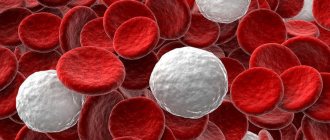
Cellular elements of blood (image obtained using a scanning electron microscope). Biconcave red blood cells and spherical white blood cells
with a rough surface
Leukocytes
(from ancient Greek λευκός - white and κύτος - container, body) - white blood cells; a heterogeneous group of human or animal blood cells of different appearance and functions, identified by the presence of a nucleus and the absence of independent coloring.
The main sphere of action of leukocytes is protection. They play a major role in the specific and nonspecific protection of the body from external and internal pathogenic agents, as well as in the implementation of typical pathological processes.
All types of leukocytes are capable of active movement and can pass through the capillary wall and penetrate into the intercellular space, where they absorb and digest foreign particles. This process is called phagocytosis, and the cells that carry it out are phagocytes.
If a lot of foreign bodies have entered the body, then the phagocytes, absorbing them, greatly increase in size and are eventually destroyed. This releases substances that cause a local inflammatory reaction, which is accompanied by swelling, fever and redness of the affected area.
Substances that cause an inflammatory reaction attract new leukocytes to the site of foreign body penetration. By destroying foreign bodies and damaged cells, leukocytes die in large quantities. Pus, which forms in tissues during inflammation, is an accumulation of dead leukocytes.
White blood cell count
The blood of an adult contains 1000 times fewer leukocytes than red blood cells, and on average their number is 4-9 109/. In newborn children, especially in the first days of life, the number of leukocytes can vary greatly from 9 to 30 109/. In children aged 1-3 years, the number of leukocytes in the blood ranges from 6.0-17.0 109/, and in 6-10 years - from 6.0-11.0 109/[1][2] .
The content of leukocytes in the blood is not constant, but changes dynamically depending on the time of day and the functional state of the body. Thus, the number of leukocytes usually increases slightly in the evening, after eating, as well as after physical and emotional stress.
An increase in the total absolute number of leukocytes per unit volume above the upper limit of normal is called absolute leukocytosis
, and its decrease below the lower limit is
absolute leukopenia
.
Leukocytosis
Main article: Leukocytosis
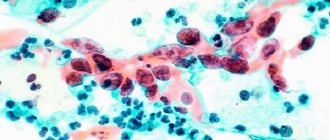
Neutrophil leukocyte engulfing anthrax cells (scanning electron microscope, pseudocolors)
True leukocytosis
occurs when the formation of leukocytes increases and their release from the bone marrow.
If the increase in the content of leukocytes in the blood is associated with the entry into circulation of those cells that are under normal conditions attached to the inner surface of the vessels, such leukocytosis is called redistributive
.
It is the redistribution of leukocytes that explains the fluctuations during the day. Thus, the number of leukocytes usually increases slightly in the evening, as well as after eating.
Physiological leukocytosis
observed in the premenstrual period, in the second half of pregnancy, 1-2 weeks after delivery.
Physiological redistributive leukocytosis can be observed after eating, after physical or emotional stress, exposure to cold or heat.
Leukocytosis as a pathological reaction most often indicates an infectious or aseptic inflammatory process in the body. In addition, leukocytosis is often detected in case of poisoning with nitrobenzene, aniline, in the initial phase of radiation sickness, as a side effect of certain medications, as well as in malignant neoplasms, acute blood loss and many other pathological processes. In its most severe form, leukocytosis occurs in leukemia.
Leukopenia
Main article: Leukopenia
Leukopenia can also be physiological (constitutional leukopenia) and pathological, redistributive and true.
Some causes of leukopenia:
- chronic infections: tuberculosis, HIV;
- hypersplenism syndrome;
- lymphogranulomatosis;
- aplastic bone marrow conditions;
- stress.
Types of main groups of leukocytes in the blood:
Of the five types of cells described above, some have their own important varieties. These varieties may be:
A) immature forms of cells
B) functional varieties of mature cells.
Now everything will become clearer.
Let's consider a group of neutrophils. They are distributed only by degree of maturity. According to this criterion, they are divided into: promyelocytes, myelocytes, metamyelocytes (young neutrophils), band neutrophils, segmented neutrophils. Only the last two types of cells are found in the blood, the rest are completely immature and are found in the bone marrow.
With lymphocytes, everything is somewhat more complicated; among them there are both “intermediate” maturing forms and different types of mature cells. A bone marrow stem cell that “decides” to become a lymphocyte first turns into a cell called a lymphopoiesis progenitor cell. That, in turn, divides and forms two daughter varieties: the predecessor of T-lymphopoiesis and the predecessor of B-lymphopoiesis.
Further from the first, several more generations of cells of different degrees of maturity occur: T-immunoblast, T-prolymphocyte, T-immunocyte, and in the end mature T-lymphocytes are formed, which are responsible for cellular immunity and directly destroy harmful particles that enter the body through direct contact.
The precursor to B-lymphopoiesis takes a slightly different route. From it originate the B-lymphoblast, B-prolymphocyte, plasmablast, proplasmocyte and, finally, the most mature forms: B-lymphocytes and plasmacytes. Their purpose is that these white blood cells in men, women and children are responsible for the production of antibodies and the formation of immune memory.
Types of leukocytes
Leukocytes is a collective concept introduced in the 19th century and retained for the sake of simplicity in contrasting “white blood - red blood”. According to modern data, leukocytes differ in origin, function and appearance. Some leukocytes are able to capture and digest foreign microorganisms (phagocytosis), while others can produce antibodies. As a result, there are several types of leukocyte division, the simplest of which is based on the presence/absence of specific granules in their cytoplasm. Based on morphological characteristics, leukocytes stained according to Romanovsky-Giemsa have been traditionally divided into two groups since the time of Ehrlich:
- granular leukocytes, or granulocytes
- cells that have large segmented nuclei and exhibit a specific granularity of the cytoplasm; depending on the ability to perceive dyes, they are divided into neutrophilic, eosinophilic and basophilic; - non-granular leukocytes, or agranulocytes
, are cells that do not have a specific granularity and contain a simple non-segmented nucleus, these include lymphocytes and monocytes.
The ratio of different types of white cells, expressed as a percentage, is called the leukocyte formula.
The study of the number and ratio of leukocytes is an important step in the diagnosis of diseases.
Eosinophils are leukocytes containing a bilobed nucleus and granules that stain red with eosin. They regulate allergic reactions, their number increases with allergies, as well as in cases of infection with parasitic worms (helminths).
Structure
All types of leukocytes have a different structure: they differ in size, staining method, content of inclusions in the cytoplasm, etc. But the main difference in structure, on the basis of which their classification is based, is the presence or absence of specific granularity in the cytoplasm - granules.
All leukocytes, based on the presence of granules in the cytoplasm, are divided into:
- Granulocytes - have granules in the cytoplasm (basophils, eosinophils, neutrophils)
- Agranulocytes - do not have granules (monocytes and lymphocytes).
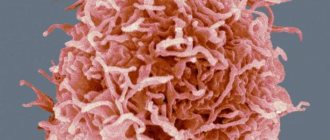
The structure of different leukocytes: agranulocytes and granulocytes
An important component of the blood system
White blood cells are an important component of the blood system, which also consists of red blood cells, platelets and plasma. Although they make up only about 1% of all blood, their impact is significant: they are essential for good health and protection against disease. We can say that these are immune cells. In a sense, they are constantly at war with viruses, bacteria and other “foreign invaders” that threaten your health.
When a specific area is attacked, white blood cells rush to destroy the harmful substance and prevent disease. White blood cells are produced within the bone marrow and stored in the blood and lymph tissues. Since the lifespan of human leukocytes is short, some types have a completely short lifespan - from one to three days. Therefore, the bone marrow is engaged in their constant reproduction.
Disorders and destruction of white blood cells
There are several pathological conditions that express a disorder of leukocytes. This is neutropenia - when the number of neutrophils in the body is very low. Also a disorder of white blood cells is an excessive number of neutrophils – neutrophil leukocytosis.
A low number of lymphocytes is called lymphocytopenia, and lymphocytic leukocytosis is a large number of lymphocytes. These two pathological conditions are also classified as leukocyte disorders.
The most common are disorders of leukocytes and neutrophils. Less – disorders of monocytes and eosinophils. A small percentage of the disorder is attributed to problems with basophils.
The life cycle of platelets, leukocytes and erythrocytes has been studied thoroughly. However, very little is said about their destruction. It has already been announced and proven that blood cells penetrate into the tissue structure after circulating in the blood. They do not return back to the blood. In tissues they perform their protective function and die.
Lifespan of white blood cells
What is the lifespan of leukocytes in the blood? We can say that white blood cells live fast and die young. They have a relatively short life cycle - from several days to several weeks. But this does not mean at all that they are fragile and unreliable. The power lies in numbers: one drop of blood can contain from 7 to 25 thousand white blood cells at the same time. This number may increase if a contagious infection is present.
The life of granulocytes after leaving the bone marrow is usually from 4 to 8 hours if they circulate in the blood, and from 4 to 5 days if they move through tissues. During severe infection, the total lifespan of white blood cells is often reduced to just a few hours. Lymphocytes enter the circulatory system constantly, along with drainage of lymph from lymph nodes and other lymphoid tissue. After a few hours, they move from the blood back into the tissue, then return to the lymph and thus circulate. The lifespan of leukocytes can vary from several weeks to several months, it all depends on the body’s need for these cells.
Types of granulocytes
Granulocytes include:
- Neutrophils,
- Basophils,
- Eosinophils.
All these blood cells are granulocytes, but they perform protective functions to varying degrees.
| Cells | Peculiarities | Functions |
| Basophils | Basophil cells are stained with basic dye, but not with acidic dye. Contain a large amount of heparin, histamine, serotonin, prostaglandin. The nucleus is fuzzy and consists of 2 segments. | The main function of basophilic elements is to create an immediate allergic reaction. Other granulocytes are attracted to the site of inflammation. Increases vascular permeability, blood and fluid flow. Example: anaphylactic shock. Other features: Heparin regulates blood clotting. They transfer Ig E and dissolve cells when interacting with an allergic agent. Degranulation of neutrophils leads to the release of histamine and the occurrence of an allergic reaction. The ability for phagocytosis is increased. |
| Eosinophils | They accept only acidic dye. The core consists of 2 segments. | Cytotoxic activity, that is, they eliminate parasites. They absorb histamine and also release it. They are able to inhibit the allergic reaction, but at the same time they can act as provocateurs. The percentage of phagocytosis is normally small: only small cells are able to absorb. |
| Neutrophils | The largest group. Dyed with basic and acidic dyes. Mature cells are polymorphonuclear, since the nucleus has up to 5 segments. Segmented neutrophils dominate in the bloodstream. Band granulocytes circulate less frequently in the blood. | Neutrophil cells are able to actively move outside the vessels to the site of damage. Neutralizes bacteria and fungi. Phagocytosis is carried out in a small volume. During inflammation, they absorb pathogenic elements and die, releasing bioactive substances. The latter help eliminate the infection and activate the process of arrival of immune defense cells to the site of damage. |