An x-ray will help you understand how far the disease has progressed. The stages of rheumatoid arthritis are visible on it, but only a specialist can accurately determine the problem. In the later stages, almost anyone can determine the presence of a problem by appearance - deformation of organs occurs. However, there are changes that are not visible to the naked eye.
This:
- Reducing joint spaces;
- Erosion of bones (that is, their thinning, the appearance of “dips”);
- Ankylosis (bones fusion with each other).
But since there are so many diseases of bones and joints, one x-ray is not enough to diagnose and determine the stage of rheumatoid arthritis. A good doctor will supplement this with a blood test.
Tests in addition to X-rays
To diagnose rheumatoid arthritis, tests are done for markers of inflammation (that is, markers that show that the body is fighting it) and rheumatoid factor. However, it is important not only to do the analysis, but also to interpret it correctly.
Analysis for inflammatory markers. If the result is positive, this may be an indication of some other disease, not necessarily arthritis. Which one exactly will be revealed by further research.
Analysis for markers of rheumatoid arthritis. It is worth diagnosing with great caution, because it occurs in 5% of healthy people (and indicates a predisposition to the disease, but not the disease itself), and it does not occur in approximately 50% of patients. That is, it is only indirect evidence of the presence of rheumatoid arthritis.
Therefore, tests for other diseases are also necessary. If, as a result of the examination, no other pathogens are found, and the x-ray indicates pathological changes, the doctor diagnoses “rheumatoid arthritis”.
Principles of treatment at various stages
Treatment of rheumatoid arthritis with massage courses
There is no standard treatment regimen for arthritis that is suitable for every patient. When prescribing therapy, the doctor relies on the symptoms of the pathology, the patient’s age and his general condition. X-ray examination is mandatory as it helps to accurately determine the stage of the disease. The principle of treatment will depend on the stage.
Features of treatment at stage 1:
- Limit physical activity and heavy lifting. It is allowed to perform a special set of exercise therapy exercises to speed up the treatment process. Gymnastics time should not exceed 40 minutes.
- People who find it difficult to perform a set of exercises should spend 30 minutes walking every day.
- Treatment involves preventive measures, since it is difficult to accurately confirm the presence of arthritis.
- If the knee joint is damaged, it is recommended to wear a brace.
- It is recommended to go swimming, but not to overload the body with physical activity.
- Medications are not prescribed at this stage. In case of severe pain, it is allowed to take painkillers.
Features of treatment at stage 2:
- Therapy is based on basic treatment. The drugs are prescribed by the doctor taking into account all the individual characteristics of the patient.
- In addition to basic medications, folic acid is recommended.
- The interval between examinations should not exceed 6 months.
- To relieve pain, NSAIDs are prescribed.
- It is imperative to perform physical exercises that will help avoid complications and slow down the progression of rheumatoid arthritis.
- Some patients are prescribed sanatorium treatment, which includes physiotherapy, mud baths and balneotherapy.
- To relieve pain and discomfort, as well as get rid of swelling, a massage course is recommended.
Features of treatment at stage 3:
At stage 3 it is not always possible to achieve recovery. Therapeutic measures are aimed at stopping the further development of arthritis.
- Therapeutic exercise, walking and physical therapy are also necessary, as in the previous stages.
- For severe pain that is not relieved by non-steroidal anti-inflammatory drugs, glucocorticosteroids are prescribed.
- Drugs from the basic group are selected individually; at stage 3, their dosage can be increased.
- It is possible to prescribe hormonal medications, which are taken either orally or injected.
- Persistent deformities are an indication for surgical intervention.
- In severe cases, it is advisable to take genetically engineered biological medications.
Features of treatment at stage 4:
The last stage is the most difficult, and it is almost impossible to achieve a complete recovery. At this stage, all measures are aimed at achieving stable remission and preventing complications.
- Treatment with basic drugs involves increasing the dosage.
- Glucocorticosteroids are injected into the joints themselves. This allows you to get rid of pain.
- In some cases, with severe pain, the use of narcotic painkillers is considered.
- Physiotherapeutic measures are taken regularly, without interruption.
- If possible, large joints are replaced with prostheses.
- Treatment begins in a hospital setting.
At the last stage, arthritis can cause serious complications, and in rare cases, disability is possible. Timely examination and treatment will help avoid these problems. Even when the disease goes into remission, treatment is not canceled, and the dosage of the drugs can be adjusted.
What does the lack of timely diagnosis using X-rays lead to?
Some people believe that due to their young age they cannot get rheumatoid arthritis, especially in the advanced stages. And this is a big mistake, because the disease is rapidly growing younger and occurs in those who are only 30 or 20 years old. The reasons are trivial - environmental degradation, unhealthy diet, sedentary lifestyle.
Heredity plays a big role. If there are people in your family who have had or are suffering from rheumatoid arthritis, the appearance of its symptoms is a very alarming symptom.
Description of the pathology
By the nature of its occurrence, rheumatoid arthritis is classified as a chronic autoimmune disease that occurs as a result of failures of the human body’s immune system. It is still difficult to establish the causes of this disease, but the factors that could trigger its development are the following:
- past infections (measles, hepatitis B, mumps),
- heredity,
- constant harmful effects of harmful substances,
- other diseases associated with dysfunction of the human immune system,
- menopause
Rheumatoid arthritis can be judged if inflammation occurs in the joints of the legs and arms (shoulders, elbows, hands, hips, knees, feet). There are certain radiological stages of rheumatoid arthritis. More on this later.
What signs of rheumatoid arthritis are visible on x-ray?
On an x-ray, the doctor can see various signs of the disease that are not noticeable at first glance and examination. An x-ray is taken of the part of the body in which the patient complains of pain. Rheumatoid arthritis can be concentrated in one part of the body or affect them all at once (hands, toes, knees, shoulders, elbows). Most often the problem begins in the extremities.
X-rays show erosion and inflammation. How strongly they will be expressed depends on the stage of the disease.
About the article
For citation: Smirnov A.V., Karateev D.E.
Stages of radiological changes in joints in rheumatoid arthritis // RMJ. 2014. No. 7. P. 551 The osteoarticular system of the hands and distal feet is the main object of study for diagnosing and determining the stage of rheumatoid arthritis (RA) and conducting a differential diagnosis with other diseases of a rheumatic and non-rheumatic nature.
The synovial membrane of peripheral joints is the target organ where chronic autoimmune inflammation develops in RA, which subsequently leads to multiple and symmetrical joint damage characteristic of RA. The symmetry of changes in the joints of the hands and feet is a distinctive feature of RA. Typical signs of RA are symmetrical damage to the metacarpophalangeal and metatarsophalangeal joints, wrist joints, and proximal interphalangeal joints of the hands. The first radiological symptoms of arthritis, including the appearance of the first erosions, can be detected in the 2nd and 3rd metacarpophalangeal joints, 3rd proximal interphalangeal joints of the hands, joints of the wrists, wrist joints, styloid processes of the ulnas, 5 x metatarsophalangeal joints. In more advanced stages of RA, changes may be detected in the distal interphalangeal joints of the hands and feet. RA never begins with damage to the distal interphalangeal joints of the hands and feet, or the proximal interphalangeal joints of the feet.
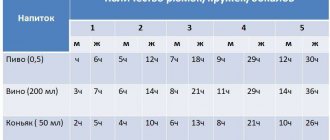
Most often in everyday practice, a radiological classification is used, based on dividing RA into modified Steinbrocker stages using plain radiographs of the hands and distal feet in a direct projection.
There are 4 radiological stages of RA, reflecting the progression of symptoms of arthritis in the joints of the hands and distal feet.
Stage 1 (early radiological changes) of RA includes periarticular thickening and hardening of soft tissues, periarticular osteoporosis (increased radiolucency of bone tissue), single cyst-like clearing of bone tissue and narrowing of individual joint spaces in joints typical of initial RA. X-ray symptoms of stage 1 are nonspecific for RA and can be detected in other rheumatic diseases, which requires mandatory consideration of clinical and laboratory indicators of the disease.
Stage 2 is characterized by an increase in periarticular osteoporosis, the appearance of multiple cyst-like clearings of bone tissue in the epiphyses of short tubular bones and carpal bones in combination with multiple narrowing of the joint spaces, erosive changes in the joints and slight marginal deformations of the bones. This stage is divided into non-erosive and erosive forms depending on the absence or presence of destructive changes in the joints. As a rule, the first erosions appear in the 2–3 metacarpophalangeal, 5 metatarsophalangeal joints, carpal bones, and in the area of the styloid process of the ulna. A distinctive feature of the 2nd stage of RA is the absence of moderate or severe deformation changes, subluxations, dislocations and bone ankylosis of the joints.
Stage 3 is characterized by an increase in radiological symptoms detected in stage 2. Destructive changes are pronounced and are detected in many joints of the hands and distal parts of the feet. Predominant in joints typical for RA. A distinctive feature of the 3rd stage is moderate and severe deformations of the epiphyses of bones, subluxations and dislocations in individual or many joints.
Stage 4 is characterized by stage 3 symptoms and the appearance of bony ankylosis of the joints. Ankyloses in the joints of the wrists (intercarpal, 2nd–5th carpometacarpal joints) are typical for RA. Ankyloses are extremely rarely detected in the proximal interphalangeal joints of the hands and wrist joints. Severe destructive changes in the bones of the wrists can lead to collapse of the wrists, which is characterized by a decrease in the height of the wrists, severe deformities, reduction in size, or osteolysis of the wrist bones. Osteolytic changes can be detected in the metacarpophalangeal and, less commonly, metatarsophalangeal joints. Radiological stages of RA are presented in Figures 1–11.
Determining the stages of rheumatoid arthritis using x-rays
Doctors have their own requirements for how to make a diagnosis, which they follow. For example, the stage of rheumatoid arthritis is determined by the joint that suffered the most, judging by the x-ray.
That is, if damage to the joints of the legs corresponds to stage 2, and to the joints of the arms to stage 4, then the patient will receive a diagnosis of stage 4. In itself, it is very difficult, but since this concerns not the whole body, but its individual parts, the situation is not as hopeless as it might seem at first glance.
Of course, all this cannot be done by a non-specialist, but with appropriate training a person can roughly understand the condition of the joints. However, to make an accurate diagnosis and determine the stage, a doctor is needed. If there are doubts about the doctor’s qualifications (he is not interested in treatment, he prescribes only ointments and/or tablets), you can show the same x-ray to another specialist.
Stages of the pathological process according to Steinbrocker
X-rays of the hands, knees, hips and ankles can determine the stage of development of the disease. Thanks to the image, the doctor can assess the condition of the surrounding tissues, the degree of damage to the joints and bones.
This procedure is important in the diagnosis of rheumatoid arthritis; among all imaging methods, it is performed first.
httpv://www.youtube.com/watch?v=embed/9kvcM0Zvfoo
httpv://www.youtube.com/watch?v=embed/9kvcM0Zvfoo
This disease is based on autoimmune inflammation, leading to the development of vasculitis and catabolic disorders.
There are 4 stages of rheumatoid arthritis. They reflect the progression of the disease in the joints and the degree of damage to bone tissue.
What do the stages of rheumatoid arthritis look like on an x-ray?
The first stage is the easiest, but even it can be seen in the picture. As already mentioned, rheumatoid arthritis most often begins in the extremities, so photographs are taken of the hands where changes occur. Signs of the first stage of arthritis:
- The soft tissue around the affected joints is thickened;
- The bones themselves are more porous, even, one might say, loose;
- The joint space is narrowed, but still weakly.
At this stage, a person feels that it is more difficult for him to move his limbs in the morning. There is slight swelling. These two symptoms are enough to start sounding the alarm and taking an x-ray. Moreover, symptoms can appear in both adults and children. Pain may be added to limited mobility in the morning. If rheumatoid arthritis is diagnosed early at a young age, you can avoid its rapid development in adulthood and old age.
Second stage. Cysts are added to existing symptoms. These are growths on bone tissue that deform the arm and further limit its mobility. The joint gap becomes even smaller. Osteoporosis (fragility and looseness of bones) is on the rise. This is what is seen on an x-ray. But in real life, mobility decreases and pain manifests itself not only in the morning, but also during the day.
It is important to note that the second stage is divided into 2 types - 2A and 2B. At stage 2A of rheumatoid arthritis, there is still no erosion in the image - pronounced bone damage, but at stage 2B they already appear. The most common type of erosion is marginal, that is, along the border of the joint.
The most vulnerable areas are those where the cartilage does not cover it. Another type is the failure of a section of bone, this is called compression erosion. The third type is destruction of the endplate (it connects the ligament to the joint). And if only a very good specialist can determine stage 1 rheumatoid arthritis by x-ray, then even an average doctor should be able to handle stage 2. In real life, the patient suffers from pain during exercise.
The third stage of rheumatoid arthritis on x-ray is characterized by a large number of erosions, namely more than 5. The doctor also notes that the muscles atrophy due to rheumatoid arthritis, as a result of tissue damage and limited mobility of the organ. The interarticular spaces are still narrower. Subluxations and dislocations of the joints appear, they are already visually deformed.
In the soft tissues near the diseased joints, in the photographs you can see nodules that form from calcium salts. This is called calcification. The nodules not only contribute to the progression of the disease, but also cause pain when touched. This is about x-rays. But in real life, a person already has to make significant efforts to perform the simplest everyday operations.
This stage is especially painful for those who engage in sports or physical labor, as it deprives them of the opportunity to have a full load.
All the signs that were mentioned in the description of the previous stages are present in X-ray 4, but to a more pronounced degree. New ones are also appearing.
Erosion. At stage 4 of rheumatoid arthritis, on x-rays they are visible not only on the joints, but also on the bones. The joint spaces narrow so much that bone fusion occurs (ankylosis). Osteophytes appear. Roughly speaking, osteophytes are growths along the edges of joints. They have different shapes. At first they are small, and then they grow larger and larger.
Classification of the disease by radiological stages
The pathogenetic mechanism for the development of rheumatoid arthritis is an autoimmune cross-reaction. The antigenic structure of hemolytic streptococcus, belonging to group B, is similar in structure to the connective tissue of the human body.
When infected with a microorganism (acute or chronic tonsillitis, pyelonephritis, intestinal pathology), the produced antibodies may damage one's own tissues. The joints are the first to suffer. With each new rheumatic attack, the affected area expands and the changes become irreversible and severe.
In the early stages, at the first signs, changes may not be detected on an x-ray. But the further the process progresses, the more obvious the damage becomes. There are four radiographic stages of pathology.
The first stage is characterized as the easiest, the changes are reversible and treatable. Clinically, the patient complains of morning stiffness in the movements of the hands, swelling is visually noted in the area of the small joints of the fingers. More often, the symptoms are associated with a recent infectious pathology (sore throat, tonsillitis, urinary tract infection, streptoderma, etc.).
The small joints of the hands and feet are the first to suffer. X-ray signs of the first stage of rheumatoid arthritis:
- predominant inflammation of the soft tissue component, which has the form of compaction of structures above the affected joint;
- slight narrowing of the interarticular space, which is not visualized on an x-ray;
- initial manifestations of osteoporosis in the form of local clearing of bone structures and loosening of only the articular surfaces.
Clinically, the second stage manifests itself in the form of severe stiffness of the hands for several hours, mainly in the morning and evening. The changes are more pronounced, manifested in the form of swelling and visible deformation, manipulative movements of the hands are significantly difficult (it is difficult for the patient to thread a button into a buttonhole, a thread into a needle, or tie shoelaces).
In the area of the joints, a compaction is palpated, skin manifestations in the form of rheumatoid nodules are often associated, the skin over them is hyperemic. Pain in the legs is acute, walking is difficult, and lameness is observed.
The second radiographic stage of the disease is divided into two subgroups, depending on the degree of damage in the form of erosion of the articular surface:
- subgroup A of the second radiological stage is characterized by the absence of erosions on the articular surfaces; the image reveals periarticular osteoporosis in the form of cysts (local clearing of bone structures), areas of bone compaction and a more noticeable narrowing of the gap between the articular surfaces;
- subgroup B of the second radiological stage of the pathology, in addition to the main manifestations, is characterized by the appearance of erosions of the surfaces of the joints, in no more than four places.
Clinically characterized by complete immobility of small joints. The pathology extends to large ones: wrist, elbow, knee, ankle, upper shoulder girdle and even intervertebral joints in rare cases. The patient experiences difficulty walking due to severe pain and stiffness of the knee joints.
Bones become fragile due to a pronounced degenerative process. Cases of subluxations, dislocations, and pathological fractures are becoming more frequent. Healing of damage takes a long time and requires surgical interventions.
Third degree of rheumatoid arthritis on x-ray:
- formation of a single bone block in the area of small joints of the hands;
- more than 5 areas of bone tissue erosion;
- narrowing of the joint spaces of small and large joints;
- the appearance of osteoporotic cysts;
- the formation of soft tissue calcifications (rheumatoid nodules), which in the image appear as rounded areas of darkening, up to 2 cm in diameter, in the area of the soft tissue component around the joints (usually the hands, elbows, knees).
The terminal stage of the rheumatoid process, which irreversibly disables the patient. Performing simple everyday activities is impossible due to severe pain and persistent joint contractures (immobility). The patient's muscles atrophy due to lack of movement. A person cannot take care of himself (eat, go to the toilet) and requires regular assistance.
Based on the results of radiography of the joints, the following changes are revealed:
- absence of joint space with compaction in the articulation area and the formation of ankylosis (joint contractures) and subchondral osteosclerosis (due to increased friction of cartilaginous structures in the absence of joint space, they calcify and sclerosis, become dense, lose shock-absorbing capabilities);
- bone growths are formed on the articular surfaces - osteophytes, which have a pointed shape;
- osteoporosis can develop into osteonecrosis.
How to recognize rheumatoid arthritis on x-ray
To understand that the X-ray shows exactly the signs of rheumatoid arthritis, you need to know how to interpret the image. Let's look at what certain signs look like on an x-ray.
Tissue compaction around the affected joint. This symptom is visible even in photographs of stages 1 and 2 of rheumatoid arthritis. The tissue around the diseased area appears smoother than that around the healthy area. They are also more transparent.
Calcifications. These are the nodules discussed above. On x-rays they simply appear as shadows or round formations. The shape does not need to be round. In rheumatoid arthritis, they can be in the form of dashes or small formations on the edge of the joint. Moreover, their density can also be different.
Some are just forming, while others are bone-like in density. Calcifications are more clearly visible on an MRI image.
Tendinitis and tenosynovitis. This is a hardening of a tendon or ligament where it attaches to the bones. This process is also visible on x-rays. An additional sign is calcifications around such compactions.
Osteoporosis. The actual destruction of the bone, increasing its fragility and weakness. Osteoporotic areas of the bone/joint appear to appear more transparent. The endplates appear thinner.
Narrowed joint space. It is possible to determine that it is narrowed due to rheumatoid arthritis only if there is a similar photograph of the healthy arm. The doctor can do this without such an image, since he knows exactly what the ratio should be. However, in later stages, even a non-specialist can see that the gap on the x-ray is significantly narrowed.
Unevenness of the articular surface. These can be both failures and growths. In the first case we are talking about erosion, in the second - about osteophyte. Osteophytes have different shapes on x-rays in rheumatoid arthritis. But it is important that they change the normal shape of the joint at a later stage. Possible crooked fingers. This is often visible without an x-ray, but the image confirms the suspicions.
Osteolysis. Rarely seen. This is a process in which bone is essentially resorbed. Accordingly, it is absent on x-rays in some areas. This sign indicates a big problem and the need for serious treatment of rheumatoid arthritis.
If tissue necrosis occurs (its death due to insufficient blood supply), this area will appear darker on the x-ray, looking like a shadow. In this case, this shadow is surrounded by a contour lighter than the color of the rest of the bone.
An indirect sign of necrosis in arthritis is the proliferation of osteophytes.
Osteophytes. Growths on the edges of joints in rheumatoid arthritis, which have already been discussed above. The more severe the stage, the larger the osteophyte. Thus, the answer to the question of whether arthritis is visible on an x-ray is yes.
Treatment and prevention of rheumatoid arthritis
Rheumatoid arthritis cannot be completely cured, this is a fact. Its treatment consists of reducing pain, reducing inflammatory and destructive processes in the joints, maintaining joint mobility and preventing the development of complications in other organs and systems of the body.
Along with drug treatment of rheumatoid arthritis, it is very important to follow a special diet; a vegetarian diet is most effective. No less important is physical therapy, which helps to maximally maintain joint mobility and, if possible, prevent muscle atrophy. At the initial stage of development of the disease, physiotherapeutic procedures, massage and applications can help. If the joint deformity is severe enough, surgical treatment is used.
It should be noted that there is an extremely high toxic effect of medications used to treat rheumatoid arthritis. Intoxication of the body and constant inflammatory process lead to a decrease in the life expectancy of patients by an average of 7 years.
In order to prevent the occurrence of this disease, it is recommended to prevent hypothermia, minimize exposure to toxic substances, avoid severe mental shock, and promptly and completely cure infections.
X-ray or MRI for rheumatoid arthritis?
Those who suspect they have rheumatoid arthritis are faced with a choice: X-ray or MRI? It is ideal to use both methods in combination, supplementing them with analyses. At the first stage of the disease, x-rays are practically useless, since pathological disorders are poorly visible. If you are worried about immobility and pain in the morning, it is better to consult an MRI.
At the same time, MRI is a more expensive procedure. Magnetic resonance imaging also has another drawback - the image provides information about the existence of a problem, but it is difficult to determine from it what kind of joint disease the patient is affected by. To classify and confirm that it is rheumatoid arthritis, an x-ray will also be required.
Alternative methods for diagnosing rheumatoid arthritis
If a classic radiograph did not allow the specialist to make a diagnosis and create a treatment program, computed tomography (CT) may be prescribed for clearer visualization of bone tissue. It is also based on the use of X-rays, but the images obtained during this procedure are not flat, but three-dimensional, layer-by-layer and more accurate. Therefore, even minimal changes in tissues are visible on them. However, CT is associated with greater radiation exposure to the patient's body.
To assess the degree of involvement of the soft tissues surrounding the affected joint in the pathological process, magnetic resonance imaging (MRI) is prescribed. It also allows, like CT, to obtain volumetric images, but involves exposing the patient to a magnetic field and radiofrequency pulses. It is known that X-rays tend to accumulate well in bone tissue and pass through soft tissue without hindrance. Therefore, if the nature of the changes in the latter is poorly visible on x-rays, then MRI displays them in the most complete volume.
Ultrasound examination (US) is more sensitive to detecting erosions in joints, compared to radiography. It is also prescribed to those patients who cannot undergo X-rays, CT, or MRI, since ultrasound has no contraindications. Thus, it is impossible to say unequivocally which examination method for rheumatoid arthritis is the best. The choice of diagnostic method is made by the attending physician based on the symptoms with which the patient came to him.
In what cases is a joint x-ray prescribed?
Some people believe that due to their young age they cannot get rheumatoid arthritis, especially in the advanced stages. And this is a big mistake, because the disease is rapidly growing younger and occurs in those who are only 30 or 20 years old. The reasons are trivial - environmental degradation, unhealthy diet, sedentary lifestyle.
Heredity plays a big role. If there are people in your family who have had or are suffering from rheumatoid arthritis, the appearance of its symptoms is a very alarming symptom.
X-ray of hands for rheumatoid arthritis
X-ray is a research technique that does not require damage to the patient’s skin. The method allows you to obtain an image of the part of the body being examined.
X-ray examination is prescribed in the following cases:
- For any injuries, including dislocations and fractures.
- For lameness.
- With partial or complete loss of limb mobility.
- If you experience discomfort or pain.
An x-ray to diagnose arthritis is prescribed if the following symptoms are present:
- Symmetrical joint damage.
- The appearance of swelling and redness.
- Stiffness of movements.
- Increased pain at night.
- The appearance of rheumatoid nodes.
- Limb deformity.
X-rays are performed not only to diagnose arthritis, but also to identify other joint problems.
The early stages of the disease are characterized by damage to the skeletal muscles. The first sign is muscle atrophy, which is directly dependent on the activity and severity of the articular syndrome. The combination of atrophy of the interosseous muscles, thenar and hypothenar muscles with swelling of the metacarpophalangeal, proximal interphalangeal joints, and wrist joints creates a picture of a typical rheumatoid hand.
In severe forms of rheumatoid arthritis, muscle atrophy is diffuse in nature with a large loss of muscle mass, often accompanied by a decrease in tone. However, muscle hypertonicity can also be observed, which causes sharp pain in this muscle group. Most often, with rheumatoid arthritis, atrophy of the extensors of the forearm, rectus femoris, and gluteal muscles is observed.
The active rheumatoid process is accompanied by myositis with foci of necrosis of muscle fibers, increased levels of creatine phosphokinase, transaminases, aldolase. Damage to the skin. Due to anemia and impaired vascular tone of the microvasculature, the skin of patients with rheumatoid arthritis becomes pale, and the color of the palmar and plantar surfaces may acquire a bright pink or cyanotic tint.
The result of cutaneous vasculitis can be subcutaneous hemorrhages (ecchymoses), small focal necrosis of soft tissues under the nail plates or in the area of the nail bed (digital arteritis). Trophic disorders lead to thinning of the skin, especially on the fingertips, and dryness. In the lower third of the leg, hyperpigmentation of the skin often occurs.
Violation of the trophism of the nails leads to their thinning, fragility, and longitudinal striations. Rheumatoid nodules are a typical extra-articular manifestation of rheumatoid arthritis. They are so specific for rheumatoid arthritis that they are included in the diagnostic criteria. Rheumatoid nodules are dense, round connective tissue formations from several millimeters to 1.5-2 cm in diameter, painless, mobile, but sometimes fused to the aponeurosis or underlying bone and then become immobile.
In 20-35% of cases, rheumatoid nodules are located on the extensor surface of the forearm, subcutaneously or periosteally. As a rule, in the presence of rheumatoid nodules in the blood, RF is detected in high titers. Rheumatoid nodules can be single or multiple, symmetrical or asymmetrical, and have different localizations - in the sacrum, back of the head, vocal cords, in the myocardium, valvular structures of the heart, lungs and even the central nervous system.
Multiple rheumatoid nodules are combined with severe synovitis and subchondral cystic changes in the small joints of the hands and feet and with a high titer of RF in the blood, called rheumatoid nodulosis. Rheumatoid nodules appear suddenly, usually during the next exacerbation. During remission they may disappear completely.
The early appearance of rheumatoid nodules is considered an unfavorable sign. Lymphadenopathy is one of the common manifestations of rheumatoid arthritis; generalized lymphadenopathy occurs in approximately 20% of patients. Enlarged lymph nodes are most often found in severe cases of rheumatoid arthritis and its variants such as Felty syndrome, SIRS.
Nodes are palpated on the neck, submandibular region, axillary, elbow, and inguinal. As the activity of the process subsides, the size and number of lymph nodes decrease. Lymphadenopathy is often combined with an enlarged spleen. Functional liver disorders are observed in 60–80% of patients. Moreover, in addition to the rheumatoid process itself, long-term use of various drugs (NSAIDs, gold salts, penicillamine, cytotoxic IDs) plays a role in liver pathology.
Among the extra-articular manifestations of rheumatoid arthritis, damage to the gastrointestinal tract is detected in more than half of the patients. However, the interpretation of these changes is difficult due to the fact that patients with rheumatoid arthritis are forced to take NSAIDs and corticosteroids for a long time, which affect the gastric mucosa.
With rheumatoid arthritis, the acid-forming function of the stomach is often impaired. Clinically, this is manifested by decreased appetite, a feeling of heaviness in the epigastric region, flatulence, and a coated tongue. Erosion of the fundus of the stomach mainly occurs due to disruption of the trophism of the gastric mucosa during vasculitis.
Intestinal damage is clinically manifested by constipation, bloating, and abdominal pain. Signs of chronic colitis are detected in 2/3 of patients. With rheumatoid arthritis, several types of damage to the lungs and pleura are distinguished: dry or effusion pleurisy, diffuse interstitial fibrosis or fibrosing alveolitis, multiple rheumatoid nodules, bronchiolitis obliterans, arteritis, small bronchi disease.
Dry, less often effusive pleurisy is the most typical pulmonary manifestation of rheumatoid arthritis. According to autopsy materials, pleural adhesions are detected in more than 40% of cases. In rheumatoid arthritis, the level of glucose in the pleural fluid is sharply reduced (to the point of complete absence), while the content of LDH, CPK, B-glucuronidase, and CEC increases.
The diagnosis of interstitial pulmonary fibrosis is usually made on the basis of an X-ray examination: symmetrical enhancement and fine-mesh restructuring of the pulmonary pattern, decreased transparency of the pulmonary background due to perivascular edema and edema of interstitial tissue are revealed. As this process progresses, a picture of a “honeycomb lung” is formed.
Pneumonitis is a rare manifestation of pulmonary pathology in rheumatoid arthritis, which is characterized by damage to the alveoli and the development of pulmonary failure. Damage to the respiratory tract in rheumatoid arthritis can also be caused by pathology of the bronchial glands if combined with Sjogren's syndrome.
Heart damage in rheumatoid arthritis is clinically manifested not so often, but according to autopsy data - in 50 - 60% of cases. Heart damage in rheumatoid arthritis includes: pericarditis, myocarditis, endocarditis, damage to the cardiac conduction tract, coronary arteritis, granulomatous aortitis. In rheumatoid arthritis, pericarditis is usually adhesive in nature (50%), effusion pericarditis is detected with high activity of the process.
There is a higher incidence of pericarditis in men. The effusion into the pericardial cavity in rheumatoid arthritis is sterile, with a low glucose content, increased levels of γ-globulins and RF. Rheumatoid granulomas can form in the pericardium in rheumatoid arthritis. Clinically, pericarditis progresses favorably, but occasional cases of complications with the development of adhesive pericarditis and cardiac tamponade have been described.
Rheumatoid pericarditis is characterized by the appearance of pain in the left half of the chest, an increase in the size of the heart, a transient friction noise of the pericardium, low voltage of the waves, and nonspecific changes on the ECG. Diagnosis of myocarditis in rheumatoid arthritis is difficult. There are only isolated descriptions of severe myocarditis with the development of heart failure.
Most often, the clinical manifestations of rheumatoid myocardial damage are nonspecific: tachycardia, muffled sounds, systolic murmur at the apex. The ECG may show changes in the ST segment of the T wave, atrioventricular block of I - II degrees, extremely rarely - III degrees. A comprehensive examination allows us to diagnose carditis in 20% of patients with rheumatoid arthritis.
A feature of rheumatoid myocarditis is a torpid course, positive dynamics are noted when the main process subsides. Granulomatous damage to the valvular apparatus can lead to the formation of heart defects with a relatively low clinical severity. The mitral valve is most often affected by rheumatoid arthritis, but involvement of the aortic valve has also been noted.
Aortic defect is detected in the form of relative insufficiency. Isolated cases of aortic valve stenosis have been described. In addition to damage to the aortic valves, specific granulomatous damage to the aortic walls is detected. Actively ongoing vasculitis can lead to the development of myocardial infarction. Kidney damage.
Rheumatoid membranous and membranous-proliferative glomerulonephritis, as a rule, is combined with high activity of rheumatoid arthritis and is characterized by trace proteinuria and microhematuria. Changes in urinary sediment may disappear completely and appear with the next exacerbation of the process. In rare cases, glomerulonephritis becomes progressive with persistent proteinuria, microhematuria, renal dysfunction, and increased blood pressure.
The prognosis for rheumatoid glomerulonephritis is favorable. In some cases, diffuse glomerulonephritis is observed, resulting in nephrosclerosis with the development of renal failure. Another cause of renal pathology in rheumatoid arthritis is the deposition of amyloid masses, which is typical for patients with a long duration of the disease (7-10 years or more) with high activity of the process.
However, in rare cases, signs of amyloid kidney damage are detected already in the first years of the disease. The most persistent sign of renal amyloidosis is proteinuria (1-3 g/l), cylindruria (usually hyaline casts), and peripheral edema. Gradually, disturbances in the concentration and nitrogen excretory function of the kidneys, anemia, arterial hypertension develop, and subsequently renal failure develops.
The prognosis for renal amyloidosis is unfavorable, the average life expectancy of patients is 1-4 years. Nephrotic syndrome in rheumatoid arthritis is almost always associated with renal amyloidosis. Amyloid nephrotic syndrome is characterized by high (6-8 g/l) proteinuria, hypoproteinemia, hypercholesterolemia, anemia, massive edema of the lower extremities, rapidly developing renal failure with normal blood pressure.
In rheumatoid arthritis, the possibility of developing drug-induced nephropathy should be considered. One of the most well-known lesions of the nervous system in rheumatoid arthritis is peripheral ischemic neuropathy, the frequency of which ranges from 1 to 10%. The leading role in the development of neuropathy is assigned to damage to the vasa nervorum.
Neuropathy occurs with sensory and/or motor disorders of varying severity. There are paresthesias, a burning sensation, a decrease in tactile, temperature, pain sensitivity or, on the contrary, hyperesthesia in the distal parts of the extremities. Multiple mononeuritis leads to motor impairment and limb weakness.
Polyneuritis is severe and is characterized by sequential damage to many peripheral nerves. Polyneuritis is manifested by severe pain in the limbs, motor and sensory disturbances, severe atrophy of regional muscles, and general weakness. Another form of damage to the peripheral nervous system in rheumatoid arthritis is compressive neuropathy, caused by compression of the peripheral nerves in the carpal, ulnar, and tarsal canals.
Often, rheumatoid arthritis reveals symptoms of functional damage to the autonomic nervous system in the form of impaired thermoregulation, sweating, diuresis, and trophic disorders. In rare cases, the central nervous system is affected, severe headaches, dizziness, and sometimes acute cerebrovascular accidents are noted.
Eye damage in rheumatoid arthritis is relatively rare and occurs in the form of episcleritis or scleritis. There is a description of the development of rheumatoid granulomas in the sclera, as well as retinal vasculitis. Necrotizing scleritis and nodular lesions can lead to perforation of this membrane of the eye and loss of vision.
Eye pathology in rheumatoid arthritis may be associated with treatment. Vasculitis is one of the extra-articular manifestations of rheumatoid arthritis; it is based on inflammation of the vascular bed - panarteritis. As a rule, vasculitis is associated with an active rheumatoid process, other extra-articular manifestations and aggravates the course of the disease.
The incidence of vasculitis varies, according to various authors, from 8 to 23%; it predominates in males. Rheumatoid vasculitis often occurs latently and is detected only at autopsy. Systemic vasculitis in rheumatoid arthritis is relatively rare (in 0.1-0.2% of patients), but its individual manifestations are a common finding.
The most common skin manifestations of vasculitis in rheumatoid arthritis are caused by obliterating endarteritis. Skin infarctions develop in the area of the nail plate or periungual bed, on the fingers or toes - the so-called digital arteritis. Outwardly, these changes resemble the mark of a splinter.
As a rule, they pass without a trace or leave a shallow scar. The development of obliterating endarteritis in larger arteries is manifested by gangrene of the finger and can lead to amputation of the phalanges. Ulcerative changes in the skin and underlying soft tissues are localized mainly in the lower third of the leg along the anterior surface.
They are usually deep, with tissue necrosis, difficult to heal during nonspecific therapy, which is practiced for trophic ulcers caused by venous insufficiency. Rarely, mainly in the lower parts of the leg, hemorrhagic vasculitis develops with rheumatoid arthritis, characterized by small rashes measuring 1-2 mm in diameter.
This type of vasculitis is associated with damage to venules, characterized by fibrinoid necrosis, inflammatory infiltrates consisting of neutrophils and mononuclear cells. Skin manifestations of vasculitis also include palmar and plantar capillaritis, livedo reticularis and Raynaud's syndrome. Secondary amyloidosis in rheumatoid arthritis is a serious complication and one of the most common causes of death of the disease.
The precursor of amyloid protein is the serum large-molecular protein SAA, produced by the liver under the influence of interleukin-6. Amyloidosis develops with high activity of the process, both in seropositive and seronegative variants of rheumatoid arthritis. Most often, amyloid deposits are fixed in the kidneys, which clinically manifests as proteinuria without significant changes in the urinary cellular sediment.
As amyloidosis progresses, proteinuria can reach high levels (3 g/l or more), and casts (hyaline and waxy) are found in the urinary sediment. Subsequently, nephrotic syndrome develops with hypoproteinemia, edema, hypercholesterolemia, increased levels of a2-globulins, and an increase in ESR to 70 mm/h, which does not coincide with the activity of the underlying disease.
Also, amyloid is often deposited in the gastrointestinal tract, but without clinical manifestations. However, persistent diarrhea, weight loss, and signs of vitamin deficiency should suggest amyloid damage to the gastrointestinal tract. In isolated cases, cardiac amyloidosis, manifested by rhythm disorders, has been described in rheumatoid arthritis , increasing circulatory failure, lack of effect from digitalis preparations.
To confirm amyloidosis a, histological examination of tissue biopsies is necessary. The most informative and safe is the study of the mucous membrane of the rectum (positive results are observed in 60-70%), the mucous membrane of the gums (40-50%) and subcutaneous fatty tissue of the abdominal wall.
First stage of the disease
So, the initial x-ray stage of rheumatoid arthritis. The carpal and metatarsophalangeal joints are most often affected at this stage. In X-ray images, you can see thick and dense elements in the soft tissues near the joints, thinning of the bone tissue and the presence of a certain amount of cyst-like enlightenment in it.
Periarticular osteoporosis is clearly visible. The disease is characterized by changes in bone structure. They become very loose, their porosity increases, and, accordingly, their fragility. At the first stage of arthritis, a slight decrease in the joint space is detected, which is an indicator of the development of the disease.
Types of deformation
There are different types of deformities for the joints of the hand. The ones that are most common are named after their types: "walrus fin", "swan neck" and "button loop". An X-ray sign of rheumatoid arthritis at this stage is the formation of deposits of calcium salts in the soft tissues located near the rheumatic joint. Their calcification refers to the formation of rheumatoid nodes, reaching two to three centimeters in diameter. An excess of deposited calcium salts causes this process.
Rheumatoid nodules have a dense structure and round shape, painless when palpated. Calcifications are clearly visible on x-rays, as they have a structure that is heterogeneous in density. The pain in the joints and their limited mobility are so severe that significant effort is required to perform normal activities. The patient at this stage is not able to engage in professional activities and sports (taking into account the age and gender of the person suffering from arthritis).
Diagnosing the disease at an early stage
Detection of pathology at the initial stages of formation allows you to begin a timely course of therapy. This helps prevent the development of complications. But the process of identifying the inflammatory reaction of connective tissue in the initial phase is due to a number of difficulties. This is the coincidence of the symptoms of the disease with other pathologies, as well as the lack of highly effective laboratory techniques for recognizing the diagnosis in the early stages. The main topic of our material is rheumatoid arthritis at the X-ray stage.
The initial stage of the disease is considered to be the period of time from the appearance of the first negative signs to the onset of destructive changes in cartilage tissue. As a rule, this period lasts about three months. Significant information for diagnosing rheumatoid arthritis in the early stages of the disease is the complaints obtained during an oral interview with the patient. Among them are:
- the occurrence of joint pain;
- the formation of stiffness and swelling in the affected area;
- pain when squeezing your hands or when walking (pain is reflected in the ankle system);
- weight loss;
- temperature increase;
- the presence of rapid fatigue;
- the presence of weakness of the body as a whole.
Types of erosion
This stage of arthritis development continues until the first erosion appears, namely bone damage. They can be grouped into three types. Marginal superficial erosions most often affect the small joints of the hands. In the place where the bone of the joint is not covered by cartilage tissue, it is susceptible to damage. Next, a racemose structure is formed and, under the influence of progressive articular osteoporosis, a deepening of the bone area occurs, which is inherent in compression erosions. This is how rheumatoid arthritis is determined through the eyes of a radiologist.
The third type of erosion is where the superficial bone tissue degrades where the endplate of the joint connects to the ligaments. A very significant radiological sign of the initial stage of rheumatoid arthritis is the identification of these erosions. After a defect is detected in the diseased joint, the next stage begins - 2B. This stage continues until no more than 4 erosions appear.
At the second stage, dysfunction of joint mobility appears, which can last up to several hours a day, due to the effect on cartilage tissue. At this stage, x-rays do not reveal any signs of changes in the cartilage of the hand or foot. With exertion, the pain intensifies. What other X-ray stages and signs of rheumatoid arthritis (RA) are there?