- How is an MRI of the brain done, how long does the procedure take?
- Features of head tomography of a healthy person
- MRI for microstroke
- Is a stroke visible on an MRI?
- MRI: stroke or multiple sclerosis
- Magnetic resonance imaging of the paranasal sinuses - how to do it
- Magnetic resonance imaging of the head - conclusion
So, why do an MRI? Magnetic resonance imaging of the brain is indicated for patients with various pathologies of the blood vessels of the head, sclerosis, epilepsy, pituitary adenoma, infectious diseases of the nervous system, brain tumors (including in the presence of tumors of the cerebellopontine ganglion), headaches of unknown origin, ENT diseases, neurodegenerative diseases , dementia. It is also necessary to do an MRI of the head to determine the condition of a patient with a traumatic brain injury.
For whom is research harmful or completely prohibited?
As for contraindications, due to the fact that magnetic resonance imaging operates through magnetic fields, which is not harmful to the body, there are very few limitations to the study, but they still exist. Among them it is worth highlighting the following points:
- claustrophobia;
- pregnancy;
- the presence of metal objects and electronic devices in the body.
The examination requires the patient to remain motionless for quite a long time, so conducting an MRI of the brain can be a problem for patients with claustrophobia. In this case, the patient has the right to ask the doctor to use one or another sedative. It is not recommended to do MRI for women in the first trimester of pregnancy - exposure to a magnet can be harmful during the period of the most intensive formation of fetal organs.
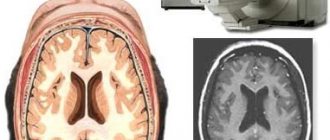
How is an MRI of the brain done, how long does the procedure take?
The tomograph visually resembles a cylinder, inside of which a movable table for the patient is placed. Magnets pass along the inner surface of the cylinder, generating radio waves. They are subsequently converted into signals that are read by sensors, the information is transferred to a computer and displayed on the screen as a series of pictures. The patient is asked to sit on a table, secured with straps so that he cannot move. It is the patient's stationary position that makes it possible to take high-quality, clear images. Magnetic resonance imaging of the brain suggests that a machine that receives radio waves will be attached to the head.
This device is quite noisy, so the patient is asked to wear headphones. If contrast is used during MRI, the nurse inserts a catheter into the vein, through which the substance will flow. The doctor calculates exactly how much of the drug to administer. After the patient is prepared, the table slides into the cylinder, and the tomograph begins to work, and the doctor in the next office reads the data: views and analyzes layer-by-layer images of organs and tissues. This is exactly how magnetic resonance imaging is done - the most informative way to visualize human organs and tissues, which makes it possible to identify the disease in the early stages of development and observe the disease over time. How long does the whole procedure take? A study with contrast generally takes no more than 50 minutes, without contrast – no more than half an hour. In most cases, the patient does not experience any unpleasant sensations during the procedure. An exception is for patients with claustrophobia - they are offered open-type tomographs with holes on the sides. This gives them the opportunity to get rid of the feeling of enclosed space. By the way, open tomographs are also used for very obese patients. The open design allows patients to feel free. Regardless of the type of tomograph, the patient is asked to lie still and even hold his breath at certain moments - this makes it possible to obtain the highest quality images. At the end of the procedure, the table with the patient is pulled out, the nurse removes the catheter, and the patient can return to the department (or home) to his normal life - his condition should not change. If the patient used sedatives, he will remain under their influence for some time, depending on how long the effect of a particular drug lasts and what effect the drug gives. If, after the procedure, the patient experiences symptoms of malaise, dizziness, nausea, itchy skin, there is a high probability of developing an allergy to the contrast agent. In such a situation, it is necessary to notify the doctor as soon as possible: timely information about the problem allows the medical staff to stabilize the patient’s condition as soon as possible.
Video MRI of the brain shows the progress of the procedure using a high-field (closed) machine. Brain MRI results are usually prepared several days after the procedure. The fact is that a radiologist analyzes the tomograph images and makes a conclusion (the analysis takes time), and this conclusion is passed on to the patient and his attending physician.
What types of brain studies are there?
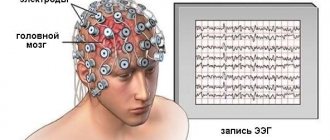
Types of research of the brain and its vessels are different and are divided according to the type of influence that is provided in order to obtain information. Some work using ultrasound, others using X-rays, and others using an electric field. Often several studies are prescribed to get a more complete picture of what is happening in a person’s head.
A study that allows you to determine the physical parameters of the brain is called echoencephalography (abbreviated EchoEG). Such a study is used when it is necessary to determine the presence of a tumor or the consequences of a traumatic brain injury.
If you need to understand how well the brain is supplied with blood, it is worth performing Doppler ultrasound (abbreviated as USDG). This way you can determine how freely blood flows through the vessels of the neck and head. Rheoencephalography gives approximately the same results . It is based on recording changes in electrical resistance of tissues and pulsating vibrations of blood vessels. This method can also identify tumors and other local lesions.
A much more common combination of letters is MRI or magnetic resonance imaging . It is a rather complex study and it is not enough to simply place a person in this apparatus. It is much more important that the researcher is able to correctly decipher the data. The machine does not make mistakes, but a person may not notice something or, conversely, notice the wrong thing. The method is based on the mechanism of nuclear magnetic resonance and is very effective and universal for different types of diseases. He also has a more advanced option - magnetic resonance angiography (abbreviated as MRA). This method allows you to build a three-dimensional model of brain vessels and work with each of them.
Computed tomography (abbreviated CT) is done if it is necessary to examine sections of the brain at different levels. The method involves passing x-rays through brain tissue. As with x-rays of bones, brain tissue has different permeability and this allows you to pinpoint where the damage or abnormality is.
CT scans are performed on such a machine.
There are a lot of research options and complex abbreviations, but often they duplicate each other, are not very effective, or simply are not used due to their narrow specificity. Truly popular and widespread studies are MRI, ultrasound, CT and PET . Let's talk about this in more detail.
Features of head tomography of a healthy person
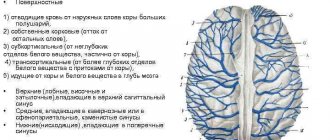
The radiologist describes a healthy brain in the study protocol as follows: All brain structures must be developed correctly, the intensity of the magnetic resonance signal is normal. The ventricular system is developed correctly, of normal size, neither dilated nor reduced. The perivascular and subarachnoid space are normal. The sulci and gyri are normal. The brain structures are of normal size and not displaced. Sella turcica, pituitary gland without pathology. The eye sockets, nasal sinuses, and ear canals are of normal size and shape, without signs of pathology. Brain tissues do not have focal or diffuse changes. If contrast was used, the brain vessels are developed correctly and are evenly filled with contrast agent.
What are positive MRI results:
- Normal arrangement and “consistency” of tissues;
- Absence of abnormal formations (“plus-shadow”);
- There are no bleedings, purulent accumulations, blood clots, or arteriovenous malformations.
What does an MRI of the brain show: normal?
Normal MRI of the brain is rare. All radiation methods should be used only after alternative methods have been performed. A patient is sent for examination with suspicion of one or another pathological process. Low frequency of normal results – consequences of eating fatty foods, prolonged exposure to a polluted environment.
The study is carried out in several projections (coronal, sagittal, axial). It is possible to use contrast enhancement by intravenous contrast. A qualified specialist selects the type and method of performing an MRI of the brain before the start of the study. Signal processing is carried out using a proprietary program. With its help, the doctor has the ability to visualize images from different angles. 3D modeling has only recently begun to be used during the procedure, but the technology allows for a clear study of the anatomical area from all sides. After introducing the simulation, doctors concluded that the absolute norm is not achievable. Each patient exhibits some deviations from the classic anatomical structure of the brain.
Software, coils
According to Vesta, MRI allows you to see what remains behind the scenes of X-rays. At the same time, a picture with fractures of the vertebra and sacrum is displayed on the screen of the doctor’s workstation. “This injury is not visible on an x-ray taken at the clinic,” explains our interlocutor.
In addition to the technical part, a set of programs for research and data analysis has a direct impact on the diagnostic process.
The device takes an image in three planes: coronal (along the body in front
MRI for microstroke
Very often, a microstroke is easier to identify from the outside than on your own (because people sometimes ignore their symptoms), so what symptoms of a microstroke appear first:
- the person suddenly, for no reason, fell silent and began to speak incoherently (the photo shows the main symptoms of a mini-stroke);
- you are forced to ask him again several times;
- he does not respond to your questions, looks confused, in prostration;
- suddenly drops an object that was previously held tightly;
- It’s not on the first try that you manage to lift that object;
- suddenly begins to stutter;
- movements resemble a person who is intoxicated.
What to do when the first signs are identified When the first symptoms and signs of a microstroke are identified, it is necessary to provide the patient with complete rest. If possible, place him on high pillows (so that his head is in an elevated position).
How to minimize the consequences
Prognosis and consequences regarding further human conditions directly depend on the causes and symptoms of a mini-stroke. If the cause is more superficial (for example, stress, obesity), then most likely, eliminating negative factors will be the best prevention of further micro-strokes and possible stroke. However, if the cause of a micro-stroke is a consequence of a certain disease, then it is worth choosing additional comprehensive treatment. It has been proven that even one minor stroke is an indication of the possibility of a major stroke in one out of ten cases. And many people know about the consequences of a massive stroke - this is irreparable damage to health. Or death. Get examined by a doctor in a timely manner to prevent relapse or the development of complications! The first micro-stroke tells us that we need to be more attentive to the body.
Video: How not to miss a micro-stroke? A microstroke does not cause significant harm, but it does indicate difficulties within the body. What are the consequences of the attack in the future?
An MRI of the cervical spine and head may not show a stroke in the acute period if standard classical research protocols are used, although even with classical protocols, MRI in diagnosing a stroke reveals changes much faster compared to CT (computed tomography). This is a T2 MRI image of a patient who showed neurological symptoms two hours ago. Conclusion is the norm. The same patient who underwent diffusion-weighted and perfusion MRI scans. Lesion in the basin of the right middle cerebral artery. The patient was prescribed intensive therapy.
What does an MRI show after a stroke?
On MRI sequences such as PD/T2WI (proton-weighted imaging) and FLAIR (fluid attenuation inversion recovery) MRI sequences appear to be high intensity signal from a lesion. MRI sequences such as PD/T2WI (proton-weighted imaging) and FLAIR (fluid-attenuated inversion recovery) detect up to 80% of strokes with first-onset symptoms within 24 hours.
In up to 30% of cases, for the first time 2-4 hours after the onset of symptoms, these sequences may not detect a stroke, then DWI (Diffusion weighted imaging) comes to the rescue. The high signal on these classic MRI sequences is the result of irreversible brain damage—cell death. A high signal is very bad news, indicating the death of brain tissue.
Who is conducting the research?
After the patient receives a referral for an MRI of the brain, he signs up for the study. It is performed not by the attending physician, but by a radiologist. This person has a higher medical education and has completed training courses to conduct MRI. Therefore, it is fundamentally wrong to consider him simply an operator of a complex device.
Before starting the examination, the radiologist carefully examines the patient’s medical history and once again asks him to tell about the complaints that led him to the MRI. Then he talks about how the scan is performed, what the person will hear and see, and what precautions must be taken.
With all the advantages of MRI, it also has contraindications.
Information about a suspected diagnosis obtained from the anamnesis helps the radiologist to correctly set the device settings and select the scanning mode.
A nurse assists the radiologist. She will insert a catheter into a vein in your arm and inject a contrast agent if necessary. Together with the doctor, she will monitor the patient's condition during the scan.
When the test is completed, the nurse will remove the catheter from the vein and help the patient get up and get dressed if he needs her help. The patient will then be asked to wait in the hallway for their exam to be transcribed. The results will be ready in about 15-20 minutes, depending on how many different pathologies the radiologist saw. You won't have to wait long for results.
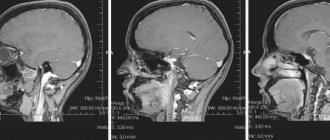
Is a stroke visible on an MRI?
Stroke is always visible on MRI, and according to the recommendations of the World Health Organization (WHO), the World Association of Neurologists (WAN) is the “Gold Standard” in identifying any type of stroke. The radiologist, after receiving the data on his personal computer, evaluates the anatomical changes of the brain. Since the data from the first study is saved to disk and printed on film, the attending neurologist after treatment can evaluate the prescribed therapy and raise the question of correcting drug treatment, which is very important for the patient’s future quality of life. In a patient even with sparse neurological symptoms, lesions are detected on classical MRI sequences.
Hemorrhagic stroke MRI
Hemorrhagic stroke occurs in 15% of all strokes. Hemorrhagic stroke is an acute cerebrovascular accident (CVA), and as a result, the release of blood from a cerebral vessel into the brain substance. This pathological condition is possible in the following cases: when a person has high blood pressure and the brain vessel cannot withstand it, its wall ruptures. “sweating” of the vascular wall with cellular elements of the blood is less common. Types of hemorrhagic stroke.
- parenchymal hemorrhage (blood in brain tissue).
- subarachnoid hemorrhage (blood in the pia mater).
- subdural hemorrhage (cause: trauma. Blood in the subdural space).
- epidural hemorrhage (cause: trauma. Blood in the epidural space).
Since the main substrate of pathology is blood that has left the normal course, then with MRI, depending on the “age” of the blood, we will see characteristic changes. Blood leaves its usual channel into the brain tissue. Hemorrhagic stroke: increased signal on T2 sequence in the left hemisphere.
Stroke on MRI
On MRI after a stroke in the acute period (1-7 days after the development of stroke symptoms), pathological foci are clearly identified and delimited from normal brain tissue. On the T1 sequence, the ischemic zone appears as a hypointense signal, and on T2, on the contrary, a hyperintense signal. Edema around this lesion and mass effect (displacement of the brain towards the normal brain) are also visualized. On MRI in the subacute period (7-21 days after the development of stroke symptoms). Resolution of edema (reduction in size), the infarction zone still appears as a hypointense signal, and on T2, on the contrary, a hyperintense signal. On MRI in the chronic period (more than 21 days after the development of stroke symptoms). Swelling is completely resolved. The infarction zone still appears as a hypointense signal, and on T2, on the contrary, a hyperintense signal. Expansion of the cortical grooves of the brain, expansion of the lateral ventricles.
MRI signs of stroke
Diffusion-weighted image: infarction in the left middle cerebral artery, stroke in the right middle cerebral artery. The hyperintense signal in this case indicates the most acute period of the stroke. Stroke in the left hemosphere of the pons. A clear delineation of normal brain tissue from the affected brain tissue is visualized along the midline. Ischemic stroke MRI - there are five main periods of completed ischemic stroke:
- Early recovery;
- Late recovery;
- Remote.
In ischemic stroke, MRI shows, respectively, the ischemic zone, that is, a deficiency of blood supply in a certain localization of the brain in the early period and in the late period - necrosis of part of the brain (zone of cerebral infarction). In addition to these pathological changes on MRI, it is possible to establish the cause of the hemorrhage, namely: if it is an atherothrombotic ischemic stroke, MRI images of the brain visualize a blood clot, a narrowing of the lumen of a brain vessel with cholesterol plaques. MRI and lacunar stroke Lacunar stroke is a type of ischemic stroke of the brain, characterized by limited small foci of the brain (up to 2.0 cm), which formed as a result of blockage of one of the small arteries of the brain and resolved over time into a cyst (lacuna).
Signs that are detected on MRI:
- Unilateral pontine infarction has a sharp midline demarcation.
- Increased intensity or density at the end of the acute or at the beginning of the subacute stage
- Small, discrete, low-density/diffusely limited lesions 3-20 mm in diameter, usually 10 mm in diameter
- The signal from the lesion is more intense compared to the signal from the cerebral fluid.
MRI for stroke - what will show, why
Stroke is a pathological condition characterized by acute cerebrovascular accident (ACVA), which is manifested by the appearance of focal or cerebral symptoms that persist in the patient for more than 24 hours or lead to the death of the patient. MRI for stroke “shows” the ischemic zone (in ischemic stroke), lacuna (cyst in lacunar infarction) or blood saturation of brain tissue (in hemorrhagic stroke). What the MRI shows is important for choosing the right treatment. The earlier adequate correct therapy for stroke is started, the higher the patient’s quality of life in the future. MRI of the brain, stroke When a stroke occurs, irreversible changes occur, which can always be diagnosed after performing an MRI. MRI is able to recognize any stroke, clarify the cause of its occurrence, its age, and is able to identify which parts of the brain are affected. All this further contributes to the appointment of correct treatment. MRI, as noted earlier, always shows a stroke. This statement is confirmed from the standpoint of evidence-based medicine. MRI examination is recommended by both the World Health Organization and the World Association of Neurologists. Since the development of medical physics does not stand still, such phenomena as diffusion and perfusion are also applicable to MRI. It is with the help of diffusion-weighted imaging (MRI scanning mode) that changes in the brain are detected minutes after the onset of stroke symptoms.
Tested for myself
Tomography is equipped with an ultra-high-field Siemens Magnetom Spectra 3 T. The unit cannot be called lightweight: its weight in running order is about 7.3 tons with a tunnel length of 173 cm. The system allows the use of up to 120 coil elements to cover the entire anatomical zone (for example, throughout the central nervous system). Siemens proprietary software is used, which primarily affects the quality of the scan and the final image with slices 0.5-1 mm thick.
MRI: stroke or multiple sclerosis
It is almost impossible to distinguish MRI images of stroke and multiple sclerosis from each other. Because stroke is a sudden disorder, multiple sclerosis is an autoimmune “sluggish” disease that affects brain tissue for years (people live with lesions of multiple sclerosis in the brain for more than 40 years after discovery).
What do pathological changes look like on the pictures? In the picture it looks like a lighter, asymmetrical spot with jagged edges (since the picture is a negative, doctors call it a darkening). The formation can deform and displace other structures (ventricles, subcortical centers). Tumor growth, as a rule, is accompanied by the rapid development of additional vessels in the affected area, so contrast is used to analyze volumetric processes.
With the development of an ischemic stroke, a zone of brain hypoxia appears; on an MRI of the head it will appear lighter in color, but unlike a tumor, the spot will correspond to the area of innervation of one of the cerebral arteries. With contrast, blood supply to the stroke area will be reduced. The smoothness of the furrows and convolutions above the affected area can be determined.
What is the brain
The brain is one of the main topics of modern medicine. You can fight diseases that affect the body as much as you like, but diseases that affect the brain are much worse. Often they do not cause any pain, but they are the ones that prevent a person from living a normal life, sometimes even changing his personality.
This is because we are the brain. A person is not a body - the body is only a tool . The entire essence and personality are contained in the brain. You can say that this is just a set of proteins or a repository of the soul, but in any case, if you replace a person’s kidney or heart, he will remain himself, and if you imagine that you can replace his brain, then what will be left of him? A set of muscles, bones and organs - that's all.
That is why the brain must be maintained in a normal state in order to minimize the risks of its premature damage. It also needs to be examined and tested in order to understand whether it is working correctly and whether it needs help in some way. One of the main studies is a brain scan, which is done using ultrasound. But this is not the usual ultrasound that is done when checking the internal organs of the abdominal cavity.
What can an MRI of brain vessels show in multiple sclerosis?
It is characterized by the formation of zones of white matter - nerve fibers that lose their myelin (outer) layer. The tomogram shows focal formations that accumulate contrast differently depending on the stage of the disease. The lesions appear as light areas and can be located in all parts of the white matter. Their number can vary greatly: from one to dozens. In the initial stage of the disease, if only one lesion is detected, it can be mistaken for a small space-occupying formation. Unlike cancer, lesions in multiple sclerosis do not deform surrounding structures.
Hydrocephalus (dropsy). Normal and hydrocephalus Dilation of the cavities of the ventricles, subarachnoid, perivascular space. Severe forms may be accompanied by compression and atrophy of the cortex and subcortical formations of the brain.
Congenital developmental anomalies Serious anomalies in brain development, as a rule, are detected in the prenatal period or in the first months of a child’s life. If the anomaly does not cause a significant loss of any body function, then it can only be detected by chance, during an MRI, which is planned for another purpose. Just as no two people are identical, different people cannot have two absolutely identical tomograms. Therefore, only a specialist with sufficient experience and qualifications can evaluate the MRI result. You should not look for abnormalities in the images yourself, since not even all doctors know how to do this correctly. Also, you should not independently analyze the description of the study, since many different abnormalities can be detected in a healthy person, but such findings are not clinically significant.
Who needs to be able to interpret MRI results?
When deciphering MRI images, the indicators of a particular study are compared with normal sections of a healthy brain. Different fabrics in the pictures have different degrees of staining. The lightest is the white substance. The gray looks a little darker. The bones will be the darkest.
An experienced specialized doctor or radiologist specializing in computed tomography and magnetic resonance imaging images can correctly interpret the MRI results.
To do this, he must have in-depth knowledge of the structure of the brain, understand all its components, know their sizes, and understand what tissue they are made of. The specialist must have knowledge of physiology and pathological anatomy.
The patient himself will not be able to cope with such a complex task; in most cases, it is not worth even trying to decipher an MRI image on his own. Moreover, the diagnosis is often made jointly by the radiologist and the attending physician.
Decryption is carried out in a certain sequence:
- The tomograph sends the results to the computer. The brain is examined in 4 projections.
- The photographs are printed.
- The specialist mounts the photographs on a special backlit stand.
- The doctor examines the images in detail and also compares them with the norm.
- The radiologist writes a report, which is given to the patient. It indicates the state of all brain tissues and their shape. There must be a conclusion about whether there are pathologies.
It is extremely important to ask your doctor questions. If there are certain changes, he should tell as fully as possible what brain structures they affected, what they could lead to, and what they are connected with.
It is possible that the study will need to be completed several times. This way the doctor will be able to observe the dynamics of the process, the speed of progress of changes. In this way, it is possible to evaluate the benignity or malignancy of changes, the results of treatment of blood vessels, and their condition.
Magnetic resonance imaging of the paranasal sinuses - how to do it
With the introduction of a contrast agent, the study takes much longer than without it. Also, the specialist must be qualified in the administration and diagnosis of its use. When the patient is stationary in the tomograph cylinder, the device takes pictures of the paranasal sinuses from different angles in several projections. The examination lasts 15-20 minutes; if a contrast agent was used, the examination time is 30-50 minutes. The device produces noise and hum while diagnosing a patient. Before the study, it is necessary to have a conversation and talk about the unpleasant sound. If necessary, you can offer the patient sedatives and secure the limbs with straps built into the device. During the MRI process, the patient is alone in the room. A medical worker monitors his condition and the quality of the images from an adjacent room.
The frontal and maxillary sinuses are located superficially, so for diseases of frontal sinusitis and sinusitis, an MRI appointment will be an unnecessary luxury. The best research option would be the least expensive x-ray of the paranasal sinuses. However, only MRI can reveal the cause and type. The sinuses of the ethmoid labyrinth and the canals of the sphenoid bone are located deeper and are more complex, because of this it is possible to identify changes using layer-by-layer research methods - CT and MRI. An experienced otolaryngologist prescribes a current sinus examination based on the nature of the disease. By contacting a good specialist, you will save not only money, but also your precious health. During a magnetic resonance imaging study, you can view the mucous membranes of the nose. It is also good to diagnose nasal polyps and the labyrinth of the sphenoid void. The test helps specialists distinguish which bacteria are causing the disease and rule out sinusitis caused by fungi. What does MRI of the paranasal sinuses show? Interpretation of the results The photographs clearly show the existing pathologies, inflammatory processes or neoplasms in the paranasal sinuses. In the process of magnetic resonance therapy it is possible to diagnose:
- Nasal bone disease
- Inflammatory process in the paranasal sinuses (sinusitis, frontal sinusitis, sphenoiditis, ethmoiditis)
- Formed cysts or polyps
- Chronic diseases
- Incorrect structure after injury
Upon completion of magnetic resonance imaging, the images are interpreted by a radiologist, who confirms or refutes the diagnosis of the attending physician. The patient is given a conclusion, photographs and a disk (which can be viewed on a home PC).
The description of the conclusion is about 20 minutes. MRI of the sinuses during pregnancy MRI in the 1st trimester is prohibited. During a magnetic resonance imaging study, a pregnant woman's body is exposed to a strong magnetic field. It is strictly not recommended to perform diagnostics in the first trimester. The fruit begins to form during this period. From the second trimester, doctors also do not recommend MRI, but in special cases it is still allowed and only as prescribed by the attending physician. Under the influence of noise and heat emitted from the device, the woman will experience anxiety, which will adversely affect the child. If possible, it is better to postpone the diagnosis before the birth of the child and before the mother feeds him with breast milk. Research during lactation is also prohibited.
Are there any tasks that are frankly difficult for a tomograph?
— When examining the abdominal cavity, for example, and if we work in automatic mode, the device adapts to the movement of the diaphragm, reading data at a certain position. This significantly increases the research time. The process can be sped up, but the patient will have to hold their breath for 20 seconds many times. Physically it's not easy.
There are no restrictions for the device when it is fully equipped with coils. For example, we do not yet look at the heart or conduct examinations of the mammary glands. But this year the necessary components will be purchased.