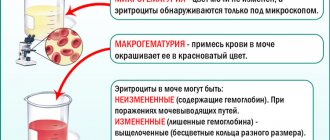
Red blood cells are changed (leached). They do not have hemoglobin. The study of laboratory urine tests clarifies the clinical picture of various pathological processes in the human body, this is due to the fact that the kidneys work as a blood filter. The phenomenon of hematuria is observed when a visible number of red blood cells appears in a general urine analysis. In the case when several red blood cells enter the field of view, they speak of microhematuria. When urea turns scarlet, it is said to have gross hematuria. The norm is considered to be no more than 2 red blood cells within the microscope's viewing circle (field of view).
Etiology
Hemolysis of red blood cells occurs on an ongoing basis in every living organism. Normally, red blood cells live for about 120 days, after which their gradual destruction begins. The membrane ruptures and hemoglobin is released. Under physiological conditions, such processes occur in the spleen with the help of cells of the immune system.
Red blood cells can die in the vascular bed. In such cases, hemoglobin interacts with a specific protein found in the blood plasma and enters the liver. After this, a whole chain of complex transformations occurs, after which the iron-containing protein becomes bilirubin and is excreted from the body along with bile. All this constitutes pathological hemolysis.
Hemolysis of red blood cells
The causes of hemolysis can be very diverse, but are often associated with the course of a disease. Thus, the following can act as provocateurs:
- diseases of an autoimmune nature;
- parasitic infestations;
- toxins - waste products of viruses or bacteria;
- penetration of toxic substances or poisons into the body - the most dangerous are lead and arsenic, gasoline and vinegar essence;
- bites from poisonous insects or snakes;
- irrational use of certain medicinal substances, in particular sulfonamides;
- eating poisonous mushrooms;
- transfusion of incompatible blood;
- conflict between the Rh factor of mother and fetus;
- DIC syndrome;
- the presence of acute infections, such as malaria or mononucleosis;
- entry into the bloodstream of cadmium, mercury or other heavy metals;
- extensive thermal or chemical burns;
- sepsis.
A genetic predisposition can contribute to the fact that red blood cells are defective (osmotic hemolysis).
Pathological hemolysis: causes and types
Types of hemolysis and the causes that caused it:
- Immune
. Caused by autoimmune diseases, hemolytic anemia, and blood transfusion incompatibility.
- Mechanical
. Occurs when tissue is crushed, extensive injuries, or careless handling of blood samples.
- Thermal
. It is caused by freezing and heating solutions.
- Chemical
. Occurs upon contact with aggressive media that penetrate through the respiratory or digestive system as a result of injections. In the laboratory, samples can be spoiled if they come into contact with acid or alkali.
- Electric
. Occurs due to electric shock, in the laboratory - when blood is placed in an electric field.
- Biological
. Develops due to exposure to poisons of animal or plant origin: snake bite, contact with toadstool and other poisonous mushrooms, penetration of malarial plasmodium into the body.
- Osmotic
. It occurs due to the effect on red blood cells of a hypotonic solution (0.48%, 0.32%) of sodium chloride, which is used to increase the volume of circulating blood and destroys red blood cells.
Classification
Based on the nature of the formation of hemolysis of red blood cells, a similar condition occurs:
- physiological;
- pathological.
Depending on where red blood cells are destroyed, there are:
- intracellular hemolysis - destruction occurs in the spleen;
- intravascular hemolysis - the process develops in the vascular bed.
There are 2 types of erythrocytolysis:
- hereditary - there is an abnormal structure of red blood cells, dysfunction of the enzymatic system or a defective composition of red cells;
- acquired.
If the destruction of red blood cells occurs due to the course of any disease or pathological process, based on the mechanism of development, the following is released:
- osmotic hemolysis - develops in laboratory conditions;
- biological hemolysis - the result of transfusion of incompatible blood components, viremia;
- temperature erythrocytolysis is a consequence of red blood cells entering a specific environment (during laboratory testing they are in a hypotonic solution);
- mechanical hemolysis - observed in persons with an artificial heart valve, occurs due to artificial circulation;
- natural hemolysis.
Types of red blood cell hemolysis
Hemolysis is distinguished in vitro - red blood cells are destroyed outside the human body, and when biological material is collected for subsequent laboratory research. As a result, the analysis will give a false result or fail at all. In such situations, the reasons are:
- incorrect blood collection technique;
- contaminated test tube;
- improper storage of seized liquid;
- repeated freezing or thawing of blood;
- shake the test tube vigorously.
Against this background, it is necessary to repeat the analysis, which is undesirable, especially for children.
Postrenal
Hematuria is observed as a consequence of diseases of the bladder, urethra and ureter.
- Cystitis. Developing inflammation of the bladder walls.
- Urolithiasis, when the stone is located in the lower organs of the urinary system.
- The process of proliferation of tumor tissue in the lower organs of the urinary system.
- Injury to the bladder or urethral canal (error during surgery, incorrect placement of the catheter).
In particular, male pathologies of the prostate gland (prostatitis, prostate adenoma) cause the appearance of an inflated number of red blood cells in urine tests. Female cervical erosion and uterine bleeding also provoke the observation of an increased number of red blood cells in laboratory urine tests.
Often the reason for seeing an increased number of red blood cells in the urine lies in normal physiological conditions:
- Severe overheating of the body.
- Depression and stress.
- Increased physical activity.
- Excessive consumption of alcoholic beverages.
- Excessive consumption of certain types of seasonings.
These reasons lead to disruption of the barriers of the vessels and arteries of the kidney, and as a result, a large number of red blood cells are observed in the urine.
Rarely occurs, but there is progression of hemolysis - the process of destruction and death of red blood cells. This phenomenon gives rise to an increase in the volume of free hemoglobin, which tends to clog the renal glomeruli, and as a result lead to renal failure.
Pregnant women may experience some urine discoloration a little red due to hormonal changes. Although such observation is not dangerous at first glance, it is necessary to urgently seek help from specialists to make the correct diagnosis.
In addition, in addition to the reasons typical for adults, a large number of red blood cells in urine tests is observed in adolescents for the following reasons:
- Congenital problems with blood vessels and arteries.
- Complications after diathesis.
- Complications after infections and inflammations.
- Intolerance to certain medications.
Please note that eating certain foods can turn urea into different colors. Therefore, you should not run to the doctor after you have eaten beets. I provoke the release of altered red blood cells in a general urine test, such foods as buckwheat, nuts and some vegetables containing a large amount of alkali.
Symptoms
Hemolysis of erythrocytes has a number of its own clinical manifestations, but they may go unnoticed by the patient - such symptoms are nonspecific and are characteristic of a large number of diseases. They may be hiding behind the clinic of the underlying disorder, which comes to the fore.
Symptoms:
- pallor or yellowness of the skin;
- temperature increase to 38–39 degrees;
- pain localized in the upper abdomen;
- heart rhythm disturbance;
- dizziness;
- muscle and joint pain;
- general weakness and malaise;
- dyspnea;
- hematosplenomegaly;
- nausea and vomiting;
- change in urine color;
- spread of pain to the lumbar region;
- decreased blood tone values;
- painful redness of the facial skin;
- increased anxiety;
- problems with emptying the bladder and bowels;
- severe headaches.
As for infants, they show signs of hemolytic disease of the newborn.
Manifestation of hemolysis
Chronic hemolysis, which accompanies diseases such as leukemia and sickle cell anemia, occurs without severe symptoms, like many other physiological processes.
Causes of acute hemolysis requiring emergency care:
- Transfusion of blood incompatible with the group and Rh factor;
- Autoimmune hemolytic anemia, or anemia caused by poisoning;
- Hemolytic disease of the newborn, where every breath the newborn takes makes the situation worse.
If the patient is conscious, he experiences the following symptoms:
- Feeling hot;
- Severe chest compression;
- Pain in the lower back, possibly in the chest and abdomen.
Other symptoms:
- A sharp decrease in blood pressure;
- Hyperemia of the facial skin, turning into cyanosis;
- Spontaneous urination and defecation;
- According to laboratory studies, intravascular hemolysis occurs in the circulatory system.
With radiation and hormonal therapy, during anesthesia, signs can be erased. After a few hours, the acute symptoms subside, leaving lower back pain.
After a short time, a relapse occurs with the following manifestations:
- Hyperthermia;
- Jaundice of the skin and sclera of the eyes;
- Severe headache;
- Renal dysfunction: protein and hemoglobin in the urine, cessation of urination, then anuria, uremia, death.
Coagulogram indicators:
- Anemia caused by the release of hemoglobin into the plasma after the destruction of red blood cells;
- Thrombocytopenia;
- High bilirubin levels;
- Violation of blood clotting processes.
The urine becomes red or black, and protein, potassium, and hemoglobin are found in it.
Diagnostics
The main diagnostic test indicating that red blood cells are being destroyed is a general clinical blood test. Biological material is taken from a finger, less often venous blood is required.
Laboratory manifestations of such a deviation are:
- increase in stercobilin;
- increase in urobilin;
- an upward change in the concentration of unconjugated bilirubin;
- hemoglobinemia;
- hemosiderinuria.
Diagnosis of red blood cell hemolysis
However, such results are not enough to identify the provoking factor; a comprehensive examination of the body is required, which begins with measures performed by the attending physician:
- studying the medical history - to detect the pathological source;
- familiarization with family history;
- collection and analysis of the patient’s life history - information about taking any medications, possible insect bites or consumption of poisonous mushrooms is taken into account;
- measurement of blood pressure and temperature values;
- assessment of the appearance of the skin;
- palpation of the anterior wall of the abdominal cavity - to detect an increase in the volume of the liver or spleen;
- a detailed interview with the patient is necessary to create a complete symptomatic picture.
An additional diagnostic scheme - instrumental procedures, laboratory tests and consultations with other specialists - is selected individually.
RDW (red cell distribution width) – anisocytosis of erythrocytes
Features of the definition
Manually calculating this metric through the Price-Jones curve by hand is extremely tedious. It is more convenient to determine it on a hematology analyzer as the coefficient of variation of the average volume of red blood cells.
Assessing the degree of anisocytosis under a microscope is accompanied by a number of errors. When red blood cells in a smear dry, their diameter decreases by 10-20%; in thick strokes it is less than in thin strokes. Only automated counting on a hematology analyzer using the conductometric method allows you to completely get rid of artifacts: this preserves cell stability and reproducibility of results.
Additional features
Mindray hematology analyzers have another calculated RDW indicator - RDW-SD. It is independent of MCV and is a direct measurement of the width of the red blood cell histogram at the 20% peak of the curve. In this case, the peak height of the RBC histogram is taken as 100%. Standard RDW-SD – 42 +/- 5 fl. Clinically significant RDW-SD value > 60 fl. Both RDW measures measure the variability of red blood cell volume.
An increase in RDW suggests the presence of a mixed population of cells (normocytes and microcytes or macrocytes and normocytes). RDW-SD is more sensitive in the presence of a minor population of macrocytes or microcytes, as it measures the lower part of the red blood cell volume distribution curve. At the same time, this indicator will change with high reticulocytosis due to their large volume, which expands the base of the red blood cell distribution curve.
RDW-CV is less sensitive to the presence of a small population of microcytes or macrocytes or reticulocytes, but better reflects the overall changes in red blood cell size in macrocytic or microcytic anemia.
Treatment
The principles of treatment of erythrocyte hemolysis will be common to all etiological factors. First of all, it is necessary to completely stop the entry of the poisonous source into the human body. You can speed up its elimination by:
- forced diuresis;
- cleansing enemas;
- gastric lavage;
- hemodialysis;
- hemosorption.
Therapy will be aimed at:
- blood or red blood cell transfusion;
- phototherapy;
- taking glucocorticoids and medications that relieve symptoms, such as antipyretics or painkillers;
- blood transfusion therapy;
- use of sodium bicarbonate.
If conservative methods are ineffective, surgical removal of the spleen is resorted to.
External reasons
Due to their anatomical structure, red blood cells can enter the urine from the genital tract. Their sources in women include uterine bleeding, erosions and tumors of the cervix, sexually transmitted diseases, and injuries. Red blood cells can be found in the urine of men with prostatitis and prostate cancer.
Diseases of the rectum, accompanied by rectal bleeding, can become a source of red blood cells in the urine. These are bleeding hemorrhoids, ulcers, polyps or rectal cancer, ulcerative colitis, anal fissures.
Prevention and prognosis
You can prevent the occurrence of such a problem as pathological or acquired hemolysis of red blood cells by observing the following preventive rules:
- complete renunciation of addictions;
- taking only medications as prescribed by your doctor;
- consumption of quality foods;
- use of personal protective equipment when working with chemicals and poisons;
- timely treatment of diseases that can lead to problems;
- regularly undergoing a full preventive examination at a medical institution - in addition to instrumental procedures, this includes donating blood for laboratory tests.
The prognosis depends on the underlying cause, since each etiological factor with a pathological basis has a number of its own complications, often leading to death.
Table of acceptable values
The excretion of red blood cells in the urine does not depend on gender and age. Acceptable indicators for the presence of cells in sediment are universal for all population groups except children:
| Categories | Content of erythrocytes in sediment |
| Men | 0-2 |
| Women | 0-2 |
| Children | 0-4 |
Functions of red blood cells
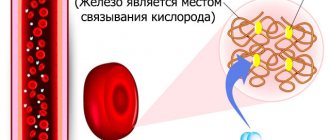
Red blood cells fulfill their main purpose in the body - they are carriers of respiratory gases - oxygen and carbon dioxide.
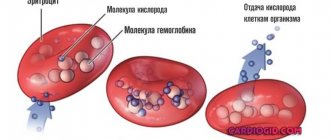
This process is carried out in a certain order:
- Nucleated discs, as part of the blood moving through the vessels, enter the lungs.
- In the lungs, the hemoglobin of red blood cells, in particular its iron atoms, absorbs oxygen, turning into oxyhemoglobin.
- Oxygenated blood, under the influence of the heart and arteries, penetrates through capillaries into all organs.
- Oxygen carried by iron is detached from oxyhemoglobin and enters cells experiencing oxygen starvation.
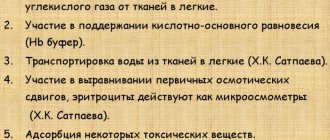
- Empty hemoglobin (deoxyhemoglobin) is filled with carbon dioxide and converted into carbohemoglobin.
- Hemoglobin combined with carbon dioxide carries CO2 to the lungs. In the vessels of the lungs, carbon dioxide is broken off and then removed to the outside.
In addition to gas exchange, formed elements also perform other functions:
- Absorb and transport antibodies, amino acids, enzymes,
- Human red blood cells
- Transport harmful substances (toxins), some medicines,
- A number of erythrocyte factors take part in stimulating and preventing blood clotting (hemocoagulation),
- They are primarily responsible for blood viscosity - it increases when the number of red blood cells increases and decreases when it decreases,
- Participate in maintaining the acid-base balance through the hemoglobin buffer system.
When is a red blood cell test prescribed?
Erythrocytes are blood cells that carry a red pigment - hemoglobin. According to its chemical properties, it is a protein that plays a key role in the processes of iron metabolism and oxygen transfer from the lungs to the tissues. Every second, the red bone marrow of a healthy person produces 2.4 million red blood cells, which have a lifespan of 100–120 days.
The red blood cell count is indicated on the blood test form as RBC. A separate test for red blood cells is not done; it is included in a general blood test, which is prescribed in the following cases:
- Preventive and clinical observation, including for pregnant women.
- Basic examination during hospitalization.
- Diagnosis of anemia.
- Diagnosis of diseases of the hematopoietic system.
- Monitoring ongoing treatment.
If, to clarify the diagnosis, a wider range of indicators is required than in a standard general (clinical) analysis, a blood test with the note “with ESR” is prescribed; it is more expensive and detailed. You can also do an ESR (erythrocyte sedimentation rate) test separately.
What is the blood collection procedure?
No special preparation is required to donate blood for analysis. It is recommended to take blood no earlier than 4 hours after the last meal. If possible, the day before you should avoid high emotional and physical stress, and drinking alcoholic beverages. It is best to rest for 10–15 minutes before entering the treatment room. Blood is taken from the fingertip of the left hand using a disposable scarifier or a syringe from a vein. A higher quality biomaterial for analysis is venous blood, so this method is more often used for adults. Within 24 hours you can get the results in your hands.
The role and properties of red blood cells
An erythrocyte (translated from Greek as red cell) is a component of blood that does not have a nucleus and contains hemoglobin. Red blood cells are shaped like a biconcave disc. They do not have a core, so they are very elastic and pass into capillaries, which are much smaller than themselves.
These cells begin their lives in the red bone marrow and end in the liver and spleen. They live for about 120 days. At the stage of development of red blood cells, they have a nucleus; as they mature, it is converted into hemoglobin, which makes up 90% of the dry matter of red blood cells.
- respiratory;
- enzymatic;
- protective;
- buffer;
- nutritious.
Hemoglobin is the main element of red blood cells, it also has its own set of functions:
- Respiratory - it is hemoglobin that carries oxygen from the lungs to the organs and back carbon dioxide.
- Regulates blood reaction.
According to its chemical structure, hemoglobin is a protein that has a complex composition and includes the globin protein and the heme prosthetic group. It contains iron, which is responsible for the attachment and detachment of oxygen molecules.
The normal level of hemoglobin in human blood is considered to be 166.7 g/l.
For men, this norm is higher than for women, since male sex hormones have a stimulating effect on red blood cells and hemoglobin, while women’s hormones, on the contrary, inhibit this process.
With a decrease in hemoglobin in the blood, anemia develops. This is very dangerous for the human body. Therefore, it is important to monitor the number of red blood cells and hemoglobin (undergo examinations, take tests).