Rubella (or German measles) is an acute infectious disease caused by the Rubella RNA virus from the Togaviridae family. If it is mild in pediatric patients, then during pregnancy it becomes quite dangerous for the healthy development of the fetus. Therefore, it is important for expectant mothers to promptly undergo a test for antibodies to the rubella virus, and if IgG is positive, find out what this means from a specialist.
A little about rubella
The disease is transmitted through the air, through household objects, close contact with an infected person, or from mother to child (in utero and during breastfeeding). It occurs in typical, atypical and innaparent forms. The incubation period after infection is two to three weeks. First, pathogens penetrate the nasal cavity and the oral part of the pharynx, then penetrate the bloodstream and lymph nodes, where they multiply intensively.
As the disease develops, the lymph nodes become inflamed, and then red rashes appear on the face. During the first 24 hours, the rash spreads throughout the body, which may be accompanied by fever, redness of the eyes, sore throat, and nasal congestion.
Adult patients have a hard time suffering from an infection that can affect the nervous system, causing pneumonia, arthritis, otitis media, tonsillitis, encephalitis, and a serous form of meningitis. Testing for rubella will not only detect the disease in time, but will also help prevent unwanted consequences.
Rubella
Rubella (Rubella) is an acute viral disease characterized by small-spotted exanthema, generalized lymphadenopathy, and moderate fever. The causative agent is an RNA virus that belongs to the Togaviridae family of the Rubivirus genus. The rubella virus has a tropism for embryonic tissue, damages the genetic apparatus of cells, suppresses mitosis of individual cell populations of the embryo and, possibly, has a direct cytopathogenic effect, which significantly disrupts the development of the fetus.
Rubella is a severe anthroponosis. The source of infection is a person with a clinically pronounced, atypical or erased form of the disease, as well as children with congenital rubella, in whose body the virus can persist for several months (up to 1.5–2 years). Along with the manifest forms of rubella, there are asymptomatic (inapparent) forms. The ratio of clinically significant rubella to asymptomatic infection in children is 1:1, and in adults 1:2–1:8. The inapparent course of rubella is observed 5–6 times more often than the clinically significant course.
Before the introduction of active immunization, rubella occurred in epidemic outbreaks with an interval of 6–9 years. During an epidemic outbreak, not only children, but also adults, especially in organized groups, get sick. Immunization contributed to a sharp decline in morbidity. The maximum number of diseases is recorded in April–June. Rubella is especially dangerous for pregnant women due to intrauterine infection of the fetus.
The incubation period lasts 15–21 days. Routes of transmission: airborne, of particular importance is the vertical (transplacental) route of transmission of rubella from mother to fetus. The patient poses an epidemic danger from the second half of the incubation period of rubella; the greatest infectiousness occurs in the prodromal period and the first days of the disease. The entrance gate is the mucous membranes of the upper respiratory tract, from where the virus penetrates into the nearest lymph nodes (especially the posterior cervical and occipital), which leads to their inflammation and enlargement. A sick person begins to excrete the virus in nasopharyngeal discharge 5 days before the rash appears and excretes it 5–7 days after it disappears. Subsequently, viremia occurs. The virus spreads hematogenously throughout the body, has dermatotropic properties, and causes changes in the lymph nodes, which increase at the end of the incubation period. The entry of the virus into the blood is the beginning of the clinical manifestations of the disease: fever, catarrhal symptoms (runny nose, sore throat, conjunctivitis), small maculopapular rash - exanthema (pale pink or red spots, 2-4 mm in diameter without peeling). Exanthema is a characteristic manifestation of rubella.
IgM antibodies in the serum appear 1–2 days after the rash, after 2–3 weeks the titer reaches its maximum level, and after 2–3 months they usually disappear. IgG antibodies to the rubella virus begin to be produced 3–4 weeks after infection, reaching a maximum level by 8–9 weeks of illness and are detected after the end of the acute illness for life, providing protection against re-infection. However, rare cases of reinfection have been described, which are accompanied by a sharp increase in the level of IgG antibodies. After the disease, stable lifelong immunity is formed, while after immunization, 10% of women do not develop protective immunity, and therefore it is advisable to examine women before planning pregnancy and if there are indications for examination.
There is no generally accepted classification of clinical forms of rubella, but depending on the nature of infection, acquired and congenital rubella are distinguished, which can occur in a typical form and atypically. Atypical rubella is mild, without exanthema, and is characterized by mild catarrhal inflammation of the upper respiratory tract and moderate lymphadenopathy. In this case, an indication of contact with a patient with rubella is the basis for a laboratory examination.
Acquired rubella
occurs cyclically in the form of an acute infectious disease. In children, the disease is relatively mild. Initially, elements of the rash appear on the face and neck, behind the ears and on the scalp. During the day, the rash spreads to various parts of the body without a specific pattern. The location of the rash is especially typical on the back, buttocks and on the extensor surfaces of the upper and lower extremities. The soles and palms are not affected. Almost simultaneously with the spread, the rash begins to fade, completely disappearing in 1-3 days, leaving no pigmentation behind. Later, enlargement of the posterior cervical and occipital lymph nodes, slight fever, and catarrh of the upper respiratory tract may occur. In 30% of cases, rubella occurs without a rash, but lymphadenitis is always present.
In adults, the disease is usually much more severe. The rash may be preceded by prodromal phenomena in the form of general malaise, headache, chills with a fever up to 38°C, joint pain, runny nose, sore throat and, as a rule, systemic enlargement of the lymph nodes, especially the posterior cervical and occipital ones. Among the complications of rubella, migratory arthritis is often encountered. They occur after the rash disappears and are more often observed in women (60%). These symptoms may last for 3–4 days, sometimes longer. Other complications include otitis, pneumonia, thrombocytopenia, manifested by a hemorrhagic rash. Rare, but very serious complications are encephalitis and encephalomyelitis (more often detected in adults) with a high mortality rate of 20–50%.
The clinical picture of rubella in pregnant women is unremarkable. Rubella disease can have various consequences: no effect on the fetus; infection of the placenta only, infection of the placenta and fetus. The adverse effect of rubella infection on the fetus is manifested by spontaneous abortions (from 10 to 40%), stillbirth (20%), and death in the neonatal period (10–25%).
The frequency and extent of fetal damage is largely determined by the gestational age at the time of infection. The shorter the pregnancy period during which a woman becomes ill with rubella, the more often and more significantly the teratogenic effects of the virus manifest themselves. The most dangerous is the first trimester of pregnancy, during the period of organogenesis. Rubella disease in the 3–4th week of pregnancy causes congenital deformities in 60% of cases, in the 9–12th week – in 15%, and in the 13–16th week – in 7% of cases.
Congenital rubella
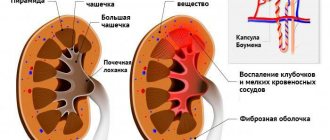
. In the first weeks of pregnancy, damage to the embryo occurs through the mother's blood and chorion during general viremia of the pregnant woman. Subsequently, after the formation of the placenta (14 weeks of pregnancy and later), the transplacental nature of infection predominates. The virus enters the placenta during viremia, where it multiplies, easily overcomes the placental barrier and infects the fetus. Through the mother's blood from the intervillous space, the pathogen penetrates the fetal vessels, then into the umbilical vessels and reaches the endocardium, from where necrotic masses containing the active virus are spread hematogenously throughout the body, infecting various organs and tissues of the fetus. At the same time, due to viral damage to the endothelium of the blood vessels of the placenta, the nutrition of the fetus is disrupted. The infection causes disturbances in mitotic activity and chromosomal changes, which is reflected in retardation in physical and mental development. Congenital rubella can also develop after asymptomatic (inapparent) rubella in the mother. The degree of damage does not depend on the severity of the disease in the pregnant woman. Several cases of intrauterine infection of the fetus have been described in women who had rubella 6–12 months before conception, which is obviously explained by the unusually long persistence of viruses in the mother’s blood.
The course of the disease with intrauterine infection differs significantly from ordinary rubella. Congenital Rubella Syndrome (CRS) depends on the timing of infection. There is a classic syndrome of congenital rubella, the so-called Greg's triad (cataracts - 75%, heart defects - 50%, deafness - 50%). Congenital rubella syndrome usually includes: cardiac malformations – patent ductus arteriosus, ventricular septal defects, pulmonary stenosis; eye damage – corneal opacities, cataracts, chorioretinitis, microphthalmia; microcephaly, mental retardation, and deafness are also characteristic. In subsequent years, thrombocytopenic purpura, enlarged liver and spleen, intrauterine growth retardation, interstitial pneumonia, myocarditis or myocardial necrosis, and bone damage in the metaphysis were additionally considered manifestations of this syndrome. The list of these manifestations began to be called extended congenital rubella syndrome. Some children showed signs of humoral and cellular immunodeficiency; later, in persons with congenital rubella, diabetes mellitus or progressive subacute panencephalitis developed.
When the fetus is infected in the early stages of development (infection is especially dangerous in the first 8 weeks of pregnancy - during the critical phase of organogenesis), multiple anomalies occur as a result of the course of the infection. The heart, organs of hearing, vision, skull bones, and limbs are damaged. Among such infants there is a very high percentage of perinatal mortality. The most common types of congenital anomalies due to infection in a woman after the first trimester of pregnancy are deafness (70–90%) and retinopathy. Hepatomegaly and splenomegaly, hemorrhagic syndrome, hepatitis, and pneumonia are somewhat less common. Children infected with rubella, even without developmental defects, are often born with low body weight and short stature, and subsequently lag behind in physical development.
With the development of intrauterine infection, a child produces specific IgM antibodies, which persist in the postnatal period (up to 6 months), with the gradual appearance of their own IgG antibodies. At the same time, the child detects IgG antibodies received from the mother, which disappear after a few months. After birth, the virus is found in the placenta. In sick newborns, it can be detected in the nasopharynx, saliva, urine, feces and excreted for 1–2 years.
Indications for examination
- Pregnancy planning;
- presence of a burdened obstetric history (perinatal losses, birth of a child with congenital malformations);
- pregnancy (primarily with ultrasound signs of intrauterine infection, developmental anomalies);
- women at the birth of a child with congenital malformations;
- children with symptoms of congenital infection, congenital malformations;
- children whose mothers are at risk for intrauterine transmission of the rubella virus;
- the presence of exanthema or “rubella-like” rash;
- established or suspected contact with a person with rubella;
- thrombocytopenia.
Differential diagnosis.
In the presence of small-spotted exanthema - adenoviral and enteroviral diseases, measles, infectious mononucleosis, pityriasis rosea, drug exanthema, erythema infectiosum; with thrombocytopenia – parvovirus infection B19.
Etiological laboratory diagnostics include detection of the virus in cell culture, detection of its RNA, determination of specific antibodies to rubella virus antigens in the blood.
Material for research
- Venous or umbilical cord blood, saliva, nasopharyngeal swabs, washings, scrapings; cerebrospinal fluid, amniotic fluid, chorionic villi, placenta - isolation of the virus in cell culture, detection of its RNA;
- serum of venous or umbilical cord blood - determination of AT.
Comparative characteristics of laboratory diagnostic methods.
To detect the rubella virus, a cell culture is infected with biomaterial. The study is carried out only in specialized virology laboratories, duration is 4–5 days.
To detect rubella virus RNA, the PCR method is mainly used. Once a rash appears, viral RNA can be detected in the blood and nasopharynx for 7 days after the rash. PCR diagnostics are used much more often in the study of nasopharyngeal discharge (from contact persons), blood, biopsy samples, and chorionic villi.
The determination of AT is used for the diagnosis of rubella, for screening in the complex of TORCH infections and for assessing the strength of post-vaccination or anti-infectious immunity. For early diagnosis, the most valuable is the detection of IgM antibodies in the blood serum, which appear within 1–2 days after the rash. Determining the avidity of specific IgG antibodies to rubella virus antigens in the blood allows one to estimate the timing of infection and differentiate an acute infection from an infection suffered in the past (from the first days to 1.5 months or more). To diagnose a primary infection, it is important to determine the avidity of IgG antibodies. Low-avidity antibodies indicate a primary infection, high-avidity antibodies exclude the possibility of an acute infectious process occurring in the last 4–6 weeks.
If it is possible to determine only IgG antibodies, it is advisable to study dynamics, while an increase in the titer of IgG antibodies by 4 or more times will indicate a current infection. An increase in antibody titer in the absence of severe symptoms may be the only evidence of the presence of reinfection or the development of infection in a vaccinated person, in the differential diagnosis of conditions clinically similar to rubella.
Indications for the use of various laboratory tests and features of interpretation of results in different categories of subjects
Screening when planning pregnancy often includes the detection of IgM and IgG antibodies. When a positive result is detected for IgG antibodies and the absence of IgM antibodies, it is generally accepted that the woman has immunity (post-vaccination, if she confirms the presence of this, or post-infectious - a history of rubella, contact with a sick person), the intensity of which is sufficient to prevent the development of placentitis and infection of the fetus with the rubella virus in case of infection.
If there is a history of contact with a patient with rubella over the past 3–6 months, to exclude (confirm) a primary infection, it is important to identify low-avidity IgG antibodies; however, it should be taken into account that vaccinated individuals, in case of infection, do not always have a low avidity index of antibodies. IgG. To establish the current infection, in the presence of a rash or established or suspected contact with a patient with rubella, the increase in the IgG antibody titer over time is determined; it is advisable to additionally conduct studies to detect the virus or its RNA.
Screening of pregnant women includes detection of IgM and IgG antibodies to the rubella virus in the blood.
Absence of IgM AT and IgG AT
in a woman in the first trimester of pregnancy indicates the absence of infection, in this case the study is repeated in the second trimester of pregnancy (up to 20 weeks). If the results of two studies are negative, further monitoring is not carried out unless there are other indications for examination (contact with a patient with rubella or suspicion of it; presence of a rash).
Presence of IgM AT and absence of IgG AT
IV at any stage of pregnancy often indicates infection, but a false positive test result should be excluded. For this purpose, it is advisable to determine IgM antibodies to individual proteins of the rubella virus using immunoblot and analysis for the rubella virus by PCR (detection of virus RNA). The presence of viral RNA indicates viremia and confirms the diagnosis of rubella. It is also advisable to examine blood serum over time after 7–10 days: re-detection of IgM antibodies and the appearance of IgG antibodies or a significant (4-fold) increase in the concentration (titer) of IgG antibodies will indicate a current infection.
Absence of IgM AT and presence of IgG AT
– to exclude (confirm) a primary infection, the identification of low-avidity IgG antibodies is important. In this case, the indication of vaccination against rubella or contact with a person with rubella or suspected of it should be taken into account. However, in vaccinated women, in case of infection, the diagnostic value of this test is reduced (a low avidity index is not always observed). To establish the current infection, the increase in the IgG antibody titer over time is determined.
If a pregnant woman develops a disease similar to rubella , or in case of contact with a sick person, the woman must be examined as soon as possible. Recognizing inapparent rubella is a difficult task. The only way to identify asymptomatic forms is laboratory diagnosis - detection of the rubella virus or RNA, IgM antibodies and an increase in the titer of IgG antibodies to the rubella virus in the blood.
When interpreting laboratory results, the following factors should be considered:
- the incubation period - from the moment of contact until the appearance of a rash or detection of AT - is 14–21 days;
- Prolonged application of a tourniquet when drawing blood and a poorly mixed blood sample lead to incorrect results
When assessing the result of determining specific antibodies to the rubella virus in the blood, the woman’s immunization before pregnancy should be taken into account.
Interpretation of laboratory results during the first 10 days from the first day of contact or 4–5 days from the onset of illness:
- There is no rubella virus RNA and/or IgM AT in the blood and IgG AT is present - there is a high probability that the woman has had rubella in the past or has been vaccinated. Contact with the patient does not pose a threat to the fetus. However, to exclude laboratory errors, it is advisable to repeat the examination after 7–10 days. Absence of rubella in a pregnant woman - repeated receipt of the same results (provided there is no increase in IgG titer). Presence of rubella in a pregnant woman - upon re-examination, IgM antibodies were detected, the titer of IgG antibodies increased, or low-avidity IgG antibodies appeared. As confirmation, it is advisable to test the blood for the presence of viral RNA; a positive result indicates viremia.;
- IgM and IgG antibodies were not detected in the blood; the biomaterial should be examined to identify the virus or its RNA. Positive results of detection of the virus or its RNA confirm the diagnosis of rubella, negative results exclude it. It is also recommended to conduct a control blood test after 7-10 days - detection of IgM antibodies to the rubella virus in the blood; a repeated positive result gives grounds for concluding that rubella is present. To exclude false-positive research results, it is advisable to determine IgM antibodies to individual rubella virus proteins using immunoblotting.
Laboratory diagnosis of rubella in the fetus is relevant only if the disease develops in a pregnant woman in the first 17–20 weeks of gestation and is advisable only in doubtful cases or when there is evidence of reinfection with the rubella virus. For prenatal diagnosis, detection of the virus in cell culture or detection of viral RNA by PCR in amniotic fluid, chorionic villus biopsies and placenta, and fetal blood obtained during cordocentesis is used.
Laboratory diagnosis of rubella in newborns
includes determination of IgM AT in umbilical cord blood and newborn blood. Detection of viral RNA in placental tissue increases the likelihood of infection of the child, but its absence does not exclude the diagnosis and requires examination of the child to detect viral RNA and/or specific antibodies. The absence of AT in the neonatal period indicates the exclusion of the diagnosis of congenital rubella, however, in the case of immunological tolerance, the result may be false negative. Additional studies of the biomaterial to detect the virus in cell culture or viral RNA by PCR are advisable. Subsequent examination of children under 1 year of age includes determination of IgM and IgG antibodies. Detection of IgG indicates a high probability of congenital infection.
Criteria for congenital infection:
- isolation of the virus or its RNA from the contents of the nasopharynx, urine, CSF in the first three months of life;
- detection of IgM antibodies from umbilical cord blood shortly after birth;
- the presence of antibodies to rubella before the age of 6 months, especially against the background of corresponding clinical manifestations, since newly acquired infection does not occur in early childhood.
Indications for examination
An infectious diseases specialist, pediatrician, gynecologist, or therapist may prescribe similar testing:
- For a woman planning pregnancy.
- In case of lymphadenopathy or small-spotted rashes in a pregnant woman, if immunity to the rubella virus was absent or not tested.
- Deciding the issue of vaccination.
Testing is performed in adult patients in the presence of severe symptoms of pathology (for example, an increase in the size of the cervical, postauricular, occipital lymph nodes, a characteristic rash, fever).
Newborns born from a sick mother with existing developmental defects are subject to examination, which indicates fetal infection (deafness, central nervous system disorders, cataracts, pathologies related to the functioning of the heart and blood vessels). Antibodies of the IgG class, like IgM, to the rubella virus are fully formed several weeks after infection, so children are diagnosed again after a short period of time.
Signs and symptoms
Since the severity of rubella tends to increase with age, it is advisable to obtain an IgG positive effect as early as possible.
The disease in young children often goes unnoticed and this can make diagnosis difficult.
In the severe form, typical symptoms include: swollen glands or lymphadenopathy, fever not exceeding 38 degrees, rashes, peeling, dry skin, cold symptoms, joint pain, swelling and loss of appetite. A maculopapular rash begins on the face and lasts from 12 hours to several days. The patient is contagious for about 1 week before obvious signs appear and for about the same amount of time after that.
Complications are rare, but rubella encephalopathy (headache, nausea, lethargy, convulsions) occurs in about 1 in 6,000 cases. Such a development of events is possible several days after the rash and, in the worst case scenario, death can occur. Other rare diseases caused by an underlying infection include orchitis, neuritis, and subacute sclerosing panencephalitis (SSP).
In 1941, among the discoveries of congenital rubella syndrome, a link was discovered between severe birth defects and the occurrence of rubella in pregnant women in the 1st trimester.
T-cell immunity plays an important role in the restoration of the body. IgM continues to circulate through the vessels for up to a year after rubella. IgG antibodies give a positive response in the same way as group A immunoglobulins in case of infection. However, their distribution throughout the body has completely different timing.
General information about antibodies
Rubella is a contagious infection that can create stable immunity in the human body. The task of laboratory screenings (tests) is to directly detect the virus in the patient’s bloodstream and determine immune defense factors.
Conventionally, antibodies formed against the rubella virus are divided into IgG and IgM immunoglobulins. These are special compounds of a protein nature. They have a certain structure, thanks to which they accurately recognize and destroy pathogenic agents.
Interaction with the virus or vaccination with further lifelong immunity is indicated by the presence of IgG antibodies. In newborns, a positive test for IgG antibodies to rubella means that the mother transmitted them during intrauterine development through the placenta, and the baby has immunity to the disease for the next six months. But the presence of IgM indicates congenital infection during uterine development.
IgM immunoglobulins are recorded during rubella infection and its initial or acute course. They are produced more actively in the acute period of the disease, and reach their maximum amount after two to three weeks. Often, immunoglobulins of this class are destroyed within one to two months after recovery, although they are sometimes observed in the body for another 6-12 months.
Important! During the primary acute stage of infection, a test for the presence of IgM antibodies to rubella is required. In this case, at least two to three weeks must pass from the moment of infection.
When is testing done?
In women who have symptoms suggestive of rubella , whether they are pregnant or not, a test is performed to detect IgG and IgM antibodies. Assessment of IgG and IgM antibody levels is mandatory in pregnant women who develop fever, rash and/or other symptoms that may indicate rubella.
Tests for the presence of IgG and IgM antibodies against rubella may also be performed in a newborn suspected of being infected with rubella virus or having birth defects that may indicate rubella (deafness, cataracts, cardiovascular disorders, central nervous system disorders).
Since the development of IgG and IgM antibodies against rubella requires a certain time from the moment of infection, the test should be repeated after 2-3 weeks.
Sometimes a test for IgG antibodies against rubella is performed to confirm resistance to infection with the virus. This may be required by healthcare workers.
Rules for passing and diagnostic methods
In any laboratory equipped with the necessary equipment, you can get tested for rubella (both private and public). Venous blood is required for the examination. If testing is carried out on newborns, then biomaterial is collected from the umbilical cord.
Screening for rubella antibodies is performed in the morning. The subject should not have breakfast (it is allowed to drink a little boiled water). 24 hours before going to the laboratory, he needs to refrain from consuming fatty foods and alcoholic beverages. You should also avoid physical overload, visiting baths and saunas. Three hours before the test you should not smoke.
Several methods are used when testing blood for rubella to detect antibodies of the IgG and IgM classes:
- Serological method . Detects the presence of protein compounds in blood plasma, but does not specify their type and class.
- Polymerase chain reaction (PCR) is a method that allows you to identify the virus before the clinical manifestation of the disease. The presence of the “positive” value indicates the presence of viral RNA in the body and the infection of a person.
- Enzyme immunoassay that determines the avidity of IgG antibodies to the rubella virus and their type.
A correct and reliable test for rubella in women during pregnancy and in persons with suspicious symptoms is deciphered by the attending physician. It takes into account not only the obtained indicators, but also other additional factors, including external manifestations.
Important! Medications can affect screening rates, so you should donate blood only two to three weeks after you finish taking them. If an urgent examination is necessary, the doctor must know which drug was taken and in what dosage.
Antibodies
These are proteins that the immune system produces to help fight various foreign invaders in the body and prevent you from getting sick. Each of them is aimed at a specific invader and immediately reacts to it, beginning to multiply intensively.
- IgM is the first class of substances that notice the virus. They can be found in the blood from 7 to 10 days after infection in adults and up to a year in newborns. You will have to take this test if your doctor thinks you are infected.
- IgG stays in your body forever. The presence of substances of this class indicates that you have been vaccinated or have suffered from a disease and will no longer be able to get it.
You will need to do both tests if you are planning to become a mother. If there is a suspicion of rubella, after the baby is born, he will also have to be tested for the presence of the virus.
Decoding
Having been tested for rubella antibodies if she is pregnant or planning a pregnancy, a woman can receive the following answers:
- IgG and IgM are negative - this means that the body does not have the Rubella virus and has never encountered it. Here you need to get vaccinated, after which you cannot become pregnant for three months. If a woman is already pregnant, then she should avoid contact with sick people, and take a control test again until the 20th week.
- IgG positive, IgM negative - observed when the infection continues to attack the body or synthesized antibodies in the blood continue to circulate due to long-standing vaccination. To determine the situation, the analysis will need to be retaken in three weeks. If the activity of immunoglobulins continues to increase, then this is a chronic form of the pathological process that requires immediate treatment. If the indicators remain unchanged, then the person has already had rubella and will not become infected with it again: he does not need vaccination.
- IgM positive, IgG negative . Indicates the onset of the disease. A woman should refrain from pregnancy until complete recovery. If she is already expecting a child, then she should test the blood using the PCR method or repeat the enzyme immunoassay after 14 days.
- IgG and IgM are positive . This means that infection has occurred and the person needs appropriate treatment. You will have to wait at least three months to become pregnant. Increased levels of antibodies to rubella IgG and IgM are observed in the acute nature of the disease. In this case, patients complain about its external signs. Here we can talk about artificial termination of pregnancy.
Laboratory examination of the fetus is relevant only if a pregnant woman who has not previously been ill is infected or in the event of reinfection in the first trimester of pregnancy.
Decoding research results
Suppose that, as a result of the study, you were given a paper on which it was written: “Rubella: IgG positive.” What does it mean? The fact that in the past you have already come into contact with the infection in one way or another and now you will never get sick again.
In the negative version of the same immunoglobulin, there is no doubt that the person has never encountered this virus before and is capable of catching it at any time.
If class M antibodies are found in the blood, this confirms the active form of the disease. Otherwise, when these substances are not found, the person does not have a current infection.
When samples are taken for both types of proteins and the results indicate that IgG is positive for the rubella virus and IgM is negative, then there is nothing to worry about. You suffered from the disease at an earlier age and, together with your unborn child, are completely safe.
Pregnancy examination
The expectant mother will have to conduct a comprehensive analysis for the presence of antibodies to the herpes virus, rubella, toxoplasmosis and cytomegalovirus immediately after registering with a gynecologist. Refusing such an important examination is not only inappropriate, but also irresponsible. After all, these infections, when initially introduced into the body, can penetrate the placental barrier and infect the developing fetus, which is fraught with congenital deformities.
It is advisable to undergo a rubella test when planning a pregnancy, but not all women pay due attention to this stage of family life. As a rule, they donate blood while already pregnant.
Indications for analysis
Indications for prescribing a rubella test are the following circumstances and symptoms:
- planning pregnancy or early pregnancy;
- finely spotted rash and lymphadenopathy that occurred during pregnancy (in the absence of immunity to rubella or the results of relevant tests);
- symptoms of intrauterine infection and placental insufficiency;
- the presence of clinical signs of the disease (lymphadenopathy in combination with a small-spotted rash, enlarged lymph nodes on the back of the head, behind the ears, on the back of the neck, etc.).
Control and processing
Rubella is typically a mild illness and no specific treatment is usually required. Rest and drinking plenty of water usually relieves symptoms. Acetaminophen and aspirin can be used to reduce fever and inflammation.
People remain contagious for about a week after the rash appears and should be isolated from school, work, and contact with people who have not previously had the disease. Treatment for CRS depends on the type of complication and is prescribed by a doctor.
We found out how dangerous the disease is for pregnant women, how important timely diagnosis of rubella is and what it means - IgG positive when receiving the results of the study. Listen to your doctor’s advice, don’t be lazy to take extra precautions, and then you will be able to avoid many problems with your health and that of your unborn baby.
Prevention and treatment of the disease
Epidemiological measures to prevent the disease include isolating the patient from the moment the elements of the rash appear on the skin for 5 days. It is especially worth limiting contacts of virus carriers with pregnant women. Special quarantine measures are not used in the children's group.
Treatment of rubella is nonspecific, since there is no etiotropic therapy. Treatment is carried out on an outpatient basis; the following groups of patients are subject to hospitalization:
- children with severe background pathology;
- patients with immunodeficiency;
- children with congenital rubella;
- patients with complicated rubella.
Treatment includes the use of antipyretics, local medications, antihistamines, and vitamins. Also, compliance with the regime is important, the patient must be at rest, the menu must be diversified with products that contain vitamins and microelements. Sufficient drinking regime is recommended. In some cases, antibacterial drugs are used if a corresponding infection has occurred.
Modern methods of diagnosing the disease
Clinical diagnosis is based on assessing the patient’s condition; the doctor examines the rash, performs auscultation and percussion, examines the skin and visible mucous membranes. A general blood test does not provide specific data; it can only be used to determine the presence of inflammation, as well as establish the fact that it is of a viral nature.
Laboratory diagnostics includes:
- Serological method (RSK, RTGA, RIF, ELISA, IgM, IgG);
- Virological method;
- PCR.
Let's take a closer look at the methods for diagnosing the disease.
The first serological diagnostic method used to diagnose rubella
- neutralization reaction. Specific antibodies neutralize the virus, which means that the pathogenic effect of the pathogen does not occur in a sensitive culture. The technique is used to confirm the authenticity of the viral microorganism.
There is also a hemagglutination inhibition reaction. This technique is somewhat simpler technically. The essence of the method is that specific serum delays the hemagglutinating effect of the antigen. For accurate diagnosis, the method of paired sera is used to study the antibody titer and its increase. Material for research is collected at intervals of two weeks. An important point is that the analysis must be carried out if no more than 10 days have passed since contact with a carrier of the virus. The technique is used to make a diagnosis, to examine immunity in the population, and is an auxiliary method in the development of therapy. This is the “gold standard” in diagnostics, since the analysis data is accurate and reliable.
Linked immunosorbent assay
- the most specific and sensitive method, which at the same time is quite simple in technical terms. The advantage of the technique is the possibility of diagnosis in one day, since there is no need to study paired sera. It is also the “gold standard” in the diagnostic scheme. There are various modifications of this diagnostic method, such as indirect or antibody capture assays.
Immunofluorescence reaction
is based on the property of immunological complexes to bind to fluorescent elements. As a result, staff see this as glowing areas. The technique is sensitive, provides reliable data and is often used to confirm the diagnosis.
The complement fixation reaction technique involves detecting a specific type of antibody that has special properties. Such antibodies can be detected when 3 years have passed since the person suffered the disease. Thus, the diagnosis is used to prove the fact that the patient has already had rubella before.
Virological diagnostics
rubella is aimed at identifying the virus in swabs from the mucous membranes of the respiratory tract, in the cerebrospinal fluid, urine, discharge from the conjunctiva. It is used quite rarely, since this procedure requires a lot of time and special laboratory conditions.
Polymerase chain reaction
is the most accurate and modern diagnostic method, as it allows you to determine the presence of sections of the nucleic acids of the virus, which allows you to 100% assert that the cause of the disease is the rubella virus.
Differential diagnosis is carried out with the following pathologies: measles, chicken pox, scarlet fever, infectious mononucleosis, pseudotuberculosis. These pathologies are united by the presence of exanthema - rashes on the skin. A thorough examination of the nature of the rash, clinical manifestations, examination of the lymph nodes, and detection of specific signs of pathology are carried out. An accurate diagnosis allows you to carry out the necessary epidemiological measures, select treatment tactics, and determine the need for hospitalization.
How to prepare for testing
For rubella, the biometric material is blood from a vein. Take it on an empty stomach; in the morning you can only drink water. The day before the test, it is strictly forbidden to drink alcohol or fatty foods. It is also not recommended the day before donating blood to go to a sauna, steam bath or other procedures that significantly increase body temperature. It is better not to overwork yourself physically on the eve of the test.
You need to donate blood no earlier than 2 weeks after the drug course of treatment. Medications may affect results. If the study is urgent, then you need to notify the doctor about this, indicating the drug you are using and the dosage.