Inflammatory processes occurring in the nasal cavity are a very big problem for children. It happens that parents carry out incorrect treatment of chronic rhinitis, since there are many varieties of this disease and each requires the use of a specific therapy technique.
It is very important to carry out diagnostics to make a diagnosis. For this purpose, a rhinocytogram is performed. Deciphering a nasal swab will allow you to determine the presence of the disease and identify the features of its course.
What is a rhinocytogram?
A rhinocytogram is a comprehensive analysis of the microflora of the nasal sinuses. To do this, a nasal swab is taken to obtain nasal secretions. This research method involves assessing the number of cells such as:
- lymphocytes;
- red blood cells;
- neutrophils;
- ciliated epithelium;
- macrophages;
- yeast mushrooms;
- eosinophils.
By conducting research, it is possible to determine which bacteria provoked the occurrence of a runny nose in order to carry out the most successful fight against it.
Main functions
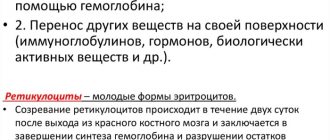
Blood leukocytes are primarily defenders of the body, and their subtype, neutrocytes, is mainly engaged in phagocytosis, in simple terms, the destruction of enemies - viruses, bacteria and parasitic microorganisms. This is the main function of neutrophils.
Blood neutrophils in the body are formed in the bone marrow, live in the blood for several hours and up to several days in tissues. Such a short lifespan of these cells suggests that the process of their renewal must occur continuously. And if the body is fighting an infection, the lifespan of neutrophils is shortened, since, having completed their task, they self-destruct. It is clear that only full-fledged mature cells effectively fight sources of infection. Such neutrophils are called segmented, and normally there are the most of them in a smear for a blood test - up to 70%.
Band neutrophils are young cells, there are fewer of them than mature ones - from 1% to 6%. There should be no embryonic forms of neutrophils in the blood - myelocytes and metamyelocytes (they are also called young cells), since they do not leave the hematopoietic organs until they have completed all stages of development.
The balance is disrupted if an acute infectious process occurs in the body, and all protective resources are mobilized to fight it - mature cells quickly die, they urgently need to be replaced with new ones, even if they are not quite ready yet.
You can see the percentage of neutrophil forms in the blood in a detailed blood test with a leukocyte formula. For deviations from the norm, speaking about the leukocyte formula, the concepts of “shift to the left” and “shift to the right” are accepted. What does this mean?
If you distribute all stages of neutrophil development from left to right, it will look like this:
myelocyte – metamyelocyte (young) – band – segmented
When the number of young neutrophils in the blood goes beyond normal limits, the formula shifts to the left. And if the number of segmented mature forms goes beyond the norm, this is a shift of the formula to the right.
Indications for the procedure
A rhinocytogram is an analysis of a smear taken from the nasal mucosa. The procedure is prescribed for adults and children. Often, such an analysis is prescribed for people who have a long-term persistent runny nose or frequent relapses of respiratory tract infections.
High-risk groups include:
- children;
- people with weakened immune systems;
- have undergone organ transplantation;
- people with diabetes.
This study is mandatory if the patient has one or several complaints, namely:
- nasal congestion lasting more than a week;
- nasal discharge that cannot be treated;
- sneezing;
- itching of the nasal mucosa.
This is a fairly simple analysis that does not cause any discomfort to the child.
Preparing for secretion collection
Many patients wonder how to do a rhinocytogram and how to prepare for the study. To obtain accurate results, you must follow certain rules. Two days before the test, you need to stop using various ointments inside and outside the nose. It is prohibited to use drops and sprays containing antibacterial components and corticosteroids.
5 days before sampling, you must stop taking antibiotics. There is no need to rinse your sinuses the day before taking a smear, and on this day it is advisable not to brush your teeth and drink only water.
Features of the procedure
A rhinocytogram in a child and an adult is performed at any time, but it is best to do this in the initial stages of the disease. The analysis is carried out in a fairly simple way. The procedure is completely painless, and even children do not need to be afraid of it.
To collect material, the patient tilts his head back slightly, and the doctor or nurse uses a cotton swab to take the required amount of material for the study. The exact same procedure must be done with the other nostril. The resulting samples are then placed in a special container with a special nutrient medium required for the growth of microorganisms.
Often, the doctor may use an endoscope to obtain a more accurate result. This study is performed under local anesthesia. This type of sampling of material for analysis causes some discomfort, since it is carried out from the paranasal sinuses. The resulting material is considered more informative, since it can be used to determine the presence of neutrophils in the smear.
How is biological material collected from the nose?
If someone is afraid of diagnostic procedures, then they can be comforted by the fact that a rhinocytogram is an absolutely painless and very quick manipulation. Even small children tolerate the collection of mucus from the nasopharynx well, although it causes minor discomfort.
To make it less scary and clear how the procedure occurs, we will tell you the step-by-step process of carrying it out by a laboratory assistant:
- The specialist takes a thin and long tube with a cotton wool tip.
- Introduces it carefully to the posterior part of the inferior nasal concha and scrapes off the mucus with a slight movement.
- He takes out the tube and packs it in a special container or a separate sterile tube, in which it is transferred to the research room.
In the laboratory, the resulting sample of biomaterial is stained to count the number of eosinophils and other formed elements. Eosinophilic bodies acquire a pink tint, separating them from other cells and microorganisms.
Taking a smear is not a procedure for which it is necessary to carefully prepare the nasopharynx or the body. Unlike donating blood, where it is important to adhere to a diet, avoid bad habits, physical influences and stressful situations that distort indicators, a rhinocytogram does not require compliance with such rules. But still, recommendations, albeit limited, are given to patients.
- Before manipulation, it is better not to intensively blow out the mucous secretions, so that the real amount of formed elements remains in the analysis.
- Do not instill intranasal drops into the nasal cavity (applies to any means - antibiotics, vasoconstrictors, etc.).
These are all the rules that you need to remember before visiting the diagnostic center. For more reliable results of mucus sampling, it is recommended to repeat the manipulation after a few days.
Many patients are interested in where they can get a nasal swab and what the cost of such a diagnosis is. There are laboratories in various clinics and clinical centers. Almost every medical institution that performs a blood test also collects mucus from the nasopharynx and analyzes the indicators. The biomaterial can be submitted to Invitro or any other laboratory.
But as for the cost, it also depends on the medical institution. If this is a paid diagnostic center, then the price will be acceptable, but not high. And in public clinics this procedure is either completely free or very cheap. Of course, the more seriously the laboratory takes its work, the more reliable the result of the smear analysis will be.
What do cells mean in the analysis?
A qualified doctor must describe the result obtained, since he knows how to decipher the analysis (rhinocytogram). The nasal mucosa consists of several cells, each of which performs a specific function. If bacteria or viruses enter the mucous membrane, the level of leukocytes increases to combat them. These cells are involved in the formation of immunity.
An increase in leukocytes indicates the presence of infection in the body, and an excess of one of the leukocyte fractions indicates the cause of the disease. When allergens come into contact with the surface of the nasal mucosa, an allergic reaction occurs. It is caused by the formation of eosinophils on the surface of the mucosa. In addition, during the study, epithelium and bacteria can be detected.
Sputum analysis
A therapist, phthisiatrician or pulmonologist may prescribe a cytological analysis of sputum.
Why get tested?
This test is necessary to make sure that the patient does not have abnormal cells in the sputum that could indicate that he has cancer. Such a cell changes its structure, and this can be seen under a microscope. If a person has cancer, then in 85% of cases these degenerated cells will be excreted in the sputum. We are talking about lung cancer. A sputum test is prescribed if the doctor suspects that the patient has this disease. But this examination is carried out not once, but several times (preferably 5 times), then the result will be the most reliable.
Normal for children and adults
When conducting research, it is imperative to know what the normal rhinocytogram is in children. The interpretation in the table allows you to determine the normal indicators of the components of discharge from the nasal sinuses for adults and children.
| Components | Norm in percent |
| Eosinophils | 0-5 |
| Neutrophils (rods) | 1-6 |
| Neutrophils (segment.) | 47-72 |
| Macrophages | 3-11 |
| Leukocytes | 65-75 |
The content of these cells is not constant; it can fluctuate throughout the day. In the morning or evening, this figure can decrease by about 20%, and at night it can increase by 30%.
When deciphering a rhinocytogram, the norm for eosinophils in children under 4 years of age should be 0-7, and in children over 4 years of age, the indicators for adults are taken into account. The rest of the test indicators depend on the age of the child, so the doctor must interpret the results.
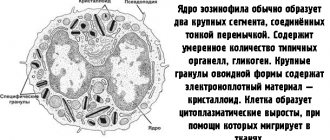
What are eosinophils
Eosinophils are a type of immune cells that are found in the blood and are part of the leukocyte formula. They are formed in the bone marrow, the whole process takes up to 8 days, then they move into the circulatory system, and from there to all organs. Life expectancy is 1–2 weeks. They perform various functions in the human body:
- destruction of foreign cells and helminths;
- bactericidal activity;
- protection from potentially dangerous microorganisms;
- slowing down the growth of tumors;
- regulate allergic reactions.
With the development of the inflammatory process, cells degenerate into phagocytes and destroy foreign particles. The eosinophil count depends on the amount of cortisol produced in plasma per day.
Decoding indicators
To determine the main cause of a prolonged, persistent runny nose, the quantitative ratio between the cells is calculated during the follow-up. When analyzing a rhinocytogram (deciphering), normally in children there should be up to several units of leukocytes in the field of view. During the course of the infectious process and inflammation, their number increases sharply.
Normally, neutrophils should be 1-3%. In the presence of a bacterial type of runny nose, frontal sinusitis or sinusitis, their number increases sharply, in proportion to the intensity and complexity of the inflammatory process. This manifests itself in the appearance of thick yellow or green nasal discharge. Initially, a viral infection can be complicated by a bacterial one, which is why the number of neutrophils can increase simultaneously with lymphocytes.
Deciphering the (normal) rhinocytogram in children suggests that lymphocytes should not exceed 5%. A sharp increase in the level of lymphocytes may indicate the presence of influenza, parainfluenza, adenovirus or any other viral infection. In addition, their number may increase with chronic runny nose.
The presence of more than 10% eosinophils in the tests indicates the presence of hay fever, or allergic rhinitis, in the body. The amount of epithelium is not always taken into account when conducting research, but a significant amount of it indicates an inflammatory process occurring in the body.
When deciphering a rhinocytogram, children should not normally have red blood cells. If they are present, we can talk about the flu, since red blood cells in this case penetrate through thinned blood vessels into the nasal cavity.
The microflora is normally negative, but if it is present, then the type of infectious agent is determined. Pathogenic microorganisms can occur with bacterial rhinitis or viral rhinitis.
Microscopic examination of a smear from the nasal mucosa
A rhinocytogram is a study of mucus from the nasal cavity under a microscope. It allows you to determine the presence in the nasal mucus of cells characteristic of allergic or infectious diseases that cause rhinitis - inflammation of the nasal mucosa. With a long runny nose, in some cases, determining the cause that caused it can be difficult. For this purpose, a rhinocytogram is performed, which reveals an increased number of eosinophils, which serves as an additional argument in favor of the allergic nature of the runny nose. Allergic and infectious rhinitis are treated differently, which is why it is important to determine the cause of the runny nose. Reference values are not given. The result is a description of the general cytological picture with a count of the number of leukocytes, eosinophils, neutrophils, ciliated epithelium, lymphocytes, macrophages, mucus, erythrocytes, yeast fungi, flora. The doctor interprets the result (differential diagnosis of rhinitis) by assessing the ratio of the number of cells.
Synonyms Russian
Rhinocytogram, cytological examination of secretions from the nasal cavity, smear for eosinophilia, examination of scrapings from the nasal mucosa, examination of nasal secretions.
English synonyms
Cytologic study of respiratory tract, Nasal Smear, Nasal smear for eosinophils, Eosinophil smear.
Research method
Microscopy.
What biomaterial can be used for research?
Nasal swab.
How to properly prepare for research?
Avoid the use of nasal sprays and drops containing corticosteroids for 24 hours before the test.
General information about the study
Rhinocytogram - examination of nasal discharge under a microscope. With its help, you can identify changes characteristic of allergic reactions of the body or infection. In this way, the cause of inflammation of the nasal mucosa (rhinitis) is determined.
Normally, all the walls of the nasal cavity are covered with a mucous membrane with a secretion that helps remove dust and germs. The secretion has this property due to the presence of ciliated epithelium, which has cilia that are able to vibrate and move mucus along with dust and microbes.
Nevertheless, normally the nasal cavity is inhabited by a large number of microbes (some types of staphylococci, streptococci, etc.) that do not cause harm to humans due to the body’s immune response. If for some reason local immunity decreases, microbes can lead to inflammation, and acute rhinitis occurs - a disorder of nasal function, accompanied by inflammatory changes in the mucous membrane and a runny nose. In addition, rhinitis can be caused by airborne viruses, including acute respiratory infections.
A decrease in local immunity can be caused by hypothermia of the body, a decrease in general human immunity. The development of a runny nose is also facilitated by slowing down the movement of the ciliated epithelium.
As a result of the immune system's response, the number of leukocytes - white blood cells - increases in the nasal mucosa. There are several varieties of them; in bacterial infections, neutrophils play the main role in protecting the body; in viral infections, lymphocytes play a major role. Macrophages may also appear.
In case of an allergy, the body is affected by a certain substance (allergen), such as pollen, wool, dust, etc., to which the immune system becomes hypersensitive. This reaction leads to the release of certain substances (histamine, bradykinin) in the nasal mucosa, causing allergy symptoms. Moreover, immune system cells such as eosinophils (one of the types of leukocytes) are of greater importance in this process. In case of allergies, they can appear in large quantities in the blood and also accumulate in the nasal mucus.
In addition, there is vasomotor (neurovegetative) rhinitis, in which exposure to cold, taking certain medications, and exposure to other physical or psycho-emotional factors causes acute swelling of the nasal mucosa and changes in the tone of the vessels of the nasal cavity.
In all cases of rhinitis, a large amount of fluid is formed and released, which is what we call a runny nose.
The allergic nature of rhinitis often remains undiagnosed, although it is quite common. A rhinocytogram can help in diagnosis: the peculiarity of eosinophils appearing in allergic rhinitis is that with a special stain (Romanovsky-Giemsa), they turn red and become available for counting under a microscope.
What is the research used for?
With a long runny nose, in some cases, determining the cause that caused it can be difficult. For this purpose, a rhinocytogram is performed, which reveals an increased number of eosinophils, which serves as an additional argument in favor of the allergic nature of the runny nose. Allergic and infectious rhinitis are treated differently, which is why it is important to determine the cause of the runny nose.
When is the study scheduled?
With prolonged runny nose (several weeks or more), accompanied by nasal congestion, sneezing of unknown origin.
What do the results mean?
Reference values for various types of microorganisms depend on their location (point of collection of biological material).
Increasing performance
- Eosinophils. A significant increase (more than 10% of the total number of leukocytes in a smear or more) in the number of eosinophils indicates an allergic origin of the runny nose. At the same time, it should be borne in mind that the absence of a large number of eosinophils in the smear does not reliably exclude the allergic nature of the disease. Eosinophil levels may also be elevated in non-allergic eosinophilic rhinitis, a disease in which there are no other signs (besides an increase in the number of eosinophils in the blood and nasal mucus) of an allergy. The disease is often accompanied by polyps and lack of response to antiallergic (antihistamine) drugs.
- Neutrophils. An increase in the number of these cells in a smear may indicate that the cause of a runny nose is infectious agents (bacteria or viruses). An increase in the level of neutrophils is especially characteristic of the acute stage of the disease.
- Lymphocytes. An increased content of lymphocytes may be associated with chronic infectious inflammation of the nasal mucosa.
- Red blood cells. The appearance of red blood cells in a smear may indicate increased permeability of the vascular wall of the nasal mucosa, which is typical for some types of rhinitis, in particular those caused by diphtheria or influenza.
It should be noted that increased levels of neutrophils and lymphocytes are not specific for infection.
Decrease in indicators
The absence of eosinophils, neutrophils, and other types of leukocytes in the smear may indicate:
- vasomotor rhinitis - runny nose not associated with allergies or infections;
- rhinitis associated with abuse of vasoconstrictor nasal sprays;
- rhinitis caused by other reasons (hormonal disorders, disorders of the psycho-emotional state, disorders of the anatomy of the nasal passages, etc.).
What can influence the result?
The use of nasal sprays, especially corticosteroids, may lead to false-negative results for eosinophilia.
The same effect is sometimes observed with the use of tablets containing corticosteroids and antihistamines (anti-allergy) drugs.
Important Notes
- The results of the study should be assessed by comparing data from the history of the development of the disease, other studies and symptoms.
- To increase the reliability of the results, it is recommended to repeat the examination after 1-2 weeks.
Also recommended
- Complete blood count (without leukocyte formula and ESR)
- Total immunoglobulin E (IgE) in serum
Who orders the study?
General practitioner, general practitioner, otorhinolaryngologist, allergist-immunologist.
Literature
- Palchun V. T. Otorhinolaryngology. National leadership, 2008, GEOTAR-media. 919 pp.
- V Paleri, J Hill. ENT Infections: An Atlas of Investigation and Management, 2010, Atlas Medical Publishing Ltd. P. 116.
- Dan L. Longo, Dennis L. Kasper, J. Larry Jameson, Anthony S. Fauci, Harrison's principles of internal medicine (18th ed.). New York: McGraw-Hill Medical Publishing Division, 2011.
If the results are normal, but the runny nose does not go away
If the rhinocytogram is normal in children, and a runny nose does not go away for a long time, then this may be a sign of:
- vasomotor runny nose;
- drug-induced rhinitis;
- another type of rhinitis.
Vasomotor rhinitis can occur as a result of vascular dysfunction.
It is observed mainly under stress and under the influence of cold air. Rhinitis medicamentosa can begin as a result of prolonged use of vasoconstrictor drugs. In addition, a runny nose can occur as a result of disruption of the endocrine or nervous systems. All these disorders require additional research and comprehensive treatment.
Reasons for the increase
The occurrence of neutrophilia is a special form of protection of the body from pathogenic bacteria and viruses, the spread of the inflammatory process. To accurately diagnose diseases, experts have identified three degrees of excess neutrophils in humans.
- An indicator of no more than 10 × 109/l indicates a moderate increase and the presence of an inflammatory process in the body.
- A level of 10-20×109/l indicates a pronounced excess and the presence of extensive inflammation in the body.
- Severe degree is considered at 20-60×109/l. This phenomenon requires urgent surgical intervention, as peritonitis or sepsis may develop.
The most common reasons for determining elevated neutrophils in the blood are physiological and pathological.
Many human diseases are accompanied by an increase in the level of neutrophils. A blood test will not reveal the exact cause, but it will make diagnosis much easier. Pathological causes include:
- Infections of various organs and systems (boils, erysipelas, rhinitis, bronchitis, dysentery, tonsillitis, salmonellosis, pyelonephritis, pneumonia, cystitis, meningitis, encephalitis). When diagnosing such diseases, be sure to take into account the patient’s complaints and accompanying symptoms, such as increased body temperature, rapid onset of symptoms, pain, and decreased immunity.
- Injuries (cuts, wounds, sprains, fractures, burns, consequences of surgical interventions).
- Vaccines. An increase in band neutrophils is possible after any vaccination. In children, a similar phenomenon occurs after DPT, BCG, polio, vaccination against rotavirus and chickenpox.
- Poisoning. The cause may be poisoning with salts of heavy metals, venoms of snakes and insects, as well as inhalation of toxic gases. With such intoxication, it is important to seek help in time, as liver and kidney failure and other serious complications may develop.
- Pathologies of internal organs (heart attack, urolithiasis, stroke, cholangitis, cholecystitis). When interviewing patients, chronic pathologies that led to this condition were identified; they felt unbearable and constant pain, and there was also a sharp deterioration in well-being. Typically, with such pathologies, neutrophils increase and low lymphocytes are determined.
- Oncological diseases of the blood (leukemia, myeloid leukemia, lymphogranulomatosis). Patients suffer from prolonged fever and bleeding gums, nosebleeds and stomach bleeding. In these pathologies, band neutrophils are increased.
Physiological causes are not associated with any disease.
An increase in granulocyte levels can be observed in the following cases:
- Food consumption. Along with it, microbes and bacteria enter the body, which it must neutralize. Therefore, after eating, an increase in segmented neutrophils or band neutrophils is observed.
- Smoking. Cigarettes contain a large number of substances, toxins and poisons that cause the development of inflammatory processes. To neutralize them, the number of neutrophils increases.
- Treatment with drugs. Many people take immunomodulators as prophylaxis and treatment, and are vaccinated. It is these components that affect the number of granulocytes.
- Alcohol. Ethanol damages internal organs and can cause inflammation.
- Intense physical exercise.
- Stress and emotional stress.