Features of adhesion
Platelets are the smallest cells in the human body that protect it from serious blood loss.
During the aggregation process, they stick together. This is the initial stage of thrombus formation. Next, it grows due to an increase in cells that are attached to the wall of the damaged vessel. A clot forms and blocks blood flow. The rate of platelet adhesion is an important indicator for human life. This process is influenced by numerous factors. For example, aggregation, in which blood cells stick together. But this phenomenon can play both a positive and negative role for the human body.
Every person should know what platelet adhesion is. The process involves the formation of a blood clot, which is necessary to prevent severe bleeding and save a person from death.
Insufficient production of these cells leads to the fact that the adhesion process is minimal and there is not enough blood substance to form a blood clot. If blood cells are produced in insufficient quantities, pathological processes occur.
An increased number of cells leads to the patient developing thrombosis and embolism. Pathological processes occur in any part of the body or in internal organs. Especially where the network of blood vessels is located quite densely.
This is explained by the fact that a high concentration of platelets increases the size of the clot. It breaks off and begins to move through the circulatory system. These are serious violations, since a clot entering the heart causes myocardial infarction. Most often, after such an event, a person dies.
Pneumonia pain in the chest, back, under the shoulder blade and migraine
How to understand the results?
An assay using three common inducers and adding new ones if required is done if one clotting factor predominates over the others. For diagnosis, the detected altered norm with one inductor in the absence of movement with the others is important. And the results are assessed by a specialist.
Here are the factors that can trigger a drop in aggregation:
- success of antiplatelet treatment;
- thrombocytopathy.
What can thrombocytopathy do?
This type of disease can be inherited from parents or acquired after suffering from certain diseases. According to statistics, every tenth person has this. What is common to such diseases is the presence of a connection with the ability of platelets to accumulate certain substances.
Because of this, the bleeding does not stop and blood clots do not form. This is fraught with the fact that the slightest scratch can cause severe external bleeding, and a bruise can lead to internal bleeding.
Thrombocytopathy is a serious disease characterized by decreased platelet aggregation
This is already noticeable in a child: such children often have bleeding gums, bleeding from the nose, bruises appear on the body from the slightest slap, and as soon as the child hits something with his knee or elbow, the place swells. Teenage girls suffering from this pathology have protracted periods, and a lot of blood is lost during them. As a result, anemia develops.
Secondary thrombocytopathies
Symptomatic, or secondary, thrombocytopathies are formed due to the following pathologies:
- chronic leukemia;
- multiple myeloma;
- pernicious anemia;
- the last stage of development of uremia;
- thyroid dysfunction.
If a patient's bleeding is too severe during surgery, the surgeon can be sure that he has thrombocytopathy.
With thrombocytopathy, it is extremely difficult to stop bleeding
Aggregation also becomes higher in the following cases:
- widespread vascular atherosclerosis;
- hypertension;
- rupture of internal organs;
- thrombosis of arteries in the abdominal cavity;
- stroke;
- diabetes.
Diagnostic methods
Platelet adhesion testing should be performed regularly. To avoid serious consequences and save your life, a person should visit doctors and undergo medical examinations. First of all, you need to donate blood for analysis. The test allows you to determine the number of platelets and compare it with acceptable standards.
Normal values range from 180–400 thousand cells per 1 ml of blood. If the parameters are too high or low, you need to go to the doctor so that he can prescribe effective treatment. You need to take test results with you from any specialized laboratory, for example, Invitro. The goal of therapeutic methods is to stabilize the level of platelets in the blood.
Medicine provides various diagnostic methods for determining coagulation parameters. The most accurate are global and local tests.
Adhesion
When the vessel wall is damaged, the collagen of the basal membrane is exposed and a foreign “thrombogenic” contact surface is created; at the same time, adhesion proteins, primarily von Willebrand factor, are released from the activated endothelium. The contact surface adheres to platelets and initiates the coagulation process.
The adhesion process involves the attachment of platelets caught in the damaged area to subendothelial structures. In this case, direct contact of platelets and collagen of the basement membrane occurs through platelet receptors GPIa/IIa. At the same time, von Willebrand f. isolated from damaged endothelial cells binds one part to the platelet receptor GPIb, and the other to subendothelial collagen.
Activation
Adhesion of platelets to collagen (GPIa/IIa receptors) and interaction with von Willebrand factor (GPIb receptor) leads to their activation.
The binding of von Willebrand factor to the GPIb receptor triggers the phospholipid-calcium signal transduction mechanism, which ultimately leads to an increase in the intracellular concentration of Ca2+ ions and activation of protein kinase C. As a result:
- ATP-dependent aminophospholipid translocase, which maintains membrane asymmetry of phospholipids, is inhibited and, as a result, negatively charged phosphatidylserine appears on the outer surface of the membrane.
- together with phosphatidylserine, a special glycoprotein (tissue factor) comes to the surface and the membrane becomes a surface for the interaction of plasma coagulation factors. This surface is called platelet thromboplastin.
- thrombostenin protein is reduced, as a result degranulation occurs and factors that activate adhesion and aggregation are released,
- the shape of the platelet changes, pseudopodia appear, and it spreads out on the contact surface,
- Phospholipase A2 is activated, which splits off polyunsaturated (for example, arachidonic) acid from the membrane phosphatidylcholine and from it thromboxane A (for example, thromboxane A2) is synthesized, a strong inducer of platelet aggregation and a vasoconstrictor. Thromboxane counteracts the influence of prostacyclins and accelerates the release of active substances (prothrombin, PAF, ADP, Ca2+ ions, serotonin, thromboxane A, etc.) from the activated platelet, which supports and enhances the activation of this and neighboring platelets.
Activation is also enhanced by the action of ADP, released from damaged erythrocytes and endothelial cells of the vascular wall.
Activated platelets have receptors on their surface for active and inactive factors V, VIII, IX, X, XI, prothrombin and thrombin.
Adhesion mechanism
When blood vessels are damaged, the receptors transmit a nerve impulse indicating the need to form a blood clot. This leads to platelet activation. It may be reversible or irreversible.
With reversible activation, platelets interact with fibrinogen, with irreversible activation - with thrombospondin.
Activators in the blood of a healthy person are Epinephrine, Serotonin, Thrombin, Vasopressin, ADP, Plasmin, TXA2, RAF, PGN2, von Willebrand factor. In a damaged vessel, collagen, von Willebrand factor, and microfibrils around elastin act as activators.
Due to activation, platelets change their shape, which leads to an increase in their area. On the cell membrane, the ratio of phospholipids changes; on the outside, acidic phospholipids predominate. Platelets stick together and then attach to the subendothelium.
The following factors contribute to this:
- increased blood viscosity;
- decreased blood flow speed;
- red blood cell aggregation;
- the presence of highly dispersed proteins and lipids in the blood plasma.
Platelet aggregation is facilitated by the protein thrombostenin, due to which these blood cells change their shape, getting as close to each other as possible. Such clots are very dense. They are strengthened by fibrin threads that form when the walls of blood vessels are damaged.
If platelets are exposed to a weak stimulus, reversible aggregation occurs. Its peculiarity is that after some time the platelet returns to its normal state.
If necessary, it can be activated again. Prolonged stimulation causes irreversible aggregation, when the clot becomes tightly attached to other cells and structures. Having entered the bloodstream in this state, the platelet is excreted from the body.
However, aggregation is not sufficient to retain clots in the bloodstream because the blood flow rate is very high. The blood clot is retained due to von Willebrand factor. It connects receptors to collagen in the walls of blood vessels.
The final phase of thrombus formation is thrombus retraction. At this stage, it is compacted and secured in the vessel.
If retraction is impaired, the clot quickly breaks down and then travels to various parts of the body, where it disrupts blood circulation. The consequence of this is embolism.
In the veins, thrombus formation occurs faster, since the speed of blood flow here is much lower than in the arteries.
Platelet adhesion
What the analysis shows
The study of the speed and quality of aggregation is used to diagnose several pathological processes:
- Thrombocytopathy. In this disorder, the number of formed cells is normal, but the functional state suffers. Simply put, the speed and quality of aggregation becomes significantly lower. Coagulopathy is observed. It is impossible to detect a disorder using testing alone. Additional tests are required to verify the diagnosis.
- Thrombocytopenia. Reverse state. With it, the number of formed cells decreases, but functional indicators remain normal. Detecting this pathological process is relatively simple. Since even standard laboratory methods detect changes in the number of formed cells.
- Thrombasthenia. It's Glanzmann's disease. Develops as a result of a chromosomal disorder. Refers to relatively rare pathological processes. It is inherited from parents to children. Other generations in the ascending line also participate. As a result of the disorder, platelets lose a special receptor that is located on the membrane. The outer shell of the cell. The result is insufficient sensitivity to fibrin and some proteins. Consequently, aggregation becomes incomplete and stops at the third stage. On the development of a loose plug.
- Vasculitis. Inflammatory processes affecting blood vessels. The pathology is accompanied by changes in arteries, veins, small capillaries and other structures. Platelet disorders develop somewhat later. To detect the disorder, a special test is needed. A modification of the standard analysis is an aggregogram.
- Von Willebrand's disease. Complex hereditary disease. Accompanied by spontaneous but intense bleeding without a clear etiology. Apparently, there is a combination of platelet dysfunction with a change in the synthesis of coagulation factors. Scientists cannot yet say more precisely. The pathological process is detected by a special test, a blood test.
In simple words, with the help of research it is possible to detect platelet disorders: the functioning of the formed cells and their structure.
This is only part of the finds. Of course, it is often impossible to talk about a pathological process based on analysis alone. It is necessary to take into account several factors and the results of other objective studies.
The question of decoding falls on the shoulders of a hematology specialist.
Causes of impaired platelet adhesion
Adhesion disorders are an increase or decrease in the formation of blood clots.
Adhesion is disrupted for the following reasons:
- heredity;
- lack of calcium;
- taking certain medications;
- lack of glycoprotein;
- von Willebrand factor deficiency.
Adhesion directly depends on the number of platelets. If there is an excess in the blood, a person is prone to the formation of blood clots. Such clots break away from the walls and can then travel through the bloodstream to any organ, causing ischemia.
An increased tendency to adhesion is observed in pregnant women, patients with diabetes mellitus, hypertension, atherosclerosis, angina pectoris, and patients with oncology. This is due to excessive production of thromboxane A2.
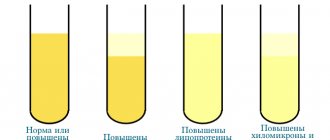
Adhesion is closely related to aggregation (sticking of platelets together). Platelets are more prone to aggregation when the concentration of adrenaline, free fatty acids, and low-density lipoproteins in the blood increases. Pathology can also be caused by a lack of prostacyclin.
When should you get tested?
Indications for the study are:
- excessive bleeding gums;
- nosebleeds;
- the appearance of hemorrhagic rashes;
- prolonged blood cessation even with minor vascular damage;
- tendency to bruise;
- the need for treatment with antiplatelet agents and anticoagulants;
- pregnancy with a high risk of developing gestosis or bleeding during childbirth;
- pathologies of the hematopoietic system.
The study must be carried out before surgery. A low degree of platelet aggregation can lead to large blood losses during surgery, which must be taken into account.
The analysis is mandatory for pregnant women to assess the functional activity of platelets. The results of the study will help select preventative agents for excessive blood loss during childbirth.
In addition, this indicator is determined if treatment with antiplatelet drugs and anticoagulants is necessary. Aspirin in small dosages is indicated for people with atherosclerosis and pathologies of the cardiovascular system. Based on the analysis data, tentative forecasts are made for the body’s reaction after taking aspirin.
It is known that platelet aggregation is also affected by drugs from other groups (antibiotics, antihistamines, anti-inflammatory drugs). Therefore, analysis is also advisable when planning to take these drugs.
Read further: Norm of platelets in the blood of women by age
How is adhesion determined?
The patient should suspect problems with platelet adhesion due to prolonged capillary bleeding. After examining the patient, the doctor issues a referral for blood tests. The form displays the number of platelets in the blood and the size of the indicated blood cells.
If the number of platelets in the blood is 600-700´109 /l, then the person is prone to thrombosis. The following categories of patients are most susceptible to this:
- patients whose spleen was removed;
- patients experiencing iron deficiency;
- patients with hematopoietic disorders who were diagnosed with myelofibrosis.
Normal and deviation during pregnancy
Deviations from the norm in the level of platelet aggregation in any direction are a sign of pathology. During pregnancy, a blood test is required to determine the risk of blood clots. In the last trimester of pregnancy, the female body prepares for possible blood loss by moderately increasing blood clotting rates. If platelet hyperaggregation is detected, this condition must be corrected.
When the levels are low, the risk of bleeding increases; when the levels are high, the risk of thrombosis increases. For pregnancy to proceed safely, platelet aggregation capabilities are required to be within normal limits - from 30 to 60%.
You can clarify the normal range in the laboratory, where a specialist will report on the risk of increased or decreased intensity of aggregation, and the likelihood of negative pregnancy complications.
Treatment of increased adhesion
Patients with an increased tendency to thrombosis are prescribed blood thinning medications. The consequence of their intake is reduced platelet aggregation and adhesion.
They have similar properties:
- Acetylsalicylic acid;
- Clopidogrel;
- Prostacyclin;
- Dipyridamole;
- Abciximab;
- Ticlopedin;
- Sulfinpyrazone;
- Ibustrin.
Acetylsalicylic acid affects the production of cyclooxygenase, as a result of which the synthesis of thromboxane is inhibited. This drug is prescribed for the prevention of embolism, treatment of heart attack and thrombosis.
It is very important that the patient adheres to the dose of medication recommended by the doctor. The medicine is well tolerated; adverse reactions may include intestinal disorders, exacerbation of gastritis and stomach ulcers.
The action of Clopidogrel is aimed at blocking platelet ADP receptors. The effect of using the drug lasts 4 days. The drug is well tolerated and rarely causes adverse reactions. Changes in the blood formula are possible.
Prostacyclin acts on platelet prostacyclin receptors. The drug causes vasodilation and reduces calcium levels in the blood. The only drawback of the medication is its rapid elimination from the body; it is considered not stable.
Dipyridamole inhibits phosphodiesterase activity, thereby reducing the production of ADP. The medication prevents platelet aggregation.
It is usually used in combination with Acetylsalicylic acid in the treatment of heart attacks and thrombosis. It is noted that the drug improves the prognosis of patients with glomerulonephritis and DIC syndrome.
Abciximab affects glycoprotein receptors. The medication is prescribed if it is planned to dilate the arteries through percutaneous coronary balloon angioplasty or atherectomy. It is also effective in preventing complications associated with such intervention.
Ticlopedine affects the platelet membrane, preventing the formation of fibrinogen bridges. It inhibits adhesion more than other drugs. The medication is effective for circulatory disorders and is prescribed to patients on hemodialysis.
It is not combined with other antiplatelet drugs because the risk of excessive bleeding increases. Among the side effects, in addition to digestive problems, there is a deterioration in liver activity, which manifests itself in jaundice.
The action of Sulfinpyrazone is similar to Acetylsalicylic acid. It has virtually no effect on the production of prostacyclin in blood vessels.
Sulfinpyrazone shows the best effect in the treatment of patients with heart attack, especially when they have undergone bypass surgery. However, in case of cerebrovascular accidents it is inferior to Acetylsalicylic acid. Adverse reactions include intestinal disorders.
Ibustrin is similar in action to Acetylsalicylic acid, but there will be fewer side effects as a result of its use. Possible problems with digestion, bleeding gums and allergies.
Platelet aggregation with inducers
According to the standard, for a more accurate diagnosis of the process, a blood test to determine the level of platelet aggregation is carried out with at least 4 inducers.
ADF inductor
Carrying out diagnostics with ADP allows us to identify process failure in the following diseases and conditions:
- Ischemia, myocardial infarction;
- Atherosclerosis;
- Diabetes;
- Arterial hypertension;
- Cerebrovascular accident;
- Hyperlipoproteinemia;
- Thrombopathy of hereditary origin;
- Thrombocytopathy in hemoblastosis;
- Taking drugs that inhibit platelet activity.
Diseases that provoke a decrease in the level of platelet aggregation:
- Essential atrombia - impaired platelet functionality;
- Wiskott-Aldrich syndrome is a rare genetically determined disease that occurs depending on the gender of the patient and is associated with changes in the size and shape of cells;
- Glanzmann's thrombasthenia is a genetic disease expressed in the absence of receptors for fibrinogen and glycoproteins;
- Thrombocytopathy with uremia;
- Aspirin-like syndrome - a violation of the second phase of platelet aggregation;
- Secondary disorders of platelet aggregation in hemoblastosis, hypothyroidism, therapy with antiplatelet agents, NSAIDs, diuretics, antibacterial drugs and drugs to lower blood pressure.
Diseases that provoke an increase in the level of platelet aggregation:
- Activation of the coagulation system during psychoemotional stress, the formation of immune complexes, and taking certain medications;
- Aspirin resistance;
- Viscous platelet syndrome: increased level of aggregation, predisposition to adhesion.
Collagen inducer
Exceeding the normative parameters in a reaction using collagen is diagnosed in case of violations at the adhesion stage. The decrease in the level of aggregation of blood plates has the same reason as in tests with ADP. An increase in level accompanies vasculitis, viscous platelet syndrome.
Inductor with adrenaline
The study of indicators of platelet aggregation ability in a test with adrenaline is considered the most informative diagnostic method. It fully demonstrates the internal mechanisms of activation, including the “release reaction.” A decrease in the normative indicator is typical for similar reasons found in reactions with ADP and collagen. An increase in the intensity of platelet aggregation is associated with increased viscosity of blood platelets, stress, and taking certain medications.
Inducer with ristocetin
The study is carried out to diagnose von Willebrand syndrome. Studying the ristocetin-cofactor activity of platelets helps to detect the severity of this factor.
All types of diagnostics using aggregation inducers make it possible to objectively assess the functionality of blood platelets. Another purpose of diagnostics is to assess the effectiveness of antiplatelet agents and help in selecting the dosage of drugs.
Reduced adhesion
This dangerous condition is classified as thrombocytopathy. The pathology is associated with the inability of platelets to perform their functions.
Signs of this deviation are:
- frequent nosebleeds;
- bleeding gums;
- a large number of bruises.
The pathology can be congenital or appear as a result of a malfunction of the thyroid gland or kidneys. Patients with low adhesion are often diagnosed with chronic leukemia and pernicious anemia.
What is this process?
Adhesion is the process of joining platelets into blood clots, due to which a kind of barrier is formed that does not allow pathogenic microflora to enter the damaged vessel.
This ability of nuclear-free cells allows a person not to worry about the consequences of a cut or soft tissue injury, since blood clots are tightly attached to the inner wall of the damaged vessel. This allows you to normalize blood flow and also avoid blood loss.
Platelets are synthesized by the bone marrow, and their lifespan is short - 5-7 days. They are formed from large cellular structures - megakaryocytes, which are located in the bone marrow. The plasma of a megakaryocyte contains from 5000 to 7000 platelets, which can fully function in the body every 7-9 days. Platelets can have different sizes, which determine their maturity: the most mature cells, which have already completed their function and are ready for disposal, have a small size and diameter compared to other cells. Young cells have a more rounded shape and are several times larger than the size of old mature cells.
If their production is imbalanced, adhesion can cause the development of pathologies and dangerous diseases. With thrombocytopenia (insufficient production of platelets), the adhesion process is minimal, since there is nothing to stick together. But with thrombocytosis (increased platelet levels), adhesion can cause the development of thrombosis and embolism in various parts of the body and internal organs that are most densely dotted with vascular mesh.
Protective and trophic functions
The protective function of blood platelets has not been fully studied. Scientists have found that when platelets function normally, they speed up the healing process of wounds and cracks. In addition, they restore internal organs that have been damaged.
Platelets are able to improve the phagocytic properties of leukocytes, including their ability to become natural killers. Due to the fact that they have separate receptors, platelets are able to respond very quickly to any type of bacterial antigen.
When platelets become active, they release a special growth factor, as well as other cytokines, which are responsible for the body's immune response. The immunity that a person receives from birth largely depends on the number of platelets and their quality.
It has been established that for those people who have pathologies in the blood, more precisely, there is a lack of platelets or problems with their functioning, the risk of mortality increases several times, especially if they receive severe injuries and injuries that lead to a septic state.
The protective properties of blood platelets have been fully proven by various experiences and experiments. Thus, if previously it was believed that platelets perform only the function of blood clotting, now their protective function has been proven. Scientists believe that in the future new properties and functions of platelets will be discovered.
- Hemoglobin
- Glucose (sugar)
- Blood type
- Leukocytes
- Platelets
- Red blood cells
Copying site materials is possible without prior approval if you install an active indexed link to our site.
In addition to the fact that platelets participate in the process of stopping blood, they are able to enhance the direct functions of leukocytes, that is:
- neutralize viruses;
- neutralize bacteria;
- reduce blood conductivity.
A blood clot formed at the site of mechanical damage to a vessel can protect the blood from infection. Cells are able to distinguish between viruses and bacteria, and also develop resistance to their activity.
Platelets take part in the formation of human immunity. Experts have proven that with a normal level of platelets in the blood, a person is exposed to diseases much less often than with an imbalance of cells in the blood.
Platelets deliver essential substances to blood vessels that protect and strengthen their walls. Thanks to this, the vessels perform their functions normally and do not burst or bleed. This is the essence of the trophic function.
Platelets are also able to bind to leukocytes, enhancing their natural functions of neutralizing and neutralizing viruses, bacteria and other foreign bodies. In addition, platelet cells reduce blood conductivity, preventing pathogenic microflora from quickly spreading throughout the body, posing a real threat to health and life in general.
Blood clots are formed from collagen cells, thanks to which the regeneration process is carried out extremely quickly. Scientists have proven that the presence of receptors at various levels on the surface helps platelets recognize viruses and bacteria at the molecular level, producing a counter-reagent.
A number of experiments have proven that platelets play an important role in the formation of immunity. If their amount in the blood is normal, then a person gets sick less often, and his life expectancy also increases.
The trophic function of platelets lies in their ability to deliver micronutrients, as well as collagen and elastin, to the cells of blood vessels, strengthening them. Thanks to the optimal level of platelets, the vessels have strong walls and do not bleed or increase in size (with thrombocytosis).
The presence of serotonin in cells, which is transported precisely by platelets, reduces the permeability of cell membranes. This factor helps the body resist various infections and bacterial infections.
Thus, due to the ability of platelets to quickly clog a damaged vessel, two advantages of adhesion are noted: stopping bleeding due to rapid blood clotting, as well as an organic barrier that prevents pathogenic microflora from entering the body through the wound.
The process of adhesion is carried out by two complementary and parallel mechanisms of gluing platelets to each other, as well as the attachment and retention of a blood clot on the surface of a vessel where there is a violation of integrity.
Adhesive effect of platelets
When studying human blood, especially when preparing for surgery, an important indicator is the adhesive effect. It is by this that they determine how susceptible a person is to the development of bleeding, as well as over what period of time the blood can completely drain. It is important to exclude the presence of pathologies and von Willebrand disease, which is genetic and involves a disruption in the production of collagen cells, which prevents normal adhesion, making the blood clot mobile.
The adhesive effect can be determined using a special study.
A portion of the blood taken from a vein is passed through a special plastic tube containing glass beads that simulate the blood composition. Next, you need to calculate the number of platelets that decreased relative to the blood sample that was not passed through a specific filter. To do this, subtract the smaller one from the larger indicator, after which the resulting value is multiplied by the first indicator and 100%. The result obtained should be within 30-50%, which is the norm. If this value is lower than recommended, the patient may suffer from embolism and may also be susceptible to developing thrombophlebitis due to thrombocytosis.
Features of adhesion
Platelets are the smallest cells in the human body that protect it from serious blood loss. During the aggregation process, they stick together. This is the initial stage of thrombus formation. Next, it grows due to an increase in cells that are attached to the wall of the damaged vessel. A clot forms and blocks blood flow. The rate of platelet adhesion is an important indicator for human life.
This process is influenced by numerous factors. For example, aggregation, in which blood cells stick together. But this phenomenon can play both a positive and negative role for the human body.
Every person should know what platelet adhesion is. The process involves the formation of a blood clot, which is necessary to prevent severe bleeding and save a person from death.
Insufficient production of these cells leads to the fact that the adhesion process is minimal and there is not enough blood substance to form a blood clot. If blood cells are produced in insufficient quantities, pathological processes occur.
An increased number of cells leads to the patient developing thrombosis and embolism. Pathological processes occur in any part of the body or in internal organs. Especially where the network of blood vessels is located quite densely.
This is explained by the fact that a high concentration of platelets increases the size of the clot. It breaks off and begins to move through the circulatory system. These are serious violations, since a clot entering the heart causes myocardial infarction. Most often, after such an event, a person dies.
Platelet aggregation or natural cessation of bleeding
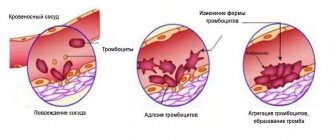
The process of stopping bleeding in the vascular network (capillaries, venules, arterioles) goes through several stages:
- After damage to the vessel, it spasms, which partially reduces the intensity of bleeding.
- At the site of traumatization of the vascular wall, blood plates are concentrated, which partially cover the defect of the damaged area - platelet adhesion occurs.
- At the site of the vessel defect, platelets accumulate, forming conglomerates; this is platelet aggregation, the first stage of thrombus formation.
- As a result of irreversible aggregation, a platelet plug is formed. It is loose, does not adhere firmly to the wound, and with a slight mechanical impact on it, bleeding resumes.
- Under the influence of thromboplastin fibrin threads, the blood plug acquires density, contracts, retraction of the thrombin thrombus occurs, and blood loss stops.
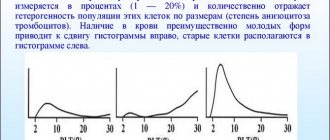
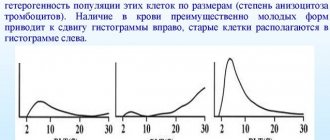
The picture below shows the stages of blood clot formation:
Platelet aggregation when stopping bleeding is not the final stage of an important process, but this does not make its importance any less. This phenomenon, which is extremely important in stopping bleeding, has a downside. With increased platelet aggregation, blood platelets stick together, even in the absence of bleeding, forming blood clots. These clots, moving through the blood vessels, provoke their blockage, disrupting the blood supply to the organs.
This is how myocardial infarction, pulmonary infarction, kidney infarction, and ischemic stroke of the brain occur. In these cases, active therapy with antiplatelet agents is prescribed for the prevention and treatment of thrombosis.
A seemingly insignificant pathological reaction of spontaneous aggregation of blood platelets can lead to thromboembolism of leading arteries, and even to the death of the patient.