General blood tests
09/23/201909/25/2019 Chernenko A. L. 857 Views many, general analyzes
This article discusses the INR blood test: what it is and how much the indicator should be.
For laboratory assessment of the quality of the external blood coagulation pathway, the study of prothrombin time (PTT) and its derivatives is used:
- prothrombin index (PTI);
- international normalized ratio (INR indicator).
These indicators are used when assessing the state of the blood coagulation system, monitoring the effectiveness of treatment with warfarin drugs (analysis of INR during warfarin therapy is a mandatory diagnostic method), liver dysfunction, vitamin K deficiency, etc.
Analysis for prothrombin time and its derivatives (blood test for INR and prothrombin index) allows you to assess the quality and activity of the first, second, fifth, seventh and tenth blood coagulation factors. To obtain more complete information, this study is often performed in combination with activated partial thromboplastin time (aPTT).
- 1 What is blood clotting?
- 2 INR blood test - what is it and how long should it be?
- 3 When is a blood test for INR indicated?
- 4 How to prepare for a blood test for INR?
- 5 Table of INR norms for women by age
- 6 Norm INR in the blood of men
- 7 INR norm when taking warfarin
- 8 What does it mean if the INR is elevated?
- 9 Reduced prothrombin
- 10 Foods that increase INR when taking warfarin
What is blood clotting?
The process of blood coagulation is the most important part of the hemostasis system (the system that maintains the liquid state of the blood, is responsible for stopping bleeding, dissolving thrombotic clots, etc.).
Blood clotting consists of several stages:
- stages of primary vascular-platelet hemostasis (the primary stage of stopping bleeding caused by vasospasm and the formation of a platelet clot);
- stage of enzymatic blood coagulation (called hemocoagulation, plasma hemostasis, secondary hemostasis), which consists in the formation of a stable thrombus strengthened by fibrin threads.
The blood coagulation process itself is a proenzyme-enzyme cascade that occurs in the form of sequential activation of blood coagulation factors by proenzymes. As a result, the blood clotting process is divided into three phases:
- activation (a complex of sequential processes that activate the formation of prothrombinases and the transformation of prothrombin into thrombin);
- coagulation (the process of formation of fibrin fibers from fibrinogen);
- retraction (the process of formation of dense fibrin clots).
To assess the functioning of the blood coagulation system, global (general) and local (specific) testing is used.
Global testing allows for a general assessment of the state of the blood coagulation system and assesses the patient's tendency to form blood clots or increased bleeding.
Global tests include:
- determination of T (time) of blood clotting using the methods of Sukharev, Morawitz, Mas-Magro;
- performing thromboelastography;
- thrombin generation tests (assessment of thrombin potential and endogenous thrombin potential);
- assessment of thrombodynamics.
Local tests include studies that make it possible to evaluate individual parts of the coagulation cascade and clarify the localization of the pathological process. Local analyzes include assessment of:
- activated partial thromboplastin time (aPTT);
- prothrombin time tests (prothrombin index, INR, etc.);
- narrowly targeted techniques to identify disturbances in the functioning of a specific blood coagulation factor.
The type of analysis is prescribed exclusively by a specialist based on the expected diagnosis of additional examination data.
Blood INR: measurement, interpretation, norms
Many people hear the blood INR indicator. What does it mean? Why do doctors pay so much attention to him? How important is the determination of blood INR in medical practice? Read about this in our article.
What is blood INR?
The abbreviation INR blood stands for International Normalized Ratio . However, for a person not involved in medicine, this is an empty phrase. To understand the essence of blood INR and its role in the body, you need to take a short excursion into the physiology of the circulatory system.
The liquid state of blood in the human body is ensured by the coordinated work of the coagulation and anticoagulation systems. Fluidity, an important property of blood, is ensured by the anticoagulant system, and during bleeding, clotting ability becomes important. If the functioning of these systems is disrupted, a person experiences increased bleeding (for example, constant bleeding of the gums when brushing teeth, frequent nosebleeds) or a tendency to thrombosis - the formation of blood clots that can “pass” through vessels of larger diameter and “get stuck” in vessels of smaller diameter diameter It is dangerous when they enter the vessels of the heart and brain, because in these cases they lead to heart attacks and strokes and, as a result, to disability.
Normally, a healthy person is in a state of slight hypercoagulation, i.e. in a healthy body there is a slightly increased functioning of the coagulation system. However, in the absence of diseases, this feature does not lead to acute vascular accidents (heart attacks and strokes). In the presence of certain diseases (and first of all, the very common atrial fibrillation), the already existing tendency to thrombus formation sharply increases. Doctors have long noticed this feature, therefore, if a person has diseases accompanied by increased thrombus formation, they prescribe antithrombotic therapy (anticoagulants and antiplatelet agents) to prevent heart attacks and strokes. I would like to emphasize that these drugs are prescribed strictly by a doctor, since if used independently and uncontrolled, they can have serious life-threatening consequences. The severity of the effects of these drugs is closely related to the concept of blood INR.
Since antithrombotic drugs thin the blood by preventing blood clots, it is extremely important to monitor blood counts that reflect “how thin” the blood is. The main indicator is blood INR. The widely used indicators PTT (prothrombin time) and PTI (prothrombin index) are slowly receding into the background, because the method for determining these indicators involves the use of each specific laboratory with its own reagent with individual sensitivity. Therefore, results may vary greatly between laboratories. The APTT (activated partial thromboplastin time) indicator is determined during treatment with heparin (strictly in hospital conditions). The blood INR indicator was introduced into medical practice in order to somehow standardize the indicators of the blood coagulation system. It is not for nothing that the abbreviation INR blood stands for international normalized ratio.
The most common antithrombotic drug prescribed by doctors is warfarin. This is a well-studied medicine with an extensive evidence base. But it is precisely when using warfarin that it is so important to determine the blood INR. The normal range of blood INR values during warfarin treatment is 2.0-3.0. If the blood INR is less than 2.0, then the risk of ischemic stroke increases, but if the blood INR is more than 3.0, the risk of cerebral hemorrhage increases. The graph below clearly shows within which blood INR values the risks of dangerous complications are minimal (the so-called “therapeutic window”).
By the way, in a person who does not use warfarin, the blood INR value ranges from 0.85-1.35.
Where can I measure blood INR?
There are 3 main ways to measure blood INR. First: you go to the clinic to see your local physician, who, after the necessary examination, prescribes a blood test for you, which you take either in the same clinic for free, or in a private laboratory at your own expense (this depends on the capabilities of your clinic). The second method is almost the same, the only difference is that the blood INR test is done by a therapist in his office (provided that he has the appropriate equipment to carry out this analysis). The third way: purchase a small portable device for testing blood INR yourself. Of course, this device is not cheap, but with it you will be confident in your safety every day, especially since warfarin treatment is usually very long, and in some cases lifelong. Therefore, you purchase this device for long-term use, making a huge contribution to your health and quality of life.
It is important to remember that warfarin, like any medicine, can interact with other drugs and substances, changing its activity. This is important to consider, since in this case dose adjustment is necessary to maintain the blood INR within the range of 2.0-3.0 . Below is a table of warfarin interactions.
Spectrum of drug and food interactions of warfarin*
| Drugs that increase the activity of warfarin | Drugs that reduce the activity of warfarin | Dietary restrictions |
| Amiodarone, anabolic steroids, antabuse, acetaminophen, bispeptol, influenza vaccine, isoniazid, lovastatin, metronidazole, miconazole, norfloxacin, NSAIDs, omeprazole, ofloxacin, propronolol, salicylates, tamoxifen, tetracycline, thyroxine, phenytoin, fluconazole, fropafenone, quinine din, cimetidine, ciprofloxacin, erythromycin | Azathioprine, barbiturates, cabamazepine, cholestyramine, cyclosporine, griseofulvin, rifampicin, sucralfate | Alcohol, herbs, green tea, ginger, garlic and more |
*Plus resistance to warfarin
In conclusion, I would like to add that there are currently new oral anticoagulants (NOACs) that are easy to use and do not require the labor-intensive process of determining blood INR and other indicators. A significant negative side of these drugs is their high cost. The table below provides examples of new oral anticoagulants.
Laboratory monitoring of NOACs
| Controlled indicators | Dabigatran | Rivaroxaban | Apixaban |
| Platelets | No control needed | No control needed | No control needed |
| INR | No control needed | No control needed | No control needed |
| APTT | If it is increased by 2 or more times, the risk of bleeding increases | No control needed | No control needed |
| Prothrombin time | No control needed | Prolonged time may increase the risk of bleeding | No control needed |
Author: therapist A.V.
Kosova
INR blood test - what is it and how long should it be?
A blood test for INR is one of the options for studying prothrombin, a complex protein that is a precursor to thrombin and stimulates the process of blood clot formation.
The International Normalized Ratio (INR) measures the rate at which a blood clot forms.
INR values are not assessed separately from prothrombin.
This is due to the fact that the INR is calculated using the formula: (patient's prothrombin time / normal prothrombin time) raised to the value of the ISI (international sensitivity index).
The MIC value usually ranges from 1 to 2 and depends on the reagent used for the analysis.
The MIR indicates the level of tissue factor (thromboplastin) activity for a given batch of reagent, compared to standardized samples.
When deciphering the test results, the prothrombin level is assessed (prothrombin according to Quick is often used, displaying prothrombin activity as a percentage), the INR and, as a rule, the prothrombin index (PTI displays the ratio of the normal prothrombin time to the patient’s prothrombin time).
Don't panic
Patients who are sent for INR measurements repeatedly (and constantly) are usually aware of all the intricacies of the analysis, but people who are just starting a “new life” (with indirect anticoagulants) may be scared if they are asked to repeat the study. There should be no panic or premature conclusions in such cases; perhaps the analysis did not work out for reasons beyond the patient’s control. For example, the following factors can distort the indicator values:
- The blood taken from a vein and placed in a test tube with an anticoagulant was not sufficiently mixed (clots had formed somewhere);
- Blood to determine the international normalized ratio was taken from capillary vessels (instead of venous ones), as a result of which tissue thromboplastin entered the sample, which sent the course of events along the wrong path;
- Improper handling of the sample and subsequent hemolysis led to distortion of the study results.
Health workers usually look for their own mistakes, noticing that the results are clearly distorted, and are in no hurry to decipher them.
And finally, it should be noted that INR does not require any special preparation on the part of the patient (diet and lifestyle - as usual), however, medications used for concomitant pathology and that can change the test results should be excluded. However, the doctor will definitely tell you about this.
Display all posts with the tag:
- Analyzes
- Blood clotting
Go to section:
Blood diseases, tests, lymphatic system
Recommendations to SosudInfo readers are given by professional doctors with higher education and specialized work experience.
One of the leading authors of the site will answer your question.
When is a blood test for INR indicated?
A study on the level of prothrombin, INR and PTI is indicated for:
- suspected bleeding disorders (increased bleeding, thrombosis);
- conducting screening studies of the hemostasis system;
- control of blood clotting in patients receiving anticoagulant therapy;
- before and after heart surgery;
- treatment of pulmonary embolism (as well as when assessing the risk of developing pulmonary embolism);
- the patient has liver cirrhosis, vitamin K deficiency, malignant neoplasms, hereditary and acquired coagulopathies;
- treatment with drugs that can increase or decrease blood clotting.
Low or high INR
A blood test to control the INR level can be performed both in the treatment room and at home (to do this, it is enough to purchase a device for measuring INR). The analysis result should be deciphered by a doctor who will adjust the dose of anticoagulants, if used. If the INR increases (the risk of bleeding increases), the dose of anticoagulants should be reduced. And as a result of a decrease in this indicator, blood clots may form, so the dose should be increased.
Other reasons for prescribing a blood test to determine the INR level may be:
- nosebleeds;
- bleeding gums;
- unreasonable occurrence of bruises;
- blood in urine;
- heavy, prolonged menstruation in women;
- traces of blood in sputum or vomiting;
- blood in stool;
- prolonged bleeding from abrasions or cuts;
- change of climate, lifestyle, diet.
If, according to the results of the analysis, the INR deviates upward, this indicates that blood clotting is increased, and accordingly the risk of diseases and pathologies is increased:
- myocardial infarction;
- liver diseases;
- congenital diseases of the circulatory system;
- pre-infarction condition;
- polycythemia;
- malignant tumors;
- impaired absorption of fats in the intestine;
- hemorrhagic disease in infants;
- problems with bile entering the duodenum from the liver.
If the INR is reduced, this also indicates problems in the body:
- blood clotting during pregnancy, as well as after delivery, is increased;
- prothrombin deficiency;
- lack of vitamin K;
- the amount of thromboplastin in the blood is increased (as a result of a cut or anesthesia).
Some factors may distort the results of the study when decoding:
- the blood tube was not filled enough and was mixed with the anticoagulant;
- destruction of red blood cells as a result of improper vein puncture;
- side effects of certain drugs (antibiotics, anabolics, steroids);
- the standard for keeping the sample at +4 °C was violated;
- a sample was taken not of venous, but of capillary blood (tissue thromboplastin was included in the sample).
It is worth emphasizing once again that timely control of INR levels can protect against various pathologies and complications, and also reduces the risk of complications during anticoagulant therapy. This test is recommended by WHO as one of the most effective and reliable for determining the state of blood clotting.
How to prepare for an INR blood test?
The analysis is given on an empty stomach. Venous blood is used for the study.
You should not smoke before the test. It is also recommended to avoid physical and emotional stress.
2-3 days before the test you should stop drinking alcohol.
The attending physician and laboratory staff should be notified about the medications the patient is taking, since some medications (anticoagulants, oral contraceptives, glucocorticoids, etc.) can affect the test parameter.
What are the indications for an emergency test?
- Acute infectious disease (respiratory, intestinal infection).
- Climate change (long-distance and long flights, transfers).
- Changing work and rest schedules, diet, physical activity, taking new medications. It should be noted that when taking new medications or consuming new foods, the INR should not be rechecked immediately, but after 2-3 days. It must be remembered that there is a list of drugs that increase or decrease the effect of warfarin.
- Frequent and prolonged bleeding (nose, gum, menstrual, blood in stool, urine, sputum).
- The appearance of compactions and swelling in the joints.
- Before planned invasive procedures (tooth extraction, gastroscopy)
In conclusion, I would like to say that following simple rules for taking anticoagulants with regular monitoring of INR will save you from unnecessary costs for expensive and inappropriate treatment and severe complications.
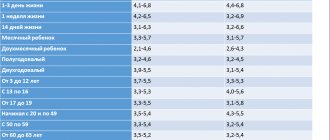
Table of INR norms for women by age
It should be noted that because different laboratories use different reagents, normal values may vary for each laboratory.
In this regard, when interpreting the results of the analysis, one should be guided by the standards indicated on the form with the results.
| The INR norm for women does not depend on age and is: | from 0.85 to 1.35. |
| During pregnancy, INR may decrease: | in the third trimester the norm is from 0.15 to 1.17 |
Norms depending on gender
The level is calculated as an index. That is, a numerical value without a unit of measurement. How the result is obtained has already been said earlier.
- The INR norm for women ranges from 0.7 to 1.3. The average value varies around unity.
- Among the male population, the coefficient is approximately the same. Plus or minus. There are several points of view on this issue. Some doctors say that there are no differences at all, others indicate that the INR norm in adult men is 1.2-1.4.
- In children, an adequate indicator is approximately 0.9-1.1. Slight deviations may occur.
What does it mean if the INR is elevated?
The INR is always assessed together with the prothrombin level. This study is not carried out in isolation (INR is calculated based on the patient’s prothrombin level). Therefore, the reasons for changes in the level of INR in the blood should be interpreted together with the level of prothrombin.
The INR level is inversely proportional to the prothrombin level and the amount of blood clotting factors (the higher the INR level, the lower the prothrombin level).
Most often, the INR is elevated when:
- liver diseases;
- consumption coagulopathies (conditions in which, against the background of active thrombus formation, blood clotting decreases due to depletion of blood clotting factors);
- fibrinogen and/or prothrombin deficiency;
- vitamin K deficiency.
A low INR level is observed in patients with an increased risk of blood clots, the early stage of thrombosis. Also, a decrease in INR levels can be observed in the last trimester of pregnancy.
An increase in the level of prothrombin according to Quick is observed with:
- tendency to thrombosis, development of thromboembolic conditions, myocardial infarction, pre-infarction conditions, increased blood viscosity due to hypohydration, with hyperglobulinemia;
- taking certain medications: drugs that can inhibit the effect of coumarin (vitamin K drugs, barbiturates), corticosteroids, oral tablet contraceptives, meprobamate drugs, antihistamines;
- polycythemia;
- the presence of malignant neoplasms in the patient.
Elevated INR level
If the INR is elevated, this indicates the following problems:
- liver diseases (cirrhosis, fatty degeneration, chronic hepatitis, toxic damage);
- disruption of vitamin K synthesis in the body;
- lack of certain plasma proteins;
- DIC syndrome;
- congenital deficiency of coagulation factors;
- diseases of the stomach and intestines, in which the absorption and breakdown of fats is impaired;
- massive blood transfusion.
An INR higher than normal is a consequence of decreased blood clotting, the so-called hypocoagulation. This condition may cause bleeding or hemorrhage.
Massive external bleeding can occur with a slight violation of the integrity of the skin (abrasion, scratch), and internal bleeding most often develops against the background of an existing disease (for example, gastric - with a stomach ulcer, uterine - with uterine fibroids).
Such conditions require immediate hospitalization of the patient and correction of the impaired coagulation system.
Decreased prothrombin
A reduced level of prothrombin can be recorded when:
- hereditary or acquired deficiencies of the first, second, fifth, seventh, tenth blood coagulation factors;
- idiopathic familial hypoprothrombinemia;
- acquired or hereditary hypofibrinogenemia;
- vitamin K deficiency (without vitamin K, the second, seventh, tenth blood clotting factors are not formed in hepatocyte cells);
- vitamin K deficiency in the mother (hemorrhagic diathesis is observed in newborns);
- taking certain medications: vitamin K antagonists (anticoagulants - phenylin, coumarin), anabolic steroids, clofibrate, glucagon, thyroxine, indomethacin, neomycin, oxyphenbutazone, salicylates, heparin, urokinase/streptokinase.
Why is determining the INR so important?
The human body has the ability to self-defense, as well as self-healing. One of the devices that provides these capabilities is the hemostasis system, which maintains the blood viscosity necessary to perform the assigned functions.
That is, it controls the clotting process, namely, when bleeding occurs, a chain of chemical reactions is launched aimed at creating blood clots. The latter block the flow of blood - “seal the gaps” in the vessels, as a result of which the bleeding stops.
At the same time, in various laboratories, different thromboplastins (from several manufacturers) were used to perform this blood test - reagents that specifically trigger the clotting process. This often led to different values obtained, which alarmed both doctors and patients themselves.
In order to avoid such inconsistencies, which show different results in several laboratories, and not be tied to the standards adopted in each specific one, the INR indicator was introduced. It cannot be unambiguously called analysis, since at its core it is an ordinary mathematical calculation using a standardized formula.
Reference! The test for determining INR was approved in 1983 by two International Committees - on standardization in hematology and on hemostasis and thrombosis.
The described parameter is calculated using a specially developed formula, including the PTT of the subject and the corresponding MIC coefficient, denoting the international thromboplastin sensitivity index. According to WHO recommendations, the manufacturer must determine the MRI for each batch of reagents by comparison with a generally recognized reference index.
Formula for calculating INR
The use of INR provides the opportunity to compare research results made in different laboratories and at different times without fear for the condition and life of patients. This is the standard ratio used by doctors in all countries.
Therefore, it is the result of calculating the INR that is indispensable when selecting and prescribing the dosage of anticoagulation drugs, transfusion of plasma and its components, as well as other agents. In addition, such a study is necessary to determine the tactics for further treatment of patients with diseases of the hemostatic system.
Conditions in which it is advisable to get tested
Separately, it is also worth highlighting diseases and pathological conditions in which a blood test for INR is not necessary, but in some cases the doctor may prescribe it. Among them:
- long-term infectious diseases;
- sudden change in lifestyle;
- change in diet;
- climate change;
- the appearance of blood in the urine;
- prolonged menstrual bleeding in women;
- frequent nosebleeds;
- causeless bruises and hematomas;
- blood in the stool;
- constant appearance of blood when brushing your teeth;
- prolonged bleeding from minor injuries;
- periodic appearance of swelling, pain and redness of the joints, which may be due to the accumulation of blood in them.
Drug and food interactions of warfarin
It is important to remember that warfarin, like any medicine, can interact with other drugs and substances, changing its activity. This is important to consider, since in this case dose adjustment is necessary to maintain the blood INR in the range of 2.0–3.0. Below is a table of warfarin interactions.
Spectrum of drug and food interactions of warfarin*
| Drugs that increase the activity of warfarin | Drugs that reduce the activity of warfarin | Dietary restrictions |
| Amiodarone, anabolic steroids, antabuse, acetaminophen, bispeptol, influenza vaccine, isoniazid, lovastatin, metronidazole, miconazole, norfloxacin, NSAIDs, omeprazole, ofloxacin, propronolol, salicylates, tamoxifen, tetracycline, thyroxine, phenytoin, fluconazole, fropafenone, quinine din, cimetidine, ciprofloxacin, erythromycin | Azathioprine, barbiturates, cabamazepine, cholestyramine, cyclosporine, griseofulvin, rifampicin, sucralfate | Alcohol, herbs, green tea, ginger, garlic and more |
* — Plus resistance to warfarin.
Technique and frequency of blood sampling
Blood for INR analysis is prescribed by the doctor conducting anticoagulant treatment, usually 2 times a month, more often if necessary. If treatment is adjusted and the patient’s condition is stable, INR monitoring is carried out once a month.
The test is taken in the morning on an empty stomach, the day before you should not drink alcohol, you need to limit physical activity . Blood for analysis is taken from a vein in the laboratory as prescribed by a doctor in the usual way, as for other studies.
Today, the problem of determining INR has been greatly simplified; it can be monitored even at home by purchasing a portable analyzer (CoaguChek XS). It allows you to receive information about your blood condition much more often without visiting a clinic or puncturing veins. All you need is a small drop of capillary blood from your finger, and the analysis itself is carried out by testing on paper strips, which are stored for up to 1.5 years.
The device performs electrochemical analysis, is quite accurate and complies with WHO international recommendations.
An analysis for PTI is also taken on an empty stomach in the laboratory, subject to the same rules. Blood is taken from a vein or from a finger (capillary), and its indicators will be slightly different.
Why measure INR and PTI?
In medical practice, INR analysis is very important for monitoring blood clotting ability in patients taking tableted (indirect) anticoagulants, for example, warfarin, phenylin, tromexane and others. They are often prescribed for conditions where there is a threat of thrombosis: heart rhythm disturbances, blood thickening, severe vascular atherosclerosis, thrombophlebitis, increased prothrombin.
Treatment with anticoagulants should always be carried out under the control of coagulation , because an insufficient dose can only “spur” thrombus formation, and excessive use, on the contrary, can reduce coagulation and lead to the development of bleeding.
It is the INR analysis that reflects the most objective picture of blood clotting, regardless of the time of day, food or liquid intake.
An analysis of the prothrombin index (PTI) reveals the very fact of a decrease or increase in blood clotting. It is always prescribed before operations, childbirth, blood transfusions and other procedures, and is prescribed to patients with cardiovascular pathology and the elderly. Deviation of PTI from the norm is an indication for examining the patient to determine the cause of the violations.