Purpose and parameters of OKA
A general blood test is carried out using a sample of capillary (finger) biofluid taken from the patient on an empty stomach. Hematological examination is prescribed:
- based on the patient’s symptomatic complaints for the primary diagnosis of the suspected disease;
- as part of routine medical examination, perinatal screening, preventive examination, etc.;
- to control the therapy;
- before hospitalization and sanatorium treatment;
- when preparing medical documents for employment, school, or preschool.
A referral for analysis is issued by a doctor (of any specialization) or the patient can donate blood on his own initiative for a fee. In the analysis form, the blood parameters being studied are written in Latin letters. White blood cells are designated WBC. The measured value is the number of cells in one liter of blood, multiplied by 10 to the 9th power (10^9/l).
| Index | Abbr. | Magnitude | Index | Abbr. | Magnitude |
| erythrocyte sedimentation rate (ESR) | ESR | mm/hour | leukocytes | WBC | 10^9/l |
| hemoglobin | NV | g/l | leukocyte formula (leukogram) | ||
| hematocrit | NST | % | neutrophils (band and segmented) | NEUT | % |
| red blood cells | R.B.C. | 10^12/l | lymphocytes | LYM | % |
| platelets | PLT | 10^9/l | monocytes | MON | % |
| reticulocytes | RET | PC. in ppm | eosinophils | EOS | % |
| basophils | BAS | % | |||
OKA does not apply to specific studies and does not diagnose a specific pathology. Unlike biochemical analysis, which reflects the degree of functionality of internal organs, its results indicate the state of the body as a whole.
Species classification of white blood cells
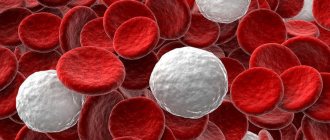
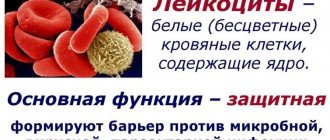
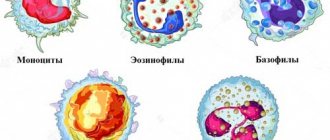
Leukocytes are white (colorless) blood cells, which are representatives of the formed elements of the cellular part of the biofluid, along with platelets and erythrocytes. Leukocyte cells are divided into two large groups:
- granulocytes (granular) – cells including monocytes and lymphocytes;
- agranulocytes (non-granular) – neutrophils (band and segmented), eosinophils and basophils.
All colorless blood cells are endowed with the function of protective phagocytosis - capturing and destroying (digesting) pathogenic microorganisms. When viruses, bacteria, fungal, protozoan and helminth parasites enter the body, white blood cells are mobilized in an effort to eliminate the threat. At the same time, their number increases sharply, which for hematological analysis is a marker of the inflammatory process, allergic reaction and other deviations from the norm.
Types of leukocytes and their functions in the body
Depending on the type of leukocyte cells, they are responsible for protecting the body from certain pathogens. Based on their abnormal number in a clinical blood test, a doctor can assume the presence of diseases.
- Lymphocytes. They are responsible for the immune system's response to invading pathogens, mainly viruses.
- Monocytes. Captures and absorbs bacteria and dead cell debris, cleansing the body for repair.
- Basophils. Provide an immune response to the penetration of allergens and parasites into the body.
- Eosinophils. Responsible for the elimination of protozoa, fungal parasites and helminths. Form antiparasitic immunity.
- Neutrophils. The most numerous group of leukocytes. They are divided into segmented - fully mature cells with a phagocytic function to bacteria and viruses. Band neutrophils are immature (young) neutrophils that help segmented neutrophils fight bacterial infections.
An increased level of band cells is determined in the analysis as a shift in the leukocyte formula to the left. An increase in the number of segmented cells shifts the leukogram to the right. Detailed parameters of granulocytes and agranulocytes are necessarily considered if the total number of leukocytes deviates from the norm.
What does a blood sugar test show?
Patients with diabetes undergo a blood test, regardless of the type of diabetes. A blood test allows you to assess the state of the body's metabolic systems and make a decision on treatment tactics for diabetics. The analysis evaluates indicators such as glucose in the blood plasma, as well as the percentage of glycated hemoglobin.
Glucose is the main and most necessary source of energy for all tissues of the human body, especially the brain. Normally, the analysis determines glucose in the range from 3 mmol/l to 6 mmol/l, which is the physiological values of glycemia. Glucose can be measured both in capillary blood, using a mini-glucometer, and in venous blood, using a stationary analyzer. The concentration of glucose in the plasma of capillary blood and venous blood may differ slightly; on average, fluctuations in the sugar level of 1 mmol/l are allowed.
Glucose levels are determined in a clinical laboratory using an automatic analyzer
Normal leukogram values
Indicators of leukocyte cells are differentiated by age. In children, leukocyte values are higher than in adults, which is due to the development of the immune system. The largest number of granulocytes and agranulocytes is recorded in a newborn child.
The composition of the blood and, accordingly, the number of cells in the leukocyte fractions changes in women during the period of bearing a child. At the beginning of the perinatal period, there should be no serious deviations.
The permissible norm is 6.8-7.4 (*10^9/l). In the second and third trimester, white blood cell production increases. This is explained by a change in hormonal status and the need to protect two organisms from viruses, bacteria and parasites at the same time.
For an objective assessment of white blood cells in the OKA, it is important to properly prepare for the study. The analysis is performed strictly on an empty stomach. The day before, it is necessary to cancel sports training and reduce other physical activities as much as possible. An increased leukocyte level is called leukocytosis, a decreased level is called leukopenia.
Interpretation of analyzes
Important. If a blood test shows a leukocyte content of more than 11 units*10^9/l, then we can conclude that there is some pathological abnormality in the body. A high concentration of white cells in itself is not considered a disease, it is just an indicator of a malfunction of the organs.
If there is an increased level of white blood cells, then the reason may be hidden in such phenomena as:
- Infectious pathologies. With the penetration of the pathogen into the body, the active work of the bone marrow begins. As a result, more white blood cells are produced than there should be. This happens so that the body can fight pathogenic bacteria. Infection often provokes the development of inflammation, which also leads to increased production of white blood cells.
- Smoking or lung disease. These factors create obstacles to the normal passage of air flow. Because of this, an inflammatory process in the lungs may develop, which will cause an increase in the number of leukocytes in a general blood test.
- Leukemia. This blood pathology is characterized by a constant high content of leukocytes in the patient’s body.
The level of white cells can also increase due to a malfunction of the immune system, severe stress, an allergic reaction, lymphocytic leukemia, myeloid leukemia, diseases of the digestive system, asthma and other pathologies.
In some cases, WBC levels may increase due to treatment with certain medications or exposure to physiological factors. For example, bearing a child, sports activities, the premenstrual period and many other phenomena not associated with pathologies can cause an increase in leukocytes.
Deviation from the normal indicator can be observed not only in the direction of increase, but also decrease. This may also indicate the development of certain diseases. Usually the decrease concerns neutrophils. At the same time, the person feels constant weakness, the immune system cannot cope with the bacteria attacking the body.
A low white blood cell count may indicate that the body has the following disorders:
- The bone marrow loses its ability to produce the required number of white blood cells, which are needed to fight infections.
- Diseases develop that adversely affect the production of white blood cells.
- A malignant neoplasm occurred that affected the bone marrow.
- There is toxic goiter, lupus or scleroderma.
- There is a deficiency of folic acid and other essential substances in the body.
- Tissue death has occurred.
- The patient became infected with AIDS, HIV infection.
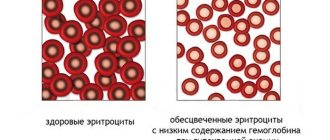
- Anemia develops due to a lack of iron in the body.
- Blood cells in the spleen are destroyed.
- There is a congenital pathology called Kostmann syndrome. It is characterized by a reduced content of neutrophils in the blood.
Just like an increase, a decrease in leukocytes in a blood test can be triggered by taking certain medications. For example, certain types of antibacterial agents, diuretics, and medications used in chemotherapy can inhibit the production of white cells or completely destroy them.
Reasons for deviations in analysis indicators
The number of leukocytes may change slightly under the influence of nutritional factors:
- Psycho-emotional stress or emotiogenic leukocytosis. In a stressful situation, the body's immune system weakens and the concentration of white blood cells drops.
- Intense physical activity – myogenic leukocytosis. After sports training and other physical activities, the amount of all formed elements in the blood increases.
- Eating before blood sampling – food leukocytosis. After eating, the number of white blood cells increases naturally, as the body's reaction to heat-treated food.
- Overheating and dehydration – anhydremic leukocytosis. When visiting a bathhouse (sauna), spending a long time in the sun, or working in hot workshops, leukocytes strive to protect the body from overheating, so their number will increase.
- Adrenaline injections. The body's reaction to the introduction of the hormone is post-adrenaline leukocytosis.
- Nicotine addiction. Toxins contained in tobacco smoke reduce the white cell count in the blood.
- Rehabilitation period after surgical interventions and viral infections. With a weakened immune system, there are not enough leukocytes in the blood.
- Unbalanced diet. Leukopenia develops against the background of a deficiency of B vitamins.
Results below normal
When the concentration of glucose in the blood falls below physiological values, this condition is called hypoglycemia. It is accompanied by characteristic symptoms. A person is worried about a feeling of weakness, drowsiness and hunger. Reasons for low glucose levels may include:
- fasting or lack of carbohydrate foods;
- incorrect dose of insulin;
- hypersecretion of own insulin;
- strong physical activity;
- neurohumoral diseases;
- liver damage.
All these conditions can lead to either a sharp decrease in sugar or a gradual decrease, which can be easily missed due to the absence of pronounced symptoms.
Types of leukocytosis and leukopenia
An increase in the concentration of certain types of leukocyte cells more specifically indicates the possible development of a particular pathology in the body.
Neutrophilia and neutropenia
Neutrophilia (neutrophilia) - a high level of neutrophilic leukocytes accompanies local or generalized infections caused by various types of bacteria:
- infection with Koch's bacillus (pulmonary tuberculosis, kidney tuberculosis);
- acute pneumonia;
- infections of the skin and oropharynx caused by streptococci and streptococci;
- acute bacterial intestinal infections;
- purulent processes in muscles, bones, subcutaneous tissue, epidermis;
- appendicitis and peritonitis.
In addition, high neutrophilic leukocytosis is characterized by necrotic conditions of internal organs (infarction, pancreatic necrosis, disintegration of a cancerous tumor, etc.). Chronically elevated rates of stabs indicate the development of oncological pathologies of internal organs, blood, and diabetic crisis.
The level of segmented cells increases with renal decompensation and depletion of the resources of the hematopoietic organs, in particular the bone marrow. Neutropenia (decreased neutrophil levels) is characteristic of the following pathological conditions:
- intensive destruction of neutrophilic leukocytes;
- infections: parasitic (worms), viral, bacterial, zoonotic (brucellosis, typhoid fever);
- clinical and hematological syndrome – agranulocytosis.
There are not enough neutrophils after a course of chemotherapy and radiation exposure (radiation sickness).
Lymphocytosis and lymphopenia
Lymphocytosis (lymphocytophilia) - an increased content of lymphocytes accompanies injuries to soft tissues and bones, burns, infection with various viruses, the condition after splenectomy (surgical removal of the spleen), cyanocobalamin deficiency, lymphocytic leukemia. Low lymphocytes or lymphopenia are characteristic of lymphogranulomatosis (Hodgkin's disease).
Monocytosis and monocytopenia
A high concentration of monocytes (monocytosis) is recorded in infectious diseases:
- herpesovirus type 5;
- tuberculosis of the kidneys and lungs;
- zoonotic infections;
- helminthic infestations;
- syphilis.
Monocytosis develops against the background of sarcoidosis (pulmonary pathology), oncohematological diseases (cancer of the blood and lymphatic system). Monocytopenia (low level) is determined in the presence of staphylococcal and streptococcal infections.
Eosinophilia and eosinopenia
Eosinophilic leukocytes respond to the penetration of allergens and parasites. Eosinophilia (high cell count) accompanies:
- accelerated allergic reactions (anaphylactic shock, Quincke's edema, etc.);
- helminthic infestations (ascariasis, enterobiasis, giardiasis, etc.);
- bronchial asthma;
- eosinophilic gastritis.
Few eosinophils in the blood (eosinopenia) occur during acute or chronic purulent processes.
Basophilia and basopenia
Basophilic leukocytosis indicates the presence of oncohematological diseases, radiation sickness, and acute autoimmune pathologies. Basopenia (low decrease in basophilic leukocytes) has no diagnostic value.
Consequences and complications of sugar abnormalities
A deviation in blood sugar levels in either one direction or the other can lead to the development of severe consequences and complications, which most often become chronic and require constant treatment.
Hyperglycemia is characterized by chronic hypoxia of body tissues (low oxygen content in the body or individual organs and tissues), as a result of which degenerative changes in organs develop.
Dystrophic changes are considered: myocardial dystrophy, liver and kidney failure, diabetic angiopathy - damage to the walls of blood vessels, diabetic polyneuropathy - damage to the sheaths of nerve fibers, encephalopathy - damage to the brain, retinopathy - damage to the retina, loss of vision.
As a result of the above changes, diseases such as vascular atherosclerosis develop, leading to stroke and heart attack, ulcerative-necrotic changes appear on the extremities, often ending in gangrene. Also, as a result of hypoxia, blood thickening develops and the likelihood of developing thrombosis and thromboembolism increases in the vessels of the extremities and internal organs (lungs, brain, abdominal cavity, kidneys).
Hypoglycemia is dangerous due to the failure of vital organs due to a decrease in metabolic cellular processes.
The brain needs glucose most of all, therefore, if there is a lack of it, its functions are disrupted, encephalopathy develops, and at a level of 2 mmol/l and below, cerebral coma develops.
Vision also suffers due to retinal atrophy, blood circulation in the legs and peripheral innervation are disrupted. With a systematic decrease in sugar levels, literally all organs and systems are affected, and often these changes are irreversible.
What are leukocytes and leukocyte formula: standard of analysis, interpretation of values in adults and children
The indicators of leukocytes (white blood cells) in the results of a general blood test are perhaps of the greatest interest to the doctor, as the most important biological marker in making a diagnosis.
Unlike red cells and erythrocytes, white blood cells occupy a small percentage of the cellular composition of the blood, but they are distinguished by greater mobility, the ability to leak through capillaries and go beyond the blood vessels, which allows them to exhibit their phagocytic activity. The following material will tell you what it is and what function blood leukocytes perform.
Conducting research
Blood is taken from a finger in the laboratory, after which it is studied and the result is deciphered. In order for the information to be reliable, it is necessary to adhere to simple rules for preparing for the study. These include the following recommendations:
- You should not smoke at least 2 hours before the procedure, because nicotine and tar cause spasm of blood vessels. Because of this, the amount of blood in the fingertip is significantly reduced, making analysis difficult.
- Three days before the test date, you should not drink alcoholic beverages or fatty foods. These substances can increase some blood parameters, which will distort the real state of the body.
- You should stop using drugs that affect blood clotting a couple of days before visiting the laboratory.
- You cannot donate blood if a person suffers from a viral pathology and within a week after recovery. This is explained by the fact that pathogenic microorganisms are able to change the composition of the blood.
Important. The attending physician will tell you what preparatory measures should be taken. He may recommend some other rules if, in addition to a blood test, additional diagnostic methods are planned.
What are white cells and what are they responsible for?
The cellular composition of blood is represented by three types of cells:
- erythrocytes, occupying 99% of the composition;
- leukocytes;
- platelets - colorless blood platelets, nuclear-free elements of blood.
Briefly, the functions of these cells can be described as a clear distribution of responsibilities - red blood cells are responsible for transporting oxygen to tissues, platelets regulate blood clotting, leukocytes perform a protective function, that is, they provide immune control.
Let's consider the ability of leukocytes to leak into the intercellular space during the process of suppuration of a splinter.
- Leukocytes flock to the site of insertion of a foreign body (splinter).
- The process of phagocytosis begins - part of the leukocytes, called phagocytes, absorbs and transforms particles of foreign material, increasing in size.
- An attempt to utilize a pathogenic agent by leukocytes is accompanied by an inflammatory process with redness, hyperthermia and swelling of the site of its penetration.
- An excessive increase in the size of phagocytes leads to their death, resulting in the formation of pus - a mass consisting of destroyed leukocytes.
- As a result, an even greater number of leukocytes are attracted to the site of injury to utilize both particles of external irritant and dead white cells, which is why the amount of pus - dead phagocytes - increases.
The activity of leukocytes in this case will be stopped only if the splinter is removed. In other cases, phagocytosis does not stop until the source of inflammation is completely eliminated.
The norm of leukocytes in a healthy person
To ensure a protective function, leukocytes must be contained in the blood in sufficient quantities, called the norm, or reference value. These values have some differences in different groups of patients.
Among women
For adults, regardless of gender, the following reference values for leukocyte concentration in absolute units (*10⁹) have been established:
- lower limit – 4*10⁹/l;
- upper limit – 9*10⁹/l.
Some laboratories set different limits for the normal white blood cell count, but the generally accepted guideline is 4-9 absolute units.
To find out your leukocyte level, just donate blood from your finger.
In men
Gender does not affect how many white blood cells a healthy adult should have. Therefore, reference values for men are within the same framework - from 4 to 9*10⁹/l. It has been noted that in 95% of healthy people the level of leukocytes corresponds to the accepted reference values. The rest have deviations not caused by pathological factors; they are considered an individual norm, which is often a hereditary feature of the body.
In children
The norm of leukocytes in the blood of young patients is related to how old the child is:
- up to 1 year – 6.5 – 12.5*10⁹/l;
- 1-3 years – 5-12*10⁹/l;
- 3-6 years – 4.5-10*10⁹/l;
- 6-16 years – 4.3-9.5*10⁹/l.
Despite the relative small number of this group of blood cells, several fractions of leukocytes are distinguished, each of which is responsible for something and performs a certain function. The picture of the percentage of different fractions of leukocytes is reflected by the leukocyte formula.
Designation, norm and increased standard indicators
The norm of eosinophils in men and women does not differ significantly, but the age of the patient plays an important role. In children from birth to one year, the rates range from 1 to 6%; by the age of two, the upper limit increases slightly (to 7%), and then by the age of 18 it decreases to 5%, as in adults.
The number of eosinophils is not a constant value; under the influence of various factors, it can change during the day. These indicators are influenced by the work of the adrenal glands (especially during sleep). The highest percentage of these cells is observed after midnight to mid-night, with a 20% decrease occurring during the morning and evening hours. In this regard, it is most rational to take a blood test for eosinophils in the morning, otherwise the indicators will not be objective.
If the transcript of the analysis shows an increased number of eosinophils, then you need to look for the cause of this pathology.
Leukocyte formula and its decoding in adults
The types of leukocytes are presented in fractions, the reference values of which are indicated in the table below. During the deciphering of the general blood test (CBC), the patient’s leukocyte formula is compared with reference values, since deviations of fractional indicators from the norm have important diagnostic significance.
Table. Normal leukocyte formula values for deciphering CBC in adults
| Factions | Content percentage |
| Basophils | 0 – 1 |
| Lymphocytes | 19 – 37 |
| Monocytes | 3 – 11 |
| Band neutrophils | 1 – 6 |
| Segmented neutrophils | 47 – 72 |
| Eosinophils | 0,5 — 5 |
The table shows that the smallest fraction of leukocytes are basophils - rare immune cells involved in triggering delayed reactions in the form of inflammatory processes. Normally, they should not be detected or should be observed in the blood in minimal quantities. If the indicator exceeds the norm by any amount, this is regarded as the likelihood of developing pathologies:
- ulcerative colitis;
- hemolytic anemia;
- Hodgkin's disease;
- nephrosis;
- chicken pox;
- deficiency of thyroid hormones and others.
An increase in basophil levels is often provoked by hormonal therapy (for example, estrogen medications or those that reduce the activity of the thyroid gland).
Lymphocytes are the second largest fraction of leukocytes after segmented neutrophils. This group is the main “weapon” of the immune system and has at its disposal pathogen-detecting cells, killer and helper cells and other interesting factions.
The state of a reduced concentration of lymphocytes in the leukocyte formula is called lymphopenia, and an increased content of these cells is called lymphocytosis. The reasons for the development of these conditions are varied.
Eozonophilic leukocytosis under a microscope
Monocytes are the largest and most active phagocytes in the blood of peripheral vessels and have an increased ability to intracellularly digest pathogenic macromolecules. A reduced level of these leukocytes in the blood is called monocytopenia, an increased level is called monocytosis.
Neutrophils are the most numerous group of leukocytes circulating in the blood. Mature neutrophils have a full-fledged segmented nucleus, for which they are called segmented. In functionally immature neutrophils, the nuclei lack segmentation and have the shape of an oblong rod, for which they are called band-nucleus. Mature neutrophils are active participants in phagocytosis, accompanied by the death of “spent” leukocytes. A decrease in this fraction in the blood is called neutropenia, an increase in concentration is called neutrophilic leukocytosis (or neutrophilosis).
Eosinophils are a small fraction of leukocytes, which generally do not remain in the blood, but reside in the tissues. The severe condition of the postoperative patient is determined by the reduced level of eosinophils (eosinopenia) in a general blood test with leukocyte formula.
Eosinophilia (increased concentration of these leukocytes) is characteristic of connective tissue diseases, parasitic infestations, immunodeficiency, tumor and allergic conditions, including bronchial asthma.
Eosinophils
Eosinophils (designated EO) are the second type of cells of the leukocyte series, which are continuously formed in the human bone marrow. After maturation, they leave the bone marrow and move through the circulatory system into tissues, where they destroy proteins foreign to the body.
If an indicator of this type is elevated (has the corresponding designation of leukocytes in a blood test), then this indicates that the body is actively fighting harmful microorganisms that have entered the blood. A decrease in the level of eosinophils in the blood is observed during the course of acute infectious diseases. If, after a long absence from analysis, they begin to appear again, this means that the person is beginning to recover.
Basophils (designated BASO) are the smallest type of leukocytes. But despite this, basophils play an important role when an allergen enters the body. When an allergen is identified, the basophil begins to destroy it by releasing biologically active substances in the blood. When allergic reactions occur, the indicator of this type is increased, which is reflected in the general blood test (we have already mentioned the designation of leukocytes of this type). This phenomenon is also typical for the onset of ovulation or the menstrual cycle in women.
Monocytes (designated MONO) are considered the largest form of white blood cells. Their main function is to work together with neutrophils to fight foreign pathogens. But due to their large size, monocytes take a little longer than neutrophils to destroy harmful organisms. An increased concentration of monocytes in the blood indicates the presence of infectious mononucleosis. A reduced level of this type of leukocyte series is a sign of severe inflammatory and infectious diseases, as well as various bone marrow lesions.
Lymphocytes (designated LYMPH) are the most active form of leukocytes involved in building the immune system. They are formed in the bone marrow and spleen, and then move to the lymph and blood, where they recognize antigens of a foreign organism that they have not encountered before. This special quality of lymphocytes makes it possible to create so-called immunity to previously suffered diseases. In turn, lymphocytes are divided into three types:
- T lymphocytes: responsible for cellular immunity;
- B lymphocytes: provide the formation of antibodies;
- NK lymphocytes: destroy their own cells if markers of infection are detected on the surface.
How are they designated as part of a general analysis?
To independently understand the blood test, you should find out how leukocytes and their fractions are designated in the analysis results. For designations in the results of clinical studies, abbreviations in Latin letters are used:
- WBC - this is the designation for the totality of fractions of leukocytes, or white blood cells, hence the abbreviation - white blood cells;
- BA - the abbreviation means that these are basophil leukocytes;
- LUM – lymphocytes;
- MON – monocytes;
- NEUT – neutrophils;
- EO – eosinophils.
Next to these symbols in the analysis document there is usually a % symbol, indicating that the data is presented in relative terms.
Why is the level increased?
The ability to understand abbreviations, of course, is not enough to make an independent diagnosis, since there are extremely many reasons for the increase in the concentration of leukocytes in the blood. When determining the exact cause, the doctor relies not only on the analysis data, but also on the symptomatic picture and medical history of the patient. List of possible provoking factors for increasing the concentration of leukocytes in the blood:
- bacterial, viral, fungal infections;
- purulent processes, sepsis;
- acute inflammation;
- injuries;
- last trimester of pregnancy;
- postpartum (lactation) period in women;
- myocardial infarction.
Leukocytosis is also characteristic of the clinical picture of malignant neoplasms.
Reasons for low content
Leukopenia can be caused by various pathological conditions:
- Addison-Beermer disease;
- aplasia or hypoplasia of the bone marrow;
- immunodeficiency and tumor diseases;
- diseases of the spleen;
- pernicious anemia;
- damage to bone marrow tissue by certain drugs or chemicals.
When treating with certain medications, it is necessary to monitor the leukocyte count at least once every 2 months and promptly respond to deviations. Medicines that lower white blood cell counts include antispasmodic and antiepileptic drugs, thyreostatics, NSAIDs and some antibiotics.
What do low scores mean?
It happens that tests show low eosinophils.
This is the first sign of exhaustion of the body due to various reasons:
- stress;
- injuries;
- pathologies of bone marrow;
- burns;
- infection (initial stage of the disease);
- blood poisoning.
When a patient takes anticancer drugs, it creates a problem for the bone marrow. It cannot form white blood cells, so the concentration of eosinophils decreases. This also happens when the body experiences physical stress.
In the postoperative period, testing for eosinophils also shows their low level. However, this indicator alone cannot help accurately determine a specific disease, so in this case a full examination is necessary.
The concentration of eosinophilic cationic protein allows us to assess the severity of allergic skin diseases.
A blood test for eosinophils is an important component in the diagnosis of serious diseases.
How to increase the quantity?
A sharp drop in the number of leukocytes can be a consequence of radiation or chemotherapy, as well as serious illnesses. Leukopenia requires taking comprehensive measures to restore the number of leukocytes to the level that should be normal. This means following a special diet, using medications that stimulate leukopoiesis (production of white blood cells) and using folk remedies agreed with a doctor. For this purpose, decoctions and infusions are usually used:
The therapeutic diet for leukopenia is based on a diet rich in vitamins and amino acids. The most useful are folic acid (B9) and ascorbic acid (vitamin C). Preference in the menu should be given to vegetables, berries and fruits, greens, green beans. The consumption of products containing gold, aluminum and cobalt should be avoided, and the amount of by-products (kidneys, liver, etc.) should be kept to a minimum.