A coagulogram (otherwise known as a hemostasiogram) is a special study that shows how well or poorly a person’s blood clotting occurs.
This analysis plays a very important role in determining a person's condition. Its indicators help predict how the operation or childbirth will go, whether the patient will survive, and whether it is possible to stop the bleeding of the wounded.
True, not all doctors have the ability to read a coagulogram. However, sometimes this research can save a person’s life.
A little about blood clotting
Blood is a special liquid that has the ability not only to circulate through vessels, but also to form dense clots (thrombi). This quality allows it to close gaps in medium and small arteries and veins, sometimes even unnoticed by humans. The preservation of the liquid state and blood clotting is regulated by the hemostasis system. The coagulation system or hemostasis system consists of three components:
- vascular cells, and specifically the inner layer (endothelium) - when the vessel wall is damaged or ruptured, a number of biologically active substances (nitric oxide, prostacyclin, thrombomodulin) are released from the endothelial cells, which trigger thrombus formation;
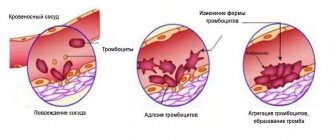
- platelets are blood platelets that are the first to rush to the site of injury. They stick together and try to close the wound (forming a primary hemostatic plug). If platelets cannot stop bleeding, plasma clotting factors are switched on;
- plasma factors - the hemostasis system includes 15 factors (many are enzymes), which, due to a series of chemical reactions, form a dense fibrin clot that finally stops bleeding.
A special feature of coagulation factors is that almost all of them are formed in the liver with the participation of vitamin K. Human hemostasis is also controlled by the anticoagulant and fibrinolytic systems. Their main function is to prevent spontaneous thrombus formation.
Etiology of low prothrombin protein levels
The Quick coefficient has been lowered, reasons:
- Lack of vitamin K in the body,
- Liver diseases,
- Genetic predisposition.
An increased percentage of prothrombin index occurs because:
- A person has problems with blood clotting, congenital in nature,
- Changes in heparin levels when taking anticoagulants,
- Vitamin K deficiency in the body
- Oncological neoplasms,
- Use in the treatment of antibacterial drugs that have a wide spectrum of action.
Vitamin K deficiency
Low prothrombin, what to do and how to increase it?
To increase prothrombin, you must follow a proper diet and use foods in your diet that can increase this protein in the body:
- Buckwheat,
- Animal fats
- Cabbage, red pepper,
- Bread,
- Smoked and pickled products,
- Beans and greens.
Indications for prescribing a hemostasiogram
- general assessment of the state of the hemostatic system;
- planned examination before operations;
- spontaneous childbirth or caesarean section;
- severe gestosis;
- control of therapy with indirect anticoagulants (aspirin, warfarin, trental), heparin preparations (clexan, fraxiparin);
- diagnosis of hemorrhagic pathologies (hemophilias, thrombocytopathy and thrombocytopenia, von Willebrandt disease);
- varicose veins of the lower extremities (see treatment of varicose veins at home);
- with a high risk of thrombosis (atrial fibrillation, coronary heart disease);
- definition of DIC syndrome;
- taking oral contraceptives, glucocorticosteroids, anabolic steroids;
- chronic liver diseases (cirrhosis);
- acute inflammatory processes in the body;
- diagnosis of various thromboses - vessels of the lower extremities, intestines, ischemic stroke, pulmonary embolism.
Hemostasiogram and coagulogram: what is the difference
A hemostasiogram is a study of venous blood that includes all indicators of liquid connective tissue involved in the functioning of the hemostasis system:
- red cell component of blood;
- small plates formed in the bone marrow;
- red blood cell volume;
- white cells of the immune system;
- the proportion of whole blood that is taken up by platelets.
A coagulogram shows the degree of blood clotting in the human body, while a hemostasiogram shows the process that ensures the functioning of the proenzyme cascade.
How to prepare for a coagulogram?
- the material is taken strictly on an empty stomach, it is advisable that the previous meal was at least 12 hours ago;
- the day before, it is recommended not to eat spicy, fatty, smoked foods, or alcohol;
- Smoking is prohibited before collecting material;
- it is advisable to stop taking direct and indirect anticoagulants, since their presence in the blood can distort coagulogram parameters;
- if taking such medications is vital for the patient, it is necessary to warn the laboratory doctor who will review the analysis.
Preparing for analysis
The method is based on the effect of special reagents on the blood and sample. To get reliable results, preparation is necessary.
- They refuse food 12 hours before. In order not to provoke false thickening of the blood.
- It is necessary to temporarily adhere to a diet. At least for two days. Avoid fatty, fried, smoked foods, salt no more than 4 grams per day. So as not to provoke a false research result.
- Anticoagulants and antiplatelet agents are stopped within two days. This will allow you to obtain the most accurate research results.
- Avoid smoking within a few hours. Also alcohol.
Blood for a coagulogram is taken from a vein, less often from a finger. It is necessary to strictly follow the recommendations of the preparation specialist. Otherwise the results will be false. And this is dangerous, because it is likely to be treated incorrectly.
How is a blood clotting test performed?
- The material is collected using a dry sterile syringe or a Vacutainer vacuum blood collection system;
- Blood collection should be carried out with a wide-bore needle without using a tourniquet;
- vein puncture must be atraumatic, otherwise a lot of tissue thromboplastin will get into the tube, which will distort the results;
- the laboratory assistant fills 2 test tubes with the material, sending only the second one for examination;
- the test tube must contain a special coagulant (sodium citrate).
Reasons for deviations from the norm?
APTT, the norm for women by age is given in the article, may change under the influence of the following factors.
Extending test results:
- massive blood transfusions;
- reception (administration) of heparin and its analogues, streptokinase;
- insufficient volume of anticoagulant or filling of the tube (laboratory error).
Shortening coagulation time:
- acute blood loss;
- contamination of the sample biomaterial with tissue proteins during blood sampling from a vein.
The use of specific reagents during the study can “push back” the normal APTT value to 22 seconds. downwards and up to 45 sec. in the direction of increase. Therefore, each laboratory accepts its own therapeutic ranges.
Changes in aPTT in diseases of the hemocoagulant system occur when the level of factors decreases or increases by 30-40%. Since false positive results are possible, in some cases it is recommended to take tests again.
Normal coagulogram
| Clotting time | ||
|
| |
| Bleeding time | ||
|
| |
| Analysis indicator | Its designation | Norm |
| Prothrombin time according to Quick | PV | 11-15 sec |
| INR (International Normalized Ratio) | INR | 0,82-1,18 |
| Activated Partial Thromboplastin Time | APTT | 22.5-35.5 sec |
| Activated Recalcification Time | AVR | 81-127 sec |
| Prothrombin index | PTI | 73-122% |
| Thrombin time | TV | 14-21 sec |
| Soluble fibrin-monomer complexes | RFMK | 0.355-0.479 units |
| Antithrombin III | AT III | 75,8-125,6% |
| D-dimer | 250.10-500.55 ng/ml | |
| Fibrinogen | 2.7-4.013 g | |
Norms of indicators by age
The normal APTT value is 25-38 seconds. It depends on the characteristics of the set of reagents, so each laboratory, when undergoing an examination, indicates the reference values that are contained in the passport of the medical diagnostic system.
This type of analysis is not standardized by the World Health Organization, since it uses various chemical compounds (animal or plant phospholipids, a mixture of them; phospholipids obtained from human blood cells). APTT norms are also not classified by the patient’s age, since there are no pronounced changes in this indicator.
Among women
Physiological changes in APTT values may occur during pregnancy and menstruation. During this period, the indicator drops to 18 seconds. A very low value is accompanied by the risk of blood clots forming in the vessels of the placenta, which can lead to abruption and miscarriage.
APTT in the blood test, normal in the table.
With a high APTT, intrauterine bleeding may develop, which also threatens the life of the fetus and the woman herself.
In men
For men, the norm remains the same - within 25-38 seconds. Conditions under which a decrease or increase in aPTT may occur are described below.
In children
The rate of activated partial thromboplastin time for children corresponds to that for adults. However, in newborns, and especially in premature infants, it typically increases by 3-5 seconds.
Decoding the coagulogram
Prothrombin time (PT)
PT is the time of formation of a thrombin clot if calcium and thromboplastin are added to the plasma. The indicator reflects phases 1 and 2 of plasma coagulation and the activity of factors 2,5,7 and 10. Norms of prothrombin time (PT) at different ages:
- Newborn premature babies – 14-19 sec;
- Newborn full-term babies - 13-17 seconds;
- Young children - 13-16 seconds;
- Older children – 12-16 seconds;
- Adults – 11-15 seconds.
Anticoagulant therapy is considered effective if the PT increases by at least 1.5-2 times.
INR
INR or prothrombin ratio is the ratio of the patient’s PV to the PV of the control tube. This indicator was introduced by the World Health Organization in 1983 to streamline the work of laboratories, since each laboratory uses different thromboplastin reagents. The main purpose of determining INR is to monitor patients’ intake of indirect anticoagulants.
Reasons for changes in PT and INR parameters:
| Increased prothrombin time and INR | Decrease in prothrombin time and INR |
|
|
APTT (activated partial thrombin time, cephalinkaolin time)
APTT is an indicator of the effectiveness of stopping bleeding by plasma factors. In fact, the APTT reflects the intrinsic pathway of hemostasis, how quickly a fibrin clot forms. This is the most sensitive and accurate indicator of the hemostasiogram. The APTT value primarily depends on the activator reagents used by the doctor, and the value may vary in different laboratories. A shortened APTT indicates increased coagulability and the possibility of blood clots. And its lengthening indicates a decrease in hemostasis.
Why does the APTT change?
| Reasons for lengthening | Reasons for shortening |
|
|
Activated recalcification time
ABP is the time required for the formation of fibrin in plasma saturated with calcium and platelets. The indicator reflects how much the plasma and cellular components of hemostasis interact with each other. Its value may vary depending on the reagents used in the laboratory. AVR lengthens with a decrease in the number of platelets (thrombocytopenia) and a change in their quality (thrombocytopathies), hemophilia. A shortened AVR indicates a tendency to form blood clots.
Prothrombin index
The prothrombin index or PTI is the ratio of the ideal prothrombin time to the patient's prothrombin time multiplied by 100%. Currently, this indicator is considered obsolete; instead, doctors recommend determining the INR. The indicator, like the INR, levels out those differences in PT results that occur due to different thromboplastin activity in different laboratories.
Under what pathologies does the indicator change?
| Increasing | Decreasing |
|
|
Thrombin time
Thrombin time shows the final stage of hemostasis. TV characterizes the length of time required for the formation of a fibrin clot in plasma if thrombin is added to it. It is always determined together with APTT and PT to monitor fibrinolytic and heparin therapy and diagnose congenital fibrinogen pathologies.
What diseases affect thrombin time?
| Diseases that prolong thrombin time | Diseases that shorten thrombin time |
|
|
Fibrinogen
Fibrinogen is the first blood clotting factor. This protein is produced in the liver and, under the influence of Hageman factor, is converted into insoluble fibrin. Fibrinogen is an acute phase protein; its concentration increases in plasma during infections, injuries, and stress.
Why does the level of fibrinogen in the blood change?
| Increase in content | Content reduction |
|
|
RFMK
SFMC (soluble fibrin-monomer complexes) are intermediate products of fibrin clot breakdown due to fibrinolysis. RFMK is very quickly eliminated from blood plasma; the indicator is very difficult to determine. Its diagnostic value lies in the early diagnosis of DIC syndrome. Also, RFMK increases with:
- thrombosis of various localizations (thromboembolism of the pulmonary artery, deep veins of the extremities);
- in the postoperative period;
- complications of pregnancy (preeclampsia, gestosis);
- acute and chronic renal failure;
- sepsis;
- shocks;
- systemic pathologies of connective tissue and others.
Antithrombin III
Antithrombin III is a physiological anticoagulant. In structure, it is a glycoprotein that inhibits thrombin and a number of coagulation factors (9,10,12). The main place of its synthesis is liver cells. Antithrombin III levels at different ages:
- Newborns – 40-80%
- Children under 10 years old – 60-100%
- Children from 10 to 16 years old – 80-120%
- Adults – 75-125%.
Why does its content in the blood change?
| Level up | Level reduction |
|
|
D-dimer
D-dimer is a remnant of fibrin filaments. This indicator reflects both the functioning of the coagulation system (if there is a lot of D-dimer in the blood, it means that a lot of fibrin has been broken down) and the function of the anticoagulant system. The indicator is contained in the blood for about 6 hours after formation, so the material must be immediately examined in the laboratory.
Only an increase in the level of the indicator, which occurs when:
- thrombosis and thromboembolism of arteries and veins;
- liver diseases;
- extensive hematomas;
- coronary heart disease and myocardial infarction;
- in the postoperative period;
- long-term smoking;
- DIC syndrome;
- seropositive rheumatoid arthritis.
Bleeding time
Method of determination: pierce the earlobe with a medical needle or scarifier. Then we note the time until the blood stops. Doctors evaluate only the lengthening of the indicator, since its shortening indicates an incorrectly conducted study. Bleeding time is prolonged due to:
- lack of platelets in the blood (thrombocytopenia);
- hemophilia A, B and C;
- liver damage by alcohol;
- hemorrhagic fevers (Crimea-Congo, Ebola fever, with renal syndrome);
- thrombocytopenia and thrombocytopathy;
- overdose of indirect anticoagulants and anticoagulants.
Blood clotting time according to Lee-White and Mass and Magro
This test shows the time it takes for a blood clot to form. The method is very simple to perform: blood is taken from a vein. The material is poured into a dry, sterile tube. Time is recorded until a visible blood clot appears. If the hemostatic system is disrupted, the clotting time can be shortened or extended. In some pathological conditions (DIC, hemophilia), a clot may not form at all.
| Prolongation of bleeding time | Shortening bleeding time |
|
|
What does the APTT test show?
APTT, the norm for women by age is discussed in the article, is an accurate indicator for identifying blood clotting disorders. The essence of the analysis is to determine the clotting time of plasma when the natural process is activated “in vitro” in the presence of special reagents.
APTT allows you to measure the effectiveness of stopping bleeding by internal and general mechanisms. In the first case, this occurs in the absence of tissue damage. Tissue factor is required to initiate the extrinsic mechanism that leads to the formation of a blood clot.
At the final stage, these 2 mechanisms combine (common coagulation pathway), which ultimately promotes the formation of thrombin and fibrin, which “clog” the vessel and prevent blood loss. Subsequently, when the damaged tissue is restored, a reverse mechanism is launched, promoting the dissolution of the blood clot.
Coagulogram during pregnancy
During pregnancy, colossal changes occur in a woman’s body, affecting all systems, including the hemostatic system. These changes are due to the appearance of an additional circulation (uteroplacental) and changes in hormonal status (prevalence of progesterone over estrogens).
During pregnancy, the activity of coagulation factors increases, especially 7,8,10 and fibrinogen. Fibrin fragments are deposited on the walls of the blood vessels of the placental-uterine system. The fibrinolysis system is suppressed. In this way, the woman’s body tries to protect itself in the event of uterine bleeding and miscarriage, and prevents placental abruption and the formation of intravascular blood clots.
Indicators of hemostasis during pregnancy
| Index | 1st trimester | 2nd trimester | 3rd trimester |
| Fibrinogen, g/l | 2,91-3,11 | 3,03-3,46 | 4,42-5,12 |
| APTT, s | 35,7-41,2 | 33,6-37,4 | 36,9-39,6 |
| AVR, with | 60,1-72,6 | 56,7-67,8 | 48,2-55,3 |
| Prothrombin index, % | 85,4-90,1 | 91,2-100,4 | 105,8-110,6 |
| RFMK, ED | 78-130 | 85-135 | 90-140 |
| Antithrombin III, g/l | 0,222 | 0,176 | 0,155 |
| Platelets, *109/l | 301-317 | 273-298 | 242-263 |
In pathological pregnancy (early and late gestosis), disturbances in the regulation of blood coagulation occur. The life of platelets is shortened and fibrinolytic activity increases. If a woman does not consult a doctor and treatment of gestosis is not carried out, a very serious complication arises - disseminated intravascular coagulation syndrome.
DIC syndrome or intravascular disseminated coagulation syndrome consists of 3 stages:
- hypercoagulation - the formation of many small blood clots, impaired blood circulation between mother and fetus;
- hypocoagulation - over time, coagulation factors are depleted in the blood, blood clots disintegrate;
- acoagulation - absence of blood clotting, uterine bleeding occurs, which threatens the life of the mother, the fetus in most cases dies.
Author:
Selezneva Valentina Anatolyevna physician-therapist
When is a test ordered?
An analysis to determine APTT is prescribed in the following cases:
- Screening examination of healthy people to identify the risk of diseases.
- Analysis of pathologies of the blood coagulation system. An enzymatic imbalance (including congenital) can lead to diseases such as thromboembolism (blockage of a blood vessel by a detached blood clot), ischemia and infarction of various organs, including the brain; atherosclerosis and other cardiovascular diseases, immune and oncological diseases. If they are present, the patient requires periodic monitoring of the APTT.
- Definition of disseminated intravascular coagulation (DIC), in which a pathological process of thrombus formation in small blood vessels occurs in the body in combination with poor blood clotting, which leads to massive hemorrhages. Often this disease is asymptomatic.
- Diagnosis of hemophilia, which is a genetically determined pathology. Such people have an increased risk of severe blood loss even with minor trauma, since the blood has a very low ability to clot. Often hemorrhages occur in joints, muscle tissue, internal organs and the brain. Increased bleeding with minimal damage is detected from the first days of life.
- Monitoring the condition of the blood during treatment with drugs that have an anticoagulant effect, in particular heparin. The latter is used to treat patients diagnosed with thrombosis, pulmonary embolism, unstable angina, acute myocardial infarction, atrial fibrillation, DIC, Gasser's disease, mitral heart disease, inflammation of the heart muscle, glomerular and lupus nephritis. This drug is also prescribed for preventive purposes during operations with extracorporeal circulation, hemodialysis (blood purification) and some other medical procedures.
- Detection of antiphospholipid syndrome - an autoimmune disease in which blood clotting activity increases, which provokes thrombus formation. It is determined by the presence of lupus anticoagulant. In pregnant women, this pathology leads to an increased risk of spontaneous abortions, as well as thrombosis.
- Diagnosis of Hageman's disease. This is a very rare hereditary disease in which the activity of one of the clotting factors is reduced. It is characterized by the development of thrombosis or hemorrhagic syndrome.
- Diagnosis of von Willebrand disease. This is a hereditary disease in which spontaneous bleeding occurs due to insufficient activity of one of the factors involved in the clotting process. This pathology is characterized by prolonged bleeding, which poses a threat to the patient’s life. One of the characteristic symptoms is bleeding from the mucous membranes of the mouth and nose, spontaneous occurrence of bruises on the skin due to impaired vascular permeability. Women also experience heavy uterine bleeding lasting more than 10 days, as well as massive blood loss during childbirth. Exacerbations may alternate with periods of relative well-being.
APTT, the norm in women by age varies within the limits established by WHO, is also monitored during pregnancy every 3 months.
This is due to changes in the level of hormones that affect the circulatory system, as well as an increased risk of complications (miscarriage, stillbirth, premature birth, preeclampsia) in those patients for whom pathologies in the coagulation system have already been diagnosed.
Elevated prothrombin levels
Many factors can increase PTI and the amount of prothrombin in general. Among them, food is not the least important. Excess consumption of foods rich in vitamin K will certainly increase the PTI and decrease the INR.
These include:
- cabbage;
- green tea;
- turnips and radishes;
- pork and beef liver;
- gooseberry;
- lettuce leaves;
- soy;
- broccoli.
The range of diseases accompanied by the described changes in the coagulogram is not wide. First of all, it is erythrocytosis or polycythemia. We are talking about increasing the content of red blood cells in the blood. This also includes vein thrombosis. A more dangerous situation is disseminated intravascular coagulation syndrome, which complicates childbirth and severe operations accompanied by blood loss.
Another important group of reasons is dehydration. This condition is caused by loss of fluid from the body. It is accompanied by vomiting and frequent loose stools. The condition is dangerous for children.
Of the medications that increase PTI, vitamin K analogues come first. This is Vikasol, which is used to stop bleeding. Diuretics will cause the same changes in the coagulogram.
For women, taking oral contraceptives is more common as a possible cause. Antacids, antihistamines, and cardiac glycosides can reduce INR and increase prothrombin.
Prothrombin index in a woman during pregnancy
During this period, all systems and organs of the mother’s body are rebuilt. Therefore, pregnancy affects hemostasis parameters. There is a clear tendency towards thrombophilia, that is, coagulation factors are slightly higher than anticoagulation factors.
After all, the body must be ready for childbirth. And they, as you know, are often complicated by massive bleeding. The hypercoagulable state aims to prevent these situations.
The coagulogram norms differ for these reasons. PTI must exceed 100%. If the indicators are lower, it is necessary to search for the cause and adequately correct it.
Kwik's method
Laboratory testing of blood plasma according to Quick is done to further study the condition of liver cells and the functioning of the digestive system.
This analysis is carried out according to Quit in the following situation:
- Blood plasma clotting is impaired,
- Pathologies in the liver,
- Thrombosis,
- Blood oncology,
- Lack of vitamin K in the body.
Norms of prothrombin index by age:
- From 0 years to 6 years of age 80.0% -100.0%,
- From 6 years old to 12 years old 79.0% -102.0%,
- From 12 calendar years to the 18th birthday 78.0% 110.0%,
- From adulthood to 25 calendar years 82.0% 115.0%,
- From 25 years to 45 years 78.0% 135%,
- From 45th birthday to 65th birthday 78.0% 142.0%.
The normal percentage for women and the normative percentage for men are the same in all age periods of life.
The normal prothrombin time in children is 14.0–18.0 seconds.
For adults, this coefficient ranges from 10.0 to 15.0 seconds.
Prothrombin in the blood is high
According to the Kwiku method, prothrombin protein is high and exceeds 150.0%.
Reasons for the increase:
- DIC syndrome,
- Fibrin deficiency
- Genetic predisposition,
- The use of drugs from groups: coagulants, antibacterial agents, heparins, as well as laxatives.
You can reduce the level of prothrombin in the blood with the help of a diet with a maximum content of foods that have a blood-thinning effect:
Oatmeal porridge,
- Tomatoes, tomato juice, and beets,
- Use olive oil
- Use apple cider vinegar
- sour fruits,
- Fish, omega 3 fat.
Prothrombin increased treatment. Anticoagulants are used to reduce prothrombin.
APTT is higher - the norm, what does this mean and what are the reasons?
Provocateurs are always pathological. There are no natural factors here. Moreover, when the indicator is persistently increased over a long period of time. If we talk about specific points:
Hereditary and genetically determined disorders
For example, Hageman's disease. With it, the human body does not have enough coagulation factor XII. There are other options as well.
Regardless of the specific diagnosis, the essence is approximately the same. The quality and speed of coagulation decrease. In the most difficult cases, protein is not produced at all.
The reasons are inherited defective material from parents. It is difficult to effectively deal with such problems. We have to introduce the necessary substances artificially, from the outside. But it is impossible to radically help, because the problem is encoded in the foundation of the body.
Oncology
Especially malignant, neglected. When the tumor begins to disintegrate. The place where the neoplasia is located does not play a big role. What is more important is how quickly cells divide.
With rapid proliferation, they consume such an amount of nutrients that they die from “gluttony.” Other cancer cells don't have enough food. They die from hunger and lack of useful compounds.
In both cases, a huge amount of dead cytological structures enters the blood. They break down, leaving behind toxins. These toxic substances inhibit the synthesis of coagulation factors. Therefore, dangerous complications cannot be avoided.
Usually, by the time the tumor begins to disintegrate, the body is already exhausted. The bone marrow is working at its limit. The general asthenic condition of the patient makes the situation even worse.
Systemic autoimmune diseases
For example, lupus erythematosus. The reason for the increase in APTT is insufficient production of coagulation factors, a massive failure of all body systems. Without treatment, the pathology quickly leads to disability and then death. Coagulation disorders are part of a huge pathological picture.
Hepatitis
Liver inflammation of various origins. Most often, infectious, viral. Patients who abuse alcohol are also at risk.
Also those who receive extensive treatment for inflammation, cancer, etc. Since it is in the liver that the body synthesizes most of the coagulation factors, even the slightest deviations immediately affect the properties of the blood.
Cirrhosis of the liver
A much more dangerous condition. Another name is hepatonecrosis. That is, the death of organ cells. In a chronic course, the degree of impairment increases gradually, intensifying as the disease progresses.
Acute variants end in rapid breakdown. As a rule, there is no need to carry out analysis. Everything is obvious.
Hemophilia
A group of diseases of the circulatory system. In hemophilia, insufficient clotting factors are produced, and the aPTT increases. For what reason - you need to find out in each case separately.
Attention:
Genetically determined forms of the disease almost always occur.
Hormonal imbalances
Excessive activity of the thyroid gland, or problems with the pituitary gland as the basis for such deviations. The aPTT is elevated until the levels of specific substances return to normal.
Problems occur with iron deficiency anemia.
There is perhaps one exception. The same effect develops if the patient takes anticoagulants. For example, heparin or other drugs. Strictly speaking, this is not a disease or pathology. More like a side effect of the medication.
As soon as the medication is discontinued, the blood condition is gradually restored. Although in some cases the coagulation rate does not return to normal on its own.
Especially if heparin was used for a long time or in large dosages. In this case, special assistance will be required. Hemostatic drugs are prescribed, and other methods are possible.
If the APTT level is higher than normal, it means the blood is too thin. Diagnosis is carried out by a hematologist. Treatment is etiotropic. Its task is to eliminate the factor provoking this disorder.