Kawasaki disease (syndrome) in children: how dangerous is this systemic vasculitis?
Description
Have you been struggling with HYPERTENSION for many years without success?
Head of the Institute: “You will be amazed at how easy it is to cure hypertension by taking it every day...
Read more "
Kawasaki disease refers to generalized vasculitis of unknown etiology of an acute necrotizing nature, affecting large and small arteries, as well as the skin and mucous membranes of the body. It was first described in 1961 by the famous Japanese physician Tomisaku Kawasaki.
All children aged from six months to eight years are at risk (approximately 80% of patients have not reached the age of three), and boys suffer from the disease 1.5 times more often than girls.
Kawasaki syndrome is most widespread in Asian countries - there its frequency is 100:100,000 children under five years of age.
In Europe and the USA, the disease is much less common - for example, in Germany, 9 children out of 100 thousand suffer from it. Also in the history of medicine, there are cases when Kawasaki disease was diagnosed in adult patients.
Causes
The exact causes of the development of Kawasaki disease are still unknown, but the fact that its outbreaks have some cyclicity and seasonal variability suggests an infectious nature.
In addition, examinations of children with this form of vasculitis revealed in their blood remains of unknown microorganisms that most closely resemble viruses.
In addition, there are theories that the disease is a response of the immune system to exposure to some kind of toxin, as well as the role of hereditary factors and ethnicity (evidence of this is the increased sensitivity of Asian children to Kawasaki syndrome).
Classification
The diagnosis of Kawasaki syndrome can be complete or incomplete: in the first case, patients have 5 of the main 6 symptoms of the disease, including high fever, or 4 symptoms in combination with coronary aneurysms.
If there are fewer signs (provided that they cannot be caused by other reasons), then the patient’s condition is defined as incomplete (atypical) Kawasaki syndrome.
There are three main stages in the clinical course of the disease:
- acute period, which lasts from 7 to 10 days;
- subacute period lasting 2-4 weeks;
- a recovery period that can last from several months to several years.
Danger and complications
Despite the threatening symptoms, with timely diagnosis, Kawasaki disease is quite treatable. The mortality rate in this case is 1-2%, and death can occur both in the first month after the onset of the disease and several years later.
The main danger is that in 5-20% large and small arteries are involved in the pathological process, resulting in a pathological dilatation of the coronary arteries.
Other complications of Kawasaki syndrome include inflammation of the meninges, joints and bladder, but they are usually not life-threatening.
Why do you feed pharmacies if hypertension is afraid of the usual like fire...
Tabakov has revealed a unique remedy against hypertension! To reduce blood pressure while preserving blood vessels, add to…
Symptoms and photos
The disease begins acutely, with a high (39-40o) temperature and strong excitability, which manifests itself more clearly than in other febrile conditions. Patients often suffer from pain in small joints and the abdomen, and if left untreated, the fever can last a very long time, from one to several weeks.
Against the background of high temperature, the child develops damage to the mucous membranes, in particular, conjunctival hyperemia, which is not accompanied by pronounced exudative manifestations and resolves within 1-2 weeks.
In addition, from the first days of the disease, the patient experiences dryness and cracks in the lips, oral mucosa, as well as swelling of the tongue, and approximately in the second week of the development of the disease it acquires a crimson tint.
Soon after the onset of fever, a rash appears on the patient’s torso and groin, which can have several variants: irregularly shaped erythrematous plaques, scarlet-like rash, etc.
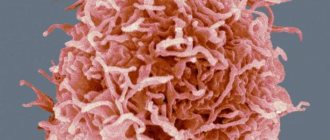
In these photos you will see the main symptoms of Kawasaki disease:
Subsequently, erythrema of the perineum, skin of the palms and feet occurs, accompanied by swelling, severe pain and limited mobility of the fingers. After some time, the rash fades and is replaced by peeling that spreads to the fingers, hands and feet.
Half of patients diagnosed with Kawasaki disease develop pathological changes in the cardiovascular system, manifested by arrhythmia, tachycardia and heart murmurs. The acute phase of the disease is often accompanied by changes in the membranes of the heart, which usually have positive dynamics and decrease as the child recovers.
Moreover, a characteristic feature of this vasculitis is that coronary artery aneurysms develop very quickly, literally within 1-4 weeks. In addition to the coronary arteries, the process can spread to other vessels: the abdominal aorta, axillary, brachial, subclavian, and renal arteries.
Diagnostics
The difficulty in diagnosing Kawasaki disease lies in the fact that it is quite a rare phenomenon (especially for European countries), so not every doctor can distinguish it from other childhood diseases: rubella, scarlet fever, chickenpox, etc.
The main criteria for diagnosis are 6 main signs (the patient must have at least 5 of them):
- fever that lasts at least 5 days;
- inflammation of the mucous membranes;
- erythrema of the palms and soles, accompanied by peeling of the fingers;
- conjunctival hyperemia;
- enlarged cervical lymph nodes;
- skin rash, which comes in different varieties.
When to see a doctor?
Since any childhood illness, including Kawasaki syndrome, is characterized by a very rapid, reactive course, any increase in temperature, accompanied by a rash and lesions of the mucous membrane, is a reason to immediately consult a doctor.
To exclude infectious diseases, the patient may need to consult an infectious disease specialist, and to confirm the diagnosis, prescribe adequate treatment and prevent cardiovascular complications, consult a rheumatologist and cardiologist.
Laboratory methods for diagnosing the disease include:
- General blood analysis. Patients may experience an increase in the number of leukocytes and an increase in ESR, thrombocytosis and normochromic anemia.
- Biochemical analysis. With lesions of the gallbladder and liver, transaminase activity often increases, as well as the level of direct bilirubin and urobilinogen.
- Immunological analysis. Kawasaki syndrome is characterized by increased levels of C-reactive protein.
- Analysis of urine. During the acute period of the disease, children experience slight microhematuria, proteinuria and sterile pyuria.
- ECG. If the pathological process extends to the cardiovascular system, the electrocardiogram shows a decrease in R wave voltage, ST segment depression and other abnormalities.
- EchoCG. This examination is carried out in the first or second week after the onset of the main symptoms, and if lesions of the coronary arteries are detected, every three months.
- Coronary angiography. Allows you to assess the condition of the arteries and identify not only aneurysms, but also stenoses of any departments.
For example, if the symptoms of suspected vasculitis are accompanied by the formation of vesicles, purpura or crusts, as well as nodules and arterial hypertension, then we are most likely not talking about Kawasaki syndrome in this case.
Treatment
The main goal of drug therapy is to protect the cardiovascular system from damage. The following drugs have a good effect:
- Immunoglobulin. The drug is administered intravenously once a day and allows the body to quickly cope with the disease by increasing passive immunity.
- Aspirin. Regular aspirin has a powerful anti-inflammatory effect and helps thin the blood, so it is widely used to treat Kawasaki disease.
- Anticoagulants. To prevent thrombosis, patients are prescribed anticoagulants, most often clopigel and warfarin.
Predictions and prevention
Most children diagnosed with Kawasaki syndrome recover completely after treatment, which means the prognosis for patients is rather favorable.
At the same time, we must not forget that the disease can lead to serious problems in the future, therefore, as a measure of secondary prevention, patients should be observed by a cardiologist for several years after recovery. Primary prevention measures for this pathology have not yet been developed.
Kawasaki syndrome, like any other form of systemic vasculitis in children, is indeed potentially life-threatening, but with parents' careful attention to the health of their child, it is possible not only to completely cure the disease, but also to prevent possible complications.
For more information about Kawasaki disease (syndrome), watch the video:
Clinical manifestations
Clinically, the disease is not expressed in any way, since the functions of leukocytes are not impaired. Leukocytes are also capable of phagocytosis of foreign cells and contain a set of enzymes identical to normal leukocytes. ESR is not increased, blood clotting is normal. Often this pathology is discovered by chance during a blood test. Due to the fact that there is a neutrophil shift to the left in the leukocyte formula, an infection can be mistakenly assumed. Reactions to blood loss, infection, etc. in people with this anomaly the reactions do not differ from healthy people.
The leukocyte formula is the ratio of several types of leukocytes in the human body
According to some sources, there may be changes in the skeletal system: hyperkyphosis, short stature, skeletal deformities.
Nurofen for high blood pressure: can you drink it?
It is known that not all medications are used by patients for their intended purpose. For example, Nurofen belongs to the group of non-steroidal anti-inflammatory drugs, and its direct purpose is to stop the inflammatory process, eliminate headaches and lower temperature.
But at the same time, Nurofen is often used by patients with high blood pressure as a remedy with a moderate hypotensive effect. Moreover, for headaches and migraines associated with high blood pressure, it is taken simultaneously with real antihypertensive drugs.
Is this acceptable, how does Nurofen actually work with high blood pressure - does it increase or decrease it? To understand this, you need to know the mechanism of action of this drug.
Composition and effect of the drug
Nurofen, whose international name is Ibuprofen, is a drug from the group of non-steroidal anti-inflammatory drugs. It is produced in various pharmacological forms:
- Pills;
- Effervescent soluble tablets;
- Capsules with liquid medicine inside;
- Suspension;
- Rectal suppositories;
- Gel for external use.
In all types of the drug, the main active component is ibuprofen. An exception is Nurofen Plus - in addition to ibuprofen, this drug also contains codeine, which enhances the analgesic effect of the main component.
Nurofen has anti-inflammatory, analgesic and antipyretic effects. It quickly reduces body temperature and relieves pain during any inflammatory processes in the body.
Ibuprofen has a suppressive effect on the synthesis of prostaglandins - substances that provoke the development of inflammation, cause pain and fever.
Nurofen begins to act as soon as it enters the digestive tract. From there it penetrates the bloodstream and remains effective for up to 8 hours.
Metabolization of the substance occurs in the liver, after which the drug is excreted along with urine and feces in the form of metabolites.
Indications and contraindications for the use of Nurofen
on
As an effective antipyretic and analgesic, Nurofen is prescribed in the following cases:
- Headaches and migraines;
- Diseases of the musculoskeletal system associated with inflammation in the joints and surrounding tissues;
- For any respiratory infections and colds;
- Toothache;
- Painful menstruation;
- Pinched or inflamed peripheral nerves;
- Pain in muscles and ligaments after injury or surgery.
Nurofen is truly a universal remedy that quickly reduces pain of any nature and origin, but we should not forget about the list of contraindications to the use of this drug.
First of all, this is hypersensitivity to the main component of the drug or other non-steroidal anti-inflammatory drugs. In addition, you should not take this medicine in the following cases:
- Bronchial or aspirin-induced asthma.
- Rhinitis with polypous growths in the nasal cavities.
- Reduced blood clotting.
- Peptic ulcers of the digestive system, gastritis and colitis.
- Kidney or liver failure.
- Pathologies of the circulatory system.
- Deficiency of leukocytes in the blood.
- Visual impairment, optic nerve diseases.
- Traumatic brain injuries, including intracranial hemorrhages.
- Hearing impairment, vestibular dysfunction.
- Hyperkalemia and some other metabolic disorders in the body.
- High blood pressure and heart failure.
So, the manufacturer itself states in the instructions for use of this drug that it is not suitable for the treatment of patients suffering from hypertension.
Ibuprofen, as the active ingredient in the drug, can really help with severe headaches, which often occur with hypertension.
But at the same time, it thins the blood and accelerates blood circulation, which, if the vascular lumen is insufficient, can lead to the most serious consequences. In addition, this drug has many side effects, primarily a toxic attack on the liver and kidneys, where it is metabolized.
Instructions for use of the drug
Nurofen tablets are prescribed depending on the diagnosis and condition of the patient in a dosage of 200 mg to 800 mg per day, divided into three to four doses. To enhance the effectiveness of the drug and reduce the aggressive effect on the digestive organs, it is recommended to take it during meals or no later than half an hour after it.
The duration of treatment may vary - for severe pain, sometimes a one-time dose of the drug is enough, in other cases the course of therapy with Nurofen lasts from five to ten days.
If the drug is used for external use, then it is applied to the skin of the affected, painful area, rubbing slightly, up to 4 times a day.
After the pain has decreased, it is enough to apply the gel twice a day, morning and evening. The course of treatment can last up to four weeks.
Side effects when using Nurofen
Even if the patient has no contraindications, when taking this drug, he should be prepared for the possible occurrence of the following side effects:
- From the digestive system: heartburn, nausea, vomiting, diarrhea, flatulence, cutting pain in the upper abdomen, discomfort in the otal cavity, drying out of the mucous membrane; with prolonged use, the formation of erosions on the mucous membrane of the esophagus and stomach is possible.
- From the central nervous system: headaches, dizziness, anxiety or depression, irritability, drowsiness and lethargy during the day, insomnia at night, sweating. Sometimes confusion, tinnitus, visual disturbances, hallucinations.
- From the liver and kidneys - hepatitis, pancreatitis, development of acute renal failure, pyelitis, inflammation of the bladder.
- From the circulatory system: anemia, thrombocytopenia, agranulocytosis, leukocytopenia.
- From the cardiovascular system: rapid heartbeat, increased blood pressure, unstable functioning of the heart muscle.
- From the respiratory system: bronchospasm, shortness of breath, asthma attacks (usually when using Nurofen plus containing codeine).
- If the drug is used for external use in the form of a gel, itching, burning, and redness of the skin may be felt at the site of application.
Usually, all these phenomena go away on their own after stopping taking Nurofen; in rare cases, symptomatic therapy is required. Urgent help is necessary if the drug was taken in an excessive dose or the patient did not know that he had an individual intolerance to the active substance ibuprofen.
In case of an overdose, symptoms such as vomiting and diarrhea, inhibition of reactions, severe abdominal pain and headaches, unstable heartbeat - accelerated or slowed down, drowsiness, breath holding, a sharp and severe drop in blood pressure, coma.
In this case, you need to provide the patient with first aid: rinse the stomach, give activated charcoal or milk, any diuretics. In case of severe intoxication, call an ambulance.
Drinking alcohol does not affect the effectiveness of this drug, but it is nevertheless recommended to avoid this combination to avoid increased side effects. When using Nurofen Plus, which contains codeine, simultaneous consumption of alcohol is strictly not recommended - unpredictable reactions of the body are possible.
The drug is available in pharmacies without a prescription; the price is determined depending on the form of the drug and the size of the package. The price for a package of 10 tablets is from 80 rubles, for a package of 20 tablets - from 150 rubles.
Gel for external use in a 50 mg tube costs from 170 rubles, the average price for the same product in a 100 mg package is 315 rubles.
Summary: Nurofen is contraindicated as an analgesic and antihypertensive drug for uncontrolled arterial hypertension; self-administration of this drug can lead to life-threatening complications for the patient. In the video in this article, a specialist will additionally talk about the properties of Nurofen.
on
Constitutional abnormalities of neutrophils
Pelger's anomaly of neutrophils
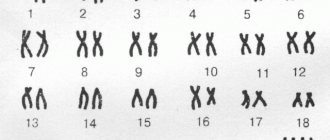
- a blood change inherited according to the dominant type. The peculiarity of the development of Pelger leukocytes is expressed mainly in the morphological change in the nuclei of neutrophils - a violation of the process of their segmentation (the nucleus is old, but its shape is young).
The structure of the nuclei of Pelger neutrophils is coarsely lumpy and pyknotic. Most Pelger neutrophils have a monolobed, unsegmented nucleus, similar in shape to rod cells, and also in the form of an ellipse, circle, bean or kidney, it is shorter than that of a regular neutrophil.
Less common are kernels with a visible constriction in the middle, resembling a gymnastic weight or a groundnut in shape.
From these two forms transitions to two-segment nuclei are observed; nuclei with three segments are very rare. Both bisegmental and trisegmental forms are distinguished by Pelger features - short bridges and lumpy structure of the nuclei.
There are neutrophils with round nuclei, resembling myelocytes in shape, but their special coarse and pyknotic structure does not allow these neutrophils to be classified as myelocytes.
Some Pelger neutrophils have large, abundant granularity, while in others it is small and scanty.
In the bone marrow, round-nuclear neutrophils predominate (up to 65%). Among them, mature cells with a round, oval or ellipsoidal nucleus are found. In the same way, the development of round-nuclear eosinophilic granulocytes characteristic of Pelger's anomaly occurs.
In order to avoid erroneous interpretation of the analysis in the presence of the indicated forms of neutrophil granulocytes, the CDL doctor is obliged to give a conclusion that the described blood picture is characteristic of Pelger’s leukocyte anomaly.
It is advisable in all cases to clarify the diagnosis of Pelger's anomaly in a patient, to examine the blood of the parents and, if they have corresponding changes, to inform them and the attending physician about this.
This will avoid the erroneous interpretation of the blood picture as a “left shift” of neutrophils and the incorrect behavior of the doctor in any disease of the carrier of the Pelger family anomaly.
Pelger neutrophils
in terms of their physiological properties - the ability to phagocytose, the content of enzymes, life expectancy in the circulating blood - they do not differ from normal, mature neutrophils. The reactions of carriers of the Pelger anomaly to infections, blood loss, etc. do not differ from the corresponding reactions in ordinary people.
Pelger's anomaly of neutrophils (photos)
Pelger-Huet anomaly. Classic pince-nez cell. Pelger-Huet cells which have no nuclear lobation. Pelger-Huet anomaly. Pelger-Huet anomaly heterozygous form.
Stoedmeister's leukocyte anomaly
- is of a family nature. It can be detected independently or in combination with Pelger anomaly.
The nuclei of Stodmeister cells are characterized by less pronounced chromatin condensation and a peculiar fringe, consisting of delicate chromatin threads, as if protruding from the main nuclear mass into the cytoplasm.
Stodmeister cells are fully mature forms of the neutrophil series. The phenomenon of nuclear segmentation is also observed in eosinophils and basophils and is absent in monocytes.
May-Hegglin anomaly
is a rare autosomal dominant disorder characterized by the presence of large pathological Dele bodies in granulocytes and monocytes. Thrombocytopenia is noted, some of the platelets are slightly granular and gigantic in size.
May-Heglin anomaly (micrographs):
May-Hegglin anomaly Dohle Bodies in the May-Hegglin Anomaly Dohle Bodies in the May-Hegglin Anomaly
Alder anomaly (Alder-Reilly anomaly)
– the cytoplasm contains numerous dark lilac granules consisting of acidic mucopolysaccharides. It is observed in genetic mucopolysaccharidosis of the Hurler, Gunter and Marote-Lamy type.
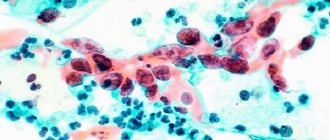
Chediak-Higashi syndrome
– a rare autosomal recessive disease, manifested by the presence of inclusions in leukocytes, partial hypopigmentation of the eyes and skin, and an increased tendency to bleeding.
The cytoplasm of neutrophils contains numerous large fused lysosomal granules, stained according to Romanovsky in a greenish-gray color. Some of them are gigantic in size and bizarre in shape.
They can also be contained in lymphocytes and other blood cells.
Chediak-Higashi syndrome (photomicrographs)
Neutrophil from a patient with Chediak-Higashi Syndrome. Chediak-Higashi syndrome Chediak-Higashi syndrome Lymphocyte inclusion in Chediak-Higashi syndrome
Hereditary giant neutrophilia
– rarely observed. It is an autosomal dominant disorder. 1-2% of segmented neutrophils are twice the normal size, the nuclei are hypersegmented.
Congenital anomaly of the formation of specific granules
– morphological abnormalities in neutrophils are manifested in the almost complete absence of specific granules and the presence of bilobed nuclei.
- L. V. Kozlovskaya, A. Yu. Nikolaev. A textbook on clinical laboratory research methods. Moscow, Medicine, 1985
- Fred J. Shiffman. “Patophysiology of blood.” Per. from English – M. – St. Petersburg: “Publishing house BINOM” – “Nevsky Dialect”, 2000
- Manual of clinical laboratory diagnostics. (Parts 1 – 2) Ed. prof. M. A. Bazarnova, Academician of the USSR Academy of Medical Sciences A. I. Vorobyov. Kyiv, “Vishcha school”, 1991
- Handbook of Clinical Laboratory Methods. Ed. E. A. Kost. Moscow “Medicine” 1975
Monoblast is the parent cell of the monocytic series. Size 12 – 20 microns. The nucleus is large, often round, delicately reticulate, light purple in color, containing 2–3 nucleoli. The cytoplasm of the monoblast is relatively small, without granularity, and colored in bluish tones.
Section: Hemocytology
Read
Degenerative changes in neutrophils occur under various pathological conditions (infections, exposure to chemicals, diseases of the hematopoietic apparatus, exposure to penetrating radiation, ingestion of radioactive substances, etc.) and can affect both the nucleus and the cytoplasm.
Section: Hemocytology
Read
The main place of formation of lymphocytes is the hematopoietic tissue of the spleen and lymph nodes. In the bone marrow and peripheral blood, only mature lymphocytes are normally found. With pathology, immature and atypical forms of lymphoid germ cells may appear in the bone marrow and peripheral blood.
Section: Hemocytology
Read
Counting the absolute number of myelokaryocytes and megakaryocytes with bone marrow dilution is not carried out in all laboratories, so bone marrow examination is often limited only to the examination of smears with myelogram counting. Myelogram – percentage of different myelokaryocytes.
Section: Hemocytology
Read
Pathological forms of erythrokaryocytes (erythroblasts and normoblasts) are observed in some pathological conditions (acute sepsis, aplastic anemia, acute leukemia, severe infectious diseases, after irradiation, etc.). The morphology of the nucleus and cytoplasm of cells at different stages of maturation changes.
Section: Hemocytology
Read
Source: https://www.clinlab.info/Hemocytology/Constitutional-neutrophil-anomalies-9
How does cardiomagnyl affect blood pressure?
Cardiomagnyl and blood pressure are not interrelated concepts, since the drug does not contain components that would affect blood pressure. Cardiomagnyl is part of a group of drugs used to prevent the formation of blood clots.
Purpose of the drug
The drug is also classified as a non-steroidal anti-inflammatory drug, since it has the ability to reduce body temperature, the severity of the inflammatory process and relieve mild pain.
The composition of the drug Cardiomagnyl includes aspirin, which prevents platelet aggregation, and magnesium hydroxide, which has an enveloping effect. Accordingly, it is obvious that neither component is used at high pressure.
Compared to regular acetylsalicylic acid, Cardiomagnyl has a smaller spectrum of negative effects on the human body.
In the modern world, acetylsalicylic acid is widely used by doctors to prevent blood clots, as it prevents the actual adhesion of platelets. If this process is started, the platelets will stick together and thereby form a blood clot, which can completely close the lumen of the blood vessel, which will end in disaster.
In most cases, blockage of a vessel ends in myocardial infarction or ischemic stroke, therefore, in order to prevent possible complications, the cardiologist prescribes Cardiomagnyl to most elderly patients.
Very often this remedy can be found in the treatment regimen for hypertension, since in such patients, blood stagnation is simultaneously detected in certain areas of the circulatory system. Most often, this pathology is observed in patients with coronary heart disease, as they develop atherosclerotic plaques that disrupt the flow of blood through the vessels to the heart.
In addition, with hypertension, blood flow in the brain is impaired, which can cause the development of a stroke. It is possible that migraine attacks may form due to a sharp expansion of the vascular bed against the background of blood stagnation and, as a result, severe headaches. It is for this reason that it is worth taking Cardiomagnyl for prevention.
Composition and action
Cardiomagnyl contains acetylsalicylic acid and magnesium hydroxide. In addition, there are auxiliary components that help form the tablet and deliver it to the desired part of the gastrointestinal tract: talc, potato and corn starch, microcrystalline cellulose, hypromelose, propylene glycol.
The tablet form of Cardiomagnyl is white and heart- or oval-shaped. This is determined by the dosage of the drug.
The main effect of the drug is inhibition of the enzymatic activity of cyclooxygenase. Aspirin prevents the clumping of blood cells - platelets, and inhibits the production of thromboxane A2, which promotes the clumping of these cells.
Absorption of one tablet occurs very quickly, namely, in a quarter of an hour. Enzymes that are in the stomach immediately hydrolyze the acid that enters the gastrointestinal tract, then it enters the bloodstream and partially into the liver.
Unlike other drugs based on acetylsalicylic acid, used for high blood pressure, Cardiomagnyl is able to inhibit the formation of thromboxanes and inflammatory mediators. In addition, it has a beneficial effect on the functioning of the bone marrow and activates the process of cellular respiration.
Indications
The attending physician prescribes Cardiomagnyl after diagnosing the following pathologies in the patient:
- history of myocardial infarction;
- conditions that precede a heart attack;
- unstable angina;
- for prophylactic purposes during vascular angioplasty;
- cerebrovascular diseases;
- thrombi and emboli in arteries and veins.
Cardiomagnyl, in addition, is used to prevent myocardial infarction and ischemic stroke. It is applicable for the prevention of coronary heart disease in patients with a history of the following predisposing factors:
- excess body weight;
- diabetes;
- hypertonic disease;
- persistent craving for alcoholic beverages and nicotine-containing products.
With extreme caution and under the supervision of a cardiologist, the drug is prescribed for malignant hypertension, namely, when blood pressure levels constantly exceed the threshold of 180/120 mm. rt. Art. In such a critical condition, it is very important to avoid bleeding and hemorrhage, because thrombocytosis decreases while taking the drug.
Contraindications to the use of Cardiomagnyl
For all medications, a list of pathologies and conditions for which they cannot be used has been developed, and Cardiomagnyl is no exception. Absolute contraindications include the following:
- peptic ulcer of the stomach and duodenum;
- predisposition to bleeding;
- hemophilia;
- hemorrhages in the membranes of the brain;
- lactation;
- renal failure;
- asthma;
- I-II trimester of pregnancy;
- age under 18 years;
- lack of potassium.
You can take this medication, but only under the dynamic supervision of a doctor, for high blood sugar, polyps in the nasal passages, gout and allergic conditions. But, if a person is at risk for a heart attack, regardless of concomitant pathologies, it is important to use Cardiomagnyl systematically.
There is no need to take medication if there is an excess of magnesium in the body, since it already contains magnesium hydroxide.
Diagnostics
Diagnosis is based on the examination of blood smears in hematology analyzers. The maturity of the nucleus, the state of chromatin (in abnormal ones it is dense), and the ratio of neutrophils in the blood are assessed. To clarify the diagnosis, you need to conduct a blood test from parents who have a similar blood formula. It should be differentiated from chronic myeloid leukemia, in which the number of young neutrophils increases, and the leukocyte formulas of both diseases are similar. In this case, a patient with Pelger anomaly will have characteristic mature bisegmented neutrophils in the blood, and the number of leukocytes and other formed elements will be normal.
In addition to the Pelger anomaly, which is congenital, there is an acquired form of neutrophil hyposegmentation. Occurs in acute and chronic myeloid leukemia, myxedema, malaria, influenza, tuberculosis, erythromyelosis, infections, systemic lupus erythematosus, Hodgkin's disease. Often occurs after chemotherapy and taking certain medications (for example, NSAIDs, sulfonamides). It differs from an anomaly in that it is a temporary condition.
Reduced leukocytes in the blood: symptoms
Leukopenia may not show any signs for a long time. Typically, symptoms arise due to the concomitant development of an infectious disease, which affects the decline in indicators.
In general, low white blood cells in the blood are accompanied by the following ailments:
- Slight increase in temperature;
- Chills;
- Weakness;
- Dizziness;
- Increased heart rate;
- Headache.
Symptoms develop gradually and worsen as immune functions decline. As a result, the patient increasingly suffers from colds and viral infections. Weakening of the body leads to exhaustion, which is noticeable even in appearance. Concomitant signs of abnormalities include enlarged tonsils.
Whatever the reasons for the disruption of the defense system, a sharp drop in leukocytes can lead to negative consequences. Many patients think that there is nothing wrong with the fact that they often suffer from infectious inflammation.
But in fact, the root cause is sometimes leukemia, a malignant cancer. If not diagnosed early, the advanced form can lead to death.
In other cases, the negative consequences of reduced leukocyte cells are viral hepatitis, AIDS and other infectious diseases that easily penetrate the weakened body and begin to slowly deplete the patient.
Signs of a decrease in leukocytes
Symptoms indicating that there are not enough white cells in the bloodstream are most often absent. But since the immune system is gradually depleted, then:
- the body begins to pick up infections one after another;
- weakness and low tolerance to stress appear;
- the temperature jumps to 38 degrees and above;
- Fever and chills are inevitable.
In the first few days of leukopenia:
- there are no inflammatory processes in the nasopharynx;
- no cough or wheezing;
- there may be an increase in the size and density of the tonsils, spleen and lymph nodes;
- there is a pronounced proliferation of opportunistic microflora, harmless to a healthy person. Fungal infection, herpes viruses, and cytomegalovirus are active.
All this is the result of intoxication, which the leukocytes did not eliminate in time, since their level is lower than necessary.
The danger is that with a significant decrease in the number of white cells, some ailments can quickly cover the entire body and create a real threat to life (septic shock).
Leukopenia is often caused by chemotherapy or radiation. After the sessions, characteristic signs associated with damage to the liver, spleen, intestinal tissue and bone marrow appear. These symptoms are:
- ulcerative stomatitis with death of affected tissues;
- swelling of the oral mucosa develops;
- constant diarrhea caused not by ingested food, but by necrotic processes in the intestines.