Some mothers are faced with the fact that breastfed children are often capricious after eating. Despite the fact that the woman eats properly and nutritiously, and the baby receives a sufficient amount of breast milk, he does not gain weight. The causes of such symptoms may be different. To make an accurate diagnosis, the doctor prescribes certain tests, including biochemical ones. Analysis of feces for carbohydrates in infants helps to identify various disorders in the intestines. Such problems in children under one year of age are quite common and require special attention.
Stool testing for carbohydrates
An experienced pediatrician can quickly make a preliminary diagnosis if certain symptoms are present. To confirm it and determine the course of the disease, specific tests are prescribed. Determining the carbohydrate content in a baby's feces is a biochemical study of fecal matter, which allows us to determine the ability of the intestines to digest and assimilate sugars.
To make a conclusion, the test can be used either independently or in combination with other studies: coprogram, intestinal dysbiosis, hemotest for lactose intolerance.
Carbohydrates in feces are in the form of milk sugar. This disaccharide is broken down into glucose and galactose in the small intestine by the action of lactase (an enzyme involved in the metabolism of carbohydrates contained in milk). Some lactose is not broken down and remains in the intestinal lumen. This leads to the development of increased gas formation, diarrhea, and colic in the abdominal area. In children, lactase activity decreases and lactase deficiency develops. Most often, the pathology is observed in premature newborns.
Using a test for determining carbohydrates in stool, diseases of the gastrointestinal tract and hypolactosia are detected. The study is widely used in pediatrics and gastroenterology.
Additional research to clarify
If there is a suspicion that the patient has pancreatitis, a scatological analysis of stool is prescribed, which is often called general, since it is complex in nature and also contains indicators for carbohydrates. This diagnostic method is necessary to identify not only the presence of this disease, but also disturbances in the functioning of the stomach, liver, intestines, and gall bladder. Scatological analysis of stool as the main method of analysis is necessary when there is a possibility that a person develops pancreatitis, cholecystitis, or hepatitis.
Diarrhea often occurs during pancreatitis. The study tests the soap content of stool, which becomes mushy, liquid, and contains pieces of undigested food. The amount of soap in waste products is no less important than the amount of carbohydrates and fat. When a coprogram is deciphered, it is necessarily taken into account. The substance is formed from fat processed by the body. Soap should be present in small amounts in feces. If they are normal, then the functioning of the gastrointestinal tract is normal. When they are absent, this indicates that a person develops pancreatitis, fermentation dispersion and other diseases.
The coprogram should reveal the content or absence of neutral fat in human waste products. Neutral fat is necessary for the normal functioning of organs, but in older children and adults it should be absent in the feces. Why? Neutral fat is one of the main sources of energy for the human body. Once it enters the cells, it must be completely processed. The waste products of infants may contain neutral fat, and then in small quantities. If it is present in the stool of older people, this will indicate a violation of the absorption of substances by the intestines or an accelerated evacuation of its contents. Such fat appears if the production of bile and its flow into the small intestine is impaired, or a person develops pancreatitis.
Fat and fatty acids are two different categories of substances. Fatty acids can be present in small amounts in the stool of children if they are breastfed or bottle-fed. But older children and adults should not have them in their waste products. Fatty acid, like neutral fat, must be completely absorbed by the body. If the opposite happens, a person experiences in the body: fermentation dispersion, evacuation of intestinal contents, or impaired absorption in it. During coprogram, fatty acid levels are examined. If they are present in the stool, there is a high probability that the patient has pancreatitis, various diseases of the liver and biliary tract.
In what cases is a stool test for carbohydrates prescribed for infants?
The main indication for the study is the suspicion of lactase deficiency in a child. A preliminary diagnosis is made based on the following symptoms:
- Underweight in a child with normal nutrition.
- Retarded physical and mental development.
- Infantile colic, bloating.
- Frequent loose and foamy stools.
- Regular regurgitation.
- Nausea.
- Short shallow sleep.
- Frequent crying at night for no apparent reason.
Also indications for the test are:
- Diseases of the small intestine: enteritis, celiac disease.
- Pathologies of the pancreas: pancreatitis.
- Congenital fermentopathy.
- Difficult to treat iron deficiency anemia.
A contraindication for testing stool for carbohydrates in infants is the age of the baby under 3 months. During this period, enzymatic processes are formed in the intestines (enzymes are formed), so the results may not be informative.
Symptoms for analysis
Certain symptoms that manifest lactase deficiency in children have been recorded.
- Slow development. In this case, the baby’s body cannot absorb enough nutrients from milk. To ensure that this fact does not go unnoticed, the newborn should be regularly weighed and compared with the indicators described by the norm for his age. If there is a lag in the weight or height of the baby, it is necessary to take the described test.
- Changes in the child's stool and frequency of bowel movements, reaching 10 times a day. The presence of foam, mucus and sour odor indicates a possible illness.
- Constipation is common.
- Manifestation of allergic reactions.
- When identifying pale skin and mucous membranes of the baby.
If at least one of the listed symptoms appears, you should consult a doctor and undergo a stool examination. The diagnosis of lactase deficiency can only be made by a doctor after conducting the necessary tests.
Preparing for the study
The reliability of an analysis for carbohydrates in a baby's stool depends on proper preparation for the test. This does not require any special actions, you just need to follow some rules:
- The baby's nutrition should remain the same. It is worth holding off on introducing new complementary foods for 1-2 days.
- If the child is bottle-fed, the formula should not be changed until the results are obtained.
- The results may be affected by the child's mental state. It is necessary to try to ensure healthy sleep for the baby.
- The container, diaper or oilcloth must be prepared in advance.
Preparation
In order to obtain reliable results from examining stool for the presence of carbohydrates, it is important to properly prepare for the test. For this, doctors recommend:
- 3 days before this, exclude the use of rectal suppositories and do not do cleansing enemas;
- a week before the procedure, stop taking medications that can affect the character of stool (stimulate diarrhea, constipation), increase peristalsis, or contain dyes;
- the day before the test, do not change your usual diet, but give up alcohol and bright, colorful vegetables and fruits such as beets, asparagus, etc.;
- 2-3 days before submitting the sample, do not undergo diagnostic tests using contrast agents (MRI, CT, etc.).
How to properly collect biomaterial
Feces are collected for carbohydrates from infants in the morning. The child is placed on an oilcloth or napkin and waits for bowel movements to occur. Defecation should be natural. The use of laxatives (suppositories, enemas) is unacceptable, as this distorts the result. You should also not collect feces from the diaper. A special lubricant located on its top layer affects the information content of the results.
The biomaterial is collected into a container with a special spatula in the amount of about two spoons. The biomaterial must be taken to the laboratory within 4-5 hours after collection. It is allowed to store feces for no more than 8 hours in the refrigerator at a temperature of +2 to +8 degrees Celsius.
Meaning of the norm and decoding
Analysis of stool for carbohydrates, which is accessible and quite simple, is performed on all infants.
- When deciphering the analysis, the pediatrician first of all pays attention to the amount of carbohydrates. This indicator is the main one, since with lactase deficiency the infant’s body loses the ability to break them down. Left undigested, carbohydrates are excreted from the baby’s body along with feces. In the feces of newborns, the carbohydrate content should not exceed 1%. As the child grows, this value should gradually decrease. The normal indicator for infants under six months of age is a value of 0.5-0.6%. In infants older than six months and up to one year, it should not be higher than 0.25%.
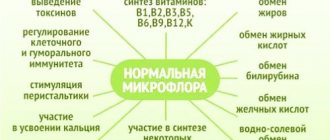
- The beneficial microflora of the large intestine has the ability to partially digest lactose. Acetic and lactic acids, formed during its breakdown, significantly increase the acidity of stool. The normal level of stool acidity should not be less than 5.5. An indicator of 5.5 or lower is grounds for suspicion of lactase deficiency.
- An increased number of leukocytes and C-reactive inflammatory protein in the stool indicates the presence of inflammatory processes in the intestines , which may be caused by lactose intolerance.
- The presence of a significant amount of fatty acids in feces may be a consequence of disturbances accompanying the process of absorption of nutrients, which are indispensable companions of lactase deficiency.
The basis for diagnosing lactase deficiency is the result of an analysis confirming a high (more than 1%) carbohydrate content in the feces of an infant, combined with the presence of a detailed clinical picture of the pathology. In this case, the child is prescribed a course of appropriate treatment.
Increased acidity of stool - coupled with an increase in the amount of C-reactive inflammatory protein, fatty acids and leukocytes - can result not only from lactase deficiency, but also from other pathologies that disrupt the functioning of the digestive system.
Analysis of stool for carbohydrates helps with a high degree of probability to verify the presence of lactase deficiency, without making it possible to establish its type and cause.
If congenital lactase deficiency is suspected, infants undergo a genetic test, which consists of searching for genes that are responsible for extremely low lactase production.
Most often, lactose intolerance occurs due to celiac disease (a digestive disorder caused by damage to the villi of the small intestine by products containing gluten and cereal proteins), various intestinal infections and an allergic reaction to cow's milk protein.
All these pathologies first disrupt the functioning of the small intestine, after which the body loses the ability to break down and absorb milk sugar.
How the test is carried out
The Benedict method is used to determine the carbohydrate content in feces. The test reflects the body's ability to absorb glucose and carbohydrates. The principle of the analysis is to identify the ability of sugars to act as a catalyst. They can, with the help of impurities and additives, restore copper from the 2+ to 1+ oxidation state.
A certain amount of distilled water is added to the biomaterial and centrifuged. A chemical substance, the so-called Benedict's reagent, is added to the resulting sample. It consists of a mixture of water, copper sulfate, sodium carbonate and sodium citrate. After addition, the oxidative reaction during which the coloring process occurs is observed. The data is interpreted as follows:
- Blue color – carbohydrate concentration less than 0.05%.
- Turquoise color – 0-0.05%.
- Green –0.6-1%.
- Light green – 1.1-1.5%.
- Yellow – 1.6-2.5%.
- Orange – 2.5-3.5%.
- Red – carbohydrate content in baby feces is 4.0%.
Norm of carbohydrates in feces
| Patient age | Amount of carbohydrates |
| Children under 1 year | 0 – 0,25% |
| Children over 1 year old and adults | Not detected |
Note: in children of the first year of life the following deviations from the norm may be observed:
- 0.3 – 0.5% (insignificant);
- 0.6 – 1% (average);
- more than 1% (significant).
Factors influencing the result:
- Violation of the rules for preparing for analysis;
- Errors when collecting biomaterial;
- Features of the daily diet;
- Patient's age;
- Genetic factors and family history;
- Intestinal infection or inflammation;
- Taking prebiotics, antibiotics and other drugs.
Normal values
The study determines not only the carbohydrate content. The degree of acidity of feces, the concentration of protein, aliphatic omega acids, and leukocytes are also determined. Test results can usually be obtained 1-2 days after submitting the biomaterial for testing. Normally, carbohydrates in a baby's feces should not exceed 0.25%. The preliminary diagnosis depends on how much the result is exceeded:
- Deviations from 0.3 to 0.5% are considered small and are not a reason to prescribe therapy.
- At values from 0.6, observation is carried out. If symptoms worsen, a repeat test is prescribed. The child's condition is assessed jointly by the mother and pediatrician.
- If the rate is more than 1%, an additional set of examinations is prescribed to identify the cause and prescribe therapy.
Indications for analysis
Determination of carbohydrates in feces can be an independent diagnostic analysis or carried out in conjunction with other studies, which include:
Biochemical research is not carried out on children in the first three months of life. At this age, digestive processes are just beginning to form, and the result of the analysis will be uninformative.
Gastrointestinal tract dysfunction
The study is prescribed for pathologies of the small intestine and pancreas. If you suspect the absence of one of the digestive enzymes in the body, the procedure helps to determine its type.
The procedure is indicated for adults and children with frequent dyspeptic disorders. Determination of carbohydrates in feces allows us to determine the cause of painful sensations in the abdomen, impaired peristalsis, and excessive gas formation. The study is prescribed to patients who complain of bloating, nausea and vomiting after each meal. Indications for laboratory testing also include:
- chronic diarrhea of unknown origin;
- the occurrence of symptoms of flatulence, especially after eating foods containing significant amounts of sugars and starch;
- sudden weight loss;
- suspected carbohydrate malabsorption.
Carbohydrates in feces can appear not only for pathological reasons. This condition is often diagnosed in people who eat an unbalanced and monotonous diet.
Warning: “Before carrying out the analysis, the laboratory assistant evaluates the external characteristics of the feces, notes signs of rotting and fermentation. These pathological processes occur in the patient’s gastrointestinal tract when it is impossible to fully break down starch. Fecal fermentation occurs in people with a partial or complete inability to absorb simple and complex carbohydrates.”
Lactase deficiency
Determination of carbohydrates in feces is necessary for the timely detection of lactase deficiency in young children. Lactose is a disaccharide that is present in large quantities in breast milk. During metabolism, it is broken down into galactose and glucose, and then completely absorbed in the gastrointestinal tract. The digestive enzyme lactase processes lactose (milk sugar). When it is deficient in the child’s body, symptoms of dyspepsia occur:
Lactase deficiency is most common in premature babies. When a pathology is diagnosed, the child is prescribed replacement therapy and the diet is adjusted.
Increased performance
The carbohydrate content in a baby's feces of 0.2-0.4 is considered a minor deviation. Even with such an excess, the pediatrician can make adjustments to his diet and, if necessary, prescribe certain medications.
The causes of increased carbohydrates in the feces of infants are various disorders of intestinal functionality. These include:
- Imbalance of intestinal microflora.
- Enzymatic insufficiency of the pancreas, characterized by disruption of the absorption and breakdown of carbohydrates.
- Congenital intolerance to disaccharides.
- Transient lactase deficiency, in which the production of the enzyme decreases (due to damage to enterocytes). It is this form of lactose disaccharide intolerance that most often causes an increase in carbohydrates in the stool in children under one year of age. Pathology develops due to exposure to rotavirus.
Analysis indicators
The analysis is designed to detect the level of carbohydrates in the stool, changes in its acid-base level, as well as counting proteins, leukocytes and fatty acids. This analysis has the following indicators.
- The amount of carbohydrates is the main indicator, since undigested lactose is excreted from the body in the feces. In infants, the content norm is no more than 1% carbohydrates, and this percentage gradually decreases to 0.5%
- In the colon, lactose is broken down into lactic and acetic acid, thereby increasing the acidity of the stool. The norm sets a pH of at least 5.5, and with lower values the child may have lactose deficiency.
- Increased inflammatory protein and white blood cells indicate the presence of inflammation in the intestinal area.
- Fatty acids indicate a malabsorption of nutrients, which occurs with lactose intolerance.
Carrying out the test is not difficult for infants, which is why it is done on almost all newborns. The decoding of the obtained indicators should be carried out at a doctor’s appointment, since if the analysis does not meet the standards, but the above symptoms are absent, only observation of the baby is required.
If after some time we carry out a second analysis, the interpretation of which gives a positive result, we can conclude that the disease is absent, and the failures are caused by the physiology of the baby’s body.
What influences the indicators
If carbohydrates in a baby’s stool are elevated, do not immediately panic. The pathology is easily treatable, despite serious clinical manifestations. In some cases (rarely) the result is false positive. There are several reasons for this:
- Incorrect collection of biomaterial: feces taken from a diaper, non-compliance with storage rules.
- On the eve of the test, the child was fed a low-lactase formula.
- Use of antibacterial drugs during the test.
How to take the test correctly?
- Before collecting material, food should not change. You cannot introduce new foods into your child’s diet or give him complementary foods, as this may affect the composition of the newborn’s stool.
- If possible, you should stop taking all medications. Before doing this, it is better to consult with your treating pediatrician, who will determine whether it is possible to stop treatment for a few days.
- Do not give your child laxatives or do enemas for 2-3 days before the procedure.
- The use of rectal suppositories is prohibited.
Preparing containers
To collect biological material, you can use pharmacy or home containers. Containers adapted for feces must be properly prepared. To destroy pathogenic microorganisms, it is necessary to boil the jar, dry it and immediately place the biological material into it. Contamination of the container with bacteria can blur the analysis picture, since microorganisms consume carbohydrates when multiplying. As a result, false negative tests can be obtained.
We recommend reading:
Intestinal dysbiosis in children: symptoms and treatment (diet, medications)
Since it is impossible to completely destroy pathogenic bacteria by boiling, it is better to use pharmaceutical containers designed for collecting feces. Special containers undergo mandatory processing, which guarantees the sterility of their walls. Therefore, the risk of incorrect results when using such containers is much lower.
Collection of material
- It is necessary to lay an impenetrable oilcloth or plastic film under the newborn.
- Wait for a bowel movement.
- Take biological material from 4-5 places on the surface of the feces, the approximate total volume of the sample should be 50 ml (1/3 of the container volume).
- If the amount of stool is very small, then you should wait until the next bowel movement, since a small sample volume cannot be used for research.
- If there is liquid stool, pour 5-10 ml of liquid into a collection container.
- Close the container tightly and take it to the laboratory.
Feces should be stored in a cool, dark place. The best option is a shelf in the refrigerator that has no food on it. The sample can only be stored for 4 hours. If the sample is delivered to the laboratory later, it cannot be used, since over time the substances in the container react and are destroyed. This may lead to unreliable results.
Feces are collected for carbohydrates from infants in the morning. The child is placed on an oilcloth or napkin and waits for bowel movements to occur. Defecation should be natural. The use of laxatives (suppositories, enemas) is unacceptable, as this distorts the result. You should also not collect feces from the diaper. A special lubricant located on its top layer affects the information content of the results.
The biomaterial is collected into a container with a special spatula in the amount of about two spoons. The biomaterial must be taken to the laboratory within 4-5 hours after collection. It is allowed to store feces for no more than 8 hours in the refrigerator at a temperature of 2 to 8 degrees Celsius.
Additional tests
Doctors do not make a conclusion that a child has lactase deficiency based on clinical manifestations and the results of one test. To confirm the pathology and prescribe adequate therapy, the pediatrician prescribes a comprehensive examination:
- Coprogram. The analysis evaluates the ability to digest food and the enzymatic activity of the digestive organs.
- Biopsy of the colon mucosa. Using a biopsy, samples of biomaterial are obtained for further histological examination.
- Analysis for dysbacteriosis. Various pathogenic organisms can interfere with the normal absorption of lactose.
- Clinical blood test. An increased level of ESR and leukocytes suggests the presence of an inflammatory process.
- Blood for biochemistry (glucose level, bilirubin).
- Immunoglobulin E test.
- Fecal analysis for helminthiasis.
What is this?
Lactose is a carbohydrate from the disaccharide group found in milk (including breast milk) and dairy products.
In order for lactose to be completely absorbed by the body of an infant, it must be broken down into monosaccharides suitable for absorption by the structures of the small intestine.
The digestive enzyme lactase, synthesized by the body specifically for this purpose, is responsible for the breakdown of lactose. If lactase is produced in insufficient quantities or is not released at all, the baby develops lactose intolerance.
As a result, lactose, which remains undigested and not absorbed in the small intestine, is sent to the large intestine, where, becoming an excellent nutrient medium, it provokes rapid growth of bacteria living in it, which contribute to the dilution of stool and the release of excess gases.
Due to the high acid content in the stool, the absorption capacity of the intestinal walls is impaired. As a result, most of the enzymes and nutrients (represented by vitamins, proteins, macro- and microelements, fats, carbohydrates) contained in breast milk are not absorbed by the baby’s body.
Lactase deficiency is often referred to by doctors as the synonymous term “lactose intolerance,” meaning that the human body either does not digest or does not tolerate lactose contained in any dairy products. This phenomenon can also occur in adults, but they - unlike infants - have the opportunity to get rid of this problem by completely abstaining from dairy products.
For infants, mother's milk is the only food available to them, so timely detection of lactase deficiency and prescribing appropriate treatment will help avoid delays in their physical and mental development.
In order to verify the presence or absence of lactose intolerance in an infant, a stool test is performed for carbohydrate content.
This study, also called the Benedict method, is aimed at identifying reducing sugars in the baby's stool that have the ability to reduce copper (II) hydroxide to copper (I) oxide. These sugars are:
- fructose;
- glucose;
- lactose;
- galactose;
- maltose.
Lactose and simple sugars (galactose and glucose), which are products of its breakdown, are most often found in infant feces. The Benedict method allows you to determine whether the processes of absorption and breakdown of carbohydrates occur normally in the body of an infant.
Treatment of abnormalities
Based on the test results, the pediatrician prescribes treatment. Before the age of one year, this specialist is the main one for the child. A gastroenterologist can only give additional advice, but the pediatrician determines the therapy. Self-treatment at this age can pose a threat not only to the health, but also to the life of the child.
If carbohydrates in the stool of infants are elevated due to lactase deficiency, then treatment is prescribed. Therapy at an early age has its own characteristics:
- The basis is therapeutic nutrition. It consists of almost completely eliminating products containing lactose. In some cases, you even have to give up natural breastfeeding and switch to lactose-free formulas.
- The use of drugs containing the lactase enzyme: “Lactazar”, “Maxilat”, “Tilactase”.
- Dairy-free porridges are introduced during complementary feeding. It is allowed to consume fermented milk products in minimal quantities.
Diet therapy is monitored by analyzing the carbohydrate content in feces.
Analysis results
Benedict's reagent contains copper sulfate, the solution of which is blue. If there are no sugars in the stool, the reaction does not occur, the mixture remains blue. If lactose is present in the stool, it oxidizes the copper ion to brick-red copper(I) oxide. A small amount of carbohydrates will produce a small amount of reddish oxide, which mixes with the blue color of the sulfate, resulting in a green color. The significant presence of carbohydrates gives the mixture a red color. The laboratory technician compares the resulting color with the colors of standard solutions. Using the table, it determines what carbohydrate content a given color corresponds to. The result is given in % or g/l.
Monitoring lactase deficiency
Children with congenital lactose intolerance are forced to follow a lifelong diet and take medications containing the enzyme lactase. In the transient form of the disease, the prognosis for recovery is favorable. Most children return to breastfeeding and tolerate foods containing milk sugar normally.
The sufficient effectiveness of treatment is judged by the child’s weight gain, disappearance of dyspeptic symptoms, and normal rates of mental and physical development. After completing the course, the doctor prescribes a repeat test for carbohydrates.
If your baby experiences the first symptoms of lactase deficiency, you should immediately contact your pediatrician. Poor absorption of sugars can be a consequence of serious pathologies. Delay in treatment contributes to the transition of the disease to a chronic form that is difficult to treat.
Indications
The indication for performing a stool test for carbohydrates is the presence in a child of certain symptoms indicating lactase deficiency.
They can be presented:
- A clear delay in the physical and mental development of the baby, caused by insufficient absorption of nutrients that occurs against the background of enzymopathy (the so-called pathology that occurs due to the lack or complete absence of cellular enzymes responsible for digestive processes). In order to detect this pathology in a timely manner, the baby must be weighed regularly, comparing weight gain with normal values. A too slow increase in a child’s anthropometric indicators is a cause for concern.
- Allergic rashes on the surface of the skin.
- The presence of frequent (eight to ten times a day) watery or foamy stools, which have a sharp sour odor, are quite abundant and contain a significant amount of mucus and undigested lumps of food.
- The occurrence of iron deficiency anemia (manifested by pallor of the mucous membranes and skin), caused by impaired intestinal absorption, difficult to treat.
- Having frequent constipation.
- The baby's restless behavior: feeling hungry, he demands the breast, but as soon as he starts sucking, he immediately throws it away and bursts into tears. As a result, the feeding process is greatly delayed, bringing suffering to both the child and his mother.
- Severe pain in the tummy of a full baby. Pain can be caused by colic and excessive accumulation of gases, under the influence of which the tummy begins to growl loudly and swell.
The occurrence of the symptoms described above is a reason to visit a pediatrician, who will give a referral to analyze stool for carbohydrates.
Examination of stool for carbohydrates can also be prescribed for adult patients:
- Suffering from chronic pancreatitis, a disease characterized by a deficiency of pancreatic enzymes, as a result of which complex carbohydrates cease to be broken down and absorbed. Once in the large intestine and subjected to fermentation, they are excreted from the body along with feces. Analysis of stool in such patients reveals the presence of amilorrhea - an extremely high content of undigested starch.
- Those who complain of sudden weight loss, severe diarrhea, characterized by a strong odor of feces, and food intolerance, since in all these cases, impaired absorption of carbohydrates may be due to insufficient efficiency of parietal digestion, caused by damage to the mucous membranes of the small intestine.
Advantages and disadvantages of the method
Fecal carbohydrate testing is widely used due to its low cost and ease of implementation. However, it has disadvantages:
- In infants, the microflora of the large intestine is just populating, so lactose is not utilized in the large intestine and more of it ends up in the feces, sometimes the content exceeds 1%.
- The method does not allow determining the content of individual carbohydrates: lactose, sucrose or glucose for the purpose of differential diagnosis of lactase, sucrase or other types of deficiency. It should be noted that lactase deficiency is much more common than other types.
Decoding
What is this?
Hello, dear visitors of my blog, it’s nice that you again indulge me with your attention. Today the topic of my article is the analysis of feces for carbohydrates in infants, the decoding of this analysis and the reasons for its prescription.
I think many will also be interested in learning what lactase deficiency and lactose intolerance are, and how lactase differs from lactose.
You will learn how to properly collect stool from an infant and what additional tests are used to conduct a more accurate diagnosis.
I will list the most common signs of lactase deficiency:
- The baby has frequent loose stools, while in the stool you can see mucus, greenish foam, undigested lumps of food, and the smell of the stool will be sour.
- The child feels hungry, asks for the breast, starts sucking and immediately refuses, crying. This continues for a long time, feeding is delayed and brings a lot of suffering for mother and baby.
- After feeding, the child experiences discomfort in the abdomen, cries, and may burp (read about this here). Regurgitation is abundant and frequent. Even vomiting is possible.
- Abdominal pain is caused by colic, bloating, and increased accumulation of gases. This can be seen in the baby's tummy and even heard: it swells and purrs.
- It also happens the other way around: instead of diarrhea, there is frequent constipation.
- Due to impaired intestinal absorption, the child experiences a lack of iron. This is manifested by blanching of the skin and mucous membranes. I wrote about the hemoglobin norm in this article.
- The skin may develop an allergic rash.
- The baby began to gain weight poorly, and its growth slowed down or stopped. Lack of lactose affects the mental and mental development of the baby.
If you notice any of these symptoms, consult your pediatrician. He will prescribe an examination and appropriate treatment.
So, you have been prescribed a stool test for a special test. I'll tell you how to do it correctly.
There are certain recommendations that are important to follow in order to obtain the most reliable research result. These are the recommendations:
- The collected material should be no less than a teaspoon in volume.
- The liquid component of the feces is taken for analysis.
- The baby must poop on his own; you cannot give him an enema or give him laxatives.
- To collect stool for analysis, you cannot take diapers or a piece of cloth. Take oilcloth material or purchase a special container for collecting and storing feces at the pharmacy. All these things must be sterile.
- It is best to donate freshly collected feces (within 4 hours after collection). The maximum permissible storage period for analysis material is 10 hours.
- Before taking the test, the child must be fed in the usual way with regular everyday food.
- Mom's menu should not differ from the usual one.
- Before taking a carbohydrate test, you should not take medications. Stop taking them a few days before your chosen date for fecal laboratory testing.
If you do everything correctly, you will not have to repeat the analysis.
Stool analysis is performed primarily to determine the amount of carbohydrates in it. In addition, with the help of this analysis, it is possible to determine the degree of acidity of feces, identify the content of protein, leukocytes and fatty acids in the composition of the biomaterial under study.
The pediatrician interprets the analysis and compares the result with the child’s general well-being. If laboratory tests show deviations from the norm, and the baby does not feel discomfort, treatment is not prescribed. The doctor will offer to monitor the little patient, and will also prescribe a repeat stool test for carbohydrates.
Of course, you want to know more about decoding the analysis? I'll try to explain everything clearly.
- Lactose is a carbohydrate for which the analysis is carried out; if it is not digested, then it can be found in children's feces. To determine whether the result corresponds to the norm, the following indicators are used: ideal - the percentage of carbohydrates is less than 0.25; from 3 to 5 – slight deviation from the norm; from 6 to 1 percent – average deviation; all values above 1 are a significant excess of the norm; such indicators give grounds to assert that the baby has lactose intolerance. Let me explain, the younger the baby’s age, the higher the norm for him. That is, in newborn babies, the percentage of carbohydrates normally approaches 1. But in children from three to six months, this value decreases to 0.5, from 6 to 12 months – to 0.25.
- If there are a lot of leukocytes in the stool and the protein content is high, then there is an inflammatory process in the intestines, which may also indicate lactose intolerance.
- Fatty acids detected in large quantities indicate that the absorption of nutrients in the intestines is impaired. This is also one of the signs of poor absorption of lactose by the body.
- Part of the undigested lactose, entering the large intestine, can be broken down by bacteria into lactic and acetic acids. Because of this, stool becomes more acidic. If the acid-base balance is less than 5.5, then the doctor can assume the presence of a disease associated with lactose intolerance.
Stool analysis, which determines the carbohydrate content in it, is a very common way to detect lactase deficiency.
However, I found out that this method does not have a high degree of reliability. Why? I will be happy to share information with you. This study does not reveal exactly what type of carbohydrates are found in stool.
Detected carbohydrates may be lactose, glucose, or galactose. In addition, the norms for carbohydrate content in young children are not clearly defined.
To confirm the diagnosis (lactase deficiency), other research methods are used. For example, these:
- Coprogram or general detailed analysis of stool.
- Hydrogen content test. The air obtained during exhalation is analyzed, the amount of hydrogen and methane in it is determined, which are obtained from the incomplete breakdown of lactose by bacteria. The patient must first consume lactose.
- Biopsy of the intestinal mucosa. This method has a high degree of reliability. However, it is very difficult to use, especially in infants.
- Test for lactose and glucose. It is necessary to donate blood on an empty stomach, then drink lactose, after which the blood is donated again after a few hours. This determines how the body reacts to lactose. An insufficient increase in blood glucose levels after consuming lactose will indicate a possible intolerance to this enzyme.
You can do all these tests both in a public clinic and in a private one. For example, the network of branches of the independent private laboratory INVITRO, which today covers the countries of Russia, Belarus, Ukraine and Kazakhstan, is very popular.
This is where I want to end my article, which I tried to make interesting and as useful as possible for you. I hope I succeeded. Thank you again for your attention, do not forget to subscribe to updates, share the article with your friends. Be healthy, take care of yourself and your children.
This article is worth sharing.
The level of carbohydrates in feces is determined as a percentage. The results of the analysis differ between children of different ages and adults. Often the cause of unfavorable indicators is dysbacteriosis or immaturity of enzymatic systems. At the same time, the pediatrician carries out therapeutic measures and corrects microbiological disorders in the baby’s intestines.
The ideal option is the absence of carbohydrates in the feces of children and adults, which indicates a normal state of health. Even those with a sweet tooth break down these organic substances, and then absorb the products of their metabolism. Carbohydrates are processed already at the stage of entering the oral cavity through enzymes in saliva. As food passes through the gastrointestinal tract (gastrointestinal tract), they are completely absorbed.
| Acceptable indicators | Breastfed children | Formula-fed children | Children over one year old |
| Daily amount of feces | 40-50 g | 30-40 g | 100-250 g |
| Consistency | Mushy, sticky, viscous | Putty-like | Decorated |
| Color | Yellow, yellow-green | Yellow-brown | Brown |
Indications for analysis
The analysis is interpreted by a gastroenterologist, therapist, pediatrician or general practitioner.
- Chronic diarrhea and digestive disorders in adults;
- Headaches, apathy and weakness, lack of body weight,
- Stomach disorders without established causes;
- Previously identified malabsorption in adults;
- Diagnosis of congenital lactase deficiency in infants under one year of age;
- Lack of required weight gain in newborns.
General information
Impaired absorption of carbohydrates in the small intestine - malabsorption - is a sign of enzymatic deficiency, which can be either hereditary or acquired.
The most common type of malabsorption is lactase deficiency - lactose intolerance, i.e. the body's inability to break down and absorb milk sugar. Congenital lactase deficiency manifests itself already in the first months of a child’s life and is characterized by a sharp delay in weight gain. In adulthood, the acquired form is most often diagnosed. Less commonly observed is a malabsorption of sorbitol alcohol, fructose, trehalose, and sucrase-isomaltase.
Regardless of the type of enzymatic deficiency, the accumulation of large amounts of undigested carbohydrates in the intestines manifests itself in the same way:
- spasmodic pain (colic) in the abdomen, provoked by impaired intestinal motility;
- increased gas formation due to increased fermentation of bacterial microflora;
- diarrhea, the cause of which is the retention of a large amount of fluid in the lumen of the intestinal tube (osmotic effect);
- signs of intoxication of the body: headaches and dizziness;
- general weakness and lethargy;
- nausea and vomiting;
Malabsorption may also be temporary. Often this condition develops after an intestinal infection or an acute inflammatory process, serious operations on the gastrointestinal tract, etc. An ill-designed diet can also affect the speed and extent of carbohydrate absorption. For example, increased sorbitol content in familiar foods can impair the absorption of fructose.