The human body has a rather complex, but impeccably thought-out structure, and the effective and healthy functioning of all systems is possible only if the basic parameters of blood and other fluids are normal.
LDL (low-density lipoprotein) or so-called “bad cholesterol” is no exception.
Timely detection of abnormal lipoprotein levels and proper treatment will prevent serious cardiovascular diseases such as myocardial infarction, stroke or atherosclerosis. Therefore, in this article we will tell you what LDL is, how to diagnose them, and what to do if their level is significantly higher than normal.
LDL (LDL) - what is it in a biochemical blood test?
LDL / LDL (or Low-Density Lipoproteins) are microparticles / protein complexes in the blood plasma (sizes from 18 to 26 nm), the main task of which is to “transport” cholesterol, triglycerides and phospholipids from the liver to peripheral tissues. Initially, they are formed from VLDL / Very Low Density Lipoproteins (during the process of lipolysis / “breakdown”), and then they are transported throughout the body - many vital / important substances. Including cholesterol, triacylglycerides (“energy source” for humans), vitamin E and others.
LDL structure: apolipoprotein B100 (98%), proteins (21-25%), phospholipids (22-24%), triglycerides (10-12%), cholesterol (35-45%)
Another very important “mission” of LDL (as recently proven by Danish/German scientists) is the “neutralization” of poisons secreted by – deadly/life-threatening – bacterial toxins. For example, even those contained in snake or spider venom.
However, despite the many useful features, there is also a downside to the coin. In fact, being a fatty (and therefore “sticky”) alcohol, LDL cholesterol (i.e. cholesterol in low-density lipoproteins) first “sticks” to the walls of blood vessels and then penetrates inside. After which (as a result of other, in fact, defensive reactions), it gradually “gets stronger,” layers, and forms “slides,” which are commonly called “cholesterol plaques.” (See VIDEO AT BOTTOM OF PAGE - 43 sec
). It's better to see once than to hear (or read) 100 times!
That is why LDL cholesterol is considered “BAD” and “harmful”. Unlike HDL cholesterol (high density lipoprotein)
, which scientists call “GOOD” cholesterol. Because its main task (initially, being an “empty taxi”, as American doctors put it) is to “pick up” excesses of the former (i.e. LDL cholesterol) in the blood and “take” it “home” - back to the liver (for processing or - disposal).
Functions in the human body
Blood lipoproteins perform certain duties in the human body that you should know about:
- construction of cell membranes, maintaining their permeability, elasticity and strengthening;
- increasing the body's defenses, improving the functioning of the immune system;
- full participation in the formation of steroid and sex hormones (estrogen, cortisol);
- converting sunlight into vitamin D;
- taking part in the formation of bile.
LDL also protects the nervous system and nerve fibers from the negative effects of stress, overexertion, and overexcitation. Substances are more beneficial to the human body, but only if their concentration is within normal limits.
Formula for calculating LDL cholesterol levels
In most clinical laboratories, the level of LDL cholesterol (or more precisely, the amount of low-density lipoprotein cholesterol) is determined by a calculation method. At the same time, experts use the Friedwald formula, substituting into it the indicators of the “standard” LIPIDOGRAM
.
That is, TC (Total Cholesterol), HDL cholesterol (the amount of high-density lipoprotein cholesterol) and TG ( TRIGLYCERIDE level)
.
As for the last indicator (that is, TG), it is necessary for laboratory staff (specifically, in this case) to calculate the amount of VLDL cholesterol.
So, Friedwald’s formula/equation (by the way, developed back in 1972) looks like this:
By the way, you can use the ONLINE CALCULATOR
on our website!
- LDL cholesterol (mg/dl) = TC (mg/dl) – HDL cholesterol (mg/dl) – VLDL cholesterol (mg/dl) *
- LDL cholesterol (mmol/l) = TC (mmol/l) – HDL cholesterol (mmol/l) – VLDL cholesterol (mmol/l) **
Where the amount of VLDL cholesterol is calculated by dividing the triglyceride value (TG) by 5 or 2.2 (depending on the unit of measurement):
- * VLDL cholesterol (mg/dl) = TG (Triglycerides): 5
- ** VLDL cholesterol (mmol/l) = (Triglycerides): 2.2
IMPORTANT NOTE:
This calculation method is NOT (!) used if the level (TG) of triglycerides is more than 4.5 mmol/l (or 400 mg/dl).
LDL calculation using the formula
LDL-Cholesterol (Low-density lipoprotein cholesterol, LDL)
A fraction of lipoproteins involved in the transport of cholesterol from the liver to other tissues.
Low-density lipoproteins (LDL) are the main transport form of cholesterol. LDL belongs to p-lipoproteins, their formation occurs in the liver and small intestine. In the blood, LDL transports lipids, including cholesterol, from one cell population to another.
It is believed that LDL is more correlated with the risk of atherosclerosis than the level of total cholesterol, since it is this fraction that ensures the flow of cholesterol to blood vessels and organs.
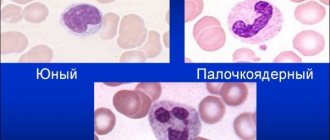
In conditions of vascular endothelial pathology, which is facilitated by various factors (high blood pressure, components of tobacco smoke coming from smoking, increased homocysteine levels), LDL is captured by the cells of the vascular walls, modified under the influence of local inflammatory factors and included in the resulting atherosclerotic plaques, which narrow the lumen of blood vessels and promote thrombosis. The main risk factors for the development of atherosclerosis include age (over 45 years for men and over 55 years for women), heredity (cases of myocardial infarction or sudden death in men under 55 years of age or women under 65 years of age), smoking, hypertension, and diabetes mellitus. In the presence of at least one of these risk factors, the recommended (desirable) values of LDL cholesterol in the blood serum - 4.14 mmol/l is regarded as a high risk of developing atherosclerosis and coronary heart disease.
Why is it important to control LDL cholesterol?
LDL-C correlates more closely with the risk of atherosclerosis and coronary artery disease than the level of total cholesterol. LDL-C can be determined by calculation using the Friedwald formula:
LDL-C = Total cholesterol - HDL-C - TG/2.2 (mmol/l)
The atherogenicity of cholesterol is primarily determined by its belonging to a particular class of drugs. In this regard, special attention should be paid to low-density lipoproteins (LDL), which are the most atherogenic for the following reasons.
LDL transports 2/3 of total plasma cholesterol and is the particle richest in cholesterol, the content of which in them can reach up to 45 - 50%. By determining beta-cholesterol, we actually determine the cholesterol content of LDL.
The particle sizes (their diameter is 21 - 25 nm) allow LDL, along with HDL, to penetrate the vessel wall through the endothelial barrier, but unlike HDL, which are easily removed from the wall, facilitating the removal of excess lipids, LDL are retained in it because they have a selective affinity for glucose-aminoglycans and smooth muscle cells. The latter is explained, on the one hand, by the presence of apo-B in LDL, and on the other, by the existence of receptors for this apoprotein on the surface of the cells of the vessel wall. For these reasons, LDL is the main transport form of cholesterol for the needs of the cells of the vascular wall, and under pathological conditions, it is a source of its accumulation in the vessel wall. That is why in type II hyperlipoproteinemia (HLP), characterized by high levels of beta-cholesterol, relatively early and pronounced atherosclerosis and ischemic heart disease are often observed. The definition of LDL-C is very informative, and a deviation of this indicator from the norm may with a high degree of probability indicate the degree of danger of developing atherosclerosis and coronary artery disease.
For what diseases is LDL cholesterol used?
Indications for the purpose of analysis:
Atherosclerosis and related diseases of the cardiovascular system: coronary heart disease, myocardial infarction (risk assessment, diagnosis, prognosis).
Screening examinations (as part of other lipid profile tests).
How to prepare for an LDL cholesterol test?
Blood collection should be done in the morning strictly on an empty stomach, 12-14 hours after the last meal.
Increases in the norm are observed in the following cholesterol diseases - LDL
Increasing values:
Primary hereditary hypercholesterolemia (hyperlipoproteinemia types IA and IIB), tendon xanthoma, previous damage to the coronary vessels.
Nephrotic syndrome, chronic renal failure.
Taking medications (ß-blockers, diuretics, progestins, oral contraceptives, glococorticoids, androgens).
A diet rich in saturated fat and cholesterol.
Decreases in the norm are observed in the following cholesterol diseases - LDL
Decrease values:
Primary disorders of lipid metabolism: hypobetaproteinemia, abetaproteinemia, alphalipoprotein deficiency, LCAT deficiency (lecithin cholesterol acyl synetatase), hyperlipoproteinemia type I, lipoprotein lipase cofactor deficiency.
Chronic lung diseases.
Taking medications such as cholestyramine, clofibrate, lovastatin, neomycin, interferon, thyroxine, estrogens.
A diet low in saturated fats and cholesterol, rich in polyunsaturated fatty acids.
Determination method Calculation using the Friedwald formula using total cholesterol, HDL cholesterol and triglycerides. Test material: Blood serum. Lipoproteins in the blood transport various classes of lipids, including cholesterol, from one cell population to another.
Low-density lipoprotein LDL is the main transport form of cholesterol, transporting it primarily in the form of cholesteryl esters. They belong to beta lipoproteins.
It has been proven that the level of LDL cholesterol is more correlated with the risk of atherosclerosis than the level of total cholesterol, since it is this fraction that ensures the transfer of both dietary and synthesized cholesterol to the cells of organs and tissues.
Search data for your request:
Go to search results >>>
WATCH THE VIDEO ON THE TOPIC: What is the profitability indicator, formula? ROI
BioximiaForYou
Determination method Calculation using the Friedwald formula using total cholesterol, HDL cholesterol and triglycerides. Test material: Blood serum. Lipoproteins in the blood transport various classes of lipids, including cholesterol, from one cell population to another.
Low-density lipoprotein LDL is the main transport form of cholesterol, transporting it primarily in the form of cholesteryl esters. They belong to beta lipoproteins.
It has been proven that the level of LDL cholesterol is more correlated with the risk of atherosclerosis than the level of total cholesterol, since it is this fraction that ensures the transfer of both dietary and synthesized cholesterol to the cells of organs and tissues.
Subfractional blood test (LDL-P / LLP-C)
It is definitely worth noting that in modern medicine there is another blood test that concerns strictly low-density lipoproteins (i.e. LDL). Its formal name is “subfractional lipid profile.” In principle, in itself, it is the “classical” blood test for LDL cholesterol (as part of the “standard” lipid profile) that can indicate the risks of developing CVD (cardiovascular diseases) quite well. However, according to the results of recent studies, scientists have found that some patients still have a high risk of CVD, even with NORMAL LDL cholesterol levels!
Likewise, people with other chronic diseases (such as type 2 diabetes) can also have healthy LDL cholesterol levels. Thus, in the future, it was decided for certain cases to take into account - NOT (!) the concentration of cholesterol within the LDL fraction, but the number and size of LDL microparticles/compounds (sdLDL). Which, circulating through the circulatory system, can change their shape: from fluffy and large to small and dense. At the same time, the latter, to a greater extent, are the main “culprits” for the development of atherosclerosis.
The official name (in foreign countries) of this blood test/test is: “Low-Density Lipoprotein Subfraction Profile”.
Indications for a blood test for LDL cholesterol
To determine the amount of low-density lipoprotein, a biochemical blood test or lipid profile is performed.
Laboratory testing must be completed:
- Patients suffering from diabetes of any degree. Insufficient insulin production has a negative effect on the entire body. The heart and blood vessels suffer, memory deteriorates. An increased concentration of low-density lipoproteins only aggravates the situation.
- If a blood test reveals elevated cholesterol, a lipid profile is additionally prescribed to determine the ratio of HDL and LDL.
- Persons with a family predisposition to heart and vascular diseases. If you have relatives suffering from atherosclerosis, coronary syndrome, or having had a myocardial infarction or micro-stroke at a young age (up to 45 years).
- For problems with blood pressure, hypertension.
- People suffering from abdominal obesity caused by poor diet.
- In cases of signs of metabolic disorders.
- It is advisable for persons over 20 years of age to undergo examination every 5 years. This will help to identify the first signs of atherosclerosis, heart disease with a genetic predisposition.
- People with coronary artery disease, after a heart attack or stroke, should undergo an extended blood test once every 6-12 months, unless otherwise prescribed by a doctor.
- For patients undergoing drug or conservative treatment to reduce LDL - as a control of the effectiveness of therapy.
When is a blood test (study) prescribed?
A biochemical blood test for LDL cholesterol, being part of a “regular” lipid profile, is primarily prescribed to adequately assess the risks of developing atherosclerotic CVD (i.e., cardiovascular disease). Since, in comparison with all other fractions of cholesterol, it is LDL cholesterol, being in excess, that is considered “undesirable” (or “bad”). Since its “excess”, (gradually) accumulating in the walls of blood vessels, forms “atherosclerotic plaques”
. These formations, somewhat similar to “growing mountains,” not only interfere with normal blood flow, but can also clog blood vessels. And this is fraught with a heart attack, gangrene of the limbs or a stroke.
Next, the doctor decides on the best method of treatment (depending on the borderline
or
a high
amount of LDL cholesterol in the blood plasma, as well as the presence of
other risk factors - they are described just BELOW
).
And, accordingly, controls its effectiveness. The most effective treatment options are some lifestyle changes (giving up bad habits, special diets and exercise therapy/physical therapy). As well as taking lipid-lowering drugs (ATC code C10), for example, STATINS
.
When prescribing the latter, treating specialists will be sure to monitor their effectiveness using a repeat blood test (LDL cholesterol) after 4-12 weeks
(from the start of drug therapy), and then
every 3-12 months
.
MAIN RISK FACTORS
development of CVD (except for high levels of LDL cholesterol):
- smoking (especially “red” tobacco products with a high content of nicotine and tar);
- overweight (with a BMI of 25 and above, according to WHO) or obesity (with a BMI of 30 and more), find out your BMI using the ONLINE CALCULATOR
; - “unhealthy” diet (with an excess of trans fats, animal fats and other foods that increase “bad” cholesterol
); - inactive / “sedentary” lifestyle or physical inactivity (“sedentary work” or other restrictions on physical activity);
- the age of the person (men – from 45 years and older, women – from 55 years and more);
- hypertension/arterial hypertension (high blood pressure syndrome ≥ 140/90 mmHg);
- family history of premature CVD (in 1st degree relatives, i.e. in fathers - up to 55 years old and mothers - up to 65 years old);
- Previous experiences – heart attack or ischemic heart disease (coronary heart disease);
- Type 2 diabetes or pre/diabetes.
NOTE:
HDL cholesterol levels - from 1.55 mmol/l (60 mg/dl) and above, according to the provisions of NCEP (2002), are considered a “negative risk factor”, which makes it possible to exclude from the total one of the above/listed risk factors .
Preventive blood tests for adult men and women
In many foreign countries, a biochemical blood test for LDL cholesterol levels (LDL-C) may be prescribed (as part of a lipid profile) during a mandatory/regular medical examination. According to NCEP recommendations (ATP III), all adult men and women without CVD risk factors (listed ABOVE) should undergo such tests every 4-6 years
.
At the same time, for people who do have 1 or more major risk factors, a blood lipid profile (fasting) can be prescribed MORE FREQUENTLY (at the discretion of the “family doctor”). In addition, it is always prescribed (by the way, both here and in foreign countries) when a general blood test (finger prick) shows elevated cholesterol (C). That is, doctors need it in order to check: is the level of total cholesterol (i.e. Total Cholesterol) high - precisely because of the increased amount of LDL cholesterol?
Blood test for LDL cholesterol for preventive purposes for adolescents and children
For example, in the USA and Canada, according to the recommendations of the AAP (American Academy of Pediatrics), children undergo a lipid profile at 9-11 years of age
(i.e. during the transition to adolescence).
And one more time, as boys and girls, from 17 to 21 years
.
Of course, earlier (and more frequent) comprehensive studies of the blood lipid spectrum can be prescribed - both for children and adolescents who have an increased risk of developing CVD. At the same time, they are exactly the same as in adults. Statistics have shown that the most common problems (from this list) are premature cardiovascular diseases in their parents (fathers and mothers), as well as diabetes, hypertension and obesity. In addition, even very young children with increased risks of CVD should also undergo a lipid profile between the ages of 2 and 8 years
. A child under 2 years old is still too young for such an analysis.
Reasons for the increase
Diseases and pathological conditions can cause LDL levels to increase:
Diseases of the liver, as well as kidneys or gall bladder. disorders of the thyroid gland, diabetes of both types and cancer are common causes. Obesity and alcoholism, Anorexia nervosa.
However, as already mentioned, you should not immediately panic if your lipid profile shows high LDL. There are also possible harmless causes of a temporary self-removing nature, such as:
pregnancy, eating large amounts of animal food, smoking, frequent alcohol consumption, taking certain medications.
In addition, these circumstances sometimes cause the “good” HDL cholesterol to be elevated.
Symptoms
How can an ordinary person who does not suffer from any chronic diseases understand that LDL cholesterol and its norm are exceeded?
It is necessary to understand that the first symptoms that the gaps in the blood vessels are narrowing will appear only when this same gap decreases by at least 70%. Before this value, you may not feel anything at all, and only a timely lipid profile can indicate that there are health problems and bad cholesterol exceeds the norm. Symptoms are usually:
chest pain, leg pain (Charcot's syndrome), xanthomas on the skin.
The last symptom is benign skin growths consisting of fatty tissue. These tumors most often form in the tendon area, as well as on the hands and feet, and have a pinkish or yellowish tint. Their formation is mostly influenced by cholesterol.
Sometimes a change in the cornea of the eyes is observed: in this case, yellowing of its rim can be detected.
Danger
Everyone probably knows that bad cholesterol is deposited in the form of plaques on the walls of blood vessels. Such accumulations of fat-like substance greatly impede blood flow, as they narrow the lumen in the vessels. Due to the fact that blood cannot actively flow, plaques form with even greater intensity, slowing down the blood flow even more: a kind of vicious circle is obtained.
As a result of this process, the blood vessels are severely damaged. This can lead to various heart diseases (angina), including myocardial infarction. But this is already an extreme situation, and at the beginning of the pathological process of the formation of cholesterol plaques, a person experiences the following symptoms:
headache, blurred vision, dizziness.
If you do not pay attention to these symptoms in time and do not start treatment, the patient may even risk a stroke.
You should know that the initial stage of excess LDL cholesterol is usually asymptomatic, and only a blood test in the form of a lipid profile can show that the pathological process is developing. That is why it is recommended to take a lipid profile test every 5 years before the age of 50 (if there is no direct indication), and after 50 years - every year. This applies to both men and women, even if there are no external reasons or indications.
By the way, if men are more at risk of heart attacks and strokes as a result of the pathological process, then women are more likely to suffer from coronary heart disease. Elevated LDL is especially dangerous for women when they enter menopause. At this time, bad cholesterol begins to be deposited on the walls of blood vessels especially actively.
Very often, elevated LDL cholesterol leads to diseases such as:
coronary artery disease (CAD), chronic renal failure, obesity, nephrotic syndrome, etc.
Elevated LDL can also indicate the development of the following diseases in the body:
diabetes mellitus, anorexia nervosa, hypothyroidism, Cushing's syndrome.
During pregnancy, blood tests often show elevated cholesterol levels. However, in this case, this is not a pathology, but a completely natural, normal process. And after the birth of the child, in most cases, everything returns to normal. This phenomenon during pregnancy is explained by the need to produce more female sex hormones necessary for the full development of the fetus.
How to properly prepare for a lipid profile
As a rule, a biochemical analysis of the blood lipid profile (spectrum) is taken on an empty stomach. However, according to the doctor’s decision (especially for young people / without the atherogenic risk factors for CVD listed above), this analysis can be performed without a “hunger strike”. That is, without preliminary/complete refusal of food 9-12 hours before donating venous blood. You can only drink plain water (not sweet/carbonated). Immediately before the lipid profile (30-40 minutes), it is not recommended to: SMOKE and over/exert yourself (both physically and emotionally). In most laboratories, before drawing blood (from a vein), the person is allowed to sit in silence and complete calm for at least 5 minutes.
What could negatively affect the results?
Undesirable distortions in the results of a blood test for LDL cholesterol (or low-density lipoprotein cholesterol) can occur for the following reasons:
- incorrect body position (during collection of venous blood, usually by inexperienced laboratory staff);
- donating blood immediately after an exacerbation of any disease, heart attack, surgery (to obtain true results, you must wait another 6 weeks);
- “stormy” holidays the day before (saturated with alcohol and fatty foods);
- serious stressful situations (divorce, accidents, accidents and even dental visits);
- intense physical activity (related to either heavy physical labor or preparation for sports competitions);
- taking medications, oral contraceptives or “sports” steroids (read: what medications increase plasma cholesterol levels?
); - pregnancy (lipidogram / or blood lipid profile is always prescribed at least 6 weeks after the birth of the child).
Thus, if you find something that is listed above, then immediately notify your doctor, who will prescribe a retake of the blood test in 1-3 months. It is certainly worth noting that the above/listed list is compiled according to statistics (of cases) - both foreign and domestic laboratories.
Normalization of cholesterol levels
There are two ways to return indicators to normal: a course of drug therapy or a transition to a healthy lifestyle. However, the second condition remains mandatory for preventive purposes. The most important thing is that you need to bring LDL cholesterol back to normal under the supervision of a specialized doctor.
Normalizing your lifestyle involves eliminating potential sources of increased cholesterol:
- inactivity;
- a diet with a bias towards food with an abundance of animal fats;
- smoking, alcohol abuse.
Daily physical activity lasting 30–60 minutes will compensate for the lack of mobility for office employees. For older people, activity in the form of light jogging or walking is sufficient.
Balancing your diet is the next task to ensure normal cholesterol levels. This is achieved by replacing foods containing fats and refined carbohydrates with products of plant origin: vegetables, fruits. This does not mean a complete rejection of meat and eggs, but a reduction in their share in the daily diet. If you have elevated LDL cholesterol, consuming baked goods and foods containing trans fats is highly discouraged.
Quitting smoking is important not only from the point of view of normalizing cholesterol levels. This bad habit has a negative effect on the walls of the arteries, further increasing the risks of atherosclerosis with high cholesterol. In addition, if LDL cholesterol is low, the body's immune system is weakened.
Decoding LDL cholesterol indicators
What do the results of a lipid profile (relative to the level of LDL cholesterol in the blood plasma) mean - are they good or bad? What do our doctors use to make their final decision? At the moment, both foreign doctors and domestic specialists use the “old” provisions of the NCEP (National Cholesterol Research Program) commission from 2002 to assess lipid levels (and prescribe treatment). Even despite the newer recommendations of the AAC (American College of Cardiology) and AHA (American Heart Association) from 2013. Which specific people should receive cholesterol-lowering therapies (particularly medications) based on age, CVD, diabetes, gender, race, blood pressure, and elevated LDL-cholesterol (LDL-C).
However, this does not mean that everything is outdated, it’s just that Americans are very careful! Therefore, due to the fact that many of the principles of the new guidance remained controversial, it was decided to return to the NCEP recommendations (ATP III). Until pundits fully understand many things, including the ASCVD (Atherosclerotic Cardiovascular Disease) calculator, used to estimate the “10-year risk of developing atherosclerotic CVD. On the results of which, in fact, the fresh recommendations were based. Although, they still began to do some things in a new way. That is, if previously clinics took into account the “target values” of LDL cholesterol (LDL-C) to reduce the risks of atherosclerotic CVD, then since 2013, many experts rely on their percentage reduction. According to recommendations from the AAC and AHA.
LDL cholesterol levels for adults
So, according to the provisions of NCEP (ATP III) for adult men and women (without CVD risk factors), LDL cholesterol levels are estimated as follows:
- less than 100 mg/dl (2.59 mmol/l) – optimal level;
- 100-129 mg/dl (2.59-3.34 mmol/l) – normal / close to optimal;
- 130-159 mg/dl (3.37-4.12 mmol/l) – elevated / borderline values
- 160-189 mg/dl (4.15-4.90 mmol/l) – elevated/high values;
- more than 189 mg/dL (4.90 mmol/L) is a very high (dangerous) level.
More detailed information about the norms of LDL cholesterol (separately for women and men) depending on AGE is presented BELOW - in separate tables.
You may be interested in: cholesterol standards (IN THE TABLE) IN ALL its fractions
LDL cholesterol indicators for children, adolescents and young people
According to the AAP (American Academy of Pediatrics), LDL cholesterol levels for children and adolescents (without CVD risk factors) aged 2 to 17 years are estimated as follows:
- less than 110 mg/dL (2.85 mmol/L) is an acceptable level;
- 110-129 mg/dl (2.85-3.34 mmol/l) – elevated/borderline values;
- more than 130 mg/dl (3.36 mmol/l) – high level.
Also read (link): CHOLESTEROL IS INCREASED IN A CHILD, WHAT SHOULD BE DONE?
Doctors consider LDL cholesterol indicators for young people (i.e. for boys and girls aged 17 to 21 years) as follows:
- less than 120 mg/dL (3.10 mmol/L) – acceptable level;
- 120-159 mg/dl (3.10-4.11 mmol/l) – elevated/borderline values;
- more than 160 mg/dl (4.12 mmol/l) – high level.
Normal LDL level in men and women
The normal content of LDL in blood plasma is calculated depending on gender and age. It is included in a special table that doctors use in their work. It is noteworthy that the increase in LDL cholesterol occurs differently in men and women.
- In males, the peak of the cholesterol curve occurs at puberty, since the amount of LDL is directly related to the concentration of androgens. As soon as sexual function begins to fade, cholesterol levels will begin to fall (unless there are reasons for hypercholesterolemia).
- In non-pregnant women, the curve is an almost flat line, gradually going upward. Each pregnancy on the cholesterol chart is manifested by a jump in LDL, but this is a physiological process: a few months after the birth of the child, the lipid profile is restored.
The target level of low-density cholesterol varies from birth to old age: by 10 years it reaches 3.3 mmol/l, by 40 – 4.4, and by 70 – 5.5 mmol/l.
During pregnancy, reference values are considered to be 6.6–11.6 mmol/l.
Just a change in normal values is not considered a disease. It can be transient and short-term, not causing pathological processes in the body, or it can be permanent with a tendency to worsen. In the latter case, the imbalance will lead to a certain disease with all its consequences.
LDL cholesterol (LDL-C) - norm in women table (by age)
Below (in the table) the norms of LDL-C / LDL cholesterol (low-density lipoprotein cholesterol) in blood plasma in girls, young women and adult women are presented by age.
| Age (girls/girls/women): | Norm LDL cholesterol (mmol/l) | LDL-C norm (mg/dL) |
| children from 5 to 10 years old | 1.76 – 3.63 | 68.1 – 140.4 |
| 10 – 15 | 1.76 – 3.52 | 68.1 – 136.1 |
| 15 – 20 | 1.53 – 3.55 | 59.2 – 137.3 |
| 20 – 25 | 1.48 – 4.12 | 57.2 – 159.3 |
| 25 – 30 | 1.84 – 4.25 | 71.1 – 164.3 |
| 30 – 35 | 1.81 – 4.04 | 70.0 – 156.2 |
| 35 – 40 | 1.94 – 4.45 | 75.0 – 172.1 |
| 40 – 45 | 1.92 – 4.51 | 74.2 – 174.4 |
| 45 – 50 | 2.05 – 4.82 | 79.3 – 186.4 |
| 50 – 55 | 2.28 – 5.21 | 88.2 – 201.4 |
| 55 – 60 | 2.31 – 5.44 | 89.3 – 210.3 |
| 60 – 65 | 2.59 – 5.80 | 100.1 – 224.3 |
| 65 – 70 | 2.38 – 5.72 | 92.0 – 221.2 |
| over 70 years old | 2.49 – 5.34 | 96.3 – 206.5 |
Also read (link): about CHANGES IN CHOLESTEROL NORMAL IN WOMEN ACCORDING TO AGE
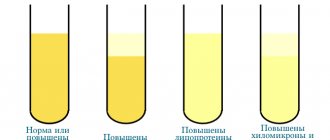
Hypercholesterolemia
When blood cholesterol is elevated, the condition is called hypercholesterolemia. It helps to make such a diagnosis by deciphering the data when analyzing the lipid profile.
| Index | Norm | Increased risk of developing atherosclerosis | The disease already exists |
| Total cholesterol | 3.1-5.2 mmol/l | 5.2-6.3 mmol/l | up to 6.3 mmol/l |
| HDL Women | more than 1.42 mmol/l | 0.9-1.4 mmol/l | up to 0.9 mmol/l |
| HDL Men | more than 1.68 mmol/l | 1.16-1.68 mmol/l | up to 1.16 mmol/l |
| LDL | less than 3.9 mmol/l | 4.0-4.9 mmol/l | more than 4.9 mmol/l |
| Triglycerides | 0.14-1.82 mmol/l | 1.9-2.2 mmol/l | more than 2.29 mmol/l |
| Atherogenic coefficient | depends on age | ||
Atherogenic coefficient (AC) is the ratio of HDL and LDL in the blood. To calculate it correctly, subtract HDL cholesterol from total cholesterol. Divide the resulting figure by the HDL value. If:
- KA less than 3 is the norm;
- KA from 3 to 5 – high level;
- KA more than 5 – greatly increased.
The norm of KA in women can vary differently. Cholesterol in women is affected by various reasons. For a low density indicator, the analysis requires a small age of women. But for very elderly women with heart disease, if the level of KA is elevated, this is the norm. Also, these density indicators depend on menopause, age, and hormonal levels of women.
Atherogenicity coefficient in women
| Age (years) | Norm for women |
| 16-20 | 3,08-5,18 |
| 21-25 | 3,16-5,59 |
| 26-30 | 3,32-5,785 |
| 31-35 | 3,37-5,96 |
| 36-40 | 3,91-6,94 |
| 41-45 | 3,81-6,53 |
| 46-50 | 3,94-6,86 |
| 51-55 | 4,20-7,38 |
| 56-60 | 4,45-7,77 |
| 61-65 | 4,45-7,69 |
| 66-70 | 4,43-7,85 |
| 71 and older | 4,48-7,25 |
LDL cholesterol (LDL-C) - norm in men table (by age)
Below (in the table) the norms of LDL-C / LDL cholesterol (low-density lipoprotein cholesterol) in blood serum in boys, young men and adult men are presented by age.
| Age (boy/youth/men): | Norm LDL cholesterol (mmol/l) | LDL-C norm (mg/dL) |
| children from 5 to 10 years old | 1.63 – 3.34 | 63.0 – 129.0 |
| 10 – 15 | 1.66 – 3.34 | 64.1 – 129.0 |
| 15 – 20 | 1.61 – 3.37 | 62.3 – 130.3 |
| 20 – 25 | 1.71 – 3.81 | 66.1 – 147.3 |
| 25 – 30 | 1.81 – 4.27 | 70.0 – 165.1 |
| 30 – 35 | 2.02 – 4.79 | 78.1 – 185.2 |
| 35 – 40 | 1.94 – 4.45 | 75.0 – 172.0 |
| 40 – 45 | 2.25 – 4.82 | 87.0 – 186.4 |
| 45 – 50 | 2.51 – 5.23 | 97.0 – 202.2 |
| 50 – 55 | 2.31 – 5.10 | 89.3 – 197.2 |
| 55 – 60 | 2.28 – 5.26 | 88.2 – 203.4 |
| 60 – 65 | 2.15 – 5.44 | 83.1 – 210.3 |
| 65 – 70 | 2.49 – 5.34 | 96.3 – 206.5 |
| over 70 years old | 2.49 – 5.34 | 96.3 – 206.5 |
(Follow the link) in more detail about AGE CHANGES IN CHOLESTEROL NORMAL IN MEN
Lower cholesterol without drugs
Before you start lowering cholesterol with medications, you should try to do this with a special diet and physical activity. How to lower LDL cholesterol without pills? Regular moderate physical activity will help solve this issue. You don’t have to go to the gym and train hard there. If there are no diseases of the cardiovascular system, you can do small 30-minute runs in your free time, but you need to monitor your pulse. It should not be higher than usual by more than 80%, i.e. immediately after a run, a pulse of 100-140 beats per minute is the norm. Moreover, after 5-10 minutes it should return to its normal values - 60-80 beats per minute.
Sometimes jogging is contraindicated; in this case, a 40-minute walk at a normal pace would be an excellent solution.
LDL cholesterol is elevated – what does this mean?
First of all, high levels of LDL cholesterol, especially in combination with a reduced content of HDL cholesterol (arterial hypertension, obesity, diabetes mellitus and other negative factors), mean an increased risk of developing atherosclerotic diseases of the blood vessels/arteries. Penetrating into the walls of blood vessels, micro/particles of LDL cholesterol form “growing hills”, which are commonly called “cholesterol plaques”. That is, a person begins to develop VASCULAR ATHEROSCLEROSIS
(perhaps even from the age of 20). Over time, the “slides” become higher and can completely block the lumen in the vessels. And this is dangerous in the following ways:
- if the blood vessels of the brain are blocked (for example, as a result of the development of cerebral atherosclerosis), then a STROKE occurs;
- if the main artery of the heart is blocked (due to the development of atherosclerosis of the aorta of the heart), then MYOCARDIAL INFARCTION occurs;
- if obliteration (i.e. blocking) of the walls of the arteries of the legs occurs (due to the development of obliterating atherosclerosis of the lower extremities), then this is fraught with GANGRENE.
However, there are other (no less serious) reasons for increased LDL cholesterol levels (in the blood of WOMEN
and
MEN
). As a rule, they can clearly indicate the development of other dangerous diseases (except for the above/described - atherosclerosis).
- IHD/coronary heart disease (especially in the presence of arterial hypertension, obesity or diabetes mellitus);
- chronic inflammation of the kidneys (advanced to the stage of nephrotic syndrome, which is accompanied, along with other signs, by hyperlipidemia, that is, an increase in the level of total cholesterol - above 6.5 mmol/l);
- cholestasis - a decrease or cessation of bile excretion caused by diseases of the liver (most often hepatitis), bile duct or pancreas;
- chronic renal failure (CRF), as a consequence of a number of diseases and dangerous disorders in the body;
- hypothyroidism (a condition caused by decreased thyroid function);
- serious problems with obesity;
- prostate cancer (prostate);
- pancreatic oncology.
Biochemistry analysis
The following categories of people must undergo an analysis for cholesterol and its LDL fraction in the lipid profile of blood biochemistry:
- To prevent atherosclerosis, especially for men after their 20th birthday, it is necessary to take a biochemical test for cholesterol with a lipid profile once every 3-5 years;
- If total cholesterol in biochemistry is increased, then it is necessary to make a lipid spectrum of the blood plasma, which includes a decoding of HDL, LDL, and triglycerides fractions, as well as an atherogenic index;
- Patients at risk of developing cardiac and vascular pathologies, especially systemic atherosclerosis. Pathologies that cause danger with high cholesterol - if the patient’s history includes cases of relatives of systemic atherosclerosis, embolism, myocardial infarction, stroke, or coronary syndrome, then blood biochemistry for cholesterol with a lipogram must be taken at least once a year;
- For arterial hypertension at very high levels, undergo blood biochemistry for lipid profile at least 1-2 times a year;
- If you have diabetes mellitus of the first and second tier, do a lipid profile at least 1 - 2 times a year;
- If a patient develops pathological obesity (in women, the waist circumference is greater than 80.0 centimeters, and in men, 94.0 centimeters), then this is a signal to do a blood test with a lipid spectrum to see the LDL level. More often than not, this level will be elevated because elevated LDL causes fat to accumulate in the body, which is deposited in the abdominal area and thighs. It is necessary to undergo biochemistry at least 2 times a year, and when treating excess weight, every quarter;
- If there is a disturbance in lipid metabolism, which leads to hypercholesterolemia;
- In case of IHD pathology, undergo biochemistry for LDL every 6 months;
- For aortic aneurysm, for atherosclerosis of the lower extremities - once every 6 months;
- For atherosclerosis of the coronary vessels, as well as the arteries of the neck and head, biochemistry is prescribed every 3 months, and in the treatment of atherosclerosis, once every 30 - 60 days;
- 30 days after the anti-cholesterol diet, it is necessary to take a biochemistry test for LDL.
It is necessary to take a biochemistry test for LDL levels
Norms
The norms for the content of cholesterol in plasma blood in men, as well as in the body of women by age:
| age category for adults | OX indicator for women unit of measurement in mmol/liter | cholesterol index for men unit of measurement in mmol/liter |
| from 20 years to 30 years | normal 3.10 - 5.160 | normal 2.90 - 5.050 |
| from 30 years to 40 years | from 3.30 to 5.790 | from 3.40 to 6.30 |
| from 40 years to 50 calendar years | ranging from 3,850 to 6,850 | ranging from 5.750 to 7.10 |
| from 50 years to 60 years | ranging from 4.050 to 7.30 | between 4.150 and 7.10 |
| from 60th birthday to 70th birthday | interval from 4,350 to 7,650 | from 4.0 to 7.150 |
| over 70 years of age | normal indicator 4.450 - 7.80 | normal index 4.050 - 7.050 |
Age/normal LDL
How to get tested?
To identify total cholesterol, as well as its fractions HDL, LDL and TG, and how high the LDL index is, it is possible only with the help of lipid biochemical analysis, the lipid spectrum method.
To do this, you need to prepare for analysis:
- Do not eat for 10 - 12 hours, but no longer. Long-term abstinence from food leads to depletion of body cells, which disrupts the correct level of cholesterol and its fractions;
- Dinner should be light and free of fatty foods and carbohydrates. It is better to eat boiled chicken or fish and a lot of fresh vegetables for dinner;
- Two per day, stop drinking alcohol;
- Do not smoke for one hour before donating blood;
- Do not perform heavy work or play sports during the day;
- You are allowed to drink a glass of purified water without gas before taking blood;
- Before donating blood, you need to sit quietly for about 15 minutes so that the body can relax and calm down;
- To take a cholesterol test, you must be in a good emotional mood;
- Do not take a biochemical test after an X-ray, ultrasound, MRI, angiography with contrast, or after physiotherapeutic procedures;
- If the patient is taking medications, then it is necessary to inform the doctor, but it is better to stop taking medications a week before the planned procedure;
- Stop taking antibacterial drugs, diuretics, hormonal contraceptives 7 - 10 days before the procedure.
Biochemistry analysis to identify the LDL index
How to reduce LDL levels in the blood to normal?
To reduce elevated LDL cholesterol levels, it is critical to go beyond (just) taking “cholesterol pills.”
(of course, STRICTLY (!) as prescribed by the treating specialist), but also follow very important rules! First, radically change your ENTIRE diet and overhaul your lifestyle. After all, you must agree, will there be any benefit from taking special medications if you immediately ate an “egg sandwich” (maybe even a couple) and had no intention of quitting smoking at all!?
Basic recommendations for changing your diet:
- significantly limit the consumption of saturated fats/fried foods and (!) give up trans fats forever;
- significantly increase the amount of plant fiber consumed in your daily menu;
- drink, eat only low-fat dairy products (or with a minimum amount of fat);
- replace animal proteins with vegetable ones (Canadian scientists have found that soy protein (even 25 grams per day) reduces LDL levels by 4-5%, and with a complete replacement of meat/products - up to 20%);
- switch to OMEGA-3 / polyunsaturated fatty acids (they are found in fatty fish or flaxseed oils);
- Replace sweet juices and carbonated drinks with tea (ideally green!) or plain water.
More detailed information based on the recommendations of domestic and foreign treating specialists can be found at the links below:
- A complete list of the best foods that lower cholesterol and cleanse blood vessels
- Recommended diet for effectively reducing “bad” cholesterol in the blood
- How to quickly lower cholesterol at home (before using pills)
We also recommend that you familiarize yourself with the brief TABLE-REMINDER
(about permitted and harmful foods for elevated cholesterol levels in the blood).
And, plus everything, with a table of cholesterol content in food
.
Basic recommendations for lifestyle changes (after consulting a doctor):
- first of all, quit smoking - find another alternative to this dubious “joy of life” or contact psychologists;
- not only lose weight, but also become a calorie expert (read more about this in the article on reducing triglycerides
); - try to move as much as possible (do regular sports, walk more in the fresh air, swim, dance or ride a bike).
And finally, NEVER TREAT YOURSELF by taking the “best” medications, or following any “dubious diets” read from a “tabloid” magazine.
Diet to lower cholesterol
Along with physical activity, you should change your taste preferences. This can be difficult to do, but we are talking about health, so this step is necessary.
You should exclude from your diet all foods that contain a lot of saturated fat. These include:
- all sausages;
- all semi-finished meat products;
- all baked goods and muffins, cakes and cookies;
- fatty meats;
- salo;
- vegetable oil (except soybean, rapeseed and corn);
- cream and sour cream;
- mayonnaise;
- hard cheeses.
Fruits, fresh vegetables and freshly squeezed juices from them, on the contrary, are recommended to be included in your diet. Sea fish will also be useful, because it contains omega-3 fatty acids. Sardines and salmon are especially healthy, but the fish should not be salted or fried. It is best to steam it or bake it in the oven.
Weak green tea also reduces cholesterol to some extent, because it contains flavonoids, which can strengthen the walls of blood vessels.
Some experts believe that drinking red wine in very small quantities can reduce bad cholesterol levels. Other scientists disagree with these data and say that alcohol, even in small doses, harms the body. Therefore, it is better to postpone such treatment until all specialists come to a consensus.
It is well established that there are foods whose regular consumption can lower cholesterol levels by 10%. These include:
- Nuts - They can interfere with the body's absorption of saturated fats. But they should be consumed in limited quantities (no more than 10-12 pieces per day), because they are too high in calories.
- Cereals - oats, barley, as well as wild rice and bran contain fiber necessary for good digestion.
- Soy, or more precisely the isoflavones it contains, can lower LDL cholesterol.
- Polyunsaturated vegetable oils (soybean, flaxseed, nut, rapeseed and corn) can be eaten if you have high cholesterol. These types of oils contain polyunsaturated fatty acids that can lower cholesterol. They are recommended for seasoning salads with fresh vegetables.
- Sea fish should be included in the menu at least 3 times a week.
- All fruits and vegetables contain soluble fiber, which helps remove LDL cholesterol from the body. It is especially useful to include cabbage, carrots, citrus fruits, apples and apricots in your diet. Beans are especially useful among legumes.
- It is believed that garlic, especially in combination with lemon, can cleanse blood vessels of cholesterol plaques. It is these two products that are included in a large number of folk recipes for cleansing blood vessels and lowering cholesterol.
If LDL cholesterol is below normal, this condition does not require treatment. This may be the result of poor nutrition and low-calorie diets. In this case, you should return to a balanced diet. It would be enough.
What does it mean if LDL cholesterol is low?
In general, decreased levels of LDL cholesterol (i.e., low-density lipoprotein cholesterol) are not clinically significant. Although, there are some reasons why this happens:
- familial (hereditary) hypocholesterolemia (hypocholesterolemia);
- severe liver diseases (in particular cirrhosis);
- oncological diseases (cancer) of the bone marrow;
- chronic alcohol intoxication (stage 2 alcoholism);
- hyperthyroidism (syndrome caused by hyperfunction of the thyroid gland);
- some inflammatory joint diseases;
- pernicious (or B12-deficiency) anemia (“malignant anemia”);
- inflammatory processes (in the body) or infectious diseases;
- COPD (Chronic Obstructive Pulmonary Disease).
VIDEO:
how are cholesterol (atherosclerotic) plaques formed in the walls of blood vessels (43 sec)?
What does it mean if low-density lipoproteins are elevated?
LDL cholesterol is elevated in patients with:
- various hereditary lipid balance disorders (hypercholesterolemia and hypertriglyceridemia);
- overweight;
- severe renal pathologies (presence of nephrotic syndrome, renal failure);
- jaundice, obstructive nature;
- endocrine pathologies (diabetes mellitus, hypothyroidism, adrenal disease, polycystic ovary syndrome, etc.);
- nervous exhaustion.
The cause of falsely elevated low-density cholesterol in tests may be the use of various medications (beta blockers, diuretics, glucocorticosteroid hormones, etc.).
What do blood test results mean (for adults and children)?
Interpretation of the results of a biochemical blood test (lipidogram) for the level of HDL cholesterol (or “good” cholesterol) for adult men and women, as well as children and adolescents. All data are presented according to NCEP guidelines. That is, the “National Cholesterol Education Program”, the main task of which is to reduce the number of cases of disability, as well as premature deaths as a result of the development of atherosclerotic cardiovascular diseases.
What do HDL cholesterol levels mean for adults?
HDL cholesterol (HDL-C) levels: less than 40 mg/dL (1.03 mmol/L)
for men and
less than 50 mg/dL (1.29 mmol/L)
for women - indicate an increased risk of cardiovascular disease and the development of atherosclerosis. At the same time, even those independent of other risk factors, including LDL-C levels (LDL-C).
The so-called typical (or normal) HDL cholesterol levels (HDL-C), indicating the average risk of developing atherosclerosis and heart disease, are in the range: from 40 to 50 mg/dl (1.03-1.29 mmol/l)
for men and
from 50 to 59 mg/dL (1.29-1.54 mmol/L)
for women.
According to the results of many epidemiological studies (conducted up to 2020), the level of HDL cholesterol is from 60 mg/dl (1.55 mmol/l) and above,
as a rule, correlate with minimal risks of developing CVD and atherosclerosis.
At the same time, for a long time it was believed (according to the recommendations of the NCEP commission of 2002) that it is precisely these indicators of PAP that are PROTECTIVE
. Therefore, they should be considered by the treating specialist as a negative factor.
HOWEVER (!)
, according to the results of the most recent studies conducted by European professors (and later confirmed by Americans), it ultimately turned out that high HDL levels (
60 mg/dL (1.55 mmol/L) and above)
are not universal / protective!
Moreover, EXTREME/HIGH levels of high-density lipoprotein ( over 3.0 mmol/L
for men, and also
3.5 mmol/L for women
) paradoxically lead to the development of CVD and premature death.
( SOURCE
: European Heart Journal, Volume 38, Issue 32, August 21, 2017, pages 2478–2486 / Christian M. Madsen, Anette Warbo, Bird Nordestgaard).
What do HDL cholesterol levels mean for teenagers and children?
If the blood level of HDL-C (HDL-C) in children and adolescents is less than 40 mg/dL (1.03 mmol/L)
, then there is an increased risk of cardiovascular disease, which (just as in adults) is independent of other risk factors, including LDL-C concentrations.
Indicators in the range from 40 to 45 mg/dl (1.03-1.17 mmol/l)
are borderline, and an HDL cholesterol level
of more than 45 mg/dl (1.17 mmol/l)
is considered acceptable.
Also read (link): HIGH CHOLESTEROL IN A CHILD, WHAT SHOULD BE DONE?
Ratio of total total cholesterol to HDL cholesterol
Some (our and foreign) laboratories additionally indicate the ratio of total cholesterol (Blood cholesterol, cholesterol total) to HDL / HDL, which is obtained by dividing them by each other. For example, if a person (according to the results of a blood test) has total cholesterol = 200 mg/dl, and HDL = 50 mg/dl, then this ratio will be indicated by the number 4 (or 4:1). Thus, the desired ratio is below 5 (or 5:1)
, and the optimal is
3.5 (or 3.5:1)
.
The American Heart Association recommends using the ratio of total total cholesterol in the blood to good HDL cholesterol (Cholesterol / HDL ratio). Since it is much more useful (for finding optimal treatment methods) than (Non-HDL-C / HDL-C ratio), i.e. atherogenic index ,
when (immediately before division) the amount of HDL is subtracted from the total cholesterol.
Blood and its tests
There are various methods for the quantitative determination of total lipids: colorimetric, nephelometric. Principle of the method. The hydrolysis products of unsaturated lipids form a red compound with the phosphovanillin reagent, the color intensity of which is directly proportional to the content of total lipids. Equipment: test tubes, pipettes, water bath, FEC, cuvettes with an optical path length of 5 mm. Hydrolysis of lipids is carried out; for this purpose, reagents are poured into dry test tubes according to the following scheme: The contents of the test tubes are mixed and left for 40 minutes. The experimental and standard samples are colorimeterized against the control using a green filter in a cuvette 0.3 cm thick. The content of total lipids is calculated using the formula. Clinical and diagnostic significance. As a physiological phenomenon, an increase in blood lipids, hyperlipemia occurs hours after eating.
Treatment is medicinal
As we found out, an increase in LDL cholesterol plays a major role in the development of atherosclerosis. To prevent the formation of this disease and its complications, it is necessary to constantly monitor the level of this substance, especially if there is a predisposition to its increase. If LDL cholesterol is elevated, treatment should be done by a cardiologist.
If diet and exercise do not help you cope with high cholesterol levels, you should take medications prescribed by your doctor. It can be:
- statins;
- niacin (nicotinic acid);
- fibrates or salts of fibric acid, which reduce triglyceride levels and increase HDL, accordingly lowering the “bad” fraction of cholesterol - LDL;
- bile acid sequestrants;
- cholesterol absorption inhibitors (the drug "Ezetimibe");
- food supplements containing omega-3 fatty acids.
How to decipher the analysis results
The doctor’s main task is to reduce the concentration of bad cholesterol to the patient’s individual norm.
General indicators of LDL norm:
- 1.2-3.0 mmol/l is the normal cholesterol level for an adult who does not have chronic diseases of internal organs.
- up to 2.50 mmol/l is the norm for cholesterol for people suffering from diabetes of any type, having unstable blood pressure or a genetic predisposition to hypercholesterolemia;
- up to 2.00 mmol/l is the normal cholesterol level for those who have suffered a heart attack, stroke, who have been diagnosed with coronary artery disease or the chronic stage of atherosclerosis.
In children, LDL and total cholesterol levels differ from adults. The pediatrician interprets children's tests. Deviations are very often observed in adolescence, but do not require specific treatment. The indicators return to normal after the end of hormonal changes.
Signs of Low LDL Cholesterol
It is possible to find out about a lack of cholesterol at the initial stage only with the help of a biochemical blood test. Because the process of lowering LDL levels occurs slowly. But in the case of prolonged hypocholesterolemia, a person may experience characteristic symptoms.
Signs of low cholesterol:
- There is a decrease in appetite or its complete absence.
- Muscle weakness is noted.
- Enlarged lymph nodes may be detected.
- Reflex and reactive abilities decrease.
- There is a tendency to aggression, irritability and depression.
- Sexual activity decreases.
When performing a lipid profile, if cholesterol levels are less than 4.6 mmol/l, hypocholesterolemia is diagnosed. In addition to problems with internal organs and the full functioning of body systems, especially the central nervous system. A person with critically reduced cholesterol levels has a tendency to suicide, alcohol and drug addiction.
What can low LDL mean:
- Genetic predisposition.
- Impaired functioning of the liver, intestines, adrenal glands or kidneys.
- Dysfunction of the gonads.
- Excessive synthesis of thyroid hormones (hypothyroidism).
- Oncological process in the central hematopoietic organ.
- A form of anemia characterized by vitamin B12 deficiency.
- Pathology of the respiratory system.
- Inflammatory process of joints.
- Acute infectious process.
HDL cholesterol is reduced - what does this mean?
In the same way as in previous cases, a decrease in the level of HDL cholesterol (HDL-C) can occur - both for temporary / correctable and for quite / serious reasons. And also testify not only to the increased risks of atherosclerotic vascular damage, but also to the presence of other diseases in the human body.
The most common causes of low HDL:
- familial hypo-alpha-lipoproteinemia (Tangier wasp disease), in other words - hereditary predisposition;
- severe liver diseases (as well as their complications);
- chronic renal failure (CRF);
- chronic kidney inflammation;
- acute infectious diseases;
- previous stress (for example, after an accident);
- “untreated” diabetes mellitus;
- cholestasis (as part of intrahepatic cholestatic syndrome).