Lesions in the white matter of the brain are areas of damage to brain tissue, accompanied by a violation of the mental and neurological functions of higher nervous activity. Focal areas are caused by infection, atrophy, loss of blood supply and trauma. Most often, affected areas are caused by inflammatory diseases. However, areas of change may also be of a dystrophic nature. This is observed mainly as a person ages.
Focal changes in the white matter of the brain can be local, single-focal, or diffuse, that is, the entire white matter is moderately affected. The clinical picture is determined by the localization of organic changes and their degree. A single lesion in the white matter may not affect the dysfunction, but massive damage to neurons causes a disruption in the functioning of nerve centers.
Symptoms of cerebral gliosis
This disease is diagnosed accidentally; there are no clear symptoms in the presence of such changes. The following signs may indicate the presence:
- frequent headaches in the parietal region, accompanied by pressure surges, are mistakenly taken for a manifestation of migraine;
- even after rest you feel very tired;
- slight dizziness and general weakness in the body;
- difficulty coordinating movements;
- significant memory impairment;
- exacerbation of vascular diseases;
- in rare cases, when the affected lesions poorly affect the active areas, brain helios is asymptomatic.
Causes of spots on MRI of the brain
When receiving images after an MRI of the brain, the patient examines them, despite the fact that he does not have the special knowledge to decipher the examination results. But even he becomes clear that there are some pathologies if he sees dots or spots of white color that stand out sharply against the general background. Let's find out what could be the causes of white spots on MRI images of the brain.
Turning to traditional methods of therapy
No matter how many medications are prescribed to the patient, additional maintenance of the body through the use of folk remedies will help improve the general condition.
- At the initial stage, in the presence of a few lesions, herbs perfectly support the human body, which help stabilize the blood supply system and increase metabolism.
- If a patient develops obesity, a diet based on a raw food diet is recommended; fasting days with periodic fasting are also required. This will contribute to the overall cleansing of the body from various substances that interfere with its healthy functioning.
- Taking tinctures and various decoctions, the action of which is aimed at combating the symptoms of the disease. At the pharmacy you can buy ready-made preparations that are balanced for treatment.
It must be emphasized that treatment using traditional methods can only be effective as a complement to traditional therapy, which should be prescribed by specialists. A long-term effect from the use of medications and treatment using traditional methods will not be achieved until the cause of glial formation is eliminated. Next, we will find out what preventive measures will help people avoid developing this disease.
How long do adults with cerebral gliosis live? This is a common question. More on this later.
Prognosis (how long people with the disease live)
Brain gliosis can be caused by diseases associated with the cardiovascular and nervous systems, but it can also provoke the appearance of diseases of this nature. Regardless of age, both adults and children have the same conditions for dealing with this problem.
But as a rule, such people do not live more than 2-3 years.
Of course, only a doctor can determine how life-threatening glial tumors are, so first of all you should contact a specialized clinic as early as possible and identify the cause of their appearance, which will help you understand further actions and develop the necessary therapy.
What is cerebral gliosis
Normally, from 10 to 40% of the total volume of the human brain is occupied by glia. These are support cells that perform a number of functions, including:
- trophic;
- secretory;
- support, etc.
Normally, the distribution of additional cells in the brain is diffuse, that is, they are present in almost all the tissues that form this organ. Their numbers are greatest in the subcortical sections of both hemispheres.
If functional brain tissue, that is, neurons, has been damaged, glia quickly become activated and begin to rapidly divide. In places of greatest structural disturbance, foci of gliosis are formed, where the density of auxiliary cells is extremely high. This is a compensatory mechanism that allows you to restore metabolic processes even with the death of a large volume of functional tissue.
Thus, the additional cells form a kind of scar, which allows the remaining functional tissues to restore their functions. Such defects are common. They can also form with microangiopathy, accompanied by small hemorrhages in the brain, and with degenerative damage to neurons.
Differential diagnosis
An important point is the differential diagnosis of dilated Virchow-Robin spaces and other brain pathologies.
Lacunar infarction
Criblurs, with their large size and fusion with each other, can be mistaken for a lacunar infarction. Often confusion arises due to the same localization - in the basal ganglia region.
The difference is that during a heart attack, the lesions usually exceed 5 mm in size. Also, the lesions are asymmetrical. An experienced radiology doctor will be able to distinguish using various imaging modes: T1, T2, FLAIR.
The differential diagnosis between an enlarged perivascular space and a stroke is important, since if left untreated, a more extensive brain catastrophe may subsequently occur with the formation of a neurological deficit.
Stroke treatment is carried out under the supervision of a neurologist.
Cystic periventricular leukomalacia
This disease occurs in premature babies due to impaired breathing. The brain suffers from oxygen deficiency and stroke lesions appear along the vessels, which are very similar to Virchow-Robin spaces.
In most cases, the disease does not require therapy. If the cysts reach large sizes, surgical removal is possible.
Multiple sclerosis
Foci of this demyelinating disease can be located in any part of the brain, including around the cortical vessels.
A distinctive feature is that in multiple sclerosis the lesions originate from the lateral ventricles, forming the so-called “Dawson's fingers”.
When clinical signs of multiple sclerosis are identified, DMT therapy is prescribed.
Cystic tumors
Often, dilated perivascular spaces may resemble a cystic neoplasm. In this case, the cyst has different intensity inside the neoplasm and accumulates contrast. In this case, you need to contact an oncologist and neurosurgeon.
Treatment methods
Treatment of brain gliosis begins in order to preserve the remaining neurons, ensure normal nutrition of brain tissue, eliminate the lack of oxygen, and maintain metabolism at the required level.
Typically, a complex of therapeutic measures is used, including the prescription of various medications:
- drugs that improve blood circulation and nutrition of brain tissue. This effect can be achieved with the help of Actovegin, Viplocetine, Cavinton, Cinnarizine;
- drugs that prevent platelet aggregation and help strengthen arterial walls. These are vitamin complexes and medications containing acetylsalicylic acid;
- nootropic drugs. They help increase the resistance of the nervous system to the influence of adverse factors. For these purposes, Piracetam, Phezam are prescribed;
- lipid-lowering drugs. The use of statins and fibrates makes it possible to stop the development of neuroglia in blood vessels due to the formation of atherosclerotic deposits;
- analgesics. Prescribed to alleviate the patient's condition and eliminate constant headaches.
In rare cases, surgical treatment may be used. Such intervention is necessary if epilepsy attacks occur under the influence of a large gliosis lesion. It is impossible to eliminate the formation of multiple lesions by surgical treatment. Therefore, the patient must take medications for the rest of his life.
Some people prefer to treat gliosis with folk remedies. To improve metabolic processes in brain tissue and stabilize the functioning of the circulatory system, medicinal plants are used.
To improve well-being, the patient is recommended to solve the problem of excess weight. To do this, it is useful to increase the level of physical activity, arrange fasting days, and make changes to your lifestyle.
Treatment of pathology should be aimed at combating the main cause of the problem. If you do not limit the impact of provoking factors, then there will be no effect from therapeutic methods.
What else leads to illness?
Focal pathologies can be caused by traumatic brain injuries, hematomas, and edema.
The following can also lead to the development of lesions:
- Spinal pathologies. One of the most common causes is osteochondrosis, in which nerves and blood vessels are compressed. As a result, an insufficient amount of blood enters the brain, cell nutrition is disrupted, and lesions of the brain arise.
- Fractures of the cervical spine. Within the neck there are two large vessels. When fractured, they can be damaged (torn, compressed). Impaired blood flow in the cervical region leads to inhibited blood supply to the brain. As a result, cells suffer from a lack of oxygen and nutrients.
- Excess weight. This reason is considered secondary. Obesity can lead to impaired brain function. Obesity with lack of physical activity is especially dangerous.
- Atherosclerosis. With this pathology, cholesterol plaques form in the vessels. They clog the lumen of the vascular bed, which leads to a lack of nutrients.
- Endocrine pathologies.
Diagnostics
Although there is no cure for gliosis, its progression can be stopped by pinpointing and eliminating the cause. This requires a thorough diagnosis.
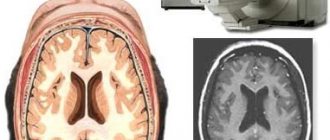
The most effective method is magnetic resonance imaging (MRI) with contrast. This instrumental method allows you to reliably determine:
- size of the lesion;
- location of the affected area;
- the reason for the development of the pathological process (a detailed neurological examination may be necessary).
MRI in the subcortical region can detect gliosis of the white matter of the frontal lobes of the brain, which cannot be detected by other methods.
Similar and even more detailed information can be obtained through computed tomography (CT), which identifies hypodense dark areas of the cortex with reduced density. Additional diagnostic methods are used:
- EEC (detects disturbances in the functioning of neurons);
- angiography (intracranial and extracranial);
- Dopplerography.
Laboratory tests (blood, urine, etc.) may also be prescribed. All this allows you to get the most complete picture of the patient’s condition.
The size of the neurogliotic formation can be calculated. It will be equal to the ratio of the number of glial cells to the number of ordinary brain neurons per unit volume of tissue.
Causes
Gliosis of the white matter of the brain interferes with the full functioning of the nervous system, but it is necessary to fight this disease not directly, but by investigating its cause.
Basically, the catalysts for the appearance of glial accumulations are infectious or other causes of diseases of the nervous system, such as:
- hereditary diseases associated with the death of neurons;
- multiple sclerosis - destruction of nerve tissue fibers in the brain and spinal cord;
- tuberous sclerosis is a genetic disease in which benign tumors develop;
- epilepsy;
- trauma at birth (in infants);
- head and back injuries;
- high blood pressure and encephalopathy;
- cerebral edema;
- chronic or acute cerebrovascular accident (CVA/CVA);
- hypoxia – acute lack of oxygen in tissues;
- neuroinfections such as leukoencephalitis, encephalomyelitis, etc., caused by viruses or bacteria;
- low blood sugar;
- high consumption of animal fats;
- previous operations;
Glial accumulations are often observed in athletes who have suffered head concussions, as well as in those who are exposed to bad habits such as alcohol and drugs that contribute to the destruction of neurons. These changes may also occur in patients taking narcotic-based medications.
Symptoms and diagnosis
Single lesions have no symptoms, so they are detected only during MRI and angiography.
Gliosis has the following symptoms:
- regular headaches;
- convulsions;
- increased blood pressure;
- dizziness and fatigue;
- numbness or paralysis of the limbs;
- hearing and vision impairment;
- disappearance of the swallowing reflex, hearing and vision in newborns.
The diagnosis cannot be made by clinical symptoms, therefore, to detect gliosis, a neurologist prescribes an MRI (magnetic resonance imaging), which establishes the location and proliferation of glial cells. In some cases, MRI can determine the time of onset of gliosis.
As additional diagnostic measures, it is possible to conduct an ultrasound examination, analysis of the lipid spectrum of the blood, examination of the cerebrospinal fluid, duplex scanning of the heart and blood vessels.
You will learn more about the diagnostic method of MRI in the following video:
This article provides more detailed information about magnetic resonance imaging.
Characteristic symptoms
Due to foci of gliosis, brain activity is disrupted and tissues atrophy. Over time, symptoms of various central nervous system diseases are observed:
- Headache. It is regular. The headache can vary in intensity, most often it is severe pain. It often appears at those moments when a person is trying to concentrate or is engaged in mental activity. Gliotic changes often make themselves felt after injuries, especially if the temple area was affected. The brain in this area is responsible for associations. Headache is considered a direct symptom of gliosis.
- The pressure jumps. This is often observed with vascular gliosis. It seriously affects blood pressure readings. Due to the fact that blood vessels are compressed and tissue atrophies, the lumen of the vessels narrows. Blood circulation is impaired. This worsens a person’s well-being, and spontaneous pressure changes appear.
- Dizziness, convulsions. They are recorded if gliosis was caused by surgery or trauma. Even small brain damage can have big consequences.
- Neurological symptoms, disturbances in the central nervous system. This is observed in the later stages of development of this pathology. To determine which area of the brain is affected, instrumental diagnostics are used.
Symptoms of the disease
Cerebral gliosis, not being a separate disease, does not have any characteristic symptoms. All disorders associated with disturbances in the functioning of the central nervous system are inherent in many other ailments.
Moreover, unless gliosis is associated with a neurological disease such as multiple sclerosis, there are no symptoms at all. Diagnosed randomly, along with the underlying disease.
The causes of the disease may be different, but the manifestation, if any, is approximately the same:
- constant headaches, treatment with standard anti-spasm drugs has no effect;
- changes in blood pressure are not specific;
- constant dizziness, general weakness or excessive fatigue. The causes of the condition may be different, but against the background of memory deterioration they should cause concern;
- deterioration in coordination of movements. The cause of the symptom is associated with the replacement of damaged nerve tissue by glia and, accordingly, poor signal transmission;
- memory deterioration, noticeable decrease in mnestic functions. The reason is the same - lack of functional nerve tissue. Treatment in this case is useless.
Sometimes the disease provokes seizures. As a rule, the cause is a large lesion.
Otherwise, the disease manifests itself in young children. The reason for the replacement of nervous tissue with glia is associated with any congenital pathologies. That is, first, as a result of the disease, nerve cells die, and then the affected area is filled with glia.
For example, Tay-Sachs disease, which results in the development of gliosis, appears at 4–5 months of a child’s life. Symptoms indicate disturbances in the functioning of the central nervous system: regression of physical and mental development, loss of hearing and vision, difficulty swallowing, convulsions. The prognosis in this case is extremely pessimistic, and treatment does not produce results.
Brain swelling
White spots on an MRI may indicate swelling of the brain tissue. They develop against the background:
- tumors;
- injuries;
- ischemia;
- inflammation;
- hemorrhages.
At the initial stage of the disease, MRI reveals signs of perifocal edema in the form of light spots in the area of the affected area of the organ. If normal blood circulation is not restored, generalized edema develops. The brain swells. On an MRI, this is visible in a blurry picture in which the structures of the organ are not visible, since they all provide a high-intensity signal to the tomograph.
Forms and degrees of development
According to morphological characteristics:
- isomorphic form of gliosis – characterized by ordered proliferation of neuroglia;
- anisomorphic type of disease – characterized by a predominance of cellular structure and chaotic growth;
- fibrous form – signs of a predominant fibrous structure are clearly expressed.
Based on the nature of the process and its prevalence, they speak of:
- The focal type of the course is a limited area of gliosis (usually in the parietal or temporal lobes), the cause of which was trauma, an infectious or inflammatory process.
- Diffuse type of course – multiple lesions of various sizes and locations. Cystic-gliotic formations of vascular origin are often found.
Depending on the location of the foci, gliosis is divided into:
- Periventricular gliosis - glial proliferations are localized in the area of the ventricles of the brain.
- Perivascular location of foci (vascular gliosis) is the most common type of course. It is distinguished by the presence of glial growths along atherosclerotic vessels. Diagnosed as microangiopathy with the presence of single or multiple foci of gliosis. The variety is the subtentorial type (a few lesions appear as a result of birth injuries or age-related changes, and multiple lesions arise as a consequence of circulatory disorders).
- Subependymal - single lesions localized on the inner lining of the ventricles.
- Marginal - foci of glial degeneration are located in the intrathecal region.
- Marginal - areas of replacement glial tissue are located on the surface of the brain.
Causes of GM damage
Focal lesions can be caused by a variety of reasons.
In case of focal lesions of the brain of a dyscirculatory nature, the cause may be a lack of nutrients caused by circulatory disorders (with ischemic heart disease, stroke and other pathologies). Often the cause of the disease is a neoplasm. It has a negative effect on neighboring areas of the brain, causing various changes in them, including the death of brain cells.
Treatment
There is no specific therapy for gliosis. Treatment methods depend on the underlying disease that caused the death of neurons. Main goals of therapy:
- slow down the progression of the process;
- ensure normal trophism of central nervous system tissues;
- eliminate oxygen starvation;
- normalize metabolic processes.
Traditional medicine
To eliminate the symptoms of brain changes, the following groups of drugs are prescribed:
- Vasoactive - drugs that activate cellular metabolism and improve tissue trophism (Cavinton, Vinpocetine).
- Antiplatelet agents are drugs that slow down platelet sedimentation (all derivatives of acetylsalicylic acid).
- Agents that improve the condition of the walls of small and large arteries (Ascorutin, vitamins).
- Nootropic substances - they increase the resistance of the central nervous system to the effects of negative factors (Piracetam, Nootropil).
- Statins – have lipid-lowering properties, preventing the development of atherosclerosis (Fenofibrate, Atorvastatin).
- Painkillers and antispasmodics to relieve headache attacks.
Surgery
Surgery for gliosis is prescribed extremely rarely.
Only for single large lesions. After surgery, treatment of the underlying disease that caused the death of neurons must be continued to avoid the development of relapses.
Indications for surgical intervention for a large single lesion are:
- violation of the outflow of fluid (CSF);
- convulsive seizures caused by a large area of gliosis;
- diagnosed neoplasm;
- changes in the functioning of internal organs.
With multifocal gliosis, only constant conservative treatment has a positive effect.
Complementary and alternative methods at home
Traditional medicine methods can be used only after consultation with a neurologist. Homeopathic remedies are prescribed as concomitants against the background of conservative therapy.
Decoctions and infusions of medicinal plants and fruits improve the functioning of the cardiovascular system and stimulate metabolism.
Diet for gliosis changes
The diet for gliosis is aimed at:
- Improving brain function and relieving vascular spasms. To achieve this result, you need to eat foods rich in magnesium: buckwheat, pearl barley, corn cereals, nuts, pumpkin seeds, lentils, cabbage of all varieties, figs.
- Relieving edema, improving heart function - foods with a high potassium content are introduced into the diet: citrus fruits, green vegetables and fruits, dried fruits, mushroom and potato dishes.
- Weight loss - to control body weight, remove baked goods, canned food, carbonated sweet drinks, smoked foods, fatty meats, fast food and semi-finished products from the daily diet.
The daily diet consists of fish, lean meat, cereals, fermented milk products, hard cheese, vegetables, nuts and fruits. It is better to steam, boil or bake foods.
Features of studying the brain using MRI
Before the invention of the magnetic tomograph, identifying brain pathologies was difficult - the only device that took pictures was an X-ray.
This method was not suitable for this type of diagnosis; the images were uninformative and gave a rough idea of the hidden pathology.
MRI helps to study the brain parenchyma and the condition of blood vessels; this method is safe; the tomograph takes many pictures from different angles.
The doctor will definitely recommend a study in the following cases:
- after a stroke;
- with constant headaches;
- if there is frequent vomiting;
- after traumatic brain injury;
- with movement coordination disorder;
- after surgery on the skull;
- if you suspect cancer.
The main feature and advantage of MRI is safety; during procedures, the body is exposed to a magnetic field that does not harm health.
MRI
Before the examination, you will need to remove metal jewelry; you cannot move during the operation of the tomograph, so the head is fixed with special devices. Pictures are taken in a prone position.
Treatment and diagnosis
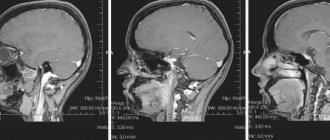
The main way to find multiple lesions is to visualize the medulla on magnetic resonance imaging. On layer by layer
Spots and pinpoint changes in tissue are observed in the images. MRI shows not only lesions. This method also reveals the cause of the lesion:
- A single lesion in the right frontal lobe. The change indicates chronic hypertension or a previous hypertensive crisis.
- Diffuse foci throughout the cortex appear when the blood supply is disrupted due to atherosclerosis of the cerebral vessels or.
- Foci of demyelination of the parietal lobes. It speaks of a disruption in the flow of blood through the vertebral arteries.
- Massive focal changes in the white matter of the cerebral hemispheres. This picture appears due to atrophy of the cortex, which forms in old age, from Alzheimer's disease or Pick's disease.
- Hyperintense lesions in the white matter of the brain appear due to acute disruption of the blood supply.
- Small foci of gliosis are observed in epilepsy.
- In the white matter of the frontal lobes, single subcortical foci are predominantly formed after a heart attack and softening of the brain tissue.
- A single focus of gliosis in the right frontal lobe most often appears as a sign of brain aging in older people.
Magnetic resonance imaging is also performed on the spinal cord, in particular on the cervical and thoracic regions.
Related research methods:
Visual and auditory evoked potentials. The ability of the occipital and temporal regions to generate electrical signals is tested.
Lumbar puncture. Changes in the cerebrospinal fluid are examined. Deviation from the norm indicates organic changes or inflammatory processes in the cerebrospinal fluid ducts.
A consultation with a neurologist and psychiatrist is indicated. The first studies the functioning of tendon reflexes, coordination, eye movements, muscle strength and synchrony of extensor and flexor muscles. The psychiatrist examines the patient’s mental sphere: perception, cognitive abilities.
Foci in the white matter are treated with several branches: etiotropic, pathogenetic and symptomatic therapy.
Etiotropic therapy is aimed at eliminating the cause of the disease. For example, if vasogenic lesions of the white matter of the brain are caused by arterial hypertension, the patient is prescribed antihypertensive therapy: a set of drugs aimed at lowering blood pressure. For example, diuretics, calcium channel blockers, beta blockers.
Pathogenetic therapy is aimed at restoring normal processes in the brain and eliminating pathological phenomena. Drugs are prescribed that improve blood supply to the brain, improve the rheological properties of blood, and reduce the need for oxygen in brain tissue. Vitamins are used. To restore the functioning of the nervous system, it is necessary to take B vitamins.
Symptomatic treatment eliminates symptoms. For example, for seizures, antiepileptic drugs are prescribed to eliminate foci of excitation. In case of low mood and lack of motivation, the patient is given antidepressants. If lesions in the white matter are accompanied by an anxiety disorder, the patient is prescribed anxiolytics and sedatives. If cognitive abilities deteriorate, a course of nootropic drugs is indicated - substances that improve the metabolism of neurons.
Didn't find a suitable answer? Find a doctor and ask him a question!
Perivascular zone, its structure and functions
Virchow-Robin spaces (VRO) are slit-like formations surrounding the cerebral vessel along its path from the subarachnoid region into the brain tissue.
There is still no single point of view on what perivascular spaces are. Most scientists believe that this is the area between the middle (arachnoid, arachnoid) and inner (pia) meninges. This area normally surrounds the substance of the brain and, together with the vessels, is drawn into the brain, surrounding them. The subarachnoid region, located in the cerebral cortex, is called the Virchow-Robin space.
There is no single point of view; only arteries or also veins surround the perivascular spaces. It was revealed that they continue to the level of capillaries.
It is believed that this formation is involved in the movement of cerebrospinal fluid and ensures the exchange of necessary substances between cerebrospinal fluid and neurons.
Another function is to isolate intravascular blood from brain tissue. The blood contains a number of toxic substances that normally should not enter the brain substrate due to the presence of the blood-brain barrier. Additionally, toxins are absorbed within the perivascular region.
Another challenge is immune regulation.
Causes and consequences of pathological complications
The etiology of development is influenced by various factors. The congenital disease is rare and leaves virtually no chance of survival. In other cases, changes occur due to past illnesses and injuries.
Gliosis can be caused by:
- heredity;
- encephalitis infection, including subcortical;
- meningitis;
- concussions and other injuries (concussion occurs);
- hypoglycemia;
- trauma received during childbirth;
- hypoxia;
- hypertensive crisis;
- damage to the central nervous system;
- elderly age;
- diseases of vascular origin;
- post-ischemic gliosis - occurs if a person has suffered an ischemic stroke.
Late diagnosis and untimely treatment in an adult can lead to complications. The consequences of neglect are dire and can lead to disability.
| Consequences/possible complications | Short description |
| Stroke | Acute cerebral circulatory disorder of a vascular nature. |
| Epilepsy | An attack with convulsions, characterized by their sudden appearance. |
| Multiple sclerosis | Damage to nerve fibers in the hypodense zone of the brain and spinal cord (possibly as a result of ischemia). Leads to atrophic changes and dysfunctions of memory, intelligence, etc. |
| Hypertensive crisis | An excessive increase in blood pressure can lead to swelling of the brain on the right or left (including in the thalamus). |
| Epiritinal gliosis | The retina of the eye stretches and distortion or loss of vision occurs. |
| Paralysis | Lack of motor functions, partial or complete. |
| Oncology | A malignant tumor of the brain tissue (gliosarcoma). |
| Endometriosis | Damage to endomitriotic lesions of the brain. |
| Dementia | Dementia, accompanied by loss of acquired skills and knowledge, eventually leads to complete degeneration. |
For newborn children, such a diagnosis means death. After a few months of birth, pathological processes worsen and develop into a severe form of gliosis. In newborns, hydrocephalus, leukomacia (perventicular necrosis), abnormal development of the cerebellum in children, etc. can be diagnosed.
Perventicular gliosis of the brain is also dangerous, but degenerative tissue changes are localized in the ventricles.
How long adults live depends entirely on the speed at which the disease is diagnosed and the start of its treatment.
Neuroglial proliferation and vascular damage
Vascular diseases of the central nervous system often lead to disability and death. The brain requires a lot of energy to function properly. It is delivered by the bloodstream using four arteries. Difficulty in their work may indicate that the patient has a disease. Over time, the malaise develops into a full-fledged disease associated with chronic cerebral circulatory failure. Chronic atherosclerosis and arterial hypertension are the most common causes of vascular diseases.
Sometimes the culprit of insufficient cerebral circulation may be osteochondrosis (the main symptom is headache in the right or left frontal lobe). Deformed intervertebral discs block the arteries, preventing them from fully performing their main function. A constant disruption of the blood supply of a local nature (age-related, toxic or other type) in the occipital region leads to the death of neurons and the appearance of glial cells.
Leukoaraiosis is diagnosed in patients with severe forms of vascular origin. The picture of manifestation is a decrease in the density of nerve tissue and headaches in the temporal region.
Microangiopathy
What it is? Pathology of blood vessels caused by their damage. The disease develops as a result of past liver diseases, oncology, diabetes, etc.
Microangiopathy with the presence of foci of gliosis is manifested by damage to small blood vessels and disturbances in the processes of blood clotting. The disease is accompanied by renal failure and purpura (subcutaneous effusions).
The disease is divided into four types:
- cerebral;
- lenticulostriate;
- diabetic;
- hypertensive.
Clinical picture of microagiopathy:
- burning and pain in the legs;
- irritation;
- stomach and nosebleeds;
- calloused and dry feet.
Symptoms also include coughing up blood, decreased vision, headache in the frontal lobes, and blood clots in the urine.
Causes of gliotic changes
Hereditary predisposition is considered one of the main (25% of cases) causes of the development of gliosis. The occurrence of gliosis changes is associated with the following diseases affecting brain tissue:
- Multiple and tuberculous sclerosis.
- Encephalitis and encephalopathies of various etiologies.
- Oxygen starvation (hypoxia).
- Status epilepticus.
- Arterial hypertension occurring in a chronic form.
- Diabetes mellitus and other metabolic disorders.
- Drug use.
- Neuroinfections occurring in acute and chronic forms.
- Cerebrovascular pathologies.
- Neurodegenerative processes.
- Chronic renal failure.
- Phakomatoses (hereditary, chronic diseases characterized by damage to the central nervous system, skin, visual organs and other body systems).
Some doctors make an analogy. If a person's skin is damaged, scars form on them. Such “scars” appear in nervous tissue after damage and partial death of neurons. The process does not occur spontaneously; it is always a consequence of primary pathology. The most common reason is deterioration of blood flow in the circulatory system supplying the brain, associated with damage to the vascular wall, narrowing of the lumen, or disruption of neurohumoral regulation.
Gliotic changes in the intracranial structures of the head in adults are detected after cerebral infarctions, strokes, and after the appearance of foci of intracerebral hemorrhage. Similar transformations of nervous tissue are detected after neurosurgical intervention and poisoning with harmful substances (carbon monoxide, salts of heavy metals, narcotic substances). Gliotic foci form around tumor neoplasms.
Types of changes
In medicine, dystrophic manifestations in the brain substance are divided into two types:
- Diffuse.
- Focal.
In the first case, pathological changes spread evenly to the entire brain, and not to its individual areas. They are caused either by general disturbances in the functioning of the blood supply system or by infections (meningitis, encephalitis, etc.).
An important cause of this condition is thought to be changes in blood flow to the area around the ventricles of the brain, which is fragile and prone to injury, especially before 32 weeks of gestation. Premature babies with intraventricular hemorrhage are also at increased risk of developing this condition
Exams used to diagnose periventricular leukomalacia include ultrasound scanning and MRI of the head. The cardiac, pulmonary, intestinal and renal activity of premature infants is carefully monitored and treated in the Neonatal Intensive Care Unit.
Diffuse changes are manifested mainly by a decrease in a person’s performance, a dull headache, difficulty switching to another type of activity, a narrowing of the patient’s range of interests, apathy and sleep disorders.
And what a focal change in the brain substance of a dystrophic nature is can be understood by the fact that it can be caused by various minor pathologies:
These problems often arise during the first or second year of life. This condition can cause cerebral palsy, especially stiffness or increased muscle tone in the legs. These will likely be those that compromise movements such as sitting, crawling, walking, and weapon movement. These children may require physical therapy. Extremely premature babies have more problems with learning than with movement.
The child should visit his regular pediatrician for scheduled exams. Neonatal diseases of prenatal and perinatal origin. Hypoxico-ischemic encephalopathy: neuropathology and pathogenesis. Introduction. The predominant semiologic picture should be considered in conjunction with the patient's clinical context and epidemiological data to reach a diagnostic conclusion.
- cysts (small cavities that form in the brain),
- small foci of necrosis (tissue death in certain areas caused by lack of nutrients);
- gliomesodermal (intracerebral) scars that occur after injuries and concussions;
- minor changes in the structure of the brain matter.
That is, these are pathologies that cause disturbances in the blood supply in a small area. True, they can be either single or multiple.
The microcirculation of the brain forms a very complex vascular network of anatomy and varies among individuals. The vesicular arteries, in their deep course in the white matter, establish very little capillary anastomosis with adjacent nutritional arterioles, constituting relatively independent arterial metabolic units. On the other hand, the deep subepidemic arteries, which occur in the choroidal arteries, give penetrating branches to the white matter, although its path is shorter than that of the parade ground arteries.
There is a second terminal system of cortical and subepidemic arteries that supply the basal ganglia. There is very little anastomosis between the superficial and deep arteriolar systems. The arterial and venous systems are anatomically quite parallel. The perivascular space surrounds the wall of arteries and arterioles, as well as veins and venules, from the subarachnoid space to its intraparenchymal path.
When expansion of perivascular spaces is normal
Perivascular canals can only be seen using MRI.
Often Virchow-Robin spaces are not visualized even on MRI images due to their small area. The resolution of the tomograph matters. A size of up to 2 mm is normal and occurs in all people.
Enlarged perivascular spaces are called criblures.
Signs of dilated perivascular spaces on MRI
Their increase does not always indicate pathology. The mechanism of their expansion is still being studied. This is possible due to inflammation of the vessel wall, when the latter becomes thinner and becomes more permeable. The released liquid causes the criblure to expand. Another reason is a violation of the flow of cerebrospinal fluid, and another is the lengthening of blood vessels.
Scientists and practicing doctors have not come to a consensus on what is considered pathology and what is not. As a rule, fixation of spaces on MRI images in people of the older age group is a variant of the norm.
Criblures in the brain are often found in children in the first year of life.
They are usually localized in three areas:
- Along the course of the lenticular arteries supplying blood to the basal ganglia - the caudate nucleus, internal capsule, fence.
- Along the course of certain arteries that enter the brain from its outside, and not like most branches of the carotid and vertebral arteries from the inside.
- Along the vessels supplying the midbrain (posterior thalamoperforating and median mesencephalothalamic arteries).
Appear symmetrically. Most often, expansion of the perivascular spaces occurs in the region of the lower basal structures and very rarely in the cerebellum. As a rule, the dimensions do not exceed 5 mm.
CSF flows in the perivascular canals, so on MRI the criblures have the same plane as the latter and appear isodense.
There are 2 projections in which MRI images of the brain are usually taken: frontal and axial. In the first case, the expanded spaces appear in the form of stripes, and in the second they take on a round or oval shape corresponding to the cross-section.
The use of various MRI modes, especially T-2, helps in diagnosis. In this mode, Virchow-Robin spaces do not have a darker rim around the filled area, which indicates that this is part of the subarachnoid membrane, and not the wall of a cavity, lesion or neoplasm.
Criblurs on MRI images
What to do and how to treat
There are no specific medical recommendations for eliminating the tumors in question. The treatment for brain gliosis prescribed by a specialist will be aimed at combating the disease that became the “trigger” mechanism for the appearance of gliosis. Medicines must be prescribed strictly by a doctor. Drug therapy will consist of taking medications that can maintain the condition of the blood vessels. In addition, patients are often prescribed antioxidants and nootropics to neutralize oxidative processes, because with this disease there is a lack of oxygen.
Diagnostics
To diagnose the disease, CT, MRI and EEG are performed. Let's consider in what cases one or another method is used.
Magnetic resonance imaging is the most preferred method. With its help, the doctor will see foci of gliosis in the frontal lobe and understand how advanced the situation is.
Computed tomography is also sometimes used by specialists to diagnose white matter gliosis in the brain. However, this method will not provide such a necessary clinical picture as MRI. A significant disadvantage for the patient will also be the presence of radiation during the procedure.
Electroencephalography - finding out how active the brain is. Electrodes and computer processing are used. This method is often used to clarify problems when epilepsy or seizures are present.
Often, in order to get a detailed picture, it makes sense to conduct additional examinations, namely, take tests or perform other manipulations.
Medicinal methods and surgery
Among drug therapy, commonly prescribed drugs are:
- Aimed at improving brain function;
- Improving cerebral circulation;
- Vitamins.
Surgeries are also considered if treatment with medications does not bring the desired result and any other treatment has been tried without a positive effect, but the focus of gliosis remains and the disease progresses.
Traditional treatment
In addition to the usual, traditional methods of treatment, there are also so-called traditional methods of combating gliosis, or rather the source disease.
So, to improve blood circulation, you can use the following herbs:
Dandelion root. Helps strengthen blood vessels and lowers cholesterol. Used as a decoction.
Melissa. Positive effect on the cerebral cortex, strengthens vascular walls, acts as a sedative, restoring nerve cells.
Dill seeds. They can restore blood circulation and help normalize blood pressure.
St. John's wort. Positive effect on vascular lesions, tissue restoration.
Dioscorea. Indicated for vascular and cardiac problems, relieves headaches. The root is crushed and brewed, after which it is taken several times a day, a tablespoon after meals.
Complications, consequences
Most often, this pathology does not cause obvious symptoms. This is her cunning. With large lesions affecting neurons, it may:
- The intellect suffers.
- Problems with speech and memory will appear.
- Increase pressure.
- Asthenia develops.
- Paresis and paralysis appear.
- Coordination is impaired.
- Visual and auditory pathologies appear.
- The psyche becomes deformed.
- Develop dementia (dementia).
More often, such a misfortune happens to adults. In this case, it becomes difficult for a person to perform even the simplest work activities. He cannot drive a car and is exempt from military service.
Complications can be very serious. It all depends on the size of the scar and how active the pathology that caused its appearance is.
Consequences and life prognosis
Gliosis of the brain cannot be called a minor pathology. This situation requires immediate medical attention. The prognosis for such patients will depend entirely on the extent of the gliosis process and the diseases that caused it. Often it is enough to undergo a course of therapy with a neurologist, and the disease will recede. Sometimes treatment can take years without improvement.
Unfortunately, newborn children suffer from this disease much more severely than adults. The death of nerve cells in infants progresses rapidly, leading to the death of the child. During routine examinations of pregnant women, ultrasound diagnostics can reveal glial changes in the fetal brain. In this case, the question of termination of pregnancy .
Who is at risk
Any disease has its own risk groups. People belonging to such groups should closely monitor their health and immediately consult a doctor at the first suspicious symptoms. With focal pathologies, this group includes patients:
- Hypertension, hypotension.
- Diabetes.
- Atherosclerosis.
- Rheumatism.
- Obesity.
- Sensitive, emotional people living in constant stress.
- Leading a sedentary life.
- Elderly people, regardless of gender (starting from 55-60 years).
They also provoke the development of vascular pathologies:
- Meteor dependence.
- Alcohol abuse.
- Osteochondrosis.
- Addiction.
- Arrhythmia.
- Aneurysms of cerebral vessels.
Signs of gliosis
Quite often, the patient learns about the presence of a single focus of gliosis in his brain, by chance, during a routine examination. At the same time, nothing bothers the person. This situation requires special attention.
The patient must be carefully examined and the reason why the lesion formed is identified, that is, the disease that provoked the proliferation of glial fibers. In the case of multiple foci of glia, the situation is different; unpleasant symptoms cannot be avoided.
Symptoms:
- Constant headaches.
- Blood pressure surges
- Dizziness.
- Violation of intellectual activity.
- Loss or impairment of coordination.
- Changes in speech functions.
- Paresis and paralysis.
- impairment .
- Changes in the mental sphere.
- Dementia.
The larger the area of brain damage, the more pronounced the symptoms of this disease.
General information about gliosis
What is the brain and how does gliosis affect it? Every second, micromovements are carried out in it at the neural level, which affect the work and vitality of the entire organism. Such processes occur unnoticed in the human brain, so disturbances in their functioning are revealed only over time. In a functioning nervous system, some components are of primary importance, while others are auxiliary.
The human central nervous system contains the following cellular formations:
- neurons - produce and propagate signals;
- ependymal cells - line the brain cavities, form the central canal of the spinal cord;
- neuroglia - provide basic metabolic processes, and after the death of neuronal cells, they take their place and perform their functions.
If the medulla has any pathologies or has been subjected to traumatic influences accompanied by the death of neurons, gliosis occurs. Neuroglial cells grow and fill the empty space, becoming catalysts for rebuilding the remaining neurons so that they can optimally perform their functions.
It is the neuroglia, replacing dead neuronal cells, that create the focus of gliosis in the brain. These cells are smaller in size than neuronal cells (about 10-15 times), while their number is greater, and the cells themselves occupy about 40% of the total mass. In addition to providing metabolic function, glial cells help neurons generate and propagate signals throughout the nervous system.
The formation of foci of gliosis occurs regardless of age, at any period of life. Although the risk of its occurrence is higher in old age. If there are no changes in the structure of the area of the brain where neuroglia are located, then there is no significant effect on the performance of brain functions.
It cannot be said that filling the resulting empty zones with glia is destructive.
Although these cells are unable to perform neuroregulatory functions, they contribute to:
- maintaining metabolic brain processes;
- protecting tissues that are still healthy;
- formation of renewed nerve fibers;
- reception and propagation of signals (less quality than those transmitted through neurons).
The study of gliosis in the brain has been going on for a long time. Clinical tests helped to identify the dependence of the growth of neuroglia on a person’s age - the older he is, the more actively these cells multiply.
The older a person gets, the more actively neuronal cells die off, and the result of this process is structural changes in the brain, against the background of which there is a deterioration in memory, reaction speed and coordination. Medications can partially restore the functionality of the central nervous system in older people.
This disease cannot be predicted, since it is caused by a mutated gene that affects the synthesis of hexoseaminidase A in the body (an enzyme that ensures the metabolism of gangliosides). When accumulated in the cells of the central nervous system, gangliosides cause dysfunction of the nervous system.
The likelihood of hereditary formation of this disease in children increases if the mutating gene is present in the body of both parents (the prognosis is approximately 25%). If the first child was diagnosed with gliosis, then parents should take part in a repeat study before planning a new addition to the family.
A geneticist is a doctor who is able to calculate the probability of having a child with such a pathology.
During their proliferation, glial cells are capable of triggering the formation of gliosis. This disease cannot be fully cured, but it is important to prevent the pathological spread of the disease.
Types of disease
Because, due to the pressure of developing neuroglia, necrotic cells gradually die and die. Against this background, small areas of gliosis of different sizes and shapes appear, which can be located in any area of the brain. The pathological process is classified into several forms:
- Intraventricular - lesions form inside the ventricles of the brain, which contributes to a significant reduction in their volume, as well as the volume of cerebrospinal fluid.
- The formation of lesion islands that form around atherosclerotic vessels, which are severely compressed under pressure.
- Regional - involves the formation of single lesions that are concentrated outside the brain tissue (this type of neuroglia is the simplest, since it does not affect the central region).
- Fibrous - gliotic foci can be filled with fibers, which can have different lengths and sizes.
- Massive neuroglia - multiple foci are formed in different areas of the brain tissue (when scanning, the image is displayed as a large spotted field).
- Intrathecal – altered areas are located under the inner membranes of the brain, which significantly complicates the diagnosis of the disease.
- Anisomorphic - altered lesions are located chaotically.
Foci of gliosis
Areas of neuroglial proliferation are a kind of scars at the site of dead neurons; they can be single, include up to 3 glial foci (few lesions) or multiple. The size of the growths can be calculated using the formula: the number of functioning neurocytes to the number of glial cells / per unit volume of tissue. Normally, this figure does not exceed 1:8/10.
With an increase in the number of gliocytes, the functioning of the central nervous system is disrupted, up to a convulsive syndrome. Neurologists believe that such a disruption of the central nervous system is often caused by subtentorial foci of gliosis of vascular origin or subcortical (subcortical) foci.
Single outbreaks
Small foci of gliosis do not cause symptomatic manifestations.
In a child, they are formed as a result of trauma received during childbirth, and the tissue of any lobe of the brain can be damaged.
But more often, single areas of glial changes are localized in the left or right parietal lobe.
In adults, the development of single foci of gliosis is caused by age-related changes or diseases of the central nervous system. Such areas practically do not change over time, therefore, in most cases, they cannot be identified without special examinations.
Multiple lesions
Multiple focal changes in brain tissue, as a rule, develop as a result of acute or chronic circulatory disorders. Forming foci of gliosis enhance the clinical picture of the disease that caused them.
Multiple foci of subtentorial gliosis of the brain appear as a result of traumatic brain injuries and hemorrhages in the tissue under the cerebellar tent. This zone is vulnerable due to the surrounding incompressible spaces filled with cerebrospinal fluid.
Multiple focal changes in the brain substance of a dystrophic nature develop with insufficient blood supply, chronic diseases of the central nervous system, and also as a result of age-related changes.
Foci of gliosis in the brain in the white matter (single) on MRI: what is it?
The nervous system is the basis of a full life and the implementation of human reflex activity. When it is damaged, all the most important functions are disrupted: nutrition, breathing, heartbeat, walking, and balance skills.
If the brain is included in the area of damage, a person may completely lose the ability to form speech, read, write and meaningful activity.
Medullary gliosis is not a disease, but an abnormal process that causes significant impairment of human life.
White matter gliosis - what is it?
Gliosis of the medulla is a complex pathological and morphophysical process that forms in brain tissue under the influence of certain traumatic etiological factors. It is based on the massive growth of a scar at the site of injury (where a certain number of neurons died), which is called neuroglia.
Neuroglia is an additional tissue component of the human brain, normally accounting for up to 30% of the weight of brain tissue. Neuroglia protects the brain substance from damage, distinguishes it from pathogenic microorganisms, secretes useful substances and actively participates in metabolic processes.
When traumatic or infectious damage to brain cells occurs in any part of the brain, an increase in the number of neuroglia is an adaptation mechanism to the changes that have occurred.
Scar tissue should form in place of dead neurons, but neuroglia demarcate it, becoming a kind of biological conductor.
Unfortunately, it cannot function like normal nerve tissue, which causes the main problems that are visible on MRI.
Manifestation of the clinical picture of the disease:
- Sudden changes in blood pressure. In the morning, blood pressure numbers are below normal, but during the day stable arterial hypertension of the second or third degree develops.
- Excruciating headaches and dizziness. Sometimes there is a picture of migraine pain with nausea, vomiting and photophobia.
- Chronic fatigue. Unexplained attacks of fatigue and loss of strength that occur even after prolonged rest in a calm environment.
- Impairments of short-term and long-term memory. The patient cannot remember what he did last evening or how he spent the previous summer.
- Changes in coordination. Frequent falls, blows and a large number of bruises indicate that the patient has severe cerebellar disorders.
- Convulsive and epileptic seizures. If the lesion is large enough, neurological symptoms may appear.
- Disorders of speech, writing and word formation. This pathology is associated with the formation of a lesion in the brain in the area of oral and written speech.
- Hallucinations. Auditory, sound and even olfactory hallucinations can serve as the first sign of the onset of the disease.
- Behavioral disorders. Apathy, depression or excessive aggression act as irrefutable witnesses in brain diseases of various origins.
Types of disease
Necrotic cells begin to gradually die under pressure from growing neuroglia. After this, gliosis islands of various shapes, sizes and locations are formed. There are several types of pathological process:
- The focus of vascular change, otherwise called the perivascular area. Neuroglia form islands, visible on CT films, around atherosclerotic altered brain vessels, causing even greater compression.
- Intraventricular form. Foci of change occur on the inner surface of the ventricles of the brain, due to which their volume and the amount of cerebrospinal fluid are significantly reduced (this change is clearly visible on MRI).
- Edge form. Single simple foci of neuroglia occur in the outer part of the brain tissue: the damage is considered one of the mildest because it does not affect the central area.
- Extensive gliosis represents massive focal tissue lesions. On an MRI, this picture looks like a spotted field.
- Fibrous changes. Gliotic lesions are usually filled with fibers of various sizes and lengths.
- Anisomorphic lesions. Characterized by a chaotic arrangement of neuroglia, more hypodense.
- Intrathecal form. This type of lesion is the most difficult to diagnose using MRI. The changed areas are located under the inner meninges.
Unit formations
Single outbreaks are much more common in the population. They can be found in infants as a consequence of recent birth trauma or in older people as a result of age-related degeneration of brain tissue. This process is completely natural and occurs in 60% of white matter MRI scans in people over eighty years of age.
Typically, such lesions become an incidental finding during screening because they do not cause any significant discomfort to patients.
However, when located in the left frontal lobe area, they can cause some hallucinations. This is explained by the fact that the most important centers of deep feelings and sensations are located in that lobe.
This lesion does not tend to grow and does not pose a great threat in chronic diseases.
Multiple lesions
The incidence of multiple lesions is much lower than a single focus of gliosis.
This pathology can occur in many diseases of the central nervous system (especially white matter), blood vessels and connective tissues.
Most often, the source of lesions of this origin are strokes, heart attacks or atherosclerosis. A similar picture often occurs with traumatic brain injury.
With mild head injuries, the size of the damage does not exceed a few millimeters, which cannot significantly affect mental functions. On a CT scan you can see even the smallest areas with a changed structure.
What diseases cause lesions in the white matter?
The occurrence of such a condition is usually considered multifactorial. The environment, bad habits, family history, genetic and infectious diseases also play a significant role in the formation of pathology. Predisposing factors:
- presence of diseases of the nervous system in relatives;
- work in chemical or physical production;
- engaging in dangerous and extreme sports;
- alcohol and nicotine abuse;
- taking drugs for a long time;
- nutritional disorders: excess fried, fatty and salty foods;
- genetic predisposition to the occurrence of metabolic failures.
Causes of tissue gliosis:
- trophic disorders and metabolic diseases associated with the deposition of pathogenic particles in the brain;
- meningitis and meningoencephalitis;
- tuberculous brain damage;
- epilepsy and status epilepticus;
- pathology of the vascular bundle;
- congenital developmental anomalies;
- infectious-toxic tissue damage;
- damage during birth (ischemia and fetal hypoxia);
- parasitic invasion of any origin;
- traumatic brain injury of any age (bruise, concussion, hematoma);
- stroke and cerebral infarction;
- hypertension or symptomatic arterial hypertension that has existed for more than ten years.
What does gliosis mean?
It is not possible to detect a neurological disorder on your own. Only thanks to a modern non-invasive procedure such as magnetic resonance imaging, a specialist is able to evaluate the neuromuscular system and brain structures, find pathologies of nerves and blood vessels, including gliosis of the brain and spinal cord.
Let's take a closer look at how this violation occurs.
In a healthy person, neurons, glia and nerve ganglia provide a close, inextricable connection between the central nervous system and all organs and tissues. Moreover, each of them carries a specific task.
Excitable neurons transmit signals to muscles and glands, glial cells participate in metabolic processes and provide protection and the necessary conditions for complete transmission of the impulse signal. An accumulation of glial, nerve cells and their processes gather in the nerve ganglia.
Under conditions of natural functioning of the central nervous system, glial cells, when neurons are damaged, are able to replace them and distinguish dead segments from healthy neighboring tissues. Thus, they prevent damage to the entire brain. But the reverse process is also possible, when glia begin to multiply, causing deformation and death of healthy nerve cells.
This is what gliosis of the brain is, which results in extensive replacement of neurons with glial cells. This process is considered quite natural in old age. The remaining categories susceptible to pathology require additional study of the problem.
to contents ^
Treatment of cognitive pathologies
Donepezil is used to improve memory, concentration, and performance. The medicine stimulates the production of neurotransmitters, improves the quality of the passage of impulses as intended. The activity of patients during the daytime improves, apathy disappears, hallucinations and meaningless mechanical repetitions of the same actions are eliminated.
Rivastigmine should not be used by people with ulcers, problems with the intestines, cardiovascular system, or respiratory disorders.
For typical emotional disorders, doctors advise using antidepressants. Selective inhibitors perform remarkably well during treatment. These products are available only with a doctor's prescription.
Gliosis of the white matter of the brain: single and multiple lesions, signs and life prognosis
Brain diseases are the most dangerous, as they can harm all organs and systems of the body, disable many functions of the nervous system and make a person disabled. Gliosis of the white matter of the brain is a very serious disease and requires immediate treatment.
Gliosis of the white matter of the brain - what is it?
For some reason, nerve cells may begin to die in the human brain. Some diseases and conditions can provoke this.
The disease begins with a single area of such a lesion, gradually this area grows, and in place of dead neurons, glia - scar-like tissues that protect the organ from various infections and injuries. Large accumulations of glia form gliosis.
The job of glial cells is to protect the brain. Forming at the site of damage to organ tissue, glia protect the damaged area by enveloping it. If the death of neurons occurs in large numbers, glia cover large areas of the brain, then the nervous system ceases to function normally.
The degree of brain damage is determined by the number of lesions; depending on this, doctors diagnose the type of disease.
Gliosis comes in several types, depending on the location and degree of proliferation of gliosis cells.
Kinds
- Anisomorphic gliosis is diagnosed if the cell fibers are located chaotically.
- The fibrous appearance of this disease is determined by the more pronounced formation of glial cells than the cellular component.
- The diffuse type of the disease means that the area of damage to the brain is very large.
- The isomorphic form of this disease occurs in patients when the glial fibers are located relatively correctly.
- Marginal gliosis is caused by the proliferation of glial cells only in the intrathecal areas of the brain.
- The perivascular type of this disease occurs with atherosclerosis of cerebral vessels. Glial fibers are formed surrounding the affected vessels.
- The subependymal appearance means that the glial growth zone is located under the epindyma.
of diseases that cause gliosis of the white matter of the brain. Even the most banal ailments, which occur quite often, can act as a provocateur of this disease.
Here you can read in detail about gliotic changes in the brain.
Foci of gliosis
Foci of gliosis can vary in number and area. This proliferation of glial tissue occurs against the background of the destruction of its own neurons, it follows that the greater the number of these nerve cells is destroyed, the larger the focus of gliosis will be.
Diseases that provoke gliosis:
- Epilepsy.
- Hypertension lasting for a long period.
- Multiple sclerosis.
- Hypoglycemia.
- Ischemic stroke.
- Low oxygen content in the blood.
- Poor blood circulation.
- Encephalitis.
- Anemia.
- Injuries and swelling of the brain.
Gliosis can also occur for other reasons not related to specific diseases.
Causes:
- Hereditary factor.
- Injuries during childbirth.
- Elderly age.
- Excessive consumption of fatty foods.
The prognosis of treatment and the patient’s life depends entirely on the extent of the gliosis process; the more advanced the process, the more complex the therapy and the longer the patient’s recovery.
Single
Single foci of gliosis can occur in many. This usually means that the patient has hypertension. With constantly elevated blood pressure, after some time, as a rule, hypertensive encephalopathy occurs, which leads to isolated foci of gliosis.
It is important to contact a medical facility to stop the process of neuronal death, otherwise the affected area and the number of lesions may increase significantly. The problem is that it is no longer possible to reverse this process, the nerve cells die irrevocably, and, most importantly, prevent their further destruction.
Gliosis often causes diseases of the nervous system , which cannot be completely cured, but modern medicine can stop the progression of such diseases, and therefore the development of gliosis itself.
Multiple
Multiple foci of cerebral gliosis are usually found in the diffuse type of this disease. A disease of this form is characterized by large foci of glial growths, which makes the functioning of the nervous system almost impossible.
If with single lesions, the symptoms of this disease are weakly expressed or may be completely absent, then with multiple lesions the symptoms are quite serious and severe .
It should be noted that gliosis of the brain can appear against the background of aging , when neurons in the brain die off. This situation is quite natural; with the help of medications, it is possible to partially restore the functions of the nervous system of an elderly person.
Signs of gliosis
Quite often, the patient learns about the presence of a single focus of gliosis in his brain, by chance, during a routine examination. At the same time, nothing bothers the person. This situation requires special attention.
The patient must be carefully examined and the reason why the lesion formed is identified, that is, the disease that provoked the proliferation of glial fibers. In the case of multiple foci of glia, the situation is different; unpleasant symptoms cannot be avoided.
Symptoms:
- Constant headaches.
- Blood pressure surges
- Dizziness.
- Violation of intellectual activity.
- Loss or impairment of coordination.
- Changes in speech functions.
- Paresis and paralysis.
- impairment .
- Changes in the mental sphere.
- Dementia.
The larger the area of brain damage, the more pronounced the symptoms of this disease.
Is gliosis dangerous?
Gliosis of the white matter of the brain is a very dangerous disease that requires special attention. Even if the focus of brain damage by gliosis cells is small and isolated, it cannot be ignored, since each department of this human organ is responsible for certain functions.
Any violations in this department negatively affect the functioning of the entire vital system.
In the case of multiple lesions, the functioning of the nervous system is completely , the functioning of all parts of the brain suffers, leading the person to complete helplessness.
What does the disease lead to:
- Severe surges in blood pressure.
- Encephalitis of the brain.
- Multiple sclerosis.
- Poor circulation in all organs.
- Complete damage to the central nervous system.
At the first symptoms of this disease, it is necessary to consult a doctor and examine the brain to identify such disorders. There are techniques to reduce the progression of gliosis.
For newborn children, a diagnosis such as gliosis is practically a death sentence .
As a result of genetic mutations, in the fetus, at the age of 5 months , pathological processes in the brain begin to occur, which leads to severe gliosis.
Children suffering from this disease rarely survive to the age of 4 years , although in the first months of their life everything seems to be fine, and the disease does not make itself felt.
Diagnostics and MRI
Diagnosis of cerebral gliosis is based on CT and MRI data:
- Magnetic resonance imaging is a priority method for identifying such abnormalities. Using this method, a specialist will see foci of gliosis in the brain, determine the degree of prevalence and determine the exact cause of the disease.
- Computed tomography can also be used as a way to diagnose gliosis of the white matter of the brain, but this method does not provide such an accurate clinical picture as MRI, and in addition, CT can be irradiated with X-rays, which does not have the best effect on overall health.
Sometimes, for a more complete picture of the disease, it is necessary to conduct additional examination in the form of tests and other manipulations. Always, after diagnosing gliosis, there is a need to treat the disease that provoked the death of neurons.
MRI results
Today MRI is considered the most popular method for studying many diseases:
- In the case of gliosis , usually the MRI report may say “a picture of a gliosis focus in the left (right) frontal lobe.”
- If there are multiple foci , then this technique will reveal all the locations of their localization and the extent of neuronal death.
- Also, a magnetic resonance imaging scanner will determine the cause of such lesions.
- If the culprit for the death of nerve cells is a vascular disease, then the MRI report will say “a picture of single (multiple) foci of gliosis in the white matter of the brain, probably of vascular origin.” Read more about vascular genesis of the brain and what it is in our similar article.
- In addition, a specialist can identify additional abnormalities in the brain, such as hydrocephalus, hematomas and other diseases.
Treatment
currently no effective treatments for cerebral gliosis. This disease is not independent, but occurs as a consequence of the development of another disease. It is necessary to accurately diagnose the cause of nerve cell death and treat it.
If the cause is not identified or ignored, the glial fibers will grow as much as the brain will be affected. This condition is considered serious, and nothing can change the situation.
When this disease occurs in older , it is necessary to take preventive measures to slow down this pathological process.
It is important to reduce blood pressure in a timely manner so that foci of gliosis do not grow.
Preparations:
- Medicines to improve brain activity.
- Drugs that improve blood circulation in the brain.
- Medicines to improve brain function.
- Vitamins , in particular, group B.
Having cured the cause of gliosis, there is no need for therapy aimed at inhibiting neuronal death.
Consequences and life prognosis
Gliosis of the brain cannot be called a minor pathology. This situation requires immediate medical attention.
The prognosis for such patients will depend entirely on the extent of the gliosis process and the diseases that caused it.
Often it is enough to undergo a course of therapy with a neurologist, and the disease will recede. Sometimes treatment can take years without improvement.
Unfortunately,
newborn children suffer from this disease much more severely than adults.
The death of nerve cells in infants progresses rapidly, leading to the death of the child. During routine examinations of pregnant women, ultrasound diagnostics can reveal glial changes in the fetal brain.
In this case, the question of termination of pregnancy .
Prevention
In order to exclude the appearance of gliosis or slow down the process of death of nerve cells, it is first necessary:
- Sport strengthens nervous system , and therefore serves as a method of preventing gliosis. It is enough to perform a small set of exercises every day, and the body will become stronger and more resilient.
- Good rest and sleep have a positive effect on the nervous system.
- You need to establish a daily routine so that your nerves remain strong and diseases in this area do not arise.
- Improve your nutrition by completely eliminating animal fats from your diet. Obesity provokes the death of neurons and, as a result, their replacement with glial cells. The menu of such a patient should consist of healthy dishes.
Required Products:
- Cereals.
- Fruits.
- Vegetables in any form.
- Lean meats.
Frying food is unacceptable; all dishes must be steamed or boiled. Each person must take care of his own health in order to prevent illness.
Such prevention methods will be useful for any person and will protect against the manifestations of such a dangerous disease as gliosis of the white matter of the brain .
21.09.2016
Source: https://mozgvtonuse.com/bolezni/glioz-golovnogo-mozga.html