Hemoglobin value
Hemoglobin is a complex globulin protein. Its molecule consists of two parts: globin
– protein (96% of the entire molecule) and
heme
– the non-protein part containing iron Fe(II). Heme iron combined with oxygen is red in color.
Hemoglobin, a “breathing” protein, is found in red blood cells. It transports oxygen O2 from the lungs to the tissues, where it exchanges it for carbon dioxide CO2, “takes” CO2 to the lungs, again exchanges it for O2 and again transports it to the tissues.
If there is little hemoglobin in red blood cells or it is unable to attach O2 to itself, then hypoxia (lack of oxygen) occurs in every cell of the body.
A decrease in hemoglobin levels in a blood test means anemia.
| Degree of anemia | HGB (Hb), g/L |
| 1 (easy) | 115 — 90 |
| 2 (moderate) | 89 — 70 |
| 3 (heavy) | ≤69 |
General blood test extended with leukocyte formula and reticulocytes (venous blood only)
Blood should be donated in the morning on an empty stomach (or in the afternoon/evening hours, 4-5 hours after the last meal). 1-2 days before the test, exclude high-fat foods from your diet.
General blood analysis
– a laboratory study aimed at determining the number of different blood cells, their parameters (size, etc.) and indicators reflecting their ratio and functioning.
The main indicators that are included in the table of results of a general blood test:
Hemoglobin (Hb, Hemoglobin)
Hemoglobin is a respiratory pigment in the blood, which is found in red blood cells and is involved in the transport of oxygen and carbon dioxide. The hemoglobin content in the blood of men is slightly higher than that of women. In children of the first year of life, a physiological decrease in hemoglobin concentration may be observed. A pathological decrease in blood hemoglobin (anemia) may be a consequence of increased losses during various types of bleeding, the result of accelerated destruction of red blood cells, and impaired formation of red blood cells. Anemia can be either an independent disease or a symptom of a chronic disease.
Hematocrit (Ht, Hematocrit)
Hematocrit is the percentage of all formed elements (quantitatively, mainly red blood cells) of the total blood volume.
Red blood cells (RBC, Red Blood Cells)
Erythrocytes (red blood cells) are highly specialized anucleate blood cells filled with a respiratory pigment - the iron-containing protein hemoglobin. The main function of red blood cells is oxygen transport. They are formed in the red bone marrow. The formation of red blood cells is stimulated by erythropoietin, synthesized in the kidneys (in increased quantities during hypoxia). For normal hemoglobin synthesis and the formation of red blood cells, vitamin B12 and folic acid are necessary, and there must be a sufficient supply of iron. Normally, the lifespan of an erythrocyte in the bloodstream is 120 days. Red blood cells are destroyed in the spleen and reticuloendothelial system. Determination of the number of red blood cells, in combination with the study of hemoglobin content, assessment of hematocrit and characteristics of red blood cells (erythrocyte indices) is used in the differential diagnosis of anemia.
MCV (Mean Cell volume, average volume of red blood cells)
A calculated indicator reflecting the average volume of red blood cells, which is used in the diagnosis of anemia (microcytic, macrocytic, normocytic). With pronounced anisocytosis (the presence of cells with different volumes), as well as the presence of a large number of red blood cells with an altered shape, this indicator is of limited value.
RDW (Red cell Distribution Width, distribution of red blood cells by size)
A calculated indicator reflecting the degree of anisocytosis (heterogeneity of red blood cells by volume). Used for differential diagnosis and monitoring of treatment of anemia of various origins.
MCH (Mean Cell Hemoglobin, average hemoglobin content in red blood cells)
A calculated indicator reflecting the average hemoglobin content in 1 cell (erythrocyte). Used, like MCV, for the differential diagnosis of anemia.
MCHC (Mean Cell Hemoglobin Concentration, mean hemoglobin concentration in red blood cells)
Concentration index is a calculated indicator reflecting the average concentration of hemoglobin in red blood cells. A sensitive indicator of changes in hemoglobin formation - in particular, in iron deficiency anemia, thalassemia, and some hemoglobinopathies.
Platelets (PLT, Platelets)
Platelets are anucleate cells that, in their granules and on the surface, contain many active substances and some coagulation factors that enter the blood when platelets are activated. Platelets are capable of aggregation (connecting with each other) and adhesion (sticking to a damaged vascular wall), which allows them to form a temporary clot and stop bleeding in small vessels. Formed in red bone marrow. The lifespan of a platelet in the bloodstream is 7–10 days. A decrease in platelet count can occur either due to increased platelet consumption or due to insufficient production. Clinical manifestations (increased bleeding, up to life-threatening conditions) occur when the platelet concentration is less than 50*103 cells/μl.
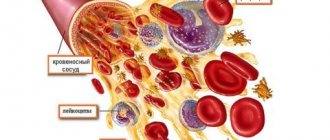
Leukocytes (WBC, White Blood Cells)
Leukocytes (white blood cells) are nucleated blood cells involved in the recognition and neutralization of foreign elements, the elimination of altered and decaying cells of one’s own body, and various immune and inflammatory reactions. This is the basis of the body's antimicrobial defense. They are formed in the red bone marrow and organs of the lymphatic system. Blood consists of cells (formed elements) and a liquid part - plasma. These cells—red blood cells, white blood cells, and platelets—are formed and mature in the bone marrow and must be released into the systemic circulation as needed.
Different types of leukocytes have slightly different functions, however, they are capable of coordinated interactions by “communicating” using certain substances - cytokines. If the analyzer detects atypical forms of cells, or significant deviations from reference values are detected, then the leukocyte formula is supplemented by a microscopic examination of a blood smear, which makes it possible to diagnose certain diseases, such as, for example, infectious mononucleosis, determine the severity of the infectious process, describe the type of atypical cells identified during leukemia.
Neutrophils
- the most numerous of the leukocytes - the first to begin to fight infection and the first to appear at the site of tissue damage. Neutrophils have a nucleus divided into several segments, which is why they are also called segmented neutrophils or polymorphonuclear leukocytes. These names, however, refer only to mature neutrophils. Maturing forms (young, rod-nucleated) contain a solid core.
At the site of infection, neutrophils surround bacteria and eliminate them by phagocytosis.
Lymphocytes
- one of the most important parts of the immune system, they are of great importance in destroying viruses and fighting chronic infection. There are two types of lymphocytes - T and B (the leukocyte formula does not count the types of lymphocytes separately). B-lymphocytes produce antibodies - special proteins that bind to foreign proteins (antigens) found on the surface of viruses, bacteria, fungi, and protozoa. Surrounded by antibodies, cells containing antigens are accessible to neutrophils and monocytes, which kill them. T lymphocytes are able to destroy infected cells and prevent the spread of infection. They also recognize and destroy cancer cells.
There are not very many monocytes in the body, however, they perform an extremely important function. After a short circulation in the bloodstream (20-40 hours), they move into tissues, where they turn into macrophages. Macrophages are capable of destroying cells, just like neutrophils, and keeping foreign proteins on their surface, to which lymphocytes react. They play a role in maintaining inflammation in some chronic inflammatory diseases such as rheumatoid arthritis.
Eosinophils
the blood contains a small amount, they are also capable of phagocytosis, however, they mainly play a different role - they fight parasites, and also take an active part in allergic reactions.
There are also few basophils in the blood. They travel to tissues where they become mast cells. When they are activated, they release histamine, which causes allergy symptoms (itching, burning, redness).
Reticulocytes
– young red blood cells (erythrocytes). They are formed in the bone marrow when stem cells differentiate and divide to become adult red blood cells through the reticulocyte stage, gradually losing their nucleus and decreasing in size.
Newborns have more reticulocytes than adults.
Most red blood cells are already fully mature when they leave the bone marrow and enter the bloodstream, but 0.5-2% of those circulating in the blood are reticulocytes, which turn into adult red blood cells within two days. This test shows the number and percentage of reticulocytes in the blood and reveals the adequacy of red blood cell production by the bone marrow and the degree of its activity.
Reasons for decreased hemoglobin
- Blood loss.
Acute bleeding due to injury, surgery or chronic internal, uterine bleeding.
- Bone marrow dysfunction.
Insufficiency of erythropoiesis, cancer.
- Iron deficiency in the body.
- Metabolic disorders due to lack of vitamins, microelements, enzymes, etc.
- Hemolysis of red blood cells.
Rapid destruction of red blood cells due to their inferiority or damage by immune complexes.
- Hemoglobinopathies.
Congenital disorders of hemoglobin synthesis.
Decoding indicators
The leukocyte level in the blood depends on diet, time of day, and age. In some cases, deviations are due to gender and are considered the norm.
Normal in the body
The normal level of leukocytes in the blood of adults and children is different - there are more leukocytes in the child's body. The designation of leukocytes is normal, table for adults:
| Leukocyte type | Norm |
| Neutrophils | from 47 to 72% |
| Lymphocytes | from 19 to 37% |
| Monocytes | from 3 to 11% |
| Eosinophils | from 0.5 to 5% |
| Basophils | from 0 to 1% |
The leukocyte norm for an adult in absolute units is from 4*109/l to 9*109/l.
Important information: What do low platelets in the blood indicate during pregnancy (increasing foods)
Normal indicators for children:
- infants - from 10 to 25*109/l;
- during the first three years of life - from 9 to 15*109/l.
As you grow older, the indicators change and range from 6 to 11*109/l.
Increased values
Leukocytosis is an increased content of leukocyte cells in the blood. Leukocytosis can be:
- physical - occurs temporarily in most people and is not a pathology, since the increase in leukocytes is insignificant, develops against the background of exposure to various external factors (stress, heavy physical activity, changes in weather conditions, pregnancy, childbirth);
- pathological - an increase in the level of leukocytes by 2-3 times, a sign of the development of an inflammatory or infectious process.
Reduced values
Leukocytopenia is a reduced concentration of leukocytes in the blood, which is characteristic of weakened immune functions. With such a diagnosis, a person requires urgent therapy, otherwise the immune system will not be able to resist viruses, and even a cold can cause complications.
The reasons for the decrease in the concentration of leukocytes in the blood are:
- pathologies that greatly weaken and deplete the immune system;
- progressive infections that lead to the death of leukocytes in large numbers, while the body is not able to restore them;
- lack of vitamins and microelements.
Deciphering a blood test in terms of the components of the leukocyte formula is an effective method for assessing the state of the functions of the immune system and monitoring the changes that occur. Indicators of the quantitative content of leukocyte cells make it possible to diagnose diseases that are already present in the body, as well as to prevent diseases that may arise. If deviations from the norm are detected in the absence of any pathologies, then to restore the defenses, the doctor may recommend adjusting the diet and taking a complex of vitamins.
Basophils
The smallest form of leukocytes is basophils. They play an important role in situations where an allergen enters the body. If the basophil recognizes it, it will begin to destroy it, releasing biologically active substances into the blood that cause clinical symptoms (allergic reactions).
Basophilia is the process of increasing these white blood cells. This is a typical reaction of the body in an allergic condition or a symptom of a disease such as chicken pox. Also, an increased level of these leukocytes is a characteristic feature of the onset of the menstrual cycle or ovulation in women.
The absence of basophils from a medical point of view has no diagnostic value, and basopenia is not taken into account when making a clinical diagnosis and deciphering the leukocyte formula.
The norm of basophils for an adult is 0-1%.
What is MSN?
Sometimes in tests you may see a designation such as MCH, indicating the amount of hemoglobin in red blood cells. The unit of measurement for this indicator is indicated in picogram. For adults, the norm is 27-33 pg, for children under 16 years old - 28-32 pg. This indicator indicates the ability of hemoglobin to saturate red blood cells with oxygen. This allows the doctor to obtain more informative data and clarify the diagnosis. An increase in this value indicates anemia, autoimmune processes in the body, and liver cirrhosis. And low levels are a sign of chronic diseases.
Neutrophils
Neutrophils (NEUT) are cells that are the first to take part in the fight against pathogenic organisms. They engulf a cell that the immune system perceives as potentially dangerous, thereby destroying it.
There are two types of neutrophils: band and segmented. The norm for the former for an adult is up to 4 percent, for the latter – from 40 to 60.
An increase in the level of neutrophils occurs in the case of a previous infectious disease, during the acute stage of development of an infection in the body, intoxication, or a tumor. Sometimes a temporary increase in neutrophils occurs after vaccination.
A decrease in the number of neutrophils is observed either when most of the cells have already died in the fight against cells dangerous to human health, that is, when a person has a severe viral or bacterial disease. The second reason is the initial failure of cells, which occurs with blood diseases or pathologies of the bone marrow, which produces blood cells.
It is important to know that neutrophil levels are assessed in the overall picture of the patient’s health. There are often cases when a slightly reduced level of neutrophils (neutropenia) is normal for the body.
Preparation for blood sampling for eosinophils
Compared to other types of diagnostic measures, preparing for an eosinophil blood test does not require special preparation. It is not recommended to eat for at least 1-2 hours before blood collection. A few days before the analysis, sweets, spicy, fried, salty foods, smoked foods, and alcoholic drinks, even with a low percentage of alcohol, should be excluded from the diet.
If food intake restrictions were not observed the day before, it is better to postpone the trip to the laboratory. It is not advisable to take blood if the person is under stress or if women are on their period. In these cases, significant changes occur in the composition of the blood, so the results will be distorted.
Some patients are treated with antibiotics or other medications. In this case, you need to wait 2 weeks after the last dose of the medicine and then plan a blood test. It is necessary to wait 1-2 days for the examination in the case of physiotherapy or radiotherapy. Following these simple recommendations will allow you to obtain reliable results.
Norm
For each group of people, certain standards are established that the hemoglobin level must meet. First of all, they depend on the age of the person. For example, the average
newborns are considered to be at 165 units.
Then the normal value begins to decrease. And after 12 years it reaches 140 units. The norms for men and women are different. For men, the acceptable limits are from 130 to 170, and for women, the normal value ranges from 120 to 150.
In the process of bearing a child, the upper limit of the permissible norm of hemoglobin
decreases. This is also typical for older people.
The child has
The maximum value of hemoglobin occurs in the first month of a child’s life. The average value is 165 units, but fluctuations of 30 units in one direction or another are also acceptable. From one month to six months, the limit of normal hemoglobin
the figure becomes 115 units.
Minor deviations are not pathology. From six months to a year, slightly increased numbers can be seen in the hemoglobin test results. However, the difference with the previous ones should not be significant.
In the period from two to six years, the level of hemoglobin becomes more or less constant.
The reference option is 125 units. From six to twelve years of age, hemoglobin levels can increase to 135 units. Until adulthood
Some fluctuations are possible. But after crossing the line of eighteen years, the indicators are equal to adults.
What are white cells and what are they responsible for?
The cellular composition of blood is represented by three types of cells:
- erythrocytes, occupying 99% of the composition;
- leukocytes;
- platelets - colorless blood platelets, nuclear-free elements of blood.
Briefly, the functions of these cells can be described as a clear distribution of responsibilities - red blood cells are responsible for transporting oxygen to tissues, platelets regulate blood clotting, leukocytes perform a protective function, that is, they provide immune control.
Leukocytes protect the body from pathogenic agents coming from outside or growing from within. Let's consider the ability of leukocytes to leak into the intercellular space during the process of suppuration of a splinter.
- Leukocytes flock to the site of insertion of a foreign body (splinter).
- The process of phagocytosis begins - part of the leukocytes, called phagocytes, absorbs and transforms particles of foreign material, increasing in size.
- An attempt to utilize a pathogenic agent by leukocytes is accompanied by an inflammatory process with redness, hyperthermia and swelling of the site of its penetration.
- An excessive increase in the size of phagocytes leads to their death, resulting in the formation of pus - a mass consisting of destroyed leukocytes.
- As a result, an even greater number of leukocytes are attracted to the site of injury to utilize both particles of external irritant and dead white cells, which is why the amount of pus - dead phagocytes - increases.
The activity of leukocytes in this case will be stopped only if the splinter is removed. In other cases, phagocytosis does not stop until the source of inflammation is completely eliminated.
Leukocytes are the main elements of the human immune system.