Spermogram: how does the procedure take place? Do you need to prepare for it?
Preparation necessarily involves sexual abstinence for 3 days. During this time, you should avoid drinking alcohol, as well as various thermal procedures: saunas and steam baths, hot baths, and heated car seats. It is advisable to stop taking any medications other than essential ones.
Otherwise, a man needs to lead a normal lifestyle.
Important! If antibiotics have been prescribed, at least 21 days must pass after finishing taking them. Biological material is obtained through masturbation, since this method is as physiological as possible.
Ejaculate color
This indicator can also speak volumes. Normal sperm is white, yellowish or grayish in color. A brown or pinkish tint is a sign of the presence of erythrocytes (red blood cells) in it. This factor can manifest itself as a result of injury to the testicles or prostate gland, or in the presence of tumors. Fragmentation of the spermogram and decoding will help you find out whether there are pathologies or not.
Sperm count
The number of sperm, as well as the volume of ejaculate, plays a crucial role in the study of the spermogram; if you look at the result of the analysis of the spermogram, the transcript will accurately show the number of sperm. It is this factor that determines the ability of the male body to conceive a child. The norm is considered to be a concentration of at least 20 million germ cells in 1 ml of ejaculate. A low number of sperm produced may indicate a deterioration in the efficiency and quality of the testicles, which usually occurs due to the following factors:
- inflammation in the testicles;
- decrease in the concentration of sex hormones in the blood of men;
- metabolic disorder.
Sperm activity
Only sperm that move actively and in a straight line can fertilize an egg, which is why it is very often necessary to decipher a DNA spermogram, the decoding of which will show the activity of the sperm. This happens due to the wave-like movements of the tail of the reproductive cell. In general, the number of active sperm in the ejaculate of a healthy man ranges from 60-70% of the total number of germ cells (10-15% are weakly motile, and 20-25% are completely immobile).
There are several groups that divide sperm according to the type of their motor activity.
- Group A. This group includes the fastest and most linearly moving germ cells, their speed is at least 0.025 mm/s. Normal semen contains at least 50% sperm belonging to group A.
- Group B. Sperm belonging to this group move more slowly than the previous ones, but at the same time maintain straightness of movement. Their number, as a rule, is 10-20% of the total number of germ cells.
- Group C. Group C sperm are cells that are characterized by slow movement and not in a straight line. Normal sperm contains no more than 20% of these spermatozoa.
- Group D. This group includes absolutely immobile sperm, the number of which does not exceed 10-20% in a healthy man.
Deciphering the spermogram, pathological forms can show the speed of sperm movement. Low speed of sperm movement and a large number of immobile cells are signs of asthenospermia (asthenozoospermia). This phenomenon can occur due to a disease such as varicocele, as well as inflammation of the testicles, exposure to toxic substances and radiation. Asthenospermia is one of the main causes of infertility among men. In any case, deciphering the spermogram analysis online for free will show whether this problem exists or not.
Expert opinion An excessive number of germ cells (over 120 ml) indicates their low ability to fertilize. This condition indicates the presence of inflammatory processes and endocrine disorders.
Khrabrov Timur Yurievich Urologist-andrologist Experience 15 years
Ask a clarifying question
Spermogram interpretation: normal
The standard indicators that specialists rely on when deciphering spermogram analysis were determined by WHO (World Health Organization) in 2010.
They include macro- and microscopic assessment of the ejaculate.
Macroscopic indicators include:
- Volume of semen obtained: more than 1.5 ml
- Liquefaction duration: maximum 60 minutes
- Viscosity: no more than 2 cm
- Color: white-grayish
- pH value: more than 7.2
- Smell: specific
Microscopic indicators include:
- Sperm concentration: not less than 15 million/ml
- Total sperm count: at least 39 million
- Viability: no less than 58%
- Total mobility (PR+NP): no less than 40%
- Progressively mobile (PR): no less than 32%
- Morphologically normal sperm: not less than 4%
- Leukocyte concentration: less than 1 million/ml
Our laboratory uses automated assessment of ejaculate quality. The SCA Microptic analyzer takes into account each cell, speed and trajectory of each sperm when assessing concentration and motility, and then calculates average values for different categories. When assessing morphology, the computer measures the dimensions of the head, neck and tail in micrometers, calculates the area of the head, and analyzes its shape according to international standards. Automatic analysis of sperm characteristics avoids the subjectivity of assessment due to human factors.
Where to get an extended spermogram and how much does it cost?
A detailed spermogram can be taken in commercial laboratories and medical centers. Examples of institutions and prices are shown in the table below:
| Name | Type of analysis | price, rub. | |
| "Sperm test", Moscow | Preliminary evaluation of ejaculate | 1500 | |
| Spermogram with Kruger assessment | 2500 | ||
| MAR test | Direct – 1290, indirect (by blood) – 3690 | ||
| Fragmentation index | 7000 | ||
| EMIS | 9000 | ||
| ROS test | In regular sperm – 2000, in washed sperm – 4000 | ||
| Biochemical analysis | Fructose | 750 | |
| Zinc | 750 | ||
| Lemon acid | 750 | ||
| Alpha glycosidase | 1500 | ||
| Protamine-histone | 4000 | ||
| NVA test | 5000 | ||
| Med, St. Petersburg | Analysis of ejaculate with assessment of cell structure according to Kruger | 3000 | |
| Preliminary sperm analysis (without morphology) | 1500 | ||
| "Citylab", Ekaterinburg | Level 2 spermogram. Includes general analysis, Kruger morphology, total antisperm antibodies. | 1580 | |
Decoding the spermogram
The results in our clinic are assessed exclusively by experienced specialists.
The main terms describing the qualitative and quantitative parameters of the ejaculate are:
- Normozoospermia.
Concentration, motility and percentage of morphologically normal sperm correspond to standard values - Aspermia.
Lack of ejaculate (or retrograde ejaculation) - Asthenozoospermia.
The percentage of progressively motile sperm is below the standard value - Oligozoospermia.
Reduced concentration or total number of sperm in the ejaculate - Cryptozoospermia.
Spermatozoa are absent in the native ejaculate, but are found in the sediment after its concentration by centrifugation - Azoospermia.
There are no sperm in the ejaculate - Teratozoospermia.
The proportion of morphologically normal sperm in the ejaculate is reduced
Important! You should not try to decipher the spermogram and make a diagnosis yourself! This is due to the fact that only specialists have all the necessary knowledge and skills to correctly evaluate the obtained biological material. In addition, professionals focus on a combination of indicators from various surveys. This improves the accuracy of the diagnosis.
If the spermogram is bad, the analysis is repeated. Usually the procedure is carried out no less than 21 days after the last spermogram. If the doctor has doubts, the test can be repeated one more time. The best result is accepted as a reliable result.
Important! There is not a single diagnostic indicator that would allow us to draw 100% conclusions about absolute infertility or perfect health of a man. Therefore, other additional examinations are often carried out.
What might be written in the transcript?
Before deciphering the spermogram analyzes yourself, you should understand some possible expert opinions located at the end of the provided conclusion.
It is the word that ends in “spermia” that will indicate what the normal spermogram indicators are and whether they should be adjusted or should be left at the same level.
If you try to decipher the analysis yourself, you can get the following data:
- azoospermia - the number of living sperm is zero, which indicates zero ability to conceive;
- akinozoospermia - similar to the first option, since there are no living sperm in the ejaculate;
- the presence of antisperm-type antibodies - indicates that the liquid contains antibodies produced by the immune system against sperm, which excludes pregnancy;
- asthenozoospermia - a condition of sperm when there are few motile sperm in it, that is, less than twenty-five percent of the total;
- hemospermia - the presence in semen, in addition to sperm, of a small number of red blood cells;
- leukocytospermia - a large number of leukocytes are present;
- necrozoospermia - determines that there are no living sperm in the semen, and the ability to conceive a baby is zero.
Don’t think that everything is so bad, since at the end of the analysis there may be one of the above words:
- normozoospermia – suitable for producing offspring, but only with minor adjustments;
- normospermia is a normal spermogram, which shows that the seminal fluid is good for conceiving babies.
If the spermogram indicator is normally defined as 20,000,000 active sperm per 1 ml, then oligozoospermia is deciphered as an indicator when the number is less than normal.
Oligospermia also indicates a problematic seminal fluid, in which no more than one and a half or two milliliters was provided. teratozoospermia indicates that the product contains more than 50 deformed sperm.
Why is the sperm count decreasing?
The main reasons are:
- Endocrine disorders.
The main ones include: underdevelopment of the gonads, diabetes mellitus, dysfunction of the thyroid gland and adrenal glands, disruption of the hypothalamic-pituitary regulation - Genetic disorders
- Aggressive effects of toxins:
sleeping pills, steroids, alcohol, nicotine - Diseases of the genitourinary system.
The most common include: trauma, orchitis, varicocele, prostatitis, cryptorchidism - Increased body temperature and feverish conditions
What abnormalities can a spermogram detect?
Using a spermogram, the following diseases and abnormalities are diagnosed:
- oligospermia – too small volume of ejaculate;
- asthenozoospermia – reduced sperm motility;
- oligozoospermia – low sperm concentration;
- akinozoospermia – absolute immobility of sperm;
- necrozoospermia – complete absence of living sperm;
- teratozoospermia – excessive concentration of abnormal sperm;
- hemospermia – red blood cells in sperm;
- leukocytospermia – increased concentration of leukocytes in the ejaculate;
- Azoospermia – ejaculate without sperm.
Why does sperm motility decrease?
This pathological condition can occur against the background of:
How the analysis is carried out
The man is given a separate room and given a signed sterile container with him. The validity period of the material from the moment of collection is only one hour. Transplantation of biomaterial can only be carried out at a temperature of +27…+37C.
The main objective of the analysis is to determine the activity of cellular elements of sperm, such as motility, morphological criteria, number, types of leukocytes, maturity and much more.
The material is sent to the laboratory, where the laboratory assistant begins his work. First, he evaluates morphological qualities. Then, after special staining, viability indicators are examined. To determine the number of sperm, a special reaction is carried out. After this, the laboratory technician calculates the formula for the index of sperm readiness for fertilization.
Sperm examination is not an easy process, and yet there are certain time limits.
There are two types of analysis.
- Base. Here we look at the big picture. This type is used to monitor treatment.
- Advanced. Involves full research. Used during initial treatment.
How to improve spermogram?
It is possible to improve important research indicators by following the following recommendations:
- Reducing the risk of genital overheating
- Elimination of the aggressive effects of toxic substances
- Proper, balanced nutrition
- Maintaining a daily routine (including a full eight-hour sleep)
- Ensuring an optimal rhythm of sexual life
- Timely elimination of endocrinological and urological diseases
- Physical therapy classes. Aerobic exercise (running, rowing) is recommended, but cycling is not recommended
- Taking medications prescribed by a doctor. Men may be recommended vitamins, biological stimulants and other remedies
It is useful to include bananas, tomatoes, avocados, pomegranates, asparagus, pumpkin seeds, and apples in your diet. It is recommended to monitor the predominance of seafood rather than meat. Vitamins and amino acids have a good effect on sperm parameters.
Norm for seminal fluid
The spermogram is deciphered according to several basic parameters that were calculated in laboratory tests.
It is possible to independently calculate all the indicators using an online program, spermogram calculators.
The normal spermogram indicates that:
- the liquefaction time is approximately ten minutes or one hour; if the indicator is exceeded, then we can talk about a decrease in enzyme levels or inflammation of the prostate;
- the norm in the volume of one portion of seminal fluid is set within two or six milliliters; if this indicator is low, then prostatitis is observed or the patient simply had sexual intercourse; if the indicators are high, then the man has not had a woman for a very long time or has cooperitis;
- good viscosity does not exceed 0.5-2 centimeters, if the transcript shows more than the highest mark, then the man has orchitis;
- pH indicators are as good as possible if the spermogram decoding indicates it as 7.2 or eight, but the slightest deviations indicate vesiculitis or prostate inflammation.
An indicator such as the color of seminal fluid can tell a lot, since its brown tint indicates prostate cancer or perineal trauma.
The red color specifies that there is vesiculitis or prostatitis, yellow indicates hepatitis, but the spermogram establishes the color standards for sperm - milky, slightly yellow, grayish and whitish.
Using an online calculator, it is easy to calculate that the normal number of sperm per average portion is 45,000,000 or 450,000,000 million; this volume is missing:
- leukocytes (more than four indicates inflammatory processes in the testicles, appendages, penis or scrotum);
- red blood cells (a large number may mean trauma to the genital organs, malignant or benign tumors, inflammation of the urethra and appendages):
- mucus.
If red blood cells are present in the sample, then professionals say that the seminal fluid is very bad, the sperm are sluggish, and it will not be possible to conceive a baby in the traditional way.
You should pay attention to the structure of sperm, since two tails, two heads, gluing or other deviations affect the speed and reduce the possibility of fertilization of the egg.
Advantages of carrying out the procedure at MEDSI
- Experienced specialists.
They provide both the study of the obtained biological material and the interpretation of the spermogram. Professionals do not make mistakes in their work - Use of modern equipment.
We have our own laboratory, which guarantees that the research will be carried out immediately after collecting the biomaterial. The study is carried out in accordance with international standards, using equipment for automated analysis of ejaculate, which ensures maximum objectivity of the results obtained - Ensuring the comfort of the spermogram procedure
(material collection). The room has a special soundproofing system and has a relaxing atmosphere - FertiProof, a unique system for monitoring the conformity of biomaterial samples.
Thanks to this, any risks of replacing the patient’s biomaterial with someone else’s are eliminated. - Tactfulness and correctness of the staff.
We understand that for some men, donating sperm in a clinic is associated with a number of psychological problems, and we successfully eliminate them - No queues
- Possibilities for treatment of identified disorders.
If necessary, the clinic can provide treatment for detected diseases. Urologists-andrologists and other specialists will be involved in the work
If you are planning to undergo a study in our clinic, call and clarify all its features and cost. A specialist will answer your questions and schedule you for diagnostics at a convenient time.
Rules for sperm donation
Before taking a spermogram analysis, you should find out all the rules for carrying out this process from your attending physician. If you have problems with the process or questions about sperm activity, you should try to find out information on the Internet on specialized websites of the medical center online.
A good spermogram can only be obtained in laboratory conditions, so you should not try to do the procedure at home and then transport it to the medical center in a latex condom. This option will be uninformative, since it gives a lot of errors - latex impurities from the condom, and cannot be carried out under conditions of ideal sterility.
To obtain seminal fluid for analysis, you should contact the center’s specialists yourself and obtain a special container made of glass or food-grade plastic for testing.
For self-masturbation, a young man is taken to a sterile room where he can relax as much as possible. Spermogram tests should be taken strictly according to the rules:
- thoroughly wash your hands and genitals with neutral soap;
- do not donate ejaculate collected after interrupted sexual intercourse;
- in parallel with the donation of seminal fluid, perform an MAP analysis;
- fill out the accompanying documents for the container with real personal data.
To get the most accurate spermogram result, the container with seminal fluid must reach the laboratory no later than an hour after delivery.
The resulting ejaculate should be stored at normal air temperatures of at least twenty degrees Celsius. After the first sperm donation and receipt of the results, you should take a second analysis and decipher the spermogram in order to obtain data over time. This allows you to eliminate the smallest errors and errors that interfere with treatment and replacement of ineffective drugs to normalize the functioning of the reproductive system.
The cost of having a semen analysis done if it needs to be professionally interpreted will vary. This indicator will depend on the level of the clinic and the characteristics of the delivery of biomaterial, so it will cost:
- at least seven hundred Russian rubles;
- maximum one and a half thousand rubles.
You should not save on men's health, so at the same time it is strongly recommended to order a MAP test, since one container of the submitted material will be enough for them and the results can be obtained the very next day.
What to do if the spermogram results are bad
First of all, there is no need to panic. You should know that no sperm indicator determines the minimum chances of fertilization. That is, even with poor ejaculate levels, pregnancies often occur. Sperm is very sensitive to various irritants such as food and bad habits, so the results may be false. To avoid mistakes, doctors prescribe a repeat test after 1-2 weeks. During this period, a man must lead a healthy lifestyle and give up all possible irritants.
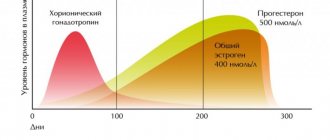
To clarify the diagnosis, additional tests are prescribed (taking into account the identified diseases). If there are endocrine disorders, the patient needs to check the level of testosterone, prolactin and other hormones.
In some cases, the doctor may prescribe an extended spermogram to fully analyze the condition of the man’s reproductive system. In addition to basic parameters, advanced analysis includes biochemical examination of sperm. The test shows the concentration of proteins, zinc, citric acid and fructose in the seminal fluid. Advanced analysis allows you to evaluate the functioning of the prostate gland and the entire reproductive system.
More information is provided by sperm DNA fragmentation. The test shows the number of damaged and abnormal germ cells in the ejaculate. Also, an extended spermogram includes a MAR test, which allows you to detect antisperm antibodies on the membranes of damaged sperm.
The presence of antibodies confirms the immunological incompatibility of partners. Antisperm antibodies trigger mechanisms of an autoimmune reaction, which provokes the adhesion of germ cells and, accordingly, a decrease in their motility.
It is recommended not only for those men who have difficulties with fertilization to undergo a spermogram. The results of a spermogram can reveal various disorders in many body systems. Sperm examination is one procedure that makes it possible to find inflammation, tumor, consequences of injury, hidden infections and other disorders.
How to get reliable results
For accurate results, sperm must be donated after 3-5 days of abstinence. Ejaculation is carried out immediately before the test, so the sample must be submitted to the laboratory. It is impossible to collect sperm from a condom, since the protection products contain harmful substances. The sample must be given in a sterile container. In the laboratory, the sample is processed 30-60 minutes after the sperm is collected. Analysis performed later may be considered unreliable, since long waiting times and refrigeration have a negative impact on sperm characteristics.
An assessment of a man's fertilizing ability should take into account all sperm parameters simultaneously, and not separately. It is also worth remembering that the characteristics of ejaculate are variable. In three months, sperm is completely renewed, and accordingly, all indicators may change. Therefore, the doctor determines the time for donating ejaculate individually for each patient.
A standard sperm examination includes 2-3 spermograms taken at intervals. This allows you to form an objective picture of the health of the male reproductive system, since sperm levels even in a healthy person change daily.
Indications for the study
It is necessary to submit ejaculate for a spermogram in the following cases:
- A man is simply interested in his reproductive health and wants to make sure of his ability to become a father;
- The partner does not become pregnant after at least one year of regular sexual activity without the use of contraception;
- A man has been diagnosed with a disease or congenital pathology that can lead to infertility (hypogonadism, varicocele, orchitis, urethritis, prostatitis, etc.);
- The couple is planning to resort to in vitro fertilization or artificial insemination.