Definition and purpose of the granulocyte series
Granulocytes are polymorphonuclear particles, one of the types of leukocytes - white blood cells.
The cells received this name due to the peculiarities of their granule-like structure, which is why they are often called granular leukocytes.
The main task of granulocytes is to prevent and eliminate inflammation, infections and allergic manifestations.
Deciphering the results of the study, by the number of granulocytes in a blood test, one can not only determine the presence of pathologies, but also determine the degree of intensity of the body’s protective reaction.
According to the specific structure and functionality, white cells are divided into two classes - granulocytes and agranulocytes.
The granulocyte series includes basophils, neutrophils, and eosinophils, while the agranulocyte series includes non-granular leukocytes—lymphocytes and monocytes.
The granulocyte series makes up about 75% of the total number of leukocytes in the blood and provides the first line of defense.
Thanks to the ability of granulocytes to be the first to respond to the appearance of problem areas, the immune system is activated, immediately forming a response to inflammatory processes and other types of pathologies.
Granulocyte cells are called polymorphonuclear cells due to the characteristics of the shape and composition of their nucleus.
During development, each of the granular cells goes through several stages: from a pluripotent mother cell, a unipotent mother cell is formed, from which a myeloblast is formed - the basis that gives birth to basophils, neutrophils and eosinophils.
Myeloblast has the property of differentiation and proliferative division. During the process of maturation, myeloblasts become promyelocytes, then myelocytes, and only after that they pass into the mature form.
Typically, immature cells are found in the bone marrow. But situations are possible when even the reserve fund of neutrophils is used, and in order to compensate for the deficiency of active cells, immature granulocytes enter the blood.
Therefore, if young granulocytes were detected in a blood test, this is regarded as an indicator of emergency situations in the immune system.
Video:
https://youtube.com/watch?v=hOugDDzX-sg
The main habitat of granulocytes is damaged tissues, poorly supplied with blood and oxygen due to inflammatory processes. Polymorphonuclear cells use the processes of anaerobic glycolysis as a source of nutrition.
The lifespan of different types of leukocytes differs significantly. For example, lymphocytes can retain the memory of a foreign protein for several years.
Granulocytes that do not have the ability to remember live up to 10 days - they die immediately after performing their protective function.
Blood sampling algorithm
The biological material is usually capillary liquid connective tissue.
Blood sampling algorithm:
- The nurse generously soaks cotton wool in an antiseptic solution and treats the pad of the ring finger of the left or right hand with it. A disposable alcohol wipe can also be used for this purpose.
- The intended puncture site is wiped with sterile dry material.
- The nurse removes from the package a disposable needle or vacuum instrument intended for collecting capillary blood.
- The specialist quickly makes a puncture. The first few drops are wiped off with a napkin or cotton wool soaked in antiseptic. The rest are collected into instruments.
- After obtaining a sufficient amount of capillary blood, the nurse applies an alcohol pad or cotton wool to the puncture site.
It is important to keep the attached material with the antiseptic for a few more minutes. Minor pain may persist at the puncture site for several hours.
Reasons for the decrease in eosinophilic and basophilic granulocytes
When the results of a blood test show a decrease in granulocytes, it is difficult to understand what this means without medical education. You need to know what analysis indicators are considered normal.
Quantitative norms of granulocyte cells in the blood are designated using the abbreviation GRA and are indicated either as a percentage of the total number of leukocytes (GRA%) or as an absolute indicator (GRA #).
Accordingly, when deciphering the results of the analysis, doctors are guided by this normal indicator - 1.2 - 6.8 * 10⁹ per liter of blood or 47 - 72 GRA% of the total level of leukocytes.
The results of the analysis indicate the number of immature granulocytes. The normal level of indicators of such cells can range from 1 to 5 percent.
If the analysis shows that immature granulocytes are low, then this is regarded as a sign of problems with the functionality of the immune system.
Video:
For each type of granulocytes, there are normal indicators established by medicine.
Reduced granulocytes cannot be regarded as evidence of any one disease. The diagnosis may differ depending on which subtype the indicators are not normal.
A decrease in the level of eosinophilic granulocytes (eosinopenia) is diagnosed when the number of cells is less than 5*10⁴/ml, which may indicate:
- septic condition;
- acute form of bacterial infection;
- physical overload;
- burn disease;
- anemia due to folate deficiency;
- side effects of glucocorticoids;
- as a result of a stressful situation;
- numerous injuries;
- hypoplastic anemia;
- post-surgical intervention.
In children, a decrease in eosinophil cells is considered a sign of pathological processes in the hematopoietic system.
Basophils are considered the largest granulocytes, the functionality of which is determined by the presence of prostaglandins, histamine and serotonin in their composition, and the ability to produce heparin, which regulates blood clotting.
Even when bitten by bees or poisonous snakes, basophilic granulocytes not only block the action of the poison, but also remove toxic substances from the body.
A decrease in the level of basophils in the blood (basopenia) is not only a rare phenomenon, but also difficult to diagnose. A deviation from the norm is considered to be a decrease in values from 0.01*10⁹/l.
In most cases, a decrease in the level of basophils is a consequence of insufficient functionality of the hematopoietic system.
Most often, basopenia develops against the background of such pathologies as:
- pneumonia;
- infections;
- pathologies of the endocrine system - Graves' disease, hyperthyroidism;
- Cushing's syndrome.
In addition, basophils decrease as a result of stressful situations, after taking hormonal anti-inflammatory drugs, as a result of chemotherapy, in women - during ovulation and during pregnancy.
Pathological anatomy
Pathological signs of agranulocytosis are necrotic-ulcerative changes, most often found in the oral cavity and pharynx. The tonsils are enlarged, loose, gray-dirty in appearance, with fibrinous deposits and ulcerations. In the area of the soft and hard palate, foci of necrosis are found, sometimes with perforation of the soft palate. Necrotic changes are detected in the skin, at injection sites, in the perineal area, and around the anus. Foci of necrosis are described in the conjunctival sac, in the mucous membrane of the larynx, esophagus and stomach. With the development of necrosis in the mucous membrane of the small or large intestine, including the appendix, intestinal bleeding and perforation are observed. Necrotic ulcers can be in the wall of the bladder, in the genitals, especially in the vaginal wall, as well as in the tissue of the liver and other organs. Microscopic examination shows that there are no neutrophilic leukocytes in areas of necrosis. The demarcation strip around the necrosis is not detected; lymphohistiocytic and plasma cell accumulations can be seen near the areas of necrosis. Pneumonia is fibrinous-hemorrhagic in nature. In this case, fibrinous deposits are also located on the pleura. In the area of pneumonia, areas of tissue decay (gangrene) may be detected. Microscopically, desquamated epithelial cells, bacteria, yeast cells and their mycelium are visible in the lumens of the alveoli. Lymph nodes are usually not enlarged. With necrotic changes in the oral cavity, a slight enlargement of the cervical and submandibular lymph nodes may be observed. Their microscopic structure is relatively preserved. In the cortex and especially in the area of the medullary cords, a large number of plasma cells are detected. Proliferation and swelling of reticuloendothelial cells in the sinuses is sharply expressed. The spleen is often unchanged. The spleen tissue is of a soft consistency; on the section there is a pink-gray pulp with a large scraping
Microscopic examination reveals a uniform decrease in the number of red pulp cells of the spleen. The bone marrow of flat bones is macroscopically more common than usual, somewhat dry, but there may be various foci of hemorrhage - from small to extensive; in the lower and middle third of the tubular bones, the bone marrow is fatty.
Microscopically, small foci of resorption of bone beams with the formation of small lacunae are revealed. Osteoblast proliferation may be observed in areas of bone resorption. The ratio of adipose and hematopoietic tissue is different. More often there is a decrease in the number of hematopoietic cells and an increase in the number of fat cells in the bone marrow
In the cellular composition, attention is drawn to a sharp decrease in the number of young, band and segmented granulocytes. There may be some predominance of young forms of granulocytes
Megacarpocytes and red row cells are usually preserved. In the most severe course of AGRANULOCYTOSIS, the picture of the bone marrow is the same as in hypoplastic anemia (see).
Reasons for the increase in young granulocytes
If neutrophils are elevated, a shift to the left is usually observed in the leukocyte formula. That is, immature and band-nuclear granulocytes are present in the blood. This indicates the development of a pathological process in the body. That is why the body begins to produce neutrophils in large quantities in order to protect against infection. Hence the large percentage of young forms. The reasons for the increase in the number of immature neutrophils are numerous. An increase in their level can be physiological:
- in newborns;
- during pregnancy;
- under stress;
- after meal;
- during physical activity.
An increase in the level of young granulocytes is observed in the following pathologies:
- pneumonia, peritonitis, osteomyelitis, appendicitis, meningitis, pyelonephritis, cholera, sepsis, tonsillitis, thrombophlebitis, cholecystitis, scarlet fever, otitis media;
- purulent processes: abscesses and phlegmon;
- typhoid fever, tuberculosis, hepatitis, malaria, measles, influenza, rubella;
- chronic skin diseases: psoriasis, some types of dermatitis;
- acute bleeding;
- burns;
- intoxications: lead poisoning, insect bites, foreign protein, diabetic acidosis, uremia, Cushing's syndrome, etc.;
- malignant diseases;
- systemic diseases;
- gout;
- myocardial infarction, pulmonary infarction;
- gangrene;
- chronic myeloplastic diseases;
- serum sickness;
- after taking certain medications: androgens, lithium preparations, glucocorticosteroids.
A particularly sharp shift to the left in the leukocyte formula is observed in myelomonocytic leukemia, as well as in purulent processes. The number of rod and immature forms increases sharply. Neutrophil granulocytes can have changes not only of a quantitative, but also of a qualitative nature, especially with severe intoxication and severe purulent-inflammatory processes. With strokes, burns, heart attacks and trophic ulcers, the increase in neutrophils occurs less frequently.
The reasons for the increase in immature forms of neutrophils in children are most often the following:
- otitis media, tonsillitis, pneumonia and other acute infections;
- purulent processes;
- acidosis;
- leukemia;
- hemolytic anemia;
- trophic ulcers;
- third and fourth degree burns.
A blood test for granulocytes is carried out in many diseases and when various pathologies are suspected. The presence of immature forms most often indicates a disease. Typically, a test for neutrophils occurs during a general blood test marked “detailed analysis,” which is taken on an empty stomach in the morning. Blood is taken from a finger. The day before, it is recommended to avoid alcoholic beverages, fatty and fried foods. At least eight hours must have passed since your last meal. It is not recommended to engage in sports or heavy physical work the day before. It is necessary to stop taking medications that may distort the results. If this is not possible, you should inform your doctor. In emergency cases, blood can be taken from a vein at any time of the day.
Modern analyzers allow you to count the number of immature granulocytes with a high degree of accuracy. Automatic calculation significantly reduces the time of analysis and delivery of the finished result.
Deciphering the leukocyte formula has important diagnostic value. Immature and band-nuclear neutrophil granulocytes especially react to inflammatory and purulent processes
At the same time, their growth occurs, as evidenced by a shift to the left in the leukocyte formula. Detection of juvenile forms in the blood makes it possible for early diagnosis.
Preparation
The collection of biomaterial is carried out in the morning. Blood must be donated on an empty stomach. The last meal should take place 8-10 hours before donating liquid connective tissue. At the same time, it is recommended to exclude fatty, fried, smoked, spicy and salty foods from the diet the day before.
In addition, it is undesirable to subject the body to high-intensity physical activity during the day. This is due to the fact that overexertion can distort the results of a blood test (the GRA indicator is also likely to change).
Immediately before submitting the biomaterial, it is recommended to sit quietly for about 15 minutes. Psycho-emotional stress is also a factor that can distort the results.
Activity of granulocytes
Granulocytes (abbreviated GRA in medical documentation) are representatives of a subgroup of leukocyte blood cells.
They owe their name to their appearance: granulocytes in the cytoplasm are small granular bodies (cells in which granules can be seen in the laboratory).
Granulocytes are represented by basophils, neutrophils and eosinophils. The majority (at least 80% of all forms of the granulocytic subgroup) are neutrophils.
This type of blood cell is responsible for immunity in the tissue cells of the human body.
Granular leukocytes are among the first to rush to the rescue if pathogens of pathological processes are detected and act as follows: they capture foreign bodies, absorb and dissolve within themselves.
The birthplace of granulocytes is the bone marrow, where they remain until they reach morphological maturity.
From the moment they enter the bloodstream, granular leukocytes live no more than 70 hours, and if phagocytosis occurs, they die immediately, becoming part of the pus, which can be observed in places of inflammation.
Granulocytes are divided into three types depending on the degree of maturity:
- young (young);
- rod (immature);
- mature (segmented).
The mature age of a granular leukocyte can be determined by the nucleus divided into lobes (in young and young specimens such division is absent).
The attending physician may suspect an infectious lesion or existing foci of inflammation if immature granulocytes are detected in the blood.
These suspicions may be justified because young granulocytes should not be found in the bloodstream of an adult, but in the blood of children a minimum percentage is acceptable, calculated in accordance with the age category of the patient.
The main functionality of granular blood cells in the blood comes down to the following actions: absorption of potentially dangerous elements, immediate response during intoxication, allergies; participation in blood clotting.
Granulocytes move quite quickly in the bloodstream and, if a focus of inflammation or infection is detected, they make their way to it, find pathogens and begin the process of absorption and digestion within themselves.
A subtype of leukocytes - blood basophil cells - instantly come to the defense of a person in the event of an allergic reaction or manifestations of intoxication (caused, for example, by the bite of poisonous animals or insects), preventing toxic substances from spreading further than the bite site.
In addition to this function, basophils take part in blood clotting.
Eosinophil granulocytes are capable of fighting and absorbing not only the simplest microorganisms, but also quite large foreign particles, for which this type of neutrophil is classified as a macrophage.
White calves - scouts
The protective function of the body is supported by basophils. Thanks to scout cells, when they detect viruses and bacteria, blood flow increases, and fluid flow increases in the area of inflammation.
If granulocytes are elevated, the causes of this condition are as follows:
- chemical contamination of humans;
- poisoning by poison, poor quality food;
- ingestion of substances to which an acute allergic reaction occurs (eosinophils are the main source of anaphylactic shock);
- reaction to a powerful drug.
Eosinophils are able to dissolve allergic substances due to vitamin E, which is present in large quantities in their composition. It is released outside to neutralize foreign substances in the human body, due to which, by the way, shock conditions develop. A special feature of these white cells is their ability to exist outside of blood vessels.
Functions of granulocytes
Granulocytes have a second name - granular leukocytes. These cells are one of the types of white blood particles that have a curved nucleus.
Granulocytes are divided into segments (a cell can have up to five lobes), in which granulation can be seen (in the laboratory, granules are stained, which makes them visible).
Granular leukocytes are born in the bone marrow; Such cells live in the tissues of the body for a very short time - about three days.
The content of granulocytes in the blood is about 79% of the total number of all leukocyte cells. About 70% of them are neutrophils, 5% are eosinophils, no more than 1% are leukocytes-basophils. Each type of granulocytic makes its contribution to the common cause - getting rid of pathogenic microorganisms.
When disease provocateurs enter the human body, granular leukocytes identify “strangers” and absorb them, dissolving them inside themselves.
The difference between granulocytes and other leukocyte blood particles (for example, lymphocytes and monocytes) is that, as a result of their short existence, granular phagocytes do not remember pathogenic microflora and, accordingly, do not affect acquired immunity.
Having completed the task of protecting the body and destroying harmful protozoa, granulocytes immediately die, so the results of the analysis may reveal a deficiency of them in the blood, and purulent discharge (consisting of dead neutrophils) at the site of infection.
Among granulocytic cells, depending on age, it is customary to distinguish mature (segmentation has occurred in them), rod (insufficiently mature, since the nucleus in them has not yet been divided into lobes) and young (immature granulocytes).
In the sheet of results of a general blood test, the types of neutrophils are indicated in order: young, not fully mature and mature.
In healthy people, immature granulocytes are practically undetectable in the blood (the only exceptions are women during pregnancy and infants), since their traditional location is the bone marrow.
Video:
https://youtube.com/watch?v=hOugDDzX-sg
However, in the case when all neutrophils are thrown into defense, a shortage of them occurs, and young cells rush to the rescue, making their way into the bloodstream, as a result of which an increased number of immature granulocytes is detected during laboratory testing.
Thus, based on the percentage of young neutrophils, one can judge the development of certain pathologies in human organs.
Exceeding the normal level of immature granulocytes in the blood often indicates the onset of an inflammatory process or infectious disease.
Reasons for the decrease in neutrophil granulocytes
Typically, granulocyte levels change throughout a person's life. Indicators in an adult differ from the level of white cells in children under one year old.
If the granulocyte counts are lower than normal, then the doctor’s task is to determine the cause of the pathology and eliminate it by prescribing a course of treatment.
Neutrophil granulocytes mature in the bone marrow. This period takes an average of 10 days, and then the cells enter the bloodstream and perform their protective functions for 10 hours. The highest concentration of neutrophils is observed in the affected tissues.
A decrease in the level of neutrophil cells (neutropenia) can be a symptom of the following human pathological conditions:
- radiation injury;
- neoplasms in the bone marrow - leukemia, myelofibrosis;
- various types of anemia;
- typhoid fever;
- diabetes mellitus;
- toxic goiter;
- malaria;
- bacterial infections - brucellosis, tularemia;
- viral infections - influenza, rubella, various subtypes of hepatitis, AIDS;
- autoimmune pathological conditions - collagenosis, lupus erythematosus;
- depletion of the biological potential of the body against the background of chronic alcoholism, cachexia;
- hypersplenism;
- taking medications with toxic effects - tranquilizers, antibiotics, immunosuppressants;
Neutrophils may be low in a child with congenital Kostman syndrome. As a result of the development of this pathology, the bone marrow loses the ability to produce the required number of neutrophils.
The consequences of the disease are more than serious - a general weakening of cellular immunity is accompanied by multiple inflammatory lesions of the skin and internal organs, which often leads to death.
The degree of development of neutropenia is reflected in the results of a blood test as follows:
- mild form - the number of neutrophils is from 1*10⁶/ml;
- severe form - the number of neutrophils is less than 5*10⁵/ml.
To make an accurate diagnosis, it is very important to know the degree of relationship between mature and immature forms of granulocytes. Autoimmune diseases and congenital forms of leukopenia can reduce the levels of immature white cells
A decrease in granulocytes against the background of an increase in the number of leukocytes is always a symptom of intense inflammatory processes.
Video:
In addition, granulocyte counts often change during the summer. Summer is the time of activity of allergens, bacteria and fungi, the damage to which is reflected in a blood test.
In children under one year old, the rate of immature granulocytes cannot exceed 4%, from one year to 6 years - 5%, upon reaching 15 years - no more than 1 - 5%.
Any pathologies that occur in the body require medical supervision and accurate diagnostic conclusions, therefore, even understanding the meaning of granulocyte indicators, you should not self-medicate.
Quantitative indicators
If granulocytes are elevated, the cause is the spread of infection throughout the body. The analyzes indicate quantitative values of the norm ranging from 1.2 to 6.8 per 10 to the 9th power. This total number may not change, but the ratio of neutrophils, basophils, lymphocytes and eosinophils varies. Indicators are indicated as percentages:
- Basophils depend on age: up to 1 year from 0.4 to 0.9%, up to 21 years from 0.6 to 1%.
- For eosinophils, the norm is from 120 to 350 per 1 ml of blood. In the morning, the normal values exceed 15% of the normal state, in the first half of the night - by 30%. Fluctuations in values occur with changes in the functioning of the adrenal glands.
- Neutrophils can normally be band-nuclear - no more than 6% and segmented - no more than 70%, but not less than 40%.
Etiology and pathogenesis
According to the mechanism of occurrence, AGRANULOCYTOSIS can be myelotoxic and immune.
Myelotoxic
AGRANULOCYTOSIS occurs as a result of suppression of the growth of prestage granulocytes in the bone marrow, including stem cells. In this regard, there is a decrease in the blood not only of granulocytes, but also of platelets, reticulocytes and lymphocytes. Myelotoxic AGRANULOCYTOSIS can develop as a result of exposure of the body to ionizing radiation, chemical compounds with cytostatic properties (antitumor drugs, benzene and others), waste products of a Fusarium type fungus that multiplies in overwintered grain (see Aleukia alimentary-toxic).
Immune
AGRANULOCYTOSIS develops as a result of accelerated death of granulocytes under the influence of anti-leukocyte antibodies; stem cells are not affected. Anti-leukocyte antibodies are formed under the influence of medications that can play the role of haptens (see Haptens). With repeated administration of such a medication, agglutination of leukocytes appears.
The development of immune agranulocytosis depends little on the dose of the drug; the most important role in its occurrence is played by the unusual sensitivity of the body. On the contrary, in myelotoxic AGRANULOCYTOSIS the decisive role is played by the magnitude of the damaging effect. Among the drugs that cause immune agranulocytosis, the main place belongs to amidopyrine. Immune agranulocytosis can also be caused by butadione, phenacetin, atophan, analgin, diacarb, barbamyl, sulfonamides, PAS, tubazide, ethoxide, streptomycin, pipolfen and some other drugs. Long-term use of the hapten drug can cause the destruction of not only mature granulocytes, but also myelocytes and promyelocytes. The development of autoimmune AGRANULOCYTOSIS, more often leukopenia, is observed with collagenosis (especially disseminated lupus erythematosus, rheumatoid polyarthritis), as well as with some infections.
A special place is occupied by AGRANULOCYTOSIS with systemic lesions of the hematopoietic apparatus - leukemia (see), hypoplastic anemia (see), as well as with metastases to the bone marrow of a cancerous tumor and sarcoma.
What are granulocytes?
Granulocytes contain nuclei that have an irregular shape. These nuclei are divided into 2-5 particles, so the second name for granulocytes is polymorphonuclear cells.
Granulocytes make up about 75% of all leukocytes. They are represented by eosinophils, basophils and neutrophils. These cells are present not only in the blood, but also in human tissues. Depending on the cause of inflammation that occurs in the body, various granulocytes come into play. This does not mean that they function in isolation from each other; they always interact with each other and with other substances. Thus, neutrophils act in tight association with macrophages, eosinophils with basophils.
Granulocytes are born in myeloblasts. After myeloblasts mature, they transform into promyelocytes and then into myelocytes. Large myelocytes are immature maternal forms, and small myelocytes are classified as mature daughter cells. In the form of myelocytes, granulocytes can no longer divide; they possessed this ability only during the period when they were represented by promyelocytes. Myelocytes cannot be detected in the blood. Normally, they do not leave the bone marrow. If emergency situations occur when all neutrophils are involved in other reactions in the body, then immature granulocytes come to their aid. Only in this case can they be detected in the blood.
For anaerobic glycolysis, granulocytes take energy even from swollen and inflamed tissues that are not supplied with sufficient oxygen. The lifespan of granulocytes is 2-10 days, which depends on the type of cell. Having fulfilled their function, they die, and new granulocytes take their place.
Promotion and relegation
According to studies, deviations in the content of cells in the blood from the norm can be presented in two varieties: when, according to a blood test, granulocytes are low or when, according to a blood test, granulocytes are increased.
An increase in granulocytes in the blood occurs during the following inflammatory processes and pathological conditions: acute infectious diseases; malignant tumors, vaccinations, intoxication, parasitic, viral infections, allergies. Treatment with certain medications can also cause elevated granulocytes in a blood test.
Exceeding the norm for the content of immature granulocytes in the blood is also evidence of trouble in the body. Most often, an increase in young granulocyte cells in the blood is due to the presence of acute and chronic diseases (tuberculosis, pyelonephritis, influenza, psoriasis, myocardial infarction, cholera, rubella). With burns, acute bleeding, and poisoning with chemicals, an increase in granulocytes in the blood is also observed.
The reasons for the increase in the level of granulocytes in the blood may be associated with the characteristics of the physiological state of the body, these include childbirth, pregnancy, nursing mothers also have an increased level of these cells, and also provoke higher than normal levels of physical activity or abundant nutrition. In women, an increase in the level of granulocytes in the blood is regularly observed before critical days.
These changes can be recognized as a physiological norm, provided that the cell level remains constant.
Autoimmune diseases such as various types of anemia, rheumatism, scarlet fever, tumor, sarcoidosis, lupus erythematosus can cause low levels and decreases in granulocytes in the blood.
In some cases, the level of deviations of granulocytes from the norm according to groups of granular leukocytes is examined:
| Cell group/ abnormality | Promotion | Demotion |
| basophils | Caused by allergic reactions, infectious diseases during the recovery stage, hypothyroidism, diseases of the gastrointestinal tract, myeloid leukemia, granulomatosis | During the first trimester of pregnancy, during stressful situations; diseases of the thyroid gland, due to taking hormonal drugs, pneumonia; during ovulation, acute infections; |
| neutrophils | Caused by bacterial infections, peritonitis, appendicitis, pyelonephritis, tissue necrosis, myocardial infarction, burns, gangrene, tumors, leukemia, intoxication, anemia | Occurs during viral diseases, taking medications, exposure to radiation, due to bone marrow damage, leukemia, anaphylactic shock |
| eosinophils | Occurs with allergies of various etiologies, intolerance to certain medications, parasitic diseases, blood diseases, eczema | For acute infectious diseases, injuries, operations, due to childbirth, shock, intense physical activity, when taking certain medications, for late gestosis in pregnant women |
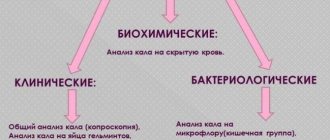
The main diagnostic method for studying the level of polymorphonuclear cells is a complete blood test for granulocytes. When preparing for blood collection, follow the rules that are typical for preparing for a general blood test for the presence of granulocytes.
Cost of analysis
Biomaterial can be submitted for general clinical examination in both public and private medical institutions. In the first case, the blood test is performed free of charge, but only if the patient has an insurance policy.
In private clinics, the cost of analysis is on average 350 rubles. Additionally, you need to pay for the collection of biomaterial. Usually the cost of this service does not exceed 150 rubles.
Analysis results are ready on the same day.