance imaging scanner can cause irreparable damage to the body, and relative contraindications, when a change in the conditions of the procedure makes it possible.
Absolute:
- The presence of a built-in pacemaker or pacemaker.
- Implantation of a defibrillator.
- Prosthetic heart valve made of ferromagnetic materials.
- Installation of a hearing implant in the middle or inner ear.
- Ilizarov apparatus.
- Built-in hormonal or insulin pump.
- Endoprostheses made of metals that respond to increased magnetic field voltage.
- Hemostatic clips.
- Standing or bypass surgery.
- Acute\chronic heart failure.
Relative:
- Claustrophobia and other anxiety disorders.
- Neurological pathologies accompanied by tremors and involuntary body movements.
- Early pregnancy.
- Obesity and dimensions exceeding the load capacity of the retractable table and the diameter of the tomograph tunnel.
- Alcohol intoxication.
- Confusion.
- Open bleeding.
How does the procedure work?
MRI examination of the spine is conventionally divided into several stages: organization, preparation, examination, and presentation of results.
- The organizational stage
involves the patient’s early arrival at the diagnostic center, checking documents confirming the discount, benefits or free MRI, and a referral from a doctor. Self-referral examinations or spinal diagnostics in a commercial clinic are carried out for a fee. To do this, you need to sign an agreement with the medical institution and make a payment. Also, in the case of MRI on your own initiative, it is necessary to set a clear task for the radiologist. The patient is given a questionnaire to fill out so that the medical staff has an idea of possible contraindications and restrictions. - Preparing
the patient for the procedure includes changing into his own comfortable clothes without metal fasteners or buckles or a disposable hospital gown. Jewelry must be removed. The nurse or radiologist explains the rules of conduct during the examination and the features of the procedure. - Magnetic resonance imaging of the spine
requires that you remain still. To do this, the nurse helps the patient position himself on a retractable table and secures the body with soft clamps. The bed is moved into the scanning capsule of a closed tomograph or under an open scanner. The study starts. When performing an MRI with contrast, a baseline scan is performed first, after which contrast is injected and the procedure begins again. The doctor monitors the patient’s condition for some time after the scan, since the administration of contrast can cause an allergic reaction or an attack of nausea and lead to excessive stress on the kidneys. - Results
are delivered within an hour, unless the radiologist's schedule is overloaded. During this time, the specialist deciphers and describes the images and fills out a protocol. The patient receives a finished image and/or a series of images recorded on disk. Some medical institutions provide the media, while others require you to bring the disk with you. The administrator must notify you of this on the day of registration for the examination. If the radiologist is under heavy workload, the results can be delivered to the patient the next day or by email.
Duration of the procedure
The duration of an MRI scan of one part of the spine on a high-field tomograph takes 20 minutes.
An MRI of the entire spinal column includes 4 sections, so diagnosis can take 80 minutes.
Contrast-enhanced MR imaging doubles the procedure time because a baseline scan is performed first, then contrast is injected and the examination starts all over again.
A software failure or stop at the request of the patient due to poor health or a panic attack can increase the examination time.
Diagnostic technique
The tomograph capsule consists of a long cylinder and a magnet located around a cylindrical tube. Tomographs have great capabilities: thanks to the scanners, clear images of various parts of the body are obtained. An MRI of the spine is performed for 30-60 minutes: the more spinal areas are examined, the longer the scanning lasts. The patient lies down on a rolling table. It is not necessary to take off your clothes; it is important to dress simply, with a minimum number of fasteners. The arms, legs and head are secured with special straps that do not allow the patient to move so that the course of the examination is not disrupted.
Contrast agents, when necessary, are administered before scanning, used in cases of suspected malignancy, the presence of metastases, chronic autoimmune disease of the myelin sheath of nerve fibers of the brain or spinal cord, and during examination after excision of an intervertebral hernia. The procedure with contrast visualizes the pathology better, marks the affected areas, and tumor parameters.
During the scan, the doctor leaves the office. Communication with the doctor is maintained using a microphone in the capsule or a special button. There is no discomfort during scanning; it is important to lie on the table without moving. The capsule is equipped with a fresh air supply. The procedure takes place, accompanied by loud sounds and the crackling sound of the apparatus. The patient is offered headphones and earplugs to minimize discomfort.
The data is sent to the computer. At the end of the process, the doctor sees the images, deciphers them and makes a conclusion. After diagnosis, the patient receives a detailed description of his health condition. An MRI scan does not harm a person.
What the results show
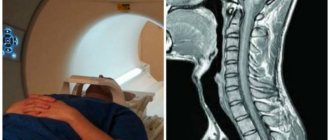
An MRI image allows you to visualize the spine in 3 planes:
- Axial projection – transverse section of the vertebra.
- Coronal projection or frontal plane of the spinal column.
- Sagittal projection – visualization of the spine from the side.
Depending on the pathology that needs to be confirmed, the leading projection is selected, and the other two serve as clarifying ones. Thanks to this, the doctor sees the location, size and shape of the destructive structure.
| MRI image of the spine in two projections: axial and sagittal. The direct coronal view is simply not shown in the picture. |
MRI allows you to identify the following disorders and pathologies with up to 95% accuracy:
- Congenital anomalies and disorders in the development of the spinal column.
- Age-related or professional degenerative changes - osteochondrosis, scoliosis, kyphosis.
- Spinal injuries - bruises, fractures, cracks.
- Autoimmune diseases – rheumatoid arthritis, spondylitis, spondyloarthrosis.
- Osteoporosis.
- Intervertebral hernia.
- Spinal stenosis.
- Poor blood supply to the spinal cord.
- Compression of the spinal nerve roots.
- Inflammatory process or infectious lesion of the spinal cord - myelitis, arachnoiditis.
- The presence of benign or malignant neoplasms of the spine or spinal cord (hemangiolipoma, sarcoma, cancer).
In the absence of spinal diseases, an MRI image will provide the following indicators:
- No signs of intrauterine pathology or developmental defects were identified.
- The joints and intervertebral discs are located in their anatomical bed and maintain their integrity.
- The blood supply to the spinal cord occurs without disruption.
Advantages of MRI diagnostics
The main advantages of such diagnostics are:
- Accurate analysis of the anatomical state of the spine in general and in detail;
- Allows you to identify emerging pathologies;
- Allows you to effectively diagnose the condition of intervertebral discs;
- Allows you to identify disease of the facet joints - arthrosis;
- Allows you to assess the condition of nerve endings and the spinal cord in specific parts of the spine;
- Allows you to detect the presence of various neoplasms, including tumors;
- Allows you to accurately identify injured areas;
- Allows you to check for changes after surgery;
- Allows you to determine the presence of inflammatory processes;
- Allows you to determine the presence of pathologies in the membrane of the spinal cord and adjacent vessels;
- Diagnosis performed by MRI does not have the harmful effects associated with ionizing radiation;
- Only with the help of an MRI machine can high-quality images be obtained;
- There are no analogues of equipment for such high-precision determination of certain spinal diseases;
- MRI, unlike other diagnostic methods, is capable of visualizing nerve endings;
- The contrast agent used in diagnostics does not contain iodine, therefore it practically does not cause allergies;
- Allows you to make the most complete diagnosis of the spine, on the basis of which it is easiest to identify the disease;
- If the operating instructions are followed, MRI is completely safe for humans.
MRI allows you to timely identify not only diseases, but also related problems, such as:
- Osteochondrosis;
- Intervertebral hernia;
- Disc protrusion;
- Scoliosis;
- Kyphosis;
- Spondylolastylosis;
- Spinal subluxations;
- Vascular pathologists;
- Tumors;
- Injuries;
- Infections;
- Demyelinating diseases.
Modern MRI machines allow you to:
- Virtual endoscopy – three-dimensional image of the examined area;
- MRI diffusion – monitors the movement of fluid within the body’s cells;
- Diffusion-weighted tomography – used for cancer, allows you to determine the movement of radiolabeled protons;
- MR perfusion – used for strokes, circulatory problems, coronary heart diseases;
- MR - spectroscopy - determines the biochemical change in the composition of liquids and tissues;
- MR angiography - helps to view the vessels in the section.
Read about degenerative-dystrophic changes in the lumbosacral region and their treatment here.
What's the difference with and without contrast?
Drugs for creating a contrast medium can improve the efficiency of MRI of the spine. In modern medicine, gadolinium derivatives are used for this purpose. The substance increases the contrast of body tissues and allows different types of cells to be differentiated.
The contrast is transported by the bloodstream. In the zone of destructive changes, the substance accumulates due to disturbances in blood circulation and highlights the pathology. Due to this, inflammatory processes, tumors, swelling, and tissue destruction are released.
Side effects from the use of a contrast solution are:
- Chills
- Burning sensation in blood vessels
- Fever
- Nausea
- Mild headache or dizziness.
Symptoms appear for a short period of time and disappear on their own.
To minimize side effects, the doctor must accurately calculate the dosage of the drug. The starting point is the patient’s weight, the presence of chronic diseases, and age.
Limitations and contraindications for the use of contrast enhancement MRI of the spine are determined at the stage of preparation for scanning.
Contraindications for the use of gadolinium:
- Dysfunction of the excretory organs. In case of renal failure, the contrast medium can provoke the development of nephrofibrosis.
- Hypersensitivity to gadolinium.
- Allergy to contrast solution.
- Early pregnancy, as the drug can affect the formation of fetal organs.
- Lactation. Gadolinium can enter the child's body through mother's milk in quantities exceeding the permissible dose. If this diagnostic method is the only solution to the problem, then you should express milk for 3 days and feed the baby formula.
- The cost of MRI with contrast increases. The cost of the drug is added to the cost of the procedure.
Here is an example of a photo with contrast - on the right and without - on the left:
| MRI of the thoracic spine showed an extradural lesion extending from T3 to T11 (left), which was enhanced by contrast injection (right). |
CT or MRI of the spine, which is better?
Computed tomography of the spinal column and MRI of this area are based on fundamentally different technologies and have their own strengths and weaknesses. To correctly compare methods and select the most suitable examination option, it is necessary to evaluate several indicators at once.
1. Equipment capabilities.
CT allows you to create the most complete clinical picture of the bone tissue of the spine. It is appropriate to use for injuries, fractures, and infectious bone lesions. If the doctor orders an examination to confirm or refute the presence of a tumor, or to examine the cerebrospinal fluid, then the preference goes to MRI. Magnetic resonance scanning visualizes the structure of soft tissues in as much detail as possible.
2. Technology of influence on the body.
A CT scanner uses X-rays to scan. MRI diagnostics is based on the magnetic resonance effect.
3. Safety.
If the rules of the procedure are followed, MRI is a safe examination method and has no restrictions on the number of scanning processes. X-ray radiation in large doses has an adverse effect on the body, so CT is recommended to be performed no more than once a year. The exception is emergency situations that pose a much greater threat to health.
4. Scan duration.
An MRI of one part of the spine on a high-field tomograph takes 20 minutes. Computed tomography takes no more than 1-2 minutes.
| CT scan of the spine | MRI of the spine |
CT also allows you to take 3D images:
| 3D CT image of the spine |
What parts of the spine are examined on MRI?
Normal anatomy: parts of the spine
The spine is a framework (support) for muscles and tissues; the following sections are distinguished in it:
The pathological process can be localized in any part of the spinal column and manifest itself in a wide variety of complaints.
MRI of all parts of the spine examines:
- osteoarticular structures;
- paravertebral tissues;
- intervertebral discs;
- spinal cord and its membranes;
- ligamentous apparatus;
- vessels;
- spinal nerves.
X-ray or MRI of the spine, which is better?
12.
X-ray and MRI of the spine are based on different technologies. It is incorrect to compare them with each other on a qualitative basis, since each method has its own strengths and personal disadvantages. For an objective assessment, it is necessary to analyze several factors.
1. Device capabilities
. An X-ray image can show in detail the bone structure of the spinal column. For fractures, displacements, and scoliosis, this examination method is sufficient to make an accurate diagnosis and select a treatment regimen. MR imaging visualizes soft tissue structures along with bone tissue. This makes it possible to determine conduction disturbances in blood vessels and the spinal canal, pathology of the spinal cord, and adjacent muscles.
2. Research technology
. Radiography is based on the use of x-rays. Layer-by-layer magnetic resonance scanning is carried out thanks to vibrations of hydrogen atoms.
3. Restrictions.
Frequent exposure of the body to x-rays negatively affects its condition. X-rays are recommended to be limited to one procedure per year. MRI is a safe procedure and can be performed every day.
4. Availability
. X-rays can be taken at a local clinic or emergency room. MRI scanners are a privilege of inpatient departments, regional medical institutions, and commercial clinics.
5. Price.
X-rays are included in the list of services provided under the general health insurance program, so they are carried out free of charge. Only severely ill patients in inpatient departments can undergo MRI without payment. In other cases, the procedure will be paid. When conducting an examination in a commercial medical institution, the price list for an x-ray will be several times lower than the cost of an MRI.
| MRI of the spine | X-ray of the spine |
Normal MRI indicators of all parts of the spine
MRI of the spine: normal and pathological
The diagnostician draws attention to the average population statistical parameters that are accepted as the norm: the absence of pathological curvatures of the spinal column, spinal cord compression, focal formations, edema, hernial protrusions, metastatic lesions, preservation of bone structures, etc. All changes will be reflected in detail in the protocol research. The final diagnosis is made by the attending physician. In doubtful cases, MRI results are assessed collectively. You can get a “second opinion” if you send the images for consultation to a specialized medical center. This service is currently provided by many large Russian and foreign clinics.
source
Ultrasound or MRI, which is better?
Ultrasound examination of the spine and magnetic resonance scanning of the spinal column are based on different technologies for influencing body tissue. Both methods allow you to collect a complete clinical picture, it’s just that each of them has its own advantages and weaknesses. To make an objective comparison, it is necessary to analyze the following aspects:
1. Operating principle of the equipment.
The ultrasound machine processes the ultrasound signal reflected from the spine and creates an image on the monitor. To visualize the internal structures of the spinal column, the MR system uses vibrations of hydrogen atoms caused by an increase in the magnetic field strength in the scanner.
2. Harmfulness.
Both diagnostic methods are safe and painless, however, MRI is contraindicated for people with ferromagnetic devices in the body: pacemaker, Ilizarov apparatus, hemostatic clips. Magnetic resonance imaging is complicated by the presence of anxiety-phobic disorders. Ultrasound does not have limitations associated with the presence of metal implants and life-supporting devices.
3. Image quality and information content.
Ultrasound images have low resolution, are replete with artifacts and noise, and therefore may miss degenerative disorders at the initial stage of formation. MRI projections performed on a tomograph with a magnetic field strength of 1.5 Tesla have high resolution, detail, and are capable of displaying organic and functional pathologies.
4. Availability.
You can undergo an ultrasound scan within the walls of your own clinic. For MRI of the spine, the doctor issues a referral to a municipal medical institution of regional significance or gives the right to choose a commercial clinic. MRI scanning is also carried out in inpatient departments, but in this case, valuable time may be lost.
5. Price.
An ultrasound of the spinal column can be performed free of charge, since the procedure is included in the basic list of services under the compulsory medical insurance program. MRI was included in the expanded list of examinations under the general health insurance program provided in inpatient departments. There is a fee for carrying out a magnetic resonance examination outside a hospital. If we compare the prices for ultrasound and MRI of the spine, the cost of the second diagnostic method will be 2-3 times higher.
6. Duration of the examination.
An ultrasound scan should take 5-10 minutes, depending on the size of the area being examined. MRI of the spinal column takes from 20 minutes to 2 hours.
| MRI of the spine | Ultrasound of the spine |
Carrying out
To prevent the patient from using his imagination, the attending physician or diagnostician must explain how an MRI of the spine is done and how long the procedure lasts. The patient will not have to experience anything terrible during this diagnostic method. Arriving at the office where the examination will take place, he will face the following. After removing all unnecessary items and changing into hospital clothes, the patient must lie down on a special movable table.
It will be fixed on it with belts and, depending on which sections will be examined, cushions will be placed in the necessary places. Before turning on the tomograph, medical personnel go to an adjacent room. The table slides into a massive cylindrical pipe. The tomography device makes loud noises during the scanning process. You can communicate with medical staff using a special microphone.
The duration of the examination, depending on the indications and diagnostic tasks, can take from 5 to 30 minutes (up to 90 with contrast). At the end of the study, the doctor must make a transcript of the results and give it to the patient on the same day. Before performing an MRI with contrast, a complete MRI examination of the problem area without contrast is performed. After this, a contrast agent is administered and a scan is performed in three areas.
If the patient is not allergic and is not registered with a nephrologist, then the procedure turns out to be completely safe and does not cause negative consequences.
To kid
MRI of the spine has no age limit. The procedure can be performed even on infants. Since it is necessary to remain still during scanning, children under 7 years of age are examined under general anesthesia. Medical institutions that do not have a license to carry out diagnostics with the administration of anesthesia set restrictions and conduct MRI for children from 7 years of age.
A child may be frightened by the narrow tunnel of a closed tomograph or the noise inside the capsule. Excitation of the body caused by a feeling of fear is reflected in the diagnostic results. Sensitive and impressionable children are recommended to be examined using an open tomograph.
Indications and contraindications for MRI of the spine
Only a specialist can prescribe diagnostics using MRI! Any study has its own indications and contraindications. Let's look at them below.
To provide diagnostic tests using MRI:
- Presence of symptoms of neurological diseases;
- The formation of pathologies in the spinal cord, detected during an X-ray examination;
- The formation of pathologies in the spine and its canal, detected during an x-ray examination;
- The formation of pathologies in the intervertebral discs, discovered during an X-ray examination;
- Spinal injuries;
- Detected oncology;
- Suspicion of abnormal neoplasms of the cranio-vertebral junction;
- Monitoring the dynamics of the disease and treatment of the spinal cord and spine;
- Various lung diseases (oncology, mediastinum, metastases, etc.);
- Determination of the nature and extent of lung injury;
- Determination of the presence of foreign bodies in the body;
Contraindications to diagnostics using MRI:
- The presence of metallic additives in the body (the magnetic field of the device can damage them - you must first consult a doctor);
- Breastfeeding women (after diagnosis using MRI, breastfeeding is prohibited for 48 hours);
- Possible allergic reactions to the components of the contrast agent (easily relieved with medication);
- Patient has claustrophobia;
- Nervous instability;
- The patient’s perseverance is low (he cannot sit in one place for more than 15 minutes), including children under 7 years of age;
- Weight more than 120 kg (some devices can support a patient’s weight up to 180 kg);
- Acute injuries;
- Pregnancy (the exact effect of MRI on this category of patients is still unknown to science, so refrain from such examination during this period); Originally Answered: What should I do about lower back pain in early pregnancy? – we wrote here.
- Pacemakers;
- Kidney failure;
- Implants in the ear.
Photo
Here are some MRI photos of the spine:
| Intervertebral hernia |
| The blue arrow is a broken vertebra during an accident, the orange arrow is a cyst. Source. |
| Scoliosis |
| Vertebral displacement |
| Tumor |