Albumin is the general name for a group of simple proteins. They are responsible for several important functions and, first of all, transport substances throughout the body. The compound makes up almost 60% of the total mass of protein fractions. Produced by the liver and hepatocyte cells.
The average lifespan of one such molecule is up to 20 days. Plus or minus, depending on environmental conditions and individual characteristics of the body.
Albumin increases and decreases as a result of the influence of various pathogenetic factors. Be it liver disease or thyroid disorders. There can be a lot of options. It is necessary to begin the examination as quickly as possible.
Albumin itself is recorded by a simple biochemical blood test. There is a group of natural moments that provoke a rise and fall in protein concentration, but this is a relatively rare situation.
What is albumin and why is it needed at all? It's worth looking into it in more detail.
The role of the substance in the body
The connection performs several essential tasks. One of them has already been partially discussed.
- Transportation of connections. According to research, it is these protein fractions that transport vitamins, hormones and other important structures.
If we talk about the mechanism of this process, albumin has high chemical activity. Physically attaches molecules to itself.
But at the same time, he gives them away just as easily, despite his apparent activity and aggressiveness. This is an important, but far from the only function of the substance.
- The compound is responsible for maintaining normal oncotic pressure. To understand the essence, you need to turn to data from anatomy and physiology.
Albumin exists in several structures in the body. In blood serum, intercellular space and spinal cord.
The second variety is capable of retaining water in the cytological structures themselves. Otherwise, the fluid would leave the cytoplasm of the cell, and the functional unit would be destroyed.
Albumin prevents this from happening, retains water and ensures a stable tissue condition.
- The ability to transport is also useful as part of correction with medications. Since the compound can bind many drugs, active substances and transport them to their destination.
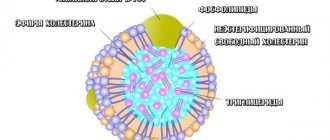
- The next important role of albumin is the neutralization of free toxins. This includes, for example, bilirubin and some poisons of chemical origin. Salts of heavy metals. This group also includes low-density lipoproteins, which can be deposited on the walls of blood vessels and cause atherosclerosis.
There are many more options. In this regard, albumin is a kind of cleaner that eliminates toxic, dangerous components from the body.
- Albumins do not contain carbohydrates. But they contain many valuable amino acids. This is the basis of the composition of the substance. Therefore, the connection acts as a backup storage for useful structures.
In case a person stops eating normally for one reason or another. The supplies will last for some time. Then dangerous changes in the body will begin.
- Albumin is involved in protein synthesis. That is, other protein compounds.
- Protection of red blood cells. Red blood cells react negatively to the presence of large amounts of fatty acids and cholesterol. The described substance is able to bind dangerous structures, so the cells are under reliable protection.
- Due to the ability to inactivate lipoproteins, albumins provide prevention of fatty liver hepatosis.
This is a dangerous pathological process, which is accompanied by tissue destruction and replacement of functionally active hepatocytes with fat.
- Finally, in the same way the substance protects blood vessels from cholesterol plaques. Prevents the development of a dangerous disorder - atherosclerosis.
There are many functions. Albumin in the blood is a protector and reliable transport for compounds. It has many tasks that the substance performs non-stop.
New proteins are produced in the liver and are utilized there after 18-22 days. Average.
There is also a less obvious task. The substance is detected using a biochemical blood test. Therefore, all changes clearly speak in favor of pathological processes almost always.
Elevated albumin can be considered as a nonspecific indicator of diseases of the liver, digestive tract and other structures. But this is rather a diagnostic rather than a natural biological function.
I. Albumins
Blood plasma protein fractions
The main protein of this fraction is albumin.
Albumin . A simple protein of 585 AAs with a mass of 69 kDa, has 17 disulfide bridges, many dicarboxylic AAs, and is highly hydrophobic. Albumin exhibits polymorphism. Synthesized in the liver (12 g/day), utilized by the kidneys, enterocytes and other tissues. T½=20 days. 60% of albumins are found in the intercellular substance, 40% in the bloodstream. Albumin in plasma is 40-50 g/l, they make up 60% of all blood plasma proteins. Functions: maintaining osmotic pressure (80% contribution), transport of free fatty acids, bilirubin, bile acids, steroid and thyroid hormones, cholesterol, drugs, inorganic ions (Cu2+, Ca2+, Zn2+), is a source of amino acids.
Transthyretin (prealbumin) . Tetramer. In plasma 0.25 g/l. Acute phase protein (group 5). Transports thyroid hormones and retinol binding protein. Decreases with fasting.
Dysproteinemia of the albumin fraction is realized mainly due to hypoalbuminemia.
The cause of hypoalbuminemia is a decrease in albumin synthesis during liver failure (cirrhosis), with increased capillary permeability, with activation of catabolism due to burns, sepsis, tumors, with loss of albumin in the urine (nephrotic syndrome), and with fasting.
Hypoalbuminemia causes tissue edema, decreased renal blood flow, activation of the RAAS, water retention in the body, and increased tissue edema. A sudden outflow of fluid into the tissue leads to a decrease in blood pressure and can cause shock.
Globulins. They contain lipoproteins and glycoproteins.
II. α1-Globulins
α1-Antitrypsin is a glycoprotein synthesized by the liver. In plasma 2.5 g/l. Acute phase protein (group 2). An important inhibitor of proteases, including neutrophil elastase, which destroy elastin in the alveoli of the lungs and liver. α1-Antitrypsin also inhibits skin collagenase, chymotrypsin, fungal and leukocyte proteases. With a deficiency of α1-antitrypsin, emphysema and hepatitis can occur, leading to cirrhosis of the liver.
Acidic α1-glycoprotein , synthesized by the liver. In plasma 1 g/l. Acute phase protein (group 2). Transports progesterone and related hormones.
HDL is synthesized in the liver. In plasma 0.35 g/l. They transport excess cholesterol from tissues to the liver and ensure the exchange of other drugs.
Prothrombin is a glycoprotein containing about 12% carbohydrates; the protein part of the molecule is represented by one polypeptide chain; molecular weight about 70,000 Da. In plasma 0.1 g/l. Prothrombin is a precursor to the enzyme thrombin, which stimulates the formation of a blood clot. Biosynthesis occurs in the liver and is regulated by vitamin K produced by intestinal flora. With a lack of vitamin K, the level of prothrombin in the blood drops, which can lead to bleeding (early childhood hemorrhage, obstructive jaundice, some liver diseases).
Transcortin is a glycoprotein synthesized in the liver, weight 55700 Da, T½=5 days. Transports cortisol, corticosterone, progesterone, 17-alpha-hydroxyprogesterone and, to a lesser extent, testosterone. In plasma 0.03 g/l. Blood concentrations are sensitive to exogenous estrogens and depend on their dose.
Thyroxine-binding globulin (TBG) is synthesized in the liver. Molecular weight 57 kDa. In plasma 0.02 g/l. Т½=5 days. It is the main transporter of thyroid hormones in the blood (transports 75% of thyroxine and 85% of triiodothyronine).
Dysproteinemia due to the α1-globulin fraction is realized mainly due to: 1). reducing the synthesis of α1-antitrypsin. 2). Loss of proteins of this fraction in the urine during nephrotic syndrome. 3). increase in acute phase proteins during inflammation.
III. α2-Globulins
α2-Macroglobulin is a very large protein (725 kDa) synthesized in the liver. Acute phase protein (group 4). In plasma 2.6 g/l. The main inhibitor of many classes of plasma proteinases, regulates blood coagulation, fibrinolysis, kininogenesis, immune reactions. The level of α2-macroglobulin in plasma decreases in the acute phase of pancreatitis and prostate carcinoma, and increases as a result of the hormonal effect (estrogens).
Haptoglobin is a glycoprotein synthesized in the liver. In plasma 1 g/l. Acute phase protein (group 2). Binds hemoglobin to form a complex with peroxidase activity and prevents the loss of iron from the body. Haptoglobin effectively inhibits cathepsins C, B and L and may participate in the utilization of some pathogenic bacteria.
Vitamin D binding protein (VBP) (mass 70 kDa). In plasma 0.4 g/l. Provides transport of vitamin A in plasma and prevents its excretion in urine.
Ceruloplasmin is the main copper-containing plasma protein (contains 95% of copper in plasma) with a mass of 150 kDa, synthesized in the liver. In plasma 0.35 g/l. Т½=6 days. Ceruloplasmin has pronounced oxidase activity; limits the release of iron, activates the oxidation of ascorbic acid, norepinephrine, serotonin and sulfhydryl compounds, inactivates reactive oxygen species, preventing lipid peroxidation.
Ceruloplasmin is an acute phase protein (group 3). It increases in patients with infectious diseases, liver cirrhosis, hepatitis, myocardial infarction, systemic diseases, lymphogranulomatosis, and malignant neoplasms of various localizations (lung, breast, cervical, gastrointestinal tract cancer).
Wilson-Konovalov disease. Ceruloplasmin deficiency occurs when its synthesis in the liver is impaired. With ceruloplasmin deficiency, Cu2+ leaves the blood, is excreted in the urine, or accumulates in tissues (for example, in the central nervous system, cornea).
Antithrombin III. In plasma 0.3 g/l. Plasma protease inhibitor.
Retinol-binding protein is synthesized in the liver. In plasma 0.04 g/l. Binds retinol, ensures its transport and prevents breakdown. Functions in combination with transthyretin. Retinol binding protein fixes excess vitamin A, which prevents the membranolytic effect of high doses of the vitamin.
Dysproteinemia due to the α2-globulin fraction can occur during inflammation, because this fraction contains acute phase proteins.
IV. β-Globulins
VLDL - are formed in the liver. Transport TG, HS.
DILI - formed in the blood from VLDL. Transport TG, HS.
LDL – formed in the blood from LDLP. In plasma 3.5 g/l. They transport excess cholesterol from peripheral organs to the liver.
Transferrin is a glycoprotein synthesized by the liver. In plasma 3 g/l. Т½=8 days. The main transporter of iron in plasma, 1 molecule of transferrin binds 2 Fe3+, and 1 g of transferrin, respectively, about 1.25 mg of iron. As iron concentration decreases, transferrin synthesis increases. Acute phase protein (group 5). Decreased in liver failure.
Fibrinogen is a glycoprotein synthesized in the liver. Molecular weight 340 kDa. In plasma 3 g/l. Т½=100 hours. Blood coagulation factor I is capable of being converted into fibrin under the influence of thrombin. It is a source of fibrinopeptides with anti-inflammatory activity. Acute phase protein (group 2). The fibrinogen content increases during inflammatory processes and tissue necrosis. Decreased in DIC syndrome and liver failure. Fibrinogen is the main plasma protein that affects the ESR value (with increasing fibrinogen concentration, the erythrocyte sedimentation rate increases).
C-reactive protein is synthesized predominantly in hepatocytes; its synthesis is initiated by antigens, immune complexes, bacteria, fungi, and during injury (4-6 hours after injury). Can be synthesized by arterial endothelial cells. In plasma <0.01 g/l. Acute phase protein (group 1). Capable of binding microorganisms, toxins, and particles of damaged tissue, thereby preventing their spread. These complexes activate complement along the classical pathway, stimulating the processes of phagocytosis and elimination of harmful products. C-reactive protein can interact with T lymphocytes, phagocytes and platelets, regulating their functions in inflammatory conditions. It has antiheparin activity and, when its concentration increases, inhibits platelet aggregation. CRP is a marker of the rate of progression of atherosclerosis. Determined for the diagnosis of myocarditis, inflammatory diseases of the heart valves, inflammatory diseases of various organs.
Dysproteinemia due to the β-globulin fraction can occur when 1). some dislipoproteinemias; 2). inflammation, because this fraction contains acute phase proteins; 3). In case of a violation of the blood coagulation system.
V. γ-Globulins
They are synthesized by functionally active B lymphocytes (plasmocytes). An adult has 107 clones of B-lymphocytes that synthesize 107 types of γ-globulins. γ-Globulin glycoproteins consist of 2 heavy (440 AA) and 2 light (220 AA) polypeptide chains of various configurations, which are connected by disulfide bridges. Antibodies are heterogeneous; individual components of polypeptides are encoded by different genes, with different abilities to mutate.
All γ-globulins are divided into 5 classes G, A, M, D, E. Each class has several subclasses.
Dysproteinemia due to the γ-globulin fraction can occur when 1). Immunodeficiency condition; 3). Infectious processes. 2). Nephrotic syndrome.
Norms by age
Among women
The normal level of albumin in the blood of women ranges from 34 to 50 grams per liter of blood and varies slightly with age.
| Age (years) | Serum level (grams per liter) |
| 14-50 | 35-50 |
| 50-60 | 35-50 |
| 60 and older | 34-49 |
In men
In men, the normal level of albumin in the blood is not very different and ranges from 34-50 g/liter of blood.
| Age (years) | Serum albumin levels (grams per liter) |
| 14-50 | 35-50 |
| 50-60 | 34-50 |
| After 60 | 35-48 |
In children
| Lifespan | Albumin concentration (g/l) |
| Newborns | 28-44 |
| Up to 4 days | 38-50 |
| Up to 5 years | 38-50 |
| 5-14 years | 38-54 |
Next, the standard is calculated based on the calculations of an adult.
During pregnancy
During gestation, the concentration of proteins is approximately the same level and amounts to 56-85 grams per liter of blood.
However, these are ideal conditions. Depending on the state of health, various deviations and pathological processes are possible. Special diagnostics are needed to give specifics.
Prealbumin
Before the albumin fraction, when using the radial immunodiffusion method, a protein is detected that forms a precipitation arc, called prealbumin. This tryptophan-rich protein (MW 60 kDa) with a half-life of 1.9 days is synthesized in the liver and primarily performs a transport function. In the blood, it circulates in a very strong complex with retinol-binding protein, prevents its exit from the bloodstream and is responsible for the transfer of retinol into tissues. There is evidence of the participation of prealbumin in the transport of thyroxine and triiodothyronine (10-20% of the total amount of hormones).
Normal values
| Serum | 0.18-0.38 g/l |
| Cerebrospinal fluid | 0.012-0.05 g/l |
Clinical and diagnostic value
The amount of protein reflects the functional state of the liver. A decrease in level occurs in liver diseases, especially in acute viral hepatitis, chronic hepatitis, and malignant neoplasms with metastases to the liver.
Prealbumin is an earlier indicator of disease than albumin.
Reasons for the increase
Among the factors for the development of growth indicators.
Intestinal infections
Various character and origin. For example, colitis due to salmonella infection or cholera. Although the second option is several times less common.
All these conditions lead to the natural breakdown of protein and increased albumin activity, since rapid transport of the substance “out” is required.
Symptoms depend on the specific pathological process. Among the possible options:
- Stomach ache. Different localizations.
- Stool disorders. Constipation and diarrhea. Or alternating them.
- Bloating. Flatulence. Increased production of intestinal gas.
- Dyspepsia. With heartburn, nausea, vomiting, belching and other delights of this condition.
Treatment is carried out under the supervision of a gastroenterologist. Antibiotic or antiviral drugs are prescribed. Depends on the specific condition.
Internal antiseptics are also used. It is important to accurately dose medications so as not to worsen the situation.
If albumin is elevated due to intestinal infections, there is no need to specifically reduce it. It will go away on its own as soon as the underlying disease is corrected.
Long-term treatment with hormones
Not necessarily glucocorticoids. Often we are talking about seemingly harmless drugs such as oral contraceptives.
In fact, they are not at all safe. Strict dosing of medications is necessary so as not to provoke disorders. Women often ignore all the rules. Even basic security measures for the sake of momentary gain.
There are no symptoms. However, with long-term use of oral contraceptives, the following manifestations occur:
- Menstrual irregularities.
- Reproductive function disorders.
- Pain in the lower abdomen.
- Acyclic bleeding.
Problems are also possible during pregnancy and childbearing.
Treatment involves discontinuing the drug that caused the abnormal manifestations or adjusting the dose. In any case, you need to consult your doctor.
Attention:
The question is complex. Solving it on your own is strictly prohibited.
Infectious diseases
Of very different origins. From simple ARVI to influenza and tuberculosis. The fact is that albumins are involved in the transfer and transportation of harmful compounds. As a result, the body needs to synthesize more protein fractions. The ones that exist don't do the job.
The phenomenon is temporary, but with chronic inflammation the disorder persists indefinitely.
The symptoms are specific. Among the common manifestations for all infectious pathologies:
- Painful sensations in the body.
- Increased body temperature.
- Signs of general intoxication. Be it headaches, nausea, vomiting, weakness, or all of them at once.
- Further manifestations depend on the specific disease.
Treatment is carried out under the supervision of a therapist and an infectious disease specialist. If there is a reason for it.
Antibiotics and antivirals of various effects are needed. Immunostimulants, when there is also a weakening of the body’s defenses.
The patient is prescribed a rest regime; it is necessary to overcome the primary focus of the pathological process. The task is not easy. Moreover, it takes quite a long time. Serum albumin and other fractions will decline on their own.
Burns
The concentration of proteins depends on the area of dermal lesions. The fact is that the compounds are contained in the intercellular space in huge quantities. When the skin is destroyed, substances are released into the blood. Thus, they are recorded by biochemical analysis.
Specific clinical picture:
- Disturbance of normal heart rhythm.
- Bleeding.
- Visible skin defects.
- An increase or, conversely, a decrease in body temperature.
- Breathing disorders.
- Possible depression of consciousness.
The patient is urgently transported to the hospital. After which treatment begins in the burn department. It is possible that resuscitation measures will be required. The task is not easy. Especially with a large affected area.
Intestinal obstruction
An acute condition in which food and feces (depending on location) cannot move through the gastrointestinal tract. It occurs relatively often, especially in older patients.
Accompanied by severe symptoms:
- Increased body temperature.
- Intense pain.
- Nausea.
- Vomiting. Moreover, regardless of food intake.
- Heaviness in the stomach.
- Impaired consciousness.
- Possible cardiac disorders.
Treatment is carried out by specialists in abdominal surgery. If the situation is urgent, general surgeons are involved. Urgent surgical elimination of the pathological condition is necessary. The task is complex and quite risky in terms of solution.
Therapy is carried out in a hospital setting. It is necessary to transport the patient as quickly as possible.
Some forms of obstruction are treated conservatively, but this is rather a rare exception to the rule.
Hepatitis
Acute or chronic inflammation of the liver. Occurs against the background of an infectious lesion. The virus of the same name. There are several strains of it that vary in aggressiveness.
The clinical picture is as follows:
- Pain in the right side.
- Nausea.
- Change in color of stool. Discoloration of the contents of the large intestine.
- Vomit.
- Increased body temperature.
The disease is relatively easily recognized by instrumental and laboratory methods.
Treatment is on an outpatient basis. Specific drugs of several pharmaceutical types are prescribed.
Antibiotics are useless here, as are anti-inflammatory ones. On the contrary, dangerous complications will develop.
Autoimmune reactions
Systemic lupus erythematosus, rheumatoid arthritis. Elevated albumin means the acute phase of the pathological process, in contrast to an infectious lesion, this is due to an inadequate immune response to a harmless factor.
Symptoms depend on the exact location of the pathological process. Therefore, there is no overall picture. There are many diseases.
Therapy is carried out under the supervision of a rheumatologist. The participation of an immunologist is possible. Glucocorticoids are prescribed in adjusted dosages to reduce the inflammatory process. Next, suppressors are shown as needed. They inhibit the work of the body's defenses.
Cirrhosis
Acute or chronic liver damage. Accompanied by severe deviations in the functioning of the organ. It begins to disintegrate and collapse under the influence of negative factors. Mainly due to alcoholism or other toxic lesions.
The clinical picture is approximately the same as for hepatitis. Then they develop:
- Brain disorders.
- Blood clotting disorders. Basically it becomes too runny.
- Formation of rashes and vascular spiders on the skin.
Recovery is carried out under the supervision of a hepatologist. If there is no such doctor, a gastroenterologist.
The treatment is as follows. Hepatoprotective drugs are used in high concentrations. Essentiale, Karsil and other names.
Diabetes
Disorder of the pancreas. Happens quite often. The disease is accompanied by insufficient production of insulin or poor sensitivity of the body to this substance.
Typical symptoms:
- Sugar intolerance.
- Destruction of blood vessels.
- Gangrene.
- Decreased vision.
Complications and manifestations are severe and dangerous. Correction is required under the supervision of an endocrinologist. Insulin is prescribed (as needed, to stop attacks).
A strict low-carbohydrate diet is also prescribed. You need to give up sugar and switch to substitutes. There are many options.
The course of therapy is worked out under the supervision of endocrinology specialists. In an individual format, since the course of diabetes is very different.
Kidney diseases
Pathologies that are associated with damage to the organ parenchyma. For example, pyelonephritis. Accompanied by intense pain, impaired filtering function and other issues.
The correction is carried out under the supervision of nephrologists or urology specialists. It is important to carry out treatment as quickly as possible so as not to provoke intoxication and kidney failure due to high protein.
Albumin in the blood is increased
Quite often, the cause of an increase in albumin in the blood is simple dehydration. But it is not always the lack of water that is a deviation from the norm.
Hyperalbuminemia is a rather rare phenomenon, but is often observed in the following pathological processes occurring in the human body:
- Infectious diseases.
- Multiple myeloma.
- Waldenström's macroglobulinemia.
- Systemic lupus erythematosus.
- Rheumatoid arthritis.
- Chronic hepatitis or cirrhosis of the liver.
- Vomiting or diarrhea are the main causes of dehydration, and, consequently, the diseases that caused them.
- Intestinal obstruction.
- Diabetes and nephritis.
- Extensive burns.
- Taking corticosteroids and bromsulfalein.
- Compression of veins, for example, when applying a tourniquet.
- Cholera.
- Dehydration in severe injuries.
- Hemoconcentration.
Reasons for the decline
There are no less factors for a drop in albumin levels.
Oncological processes
Mostly malignant. They develop against the background of various types of lesions. From chemical to radiation. Negative heredity also plays an important role.
The clinical picture depends on the specific pathological process. And its localization.
Treatment is strictly surgical. The neoplasia must be removed. Then, after this, a course of radiation and chemotherapy is prescribed. According to need. The question is complex and will have to be resolved by the oncologist.
Heart diseases
Albumin almost always falls against the background of pathologies of cardiac structures. It is necessary to carry out the correction as quickly as possible.
Among the diagnoses:
- IBS.
- Previous heart attack.
- Angina pectoris.
- Coronary insufficiency.
- Ischemia-type disorders.
The cause of low albumin concentration in the blood is corrected with the help of cardioprotectors and drugs to control blood pressure.
Pathologies of the digestive tract
Some of them can provoke not an increase, but a decrease in the substance’s indicator. Reason for low albumin: gastritis, stomach or intestinal ulcer, dysbiosis.
They are relatively simple to correct, but treatment must be carried out under the supervision of a gastroenterologist.
Excess water in the body
Liquid intoxication is a relatively rare phenomenon. Develops against the background of insufficient kidney function. The goal is to remove excess water artificially.
Powerful diuretics are prescribed. Loop diuretics (Torasemide or Furosemide), less often - osmotic agents. The main thing is not to exceed the dosage so as not to provoke dehydration.
Excessive use of antibiotics and non-steroidal anti-inflammatory drugs
To adjust protein levels, it is enough to stop taking these drugs or replace them with others.
Massive blood loss
For example, as a result of injuries. Restoration is required immediately. It takes place in a hospital setting. Hematology or traumatology department.
The cause of low albumin is eliminated by transfusion of plasma, red blood cells or whole blood. The goal is to restore the natural concentration of proteins, which are mechanically removed from the body with liquid connective tissue.
Alcoholism
Chronic dependence on alcohol. Accompanied by severe dysfunctional processes in the body. Treatment under the supervision of a narcologist is necessary.
Low albumin: causes
When the albumin content decreases and reaches 25 - 30 g/l, hypoalbuminemia is stated.
A reduced protein concentration indicates conditions such as:
- malignant process in the body;
- inflammatory kidney disease - diabetic nephropathy, nephrotic syndrome;
- diseases of the digestive system;
- leukemia, blood sepsis;
- dysfunction of the cardiovascular system;
- functional liver disorders - atrophy, cirrhosis, hepatitis;
- connective tissue damage;
- presence of severe injuries, burns;
- excessive water content in the body;
- pulmonary edema;
- severe blood loss, transfusion of blood substitutes;
- genetic pathologies due to which albumin levels decrease;
- prolonged fasting caused by adherence to low-protein and unbalanced diets.
Other reasons why albumin levels decrease:
- taking certain medications, especially in case of overdose;
- alcohol and tobacco abuse.
If your albumin level is elevated, do not panic and do not look for illness.
Reduced protein levels in biochemical analysis appear as a result of taking estrogen-containing drugs, fasting and the use of glucocorticosteroids.
After receiving the results, contact your doctor to schedule additional tests.
How to increase albumin in the blood?
The easiest way to increase albumin concentration is to eat foods high in protein, fat and fiber every day:
- eggs;
- dairy and fermented milk products;
- chicken;
- oatmeal;
- fish, seafood;
- nuts and lipids;
- fruits and vegetables.
It is advisable to coordinate the nutritional regimen with your doctor.
Hypoalbuminemia is often associated with improper liver function, so doctors advise eliminating from the diet:
- salted, smoked, fried, spicy;
- alcohol.
It is also important to treat infections, start the fight against obesity, and not abuse medications without the prescription of a specialist.
Another method of increasing protein content is drinking liver tea. The herbal collection helps normalize liver function, cleanses the organ of waste and toxins, improving the general condition of the patient.
The drink has a minimum of contraindications with the exception of individual intolerance and the presence of gallstones, but before use it is advisable to consult with your doctor.
In the photo: liver herbal tea
For hypoalbuminemia, the drug Albumin is prescribed . The medicine is administered by intravenous jet and drip infusion. The dosage depends on individual indications, age and position of the patient - sometimes Albumin is used to treat pregnant women.
In the photo: human Albumin, 20%, 50 ml.
Reference! The medication has contraindications and a number of side effects, so you should not self-medicate.
Additional examinations
A blood test for albumin is far from the only diagnostic method. It is carried out within the framework of venous blood biochemistry and does not provide accurate data about the disease. Therefore, auxiliary measures are needed.
- Oral questioning of the patient.
- Anamnesis collection.
- Ultrasound of the digestive tract.
- EGC.
- ECHO.
- Ultrasound scan of the kidneys.
- Liver scintigraphy. Radioisotope research. The same applies to the paired filter organ.
- MRI as needed. Mainly to diagnose cancer.
Albumins are essential and extremely active proteins that work as transport and as protection of the body from harmful factors. It makes sense to check the concentration of the compound regularly.