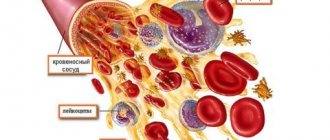
Leukocytes, or white blood cells, are components that protect the body from infectious agents. They play an important role in protecting the immune system by identifying, destroying, and removing pathogens, damaged cells (such as cancer cells), and other foreign substances from the body. White blood cells are formed from stem cells in the bone marrow and circulate in the blood and lymph fluid. How are they formed and what is their life cycle? What is the lifespan of white blood cells?
Leukocyte formation
White blood cells are produced primarily in the bone marrow, with some maturing in the lymph nodes, spleen, and thymus. The lifespan of leukocytes ranges from approximately several hours to several days. Blood cell production is often regulated by body structures such as the lymph nodes, spleen, liver and kidneys. Low white blood cell counts may be due to disease, radiation exposure, or bone marrow damage. High may indicate the presence of an infectious or inflammatory disease, anemia, leukemia, stress, or extensive tissue damage in the body.
Lifespan of leukocytes
· Granulocytes
live in the circulating blood for 4–5 hours, and in tissues for 4–5 days. In cases of serious tissue infection, the lifespan of granulocytes is shortened to several hours, since granulocytes very quickly enter the site of infection, perform their functions and are destroyed.
· Monocytes
after 10–12 hours of residence in the bloodstream, they enter the tissues.
Once in the tissue, they increase in size and become tissue macrophages
. In this form, they can live for months until they are destroyed, performing the function of phagocytosis.
· Lymphocytes
enter the circulatory system constantly in the process of draining lymph from the lymph nodes. A few hours later, they return to the tissues through diapedesis and then return again and again with lymph into the blood. Thus, there is a constant circulation of lymphocytes through the tissue. The lifespan of lymphocytes is months and even years, depending on the body's needs for these cells.
Microphages and macrophages
.
The main function of neutrophils and monocytes is phagocytosis and subsequent intracellular destruction of bacteria, viruses, damaged cells that have completed their life cycle, and foreign agents. Neutrophils (and to some extent eosinophils) are mature cells that phagocytose various materials (another name for phagocytic neutrophils is microphages
).
Blood monocytes are immature cells. Only after entering tissues do monocytes mature into tissue macrophages
and acquire the ability to fight pathogenic agents. Neutrophils and macrophages move through tissues through amoeboid movements stimulated by substances produced in the inflamed area. This attraction of neutrophils and macrophages to the area of inflammation is called chemotaxis.
Neutrophils
Neutrophils (Fig. 24–17, see also Fig. 24–2, 2) are the most numerous type of leukocytes. They make up 40–75% of the total number of leukocytes. Neutrophil dimensions: in a blood smear - 12 microns; the diameter of a neutrophil migrating in tissues increases to almost 20 microns. Neutrophils are formed in the bone marrow within 7 days, after 4 days they enter the bloodstream and remain in it for 8–12 hours. Life expectancy is about 8 days. Old cells are phagocytosed by macrophages. The neutrophil contains several mitochondria and a large amount of glycogen. The cell receives energy through glycolysis, which allows it to exist in oxygen-poor damaged tissues. The number of organelles required for protein synthesis is minimal; therefore, the neutrophil is not capable of prolonged functioning and dies after a single burst of activity. Such neutrophils constitute the main component of pus (“pus” cells). The composition of pus also includes dead macrophages, bacteria, and tissue fluid.
Rice
.
24–18
.
Neutrophil
[11]. (see also Fig. 24–2, 2). The core consists of 3-5 segments connected by thin bridges. The cytoplasm contains a minimal number of organelles, but many glycogen granules. The neutrophil contains a small number of azurophil granules (specialized lysosomes) and numerous smaller specific granules.
· Neutrophil pools
. There are three pools of neutrophils: circulating, border and reserve.
a Circulating
- passively transported blood cells. When a bacterial infection of the body occurs, their number increases several (up to 10) times within 24–48 hours due to the border pool, as well as due to the accelerated release of reserve cells from the bone marrow.
à Borderline
the pool consists of neutrophils associated with endothelial cells of small vessels of many organs, especially the lungs and spleen. The circulating and boundary pools are in dynamic equilibrium.
à Reserve
pool—mature bone marrow neutrophils.
· Core
.
Depending on the degree of differentiation, band and segmented
neutrophils are distinguished (see Fig. 24–1, B).
In neutrophils in women, one of the nuclear segments contains a drumstick-shaped outgrowth - Barr body
, or sex chromatin (this inactivated X chromosome is visible in 3% of neutrophils in the blood smear of women).
Ú Band neutrophils
- immature forms of cells with a horseshoe-shaped nucleus. Normally, their number is 3–6% of the total number of leukocytes.
Ú Segmented neutrophils
- mature cells with a nucleus consisting of 3–5 segments connected by thin bridges.
a Nuclear shifts in the leukocyte formula
. Since during blood smear microscopy the main criterion for identifying different forms of maturity of granular leukocytes is the nature of the nucleus (shape, size, color intensity), shifts in the leukocyte formula are designated as “nuclear.”
Ú Shift left
characterized by an increase in the number of young and immature forms of neutrophils (see Fig. 24–6). In acute purulent-inflammatory diseases, in addition to leukocytosis, the content of young forms of neutrophils, usually band neutrophils, less often young neutrophils (metamyelocytes and myelocytes), increases, which indicates a serious inflammatory process.
Shifts in the leukocyte formula of neutrophils to the left
determined by the appearance of immature forms of neutrophils. There are hyporegenerative, regenerative, hyperregenerative and regenerative-degenerative types of shift to the left.
Ú Hyporegenerative
. It is indicated by an increase in the content of band neutrophils above normal (more than 6%) and moderate leukocytosis (usually up to 10–11´109/l).
Ú Regenerative
. It is characterized by an above-normal increase in the percentage of band neutrophils, the appearance of metamyelocytes in the peripheral blood, and leukocytosis up to 13–18´109/l.
Ú Hyperregenerative
. It is manifested by a significant increase in the content of band neutrophils, the presence in the peripheral blood of a large number of metamyelocytes and the appearance of myelocytes, an increase in the total number of leukocytes to 20–25´109/l. However, the total number of leukocytes may be normal or even reduced. In some cases, the latter is observed after a long period of significant leukocytosis and is caused by depletion of the myeloid lineage of hematopoietic tissue.
Ú Regenerative-degenerative
. It is observed in some infections, chronic purulent processes that occur with significant intoxication. It is characterized by a more or less pronounced increase in the level of band neutrophils, metamyelocytes and myelocytes, a decrease in the number of segmented neutrophils (as a rule), signs of degenerative changes in the cytolemma, cytoplasm and nucleus, and an increase in the total number of leukocytes.
Ú Shift right
manifested by an increase in the number of segmented nuclear forms of neutrophils.
a Nuclear shift index
reflects the ratio of the percentage of the sum of all young forms of neutrophils (band, metamyelocytes, myelocytes, promyelocytes, see Fig. 24–6) to their mature forms. In healthy adults, the nuclear shift index ranges from 0.05 to 0.10. An increase in it indicates a nuclear shift of neutrophils to the left, a decrease indicates a shift to the right.
· Neutrophil granules
à Azurophilic granules
neutrophils contain various proteins that destroy components of the extracellular matrix and have antibacterial activity. The granules contain cathepsins, elastase, proteinase 3 (myeloblastin), azurocidin, defensins, cationic proteins, lysozyme, arylsulfatase. The main enzyme of azurophilic granules is myeloperoxidase. This protein makes up 2–4% of the neutrophil's mass and catalyzes the formation of hypochlorous acid and other toxic agents that significantly enhance the bactericidal activity of the neutrophil.
à Specific granules
much smaller than azurophiles, but twice as numerous. The granules contain proteins with bacteriostatic properties: lactoferrin, vitamin B12-binding proteins. In addition, the granules contain lysozyme, collagenase, alkaline phosphatase, and cationic proteins.
· Receptors
. Receptors for adhesion molecules, cytokines, colony-stimulating factors, opsonins, chemoattractants, and inflammatory mediators are built into the plasmolemma of neutrophils. Binding of their ligands to these receptors leads to activation of neutrophils (exit from the vascular bed, migration to the site of inflammation, degranulation of neutrophils, formation of superoxides).
Granulocyte colony-stimulating factor receptor
(G-CSF) are expressed not only by neutrophil precursors, but also by differentiated cells.
Opsonin receptors
bind Fc fragments of IgG, complement proteins C3a, C3b, C3bi, C4b, C5a.
Inflammatory mediator receptors
(eg, leukotriene B4, platelet activating factor PAF, C5a).
Chemoattractant receptors
(for example, f-Met-Leu-Phe (Table 24–11).
· Neutrophil function
. Neutrophils remain in the blood for only a few hours (in transit from the bone marrow to tissues), and their inherent functions are performed outside the vascular bed (exit from the vascular bed occurs as a result of chemotaxis) and only after activation of neutrophils. The main function is phagocytosis of tissue debris and destruction of opsonized microorganisms. Phagocytosis and subsequent digestion of the material occurs in parallel with the formation of arachidonic acid metabolites and respiratory burst. Phagocytosis occurs in several stages. After preliminary specific recognition of the material to be phagocytosed, invagination of the neutrophil membrane around the particle occurs and the formation of a phagosome. Next, as a result of the fusion of the phagosome with lysosomes, a phagolysosome is formed, after which the bacteria are destroyed and the captured material is destroyed. For this, the following enter the phagolysosome: lysozyme, cathepsin, elastase, lactoferrin, defensins, cationic proteins; myeloperoxidase; superoxide O2– and hydroxyl radical OH–, formed (along with H2O2) during a respiratory explosion. After a single burst of activity, the neutrophil dies. Such neutrophils constitute the main component of pus (“pus” cells).
Activation
. Biologically active compounds of various origins [for example, the contents of platelet granules, arachidonic acid metabolites (lipid mediators)], acting on neutrophils, stimulate their activity (many of these substances are at the same time chemoattractants, along the concentration gradient of which neutrophils migrate).
Lipid mediators
produce activated neutrophils, as well as basophils and mast cells, eosinophils, monocytes and macrophages, platelets. In an activated cell, arachidonic acid is released from membrane phospholipids, from which prostaglandins, thromboxanes, leukotrienes and a number of other biologically active substances are formed.
Respiratory Burst
.
During the first seconds after stimulation, neutrophils sharply increase oxygen absorption and quickly consume a significant amount of it. This phenomenon is known as respiratory
(
oxygen
)
burst
. This produces H2O2, superoxide O2–, and hydroxyl radical OH–, which are toxic to microorganisms.
Chemotaxis
. Neutrophils migrate to the site of infection along a concentration gradient of many chemical factors (Table 24–11). Important among them are N-formylmethionyl peptides (for example, the chemoattractant f-Met-Leu-Phe), which are formed during the breakdown of bacterial proteins or mitochondrial proteins during cell damage.
Adhesion
. The activated neutrophil attaches to the vascular endothelium. Adhesion to the endothelium is stimulated by many agents: anaphylatoxins, IL-I, thrombin, platelet activating factor PAF, leukotrienes LTC4 and LTB4, tumor necrosis factor a, etc.
Migration
.
After attaching to the endothelium and leaving the vessel, neutrophils increase in size, elongate and become polarized, forming a broad head end (lamellipodia) and a narrowed posterior part. The neutrophil, moving the lamellipodia forward, migrates to the source of the chemoattractant. In this case, the granules move to the head end, their membranes merge with the plasmalemma, and the contents of the granules (including proteases) are released from the cell - degranulation
.
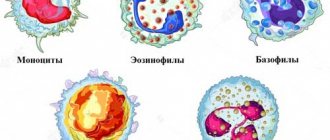
Eosinophils
Eosinophil (Fig. 24–19, see also Fig. 24–2, 4) is a granular leukocyte involved in allergic, inflammatory and antiparasitic reactions. Eosinophils make up 1–5% of white blood cells circulating in the blood. Their number varies throughout the day and is maximum in the morning. Eosinophils remain in the bone marrow for several days after formation, then circulate in the blood for 3–8 hours, most of them leaving the bloodstream. Eosinophils migrate to tissues in contact with the external environment (mucous membranes of the respiratory and genitourinary tracts, intestines). The size of the eosinophil in the blood is >12 µm, increasing after entering the connective tissue to 20 µm. Life expectancy is estimated to be 8–14 days. Eosinophils on their surface have membrane receptors for the Fc fragments of IgG, IgM and IgE, complement components C1s, C3a, C3b, C4 and C5a, the chemokine eotaxin, IL5. The migration of eosinophils in tissues is stimulated by eotaxin, histamine, eosinophil chemotaxis factor ECF, IL5, etc. After performing their functions (after degranulation) or in the absence of activation factors (for example, IL-5), eosinophils die.
Rice
.
24–19
.
Eosinophil
[11]. The eosinophil nucleus usually forms two large segments connected by a thin bridge. The cytoplasm contains a moderate amount of typical organelles, glycogen. Large ovoid-shaped granules contain electron-dense material - crystalloid. The cell forms cytoplasmic projections, with the help of which it moves in tissues.
· Specific granules
.
The cytoplasm of the eosinophil contains large and small specific granules (red-orange). Large granules
measuring 0.5–1.5 µm are ovoid in shape and contain an elongated crystalloid.
The crystalloid has a cubic lattice structure and consists mainly of the antiparasitic agent major alkaline protein (MBP). Large granules also contain neurotoxin (protein X), eosinophil peroxidase EPO, histaminase, phospholipase D, hydrolytic enzymes, acid phosphatase, collagenase, zinc, cathepsin. Small granules
contain arylsulfatase, acid phosphatase, peroxidase, and cationic eosinophil protein ECP. During allergic and inflammatory reactions, the contents of the granules are secreted (degranulation).
· Metabolic activity
. Like neutrophils, eosinophils synthesize arachidonic acid metabolites (lipid mediators), including leukotriene LTC4 and platelet activating factor PAF.
· Activation
. Eosinophils are activated by many factors from a wide variety of cells: interleukins (IL2, IL3, IL5), colony-stimulating factors GM-CSF and G-CSF, platelet activating factor PAF, tumor necrosis factor TNF, interferons and factors from parasites.
· Chemotaxis
. Activated eosinophils move along a gradient of chemotaxis factors - bacterial products and complement elements. Particularly effective as chemoattractants are substances secreted by basophils and mast cells—histamine and eosinophil chemotaxis factor ECF.
· Functions
. Destruction of parasites, participation in allergic and inflammatory reactions. Eosinophils are capable of phagocytosis, but less pronounced than neutrophils.
à Destruction of parasites
. Eosinophilia occurs in many parasitic diseases. Eosinophils are especially active in destroying parasites at the sites of their introduction into the body, but are less effective against parasites that have reached the area of final localization. After activation by AT and complement components, eosinophils release the contents of granules and lipid mediators, which has a damaging effect on parasites. Secretion of the contents of the granules starts within a few minutes and can last for several hours.
à Participation in allergic reactions
. The contents of eosinophil granules inactivate histamine and leukotriene LTC4. Eosinophils produce an inhibitor that blocks mast cell degranulation. Slow reacting factor anaphylaxis (SRS-A), released by basophils and mast cells, is also inhibited by activated eosinophils.
à Participation in inflammatory reactions
. Eosinophils respond by chemotaxis to many signals emanating from the endothelium, macrophages, parasites and damaged tissues.
à Side effects of eosinophils
. Substances secreted by the eosinophil can damage normal tissue. Thus, with a constant high content of eosinophils in the blood, chronic secretion of the contents of eosinophil granules causes thromboembolic damage, tissue necrosis (especially the endocardium) and the formation of fibrous tissue. IgE stimulation of eosinophils can cause reversible changes in vascular permeability. Secretion products of eosinophils damage the bronchial epithelium and activate complement and the blood coagulation system.
Basophils
Basophils (Fig. 24–20, see also Fig. 24–2, 5) make up 0–1% of the total number of leukocytes in circulating blood. Basophils with a diameter of 10–12 microns remain in the blood for 1–2 days. Like other granular leukocytes, basophils can leave the bloodstream when stimulated, but their ability for amoeboid movement is limited. Lifespan and tissue fate are unknown.
Basophils and mast cells are similar in many ways. However, they have morphological and functional differences, are distributed differently in tissues and belong to different cell types.
Rice
.
24–20
.
Basophil
[11]. The weakly lobed nucleus is curved in the shape of the letter S. Specific granules vary in size and shape.
· Specific granules
quite large (0.5–1.2 µm), colored metachromatically (in a different color than the dye, from reddish-violet to intense violet). The granules contain various enzymes and mediators. The most significant of them include heparin sulfate (heparin), histamine, inflammatory mediators (for example, slow-reacting anaphylaxis factor SRS-A, eosinophil chemotaxis factor ECF).
· Metabolic activity
. When activated, basophils produce lipid mediators. Unlike mast cells, they do not have PGD2 synthetase activity and oxidize arachidonic acid predominantly to leukotriene LTC4.
· Function
. Activated basophils leave the bloodstream and participate in allergic reactions in tissues. Basophils have high-affinity surface receptors for the Fc fragments of IgE, and IgE is synthesized by plasma cells when Ag (allergen) enters the body. Basophil degranulation is mediated by IgE molecules. In this case, cross-linking of two or more IgE molecules occurs. The release of histamine and other vasoactive factors during degranulation and the oxidation of arachidonic acid cause the development of an immediate allergic reaction (such reactions are characteristic of allergic rhinitis, some forms of bronchial asthma, anaphylactic shock).
Monocytes
Monocytes (Fig. 24–1, E; see also Fig. 24–2,7) are the largest leukocytes (diameter in a blood smear is about 15 µm), their number is 2–9% of all leukocytes in circulating blood. They are formed in the bone marrow, enter the bloodstream and circulate for about 2–4 days. Blood monocytes are actually immature cells on their way from the bone marrow to the tissues. In tissues, monocytes differentiate into macrophages; a collection of monocytes and macrophages - a system of mononuclear phagocytes
.
· Monocyte activation
. Various substances formed at sites of inflammation and tissue destruction are agents of chemotaxis and activation of monocytes. As a result of activation, cell size increases, metabolism increases, monocytes secrete biologically active substances (IL1, colony-stimulating factors M-CSF and GM-CSF, Pg, interferons, neutrophil chemotaxis factors, etc.).
· Function
. The main function of monocytes and macrophages formed from them is phagocytosis. Lysosomal enzymes, as well as intracellularly formed H2O2, OH–, O2–, participate in the digestion of phagocytosed material. Activated monocytes/macrophages also produce endogenous pyrogens.
Pyrogens
.
Monocytes/macrophages produce endogenous pyrogens
(IL1, IL6, IL8, tumor necrosis factor TNFa, a-interferon) - polypeptides that trigger metabolic changes in the thermoregulation center (hypothalamus), which leads to an increase in body temperature.
The formation of prostaglandin PGE2 plays a critical role. The formation of endogenous pyrogens by monocytes/macrophages (as well as a number of other cells) is caused by exogenous pyrogens
- proteins of microorganisms, bacterial toxins. The most common exogenous pyrogens are endotoxins (lipopolysaccharides of gram-negative bacteria).
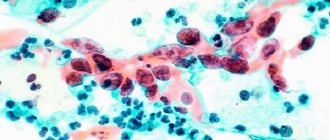
Macrophage
- differentiated form of monocytes - large (about 20 microns), mobile cell of the mononuclear phagocyte system.
Macrophages
are
professional phagocytes
, they are found in all tissues and organs; they are a mobile population of cells. The lifespan of macrophages is months. Macrophages are divided into resident and mobile. Resident macrophages are present in tissues normally, in the absence of inflammation. Among them, there are free, round-shaped, and fixed macrophages - star-shaped cells, attached with their processes to the extracellular matrix or to other cells.
· Properties of a macrophage
depend on their activity and location. The lysosomes of macrophages contain bactericidal agents: myeloperoxidase, lysozyme, proteinases, acid hydrolases, cationic proteins, lactoferrin, superoxide dismutase, an enzyme that promotes the formation of H2O2, OH–, O2–. Under the plasmalemma, actin microfilaments, microtubules, and intermediate filaments necessary for migration and phagocytosis are present in large quantities. Macrophages migrate along a concentration gradient of many substances coming from various sources. Activated macrophages form irregularly shaped cytoplasmic pseudopodia that participate in amoeboid movement and phagocytosis.
· Functions
.
Macrophages capture denatured proteins and aged red blood cells from the blood (fixed macrophages of the liver, spleen, bone marrow). Macrophages phagocytose cell debris and tissue matrix. Nonspecific phagocytosis
is characteristic of alveolar macrophages, capturing dust particles of various natures, soot, etc.
Specific phagocytosis
occurs when macrophages interact with an opsonized bacterium. An activated macrophage secretes more than 60 factors (Table 24–12). Macrophages exhibit antibacterial activity by releasing lysozyme, acid hydrolases, cationic proteins, lactoferrin, H2O2, OH–, O2–. Antitumor activity consists of the direct cytotoxic effect of H2O2, arginase, cytolytic proteinase, tumor necrosis factor (TNF) from macrophages. A macrophage is an antigen-presenting cell: it processes Ag and presents it to lymphocytes, which leads to stimulation of lymphocytes and the launch of immune reactions (see more in Chapter 29). IL1 from macrophages activates T lymphocytes and, to a lesser extent, B lymphocytes. Macrophages produce lipid mediators - PgE2 and leukotrienes, platelet activating factor PAF. The cell also secretes α-IFN, which blocks viral replication. An activated macrophage secretes enzymes that destroy the extracellular matrix (elastase, hyaluronidase, collagenase). On the other hand, growth factors synthesized by macrophages effectively stimulate the proliferation of epithelial cells (transforming growth factor TGFa, fibroblast growth factor bFGF), proliferation and activation of fibroblasts (platelet-derived growth factor PDGF), collagen synthesis by fibroblasts (transforming growth factor TGFb), formation new blood vessels - angiogenesis (fibroblast growth factor bFGF). Thus, the main processes underlying wound healing (reepithelialization, extracellular matrix formation, repair of damaged vessels) are mediated by growth factors produced by macrophages. By producing a number of colony-stimulating factors (macrophages - M-CSF, granulocytes - G-CSF), macrophages influence the differentiation of blood cells.
Lymphocytes
Lymphocytes (Fig. 24–1, E; see also Fig. 24–2,6) make up 20–45% of the total number of blood leukocytes. Blood is the medium in which lymphocytes circulate between the organs of the lymphoid system and other tissues. Lymphocytes can exit the vessels into the connective tissue, and also migrate through the basement membrane and penetrate the epithelium (for example, in the intestinal mucosa). Lifespan of lymphocytes: from several months to several years. Lymphocytes are immunocompetent cells that are of great importance for the body’s immune defense reactions (see Chapter 29 for more details). From a functional point of view, B lymphocytes, T lymphocytes and NK cells are distinguished.
· B lymphocytes
(pronounced “b”) are formed in the bone marrow and make up less than 10% of blood lymphocytes. Some B lymphocytes in tissues differentiate into clones of plasma cells. Each clone synthesizes and secretes antibodies against only one Ag. In other words, plasma cells and the antibodies they synthesize provide humoral immunity.
Differentiation B
-
lymphocytes in Ig
-
producing plasma cells
. Bone marrow stem cells undergo a series of differentiation steps to become mature B lymphocytes (plasma cells). There are six stages of B cell maturation: pro-B cell ® pre-B cell ® B cell expressing membrane Ig (m-chain or m-chain and d-chain) ® activated B cell ® B lymphoblast ® plasma cell that secretes Ig.
· T
-
lymphocytes
The precursor cell of T-lymphocytes enters the thymus from the bone marrow. Differentiation of T lymphocytes occurs in the thymus. Mature T lymphocytes leave the thymus and are found in the peripheral blood (80% or more of all lymphocytes) and lymphoid organs. T-lymphocytes, like B-lymphocytes, respond (i.e., recognize, multiply and differentiate) to specific Ags, but - unlike B-lymphocytes - the participation of T-lymphocytes in immune reactions is associated with the need to recognize other cells in the membrane MHC major histocompatibility complex proteins. The main functions of T‑lymphocytes are participation in cellular and humoral immunity (thus, T‑lymphocytes destroy abnormal cells of their body, participate in allergic reactions and in the rejection of foreign transplants). Among T‑lymphocytes, CD4+- and CD8+‑lymphocytes are distinguished. CD4+ lymphocytes (T helper cells) support the proliferation and differentiation of B lymphocytes and stimulate the formation of cytotoxic T lymphocytes, as well as promote the proliferation and differentiation of suppressor T lymphocytes.
· NK cells
— lymphocytes lacking the surface cellular determinants characteristic of T and B cells. These cells make up about 5–10% of all circulating lymphocytes, contain cytolytic granules with perforin, and destroy transformed (tumor) and virus-infected cells, as well as foreign cells.
Classifications
. Previously, lymphocytes were divided into various categories based on their size, but their functional classification is much more important.
· Cell size
. The population of lymphocytes according to this characteristic is heterogeneous; their size in the blood varies from 4.5 to 10 µm: small (4.5–6 µm), medium (7–10 µm) and large lymphocytes (10–18 µm).
· Functional classification
. Lymphocytes include morphologically similar but functionally different cells: B lymphocytes, T lymphocytes and NK cells. The classification of lymphocytes according to differentiation Ag - CD markers is also of great practical importance.
6
Didn't find what you were looking for? Use Google search on the site:
Lifespan of white blood cells
What is the lifespan of leukocytes in the blood? We can say that white blood cells live fast and die young. They have a relatively short life cycle - from several days to several weeks. But this does not mean at all that they are fragile and unreliable. The power lies in numbers: one drop of blood can contain from 7 to 25 thousand white blood cells at the same time. This number may increase if a contagious infection is present.
The life of granulocytes after leaving the bone marrow is usually from 4 to 8 hours if they circulate in the blood, and from 4 to 5 days if they move through tissues. During severe infection, the total lifespan of white blood cells is often reduced to just a few hours. Lymphocytes enter the circulatory system constantly, along with drainage of lymph from lymph nodes and other lymphoid tissue. After a few hours, they move from the blood back into the tissue, then return to the lymph and thus circulate. The lifespan of leukocytes can vary from several weeks to several months, it all depends on the body’s need for these cells.
Functions of leukocytes
The main purpose of leukocytes is to prevent infection from attacking the body, i.e. During their existence, they constantly fight with foreign bodies.
Several of their functions should be highlighted:
- informational;
- protection against malicious agents;
- antibody production;
- hemostatic;
- transport;
- synthetic;
- movement of leukocytes.
The concentration of white cells in the blood can indicate existing disorders or the possible development of pathology. Protective function, or phagocytosis, is the process of absorption and destruction of harmful microorganisms by leukocytes.
The hemostatic effect ensures blood clotting based on the synthesis of histamine and heparin.
The production of antibodies involves the formation of protein compounds capable of actively resisting pathogens.
White cells perform a transport function, ensuring the transfer of active components, substances and amino acids to organ tissues through blood vessels.
With the development of any inflammatory process or disease, active emigration of white blood cells occurs, in which protective cells are transferred to the affected areas of the body, destroying diseased tissue.
Important information: What are platelets according to Fonio (normal)
Protection against infections
Blood is made up of several components, including red blood cells, white blood cells, platelets, and plasma. A healthy adult has between 4,500 and 11,000 white blood cells per cubic millimeter of blood. White blood cells, also called leukocytes or white corpuscles, are a cellular component of blood that protects the body from infection and disease by ingesting foreign materials and destroying infectious agents, including cancer cells, and by producing antibodies.
An abnormal increase in the number of white cells is known as leukocytosis, while an abnormal decrease in the number is called leukopenia. The number of white blood cells can increase in response to intense physical activity, convulsions, acute emotional reactions, pain, pregnancy, childbirth and some other painful conditions, such as infections and intoxications. Their numbers may decrease in response to certain types of infections or drugs, or in combination with certain conditions, such as chronic anemia, malnutrition, or anaphylaxis.
Blood composition
This section of the article is devoted to all components of human blood. What does it consist of? So, in human blood we can find the following components:
All components are necessary and perform their special function. Thus, red blood cells perform the function of transporting oxygen. They are red in color due to the content of hemoglobin; their quantity exceeds all other components. Leukocytes are white and perform a protective function. The lifespan of leukocytes is short. Platelets are responsible for blood clotting, thanks to them we do not bleed due to an ordinary small cut with a knife.
An important component of the blood system
White blood cells are an important component of the blood system, which also consists of red blood cells, platelets and plasma. Although they make up only about 1% of all blood, their impact is significant: they are essential for good health and protection against disease. We can say that these are immune cells. In a sense, they are constantly at war with viruses, bacteria and other “foreign invaders” that threaten your health.
When a specific area is attacked, white blood cells rush to destroy the harmful substance and prevent disease. White blood cells are produced within the bone marrow and stored in the blood and lymph tissues. Since the lifespan of human leukocytes is short, some types have a completely short lifespan - from one to three days. Therefore, the bone marrow is engaged in their constant reproduction.
Leukocytes in the blood
Leukocytes in the blood are components of the main biological fluid of the human body. They are divided into several subspecies, each of which performs its own specific function. The main task of white blood cells is to protect internal organs and systems from various infections.
The concentration of such substances has its own norm, which differs depending on the age category and gender. Acceptable indicators can either increase or decrease. Such deviations occur due to either pathological or physiological reasons.
If the leukocytes in the analysis differ from the acceptable values, then this will in any case affect the person’s well-being. For example, you may experience: dizziness, headaches, fatigue, weakness, increased temperature and problems sleeping.
The norm of leukocytes in the blood is calculated during the decoding of a general clinical analysis of biological fluid. However, to find the factor that provoked any deviation from the norm, a comprehensive examination is necessary.
The tactics for normalizing the concentration of such components of the main biological fluid are compiled individually for each person, but in general they are based on getting rid of the provoking disease. Leukocytes in the blood should always be normal.
Leukocytes in the blood are a group of cells that are responsible for the human body’s resistance to various pathogenic bacteria, viruses, helminths, parasites and other pathological microorganisms.
They also fight not only infectious agents, but also any foreign object:
- malignant or benign neoplasms of any location;
- transplanted donor organ;
- a foreign object that may accidentally enter the body.
The place of formation of leukocytes is blood stem cells, which are localized in the red bone marrow. In order to fully carry out their work, they undergo a large number of transformations, during which their structure and functions change.
In addition to blood, they are also found in fluids such as:
- urine;
- cerebrospinal fluid;
- pleural effusion;
- feces;
- gastric juice.
However, their concentration in such cases will be significantly lower, for example, for urine analysis, from 4 to 6 leukocytes are acceptable, and no more than 8 white blood cells should be present in the cerebrospinal fluid.
An increase or decrease in such blood components in any of the above structures most often indicates the occurrence of a disease.
In addition to the main task, the functions of leukocytes include:
- release of specific substances to combat various tumors;
- absorption and digestion of the pathogenic agent;
- relief of hemorrhages;
- acceleration of wound healing.
As stated above, white blood cells have several subtypes.
Thus, there are the following types of leukocytes:
- neutrophils - aimed at destroying bacterial infection;
- lymphocytes – responsible for the immune system and immune memory;
- monocytes - absorb and digest particles of foreign cells;
- eosinophils - fight allergen carriers;
- basophils - assist other particles in detecting foreign agents, however, they perform all their “duties” outside the bloodstream - in the internal organs.
It follows from this that subtypes of leukocytes perform their own mission.
All types of such substances, in addition to their functions, differ in the following indicators:
- dimensions;
- core shape;
- way of development.
It is also worth noting about the structural features of each type of white blood cell. For example, neutrophils, eosinophils, basophils and monocytes are born from myeloblasts, the precursor of which is myelopoiesis. This happens under the influence of a stimulator cell in the bone marrow.
The lifespan of leukocytes is on average 2-4 days, and they are often destroyed in the liver, spleen and foci of inflammatory processes. The only exceptions are lymphocytes, some of which live in the human body from birth to death.
In neutrophils, eosinophils and basophils, the entire life cycle takes place in the bone marrow, which is why their immature cells are normally completely absent from the blood. Monocytes continue to exist in the spleen, liver and skeletal system, where they degenerate into macrophages and dendrocytes. Lymphocytes have a longer “life” in the spleen, lymph nodes and thymus.
Leukocytes received their common name - white blood cells - because, unlike red blood cells, they are colorless.
From all of the above, it follows that if there are no leukocytes in the blood, the human body simply will not be able to function.
The norm of leukocytes in the blood differs according to two parameters - gender and age category. The total number of such particles can be detected during a general blood test, but to identify the concentration of a particular subspecies, an extensive study of biological material is required.
Leukocytes should normally be:
- neutrophils – 55%;
- lymphocytes – 35%;
- monocytes – 5%;
- basophils – 1%;
- eosinophils – 2.5%.
In general, the normal leukocyte count in the blood is:
| Age category | Acceptable values (x 109/l) |
| Infants | 7-32 |
| Children under one year old | 6-18.5 |
| 1-2 years | 5-17 |
| 2-6 years | 5-16.5 |
| 6-15 years |
Source: https://MedAnaliz.pro/krov/lejkocity
Types of leukocytes
- Monocytes. They have a longer lifespan than many white blood cells and help destroy bacteria.
- Lymphocytes. They produce antibodies to protect against bacteria, viruses and other potentially harmful invaders.
- Neutrophils. They kill and digest bacteria and fungi. They are the most numerous type of white blood cells and the first line of defense against infections.
- Basophils. These small cells release chemicals such as histamine and an allergy marker that help control the body's immune response.
- Eosinophils. They attack and kill parasites, destroy cancer cells and help with allergic reactions.
Types of leukocytes
There are several patterns of white blood cells responsible for fixed processes:
- Monocytes. Their main task is to suppress and remove harmful bacteria through urine and pus. Their lifespan is longer than that of other white cells.
- Lymphocytes. These blood cells are the main element of immunity. Lymphocytes strike at harmful “invaders”, while retaining all information about them, which makes it possible to react faster and more actively in the event of a repeated attack. In addition, they are able to transform into lymphoblasts, which are distinguished by a high reproduction rate, and transform into killer cells that destroy foreign bodies. This is how human immunity is formed and works.
- Basophils. They play their main role in the process of blood clotting. They also secrete special substances that help the body when it is poisoned by various poisons, toxins or vapors.
- Neutrophils. Their total amount in the blood is 70%. Their main purpose is to eliminate infectious agents and other harmful particles that penetrate along with the infection.
- Eosinophils. Actively participate in the absorption of harmful microbes and neutralize allergic manifestations.
Important information: What are atypical lymphocytes in a blood test (interpretation for adults and children)
The bigger, the better?
Even with all their disease-fighting abilities, too many white blood cells can be a bad sign. For example, a person suffering from leukemia, a blood cancer, may have up to 50,000 white blood cells in one drop of blood. All its elements (erythrocytes, leukocytes and platelets) come from hematopoietic stem cells and bone marrow, as well as the umbilical cord of newborn children. On average, the body of an adult contains about 5 liters of blood, which mainly consists of plasma (55-60%) and blood cells (40-45%). The lifespan of red blood cells, white blood cells and platelets, as well as their structure and composition, differ, but they all play an important role in the functioning of the body.
The number of red and white blood cells in the blood can serve as an indicator of certain diseases. Leukopenia can be caused by factors that can impair bone marrow function. A condition characterized by a low number of red blood cells is usually called anemia, and can include iron deficiency and vitamin B12 deficiency. This disease can impair the blood's ability to carry oxygen, which may result in increased fatigue, shortness of breath, and paleness. The lifespan of white blood cells, platelets and red blood cells, their appearance, composition and functions are radically different, but they all play an important role. Thus, a reduction or significant increase in their number can lead to various health problems.
Leukocytes in the blood: where they are formed and what they are responsible for in the body
Blood structure.
Leukocytes are distinguished by their lack of color. Due to their colorless cytoplasm, variable shape, and amoeboid movement, leukocytes are called white cells (or amoebae) that “float” in the lymph or blood plasma. The rate of leukocytes is within 40 µm/min.
Important! An adult in the morning on an empty stomach has a leukocyte ratio of 1 mm - 6000-8000. Their numbers change during the day due to a different functional state. A sharp increase in the level of leukocytes in the blood is leukocytosis, a decrease in the concentration is leukopenia.
Main functions of leukocytes
The spleen, lymph nodes, red marrow in the bones are organs where leukocytes are formed. Chemical elements irritate and force leukocytes to leave the bloodstream, penetrate the endothelium of the capillaries in order to quickly reach the source of irritation.
These can be remnants of the vital activity of microbes, decaying cells, anything that can be called foreign bodies or antigen-antibody complexes. White cells use positive chemotaxis towards stimuli, i.e.
they have a motor response.
Characteristics of leukocytes
The main functional work for which leukocytes are responsible is the transport of oxygen to all tissues at the cellular level and the removal of carbon dioxide from them, as well as the protection of the body: specific and nonspecific from external and internal pathological influences and processes, from bacteria, viruses and parasites. Wherein:
- immunity is formed: specific and nonspecific;
- nonspecific immunity is formed with the participation of the resulting antitoxic substances and interferon;
- The production of specific antibodies begins.
We also recommend that you pay attention to the article: “Blood gas analysis”
Leukocytes, using their own cytoplasm, surround and digest a foreign body with special enzymes, which is called phagocytosis.
Important! One leukocyte digests 15-20 bacteria. Leukocytes are capable of secreting important protective substances that heal wounds and have a phagocytic reaction, as well as antibodies with antibacterial and antitoxic properties.
In addition to the protective function of leukocytes, they also have other important functional responsibilities. Namely:
- Transport. Amoeba-shaped white cells adsorb protease from the lysosome with peptidase, diastase, lipase, deoxyribronuclease and carry these enzymes on themselves to problem areas.
- Synthetic. If there is a lack of active substances in the cells: heparin, histamine and others, white cells synthesize biological substances that are missing for the life and activity of all systems and organs.
- Hemostatic. Leukocytes help the blood to quickly clot with the leukocyte thromboplastins they secrete.
- Sanitary. White blood cells promote the resorption of cells in tissues that died during injuries, due to the enzymes that they carry from lysosomes.
About
The white blood cell count should be under control
Doctors recommend checking your white blood cell levels periodically. If their number remains high or low for a long time, this may indicate a deterioration in health. As for red blood cells, their lifespan is three to four months. Leukocytes are significantly inferior in this regard. Yet it is an important part of the body’s defense against infectious and foreign substances. You can check the amount and condition of your blood using special laboratory tests.
Where are leukocytes produced?
Leukocytes with red blood cells and platelets are formed by the hematopoietic immune system, which contains:
- tonsils;
- Bone marrow;
- thymus gland (thymus);
- lymphoid formations in the intestines (Peyer's patches);
- spleen;
- The lymph nodes.
The bone marrow is the main site of formation of leukocytes. These cells are produced in large numbers in the body because after the harmful body is destroyed, they die along with it.
Bodies spread in the following fluids of biological origin: in blood plasma, in urine (in small quantities in a healthy person), in a woman’s vaginal lubrication, etc.
Leukocyte disorders
The main disorders of leukocytes include the following pathological conditions:
- Neutropenia (abnormally low neutrophil count).
- Neutrophil leukocytosis (abnormally high number of neutrophils).
- Lymphocytopenia (abnormally low number of lymphocytes).
- Lymphocytic leukocytosis (abnormally high number of lymphocytes).
The most common are disorders of neutrophils and lymphocytes. Abnormalities associated with monocytes and eosinophils are less common, and problems associated with basophils are less common.
Classification of leukocytes
All leukocytes are conventionally divided into two large groups:
- Granulocytes are distinguished by the granular structure of the cytoplasm. Granulocytes have an irregularly shaped nucleus divided into segments. As the cell ages, the number of segments increases.
- Agranulocytes - characterized by the absence of granularity in the cytoplasm, have a rounded nucleus, not divided into fragments.
The following table will help you study all types of leukocytes:
| Leukocytes | Size | Structure | Quantity | Coloring |
| Granulocytes | Neutrophils | 9-12 microns | They have a core segmented into 4-5 parts | 60-70% of the total number of leukocytes | Stained with eosin and basic dyes |
| Eosinophils | 12-17 microns | They have a core segmented into 2 parts | 1-5% of total leukocytes | Stained only with eosin (red) | |
| Basophils | 10-15 microns | Have an unsegmented nucleus | Less than 1% of total leukocytes | Can be dyed with basic dyes only | |
| Agranulocytes | Lymphocytes | 6-10 microns, sometimes up to 12 microns | Globular cell with a very large round nucleus | 25-35% of the total number of leukocytes | Stained according to Romanovsky-Giemsa blue with purple nuclei |
| Monocytes | 18-20 microns | Oval cell with eccentrically located bean-shaped nucleus | 3-10% of the total number of leukocytes | Stained according to Romanovsky-Giemsa in gray with red nuclei |
Destruction of leukocytes
The lifespan of leukocytes, platelets and erythrocytes has been sufficiently studied, which cannot be said about the processes of their destruction. It is known that all types of white cells, after a certain period of circulation in the blood, enter the tissues. There is no turning back now. In tissues they perform their phagocytic function and die. Important contributions to the study of white blood cells and their properties were made by Ilya Mechnikov and Paul Ehrlich. The first discovered and studied the phenomenon of phagocytosis, and the second brought out various types of leukocytes. In 1908, the scientists were jointly awarded the Nobel Prize for these achievements.
Formation of leukocytes
The shape of the cells resembles a sphere, inside of which there is a large nucleus and a small amount of cytoplasm. It is considered the most common type of white blood cell.
As a rule, they form in the bone marrow. This is explained by the fact that after the destruction of foreign harmful substances, leukocytes die along with them. However, in small quantities they are also formed in the thymus gland, spleen, lymph nodes and in the intestines and tonsils.
This is interesting! Leukocytes are non-white. When examined in more detail under a microscope, they have a pink-violet color.
Leukocytes have very complex chemical pathways. They are capable of synthesizing protein and producing ribonucleic acid. However, they do not undergo mitosis in the blood, but there are some types that still retain this function. White cells are divided into three classes. They all perform their specific role and functions.
White blood cells are counted as follows:
- Acetic acid, tinted with methylene blue, is poured into a glass test tube. This is a reagent into which you need to drop a little blood using a pipette for analysis. Afterwards everything is mixed well.
- Wipe the glass and camera with gauze. Next, the glass is ground against the chamber until rings of different colors begin to form. The chamber is completely filled with plasma. You need to wait 60 seconds until the cell movement stops. The calculation is carried out using a special formula.
What does an increase in the concentration of leukocyte particles in the blood mean?
An increase in the number of white blood cells is called leukocytosis. The physiological form of this condition is observed even in a healthy person. And this is not a sign of pathology. This occurs after long-term exposure to direct sunlight, due to stress and negative emotions, and heavy physical exercise. In females, high white blood cells are observed during pregnancy and the menstrual cycle.
When the concentration of leukocyte cells exceeds the norm several times, you need to sound the alarm. This is a dangerous signal indicating the occurrence of a pathological process. After all, the body tries to protect itself from a foreign agent by producing more defenders - leukocytes.
After making a diagnosis, the attending physician should solve one more problem - to find the root cause of the condition. After all, it is not leukocytosis that is treated, but what caused it. Once the cause of the pathology is eliminated, after a couple of days the level of leukocyte cells in the blood will return to normal on its own.
Structure and what they look like
The shape of leukocytes is round or oval. Their color is usually considered white, since there is no independent coloring. In order to see leukocytes under a microscope, the biomaterial is pre-stained; each type of cell reacts to staining in its own way.
Cell morphology:
- granular granulocytes,
- agranulocytes are not granular.
The simplified structure of leukocytes is characterized by the presence of a nucleus and cytoplasm, but each type has its own structural features:
- Neutrophilic. The cytoplasm is fine-grained with a homogeneous narrow border containing thin filaments. The cytoplasm also contains mitochondria, organelles, the Golgi complex, inclusions of glycogen, lipids, and granular endoplasmic reticulum. The nucleus contains dense chromantin.
- Eosinophilic. The nucleus includes heterochromatin. The cytoplasm contains granules of two types:
- oval-shaped, 0.5-1.5 microns in size, containing the amino acid arginine, hydrolytic enzymes,
- round in size, 0.1-0.5 microns in size, containing arylsulfatase and acid phosphatase.
- Basophilic. The cytoplasm includes round, large basophilic granules with a diameter of 0.5-1.2 microns. They contain acid glycosaminoglycan-heparin and histamine. The nucleus is weakly lobed and sometimes spherical.
Lymphocytes are characterized by a rounded nucleus with intense color and a small rim of cytoplasm, which contains a small content of ribosomes and polysomes. The nucleus is round with chromatin condensed along the periphery.
Depending on the structural features and functions of cells, the lifespan of leukocytes in human blood has the following range: from 2 to 15 days. The exception is lymphocytes, which live from a couple of days to several years, some of them accompany a person throughout his life.