The BL smear is a test for diphtheria, “BL” stands for “Leffler’s bacillus.” The disease is caused by corynebacteria, or diphtheria bacillus, which in most cases (more than 90%) affects the oropharynx, but can affect the larynx, bronchi, skin and other organs.
The main route of transmission is airborne, but infection through contact-household and oral-fecal (through food) methods is possible, especially in countries with hot climates.
The severity of the disease is due to an extremely dangerous toxin secreted by Loeffler's bacilli. Although sometimes there are non-aggressive forms, in particular, nasal diphtheria, which occurs without any complications.
Information: If the oropharynx is affected, croup may develop - narrowing of the lumen of the larynx due to the formation of a diphtheria film and swelling. This happens especially often in childhood.
What is bacterioscopy?
For doctors of various specialties, bacterioscopic analysis serves as an important diagnostic indicator when infection of an organ or organ system is suspected. Purulent skin discharge requires subsequent laboratory analysis indicating the types of bacteria that have settled and the prescription of antibacterial agents against specific pathogens.
In gynecology, smears on the flora prevent the spread of infection and the development of a more serious disease (or the transition of the pathological process to a chronic period). Bacterioscopy of feces, urine and blood has become widespread. The method for determining pathogenic bacteria is used by ophthalmologists, otorhinolaryngologists, dermatologists, etc.
Not only a purulent inflammatory process is the basis for taking an analysis. The laboratory procedure is also carried out during a clinical examination.
When deciphering the results of the analysis, attention is paid to the number of pathogenic organisms per unit of measurement, the ability of bacteria to be stained with different dyes and is the basis for dividing them into 2 large groups: gram-negative and gram-positive.
Often, protozoa and microscopic fungi are found in the analysis of biopsy specimens.
More details about Gram bacterioscopy in the video below:
Why is bacterioscopy done, indications
The results of a smear analysis of the flora provide the doctor with information about the state of the microflora of the woman’s genital organs. In particular, this could be:
- presence of pathogenic microorganisms;
- the number of beneficial microorganisms that normally populate the vaginal mucosa;
- the number of leukocytes, red blood cells and other blood cells.
In this regard, bacterioscopy is indicated for carrying out in such cases as:
- itching of the labia majora and minora;
- discomfort in the genital area;
- burning sensation;
- abdominal pain not related to the menstrual cycle;
- the presence of unusual discharge of different shades with or without odor;
- long-term treatment with antibacterial drugs.
In addition, a gynecological smear for flora is mandatory in the process of planning pregnancy, as well as upon its occurrence. In the latter case, bacterioscopy is carried out several times (at least three).
Who is it prescribed to?
In dermatology, bacterioscopy is prescribed for any suspicion of an infectious skin disease, including venereal diseases. The object for taking a smear is chancre, papules, purulent scabs and other pathological skin formations. Most often it is possible to detect staphylococci and streptococci under a microscope. If it is not possible to take a smear, scraping the skin surface is performed.
More often than others, Staphylococcus aureus causes purulent processes on the skin surface. A microorganism has a survival advantage over other organisms. Ultraviolet light, alcohol solutions, and hydrogen peroxide do not cause the death of a prokaryotic organism. The only enemy for Staphylococcus aureus is brilliant green, popularly called “brilliant green”. Under a microscope, these organisms appear as bright yellow balls collected in cluster-shaped colonies.
Other pathogenic microorganisms that affect the skin are corynebacteria and propionibacteria.
Why and how often is it carried out?
- Microscopic examination of pathogenic bacteria is carried out to differentiate prokaryotes using Gram staining. Pathogenic microorganisms are applied to a glass slide by smearing or scraping. Varieties of the pathogen, colored differently, serve as the basis for the prescription of antibacterial agents.
- Other parameters monitored in bacteriological analysis are the quantitative composition of different groups of leukocytes, the presence of cellular elements of the epithelium, individual organelles and components of damaged cells.
- Using the microscopic method, the doctor has preliminary grounds for establishing a diagnosis and the advisability of carrying out bacteriological culture in a nutrient medium.
The frequency of the analysis is determined by the treating doctor and is not limited by time frame.
Examination preparation and procedure
This analysis is quite simple. It is performed by a gynecologist or midwife.
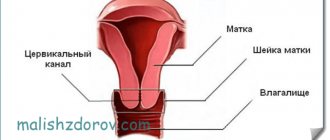
A smear is taken in three places:
- from the vaginal mucosa;
- from the base of the urethra (urethra);
- cervix.
The biomaterial is collected using a special plastic spatula. In this case, the mucous membrane itself is not injured. The procedure does not cause pain or severe discomfort.
Diagnosis is not possible during menstruation, as the sample will not be suitable for analysis under a microscope.
The technique is simple, but for its maximum accuracy a number of requirements must be met:
- a week before the study, stop taking medications that may affect the vaginal microflora (for example, antibiotics);
- at least two days before the test, avoid sexual contact;
- exclude the introduction of any drugs into the vagina (suppositories, ointments, solutions) two days before the test;
- Do not take a bath the day before the test, limit yourself to a shower.
In the evening, before the day of collection of biomaterial, it is necessary to carry out hygiene of the external genital organs without the use of detergents.
On the morning of the test, genital hygiene procedures are not performed.
It is not recommended to urinate 2–3 hours before taking a smear, since the material necessary for the study can be washed away from the urethra.
The biomaterial is applied to glass slides and sent to the laboratory.
Types of procedure
To determine the skin disease of aphids and to refer to another specialist in the presence of dermatological symptoms, it is often necessary to conduct a bacteriological analysis of several biopsy specimens, which constitutes the classification of bacterioscopy.
- Urethral smear. The procedure is 100% sterile and uses a sterile cotton swab inserted a short distance through the urethra. After removing the tampon, it must be placed in a sterile container with a stopper.
- A vaginal smear uses a spatula to run along the walls of the vagina and smear the contents onto a glass slide.
- Cervical analysis uses a swab and a speculum. The penetration procedure of the tampon is deeper than with urethral and vaginal smears.
- Bacterioscopy of urine sediment is carried out by giving urine to the patient in a plastic or glass container. In infants and newborns, urine collection requires the use of catheterization or the installation of special urine collectors. Fresh urine is required for analysis, otherwise fermentation processes begin in it and the results of bacterioscopy become unreliable.
- Bacterioscopic examination of sputum , carried out by smear. For further examination, the smear is impregnated with Ziehl fuchsin and covered with special paper. Before being examined under a microscope, the smear is heated and placed in sulfuric acid.
- Due to the huge number of bacteria in stool, pathogenic organisms are difficult to identify. Stool bacterioscopy is performed with iodine staining of the smear. The pathogenic stool bacteria most sensitive to iodine.
Read below about the indications for taking smears for bacterioscopic examination.
Algorithm for taking a throat swab
An important condition is strict adherence to the correct technique. During the procedure, you should not touch the epithelium of the throat and tongue with the instrument, since they contain Hoffmann's pseudodiphtheria bacilli.
They are very similar to real Loeffler's bacilli and have almost the same structure, but are not pathogens. If there are pockets of filmy plaque in the oral cavity, a smear is taken along the edge.
The sampling algorithm is as follows:
Taking a smear for enterobiasis
- The patient is seated facing the light source.
- In his left hand, the physician takes a sterile spatula marked Z (throat) and a test tube.
- The patient opens his mouth, and the laboratory assistant presses with a spatula on the root of the tongue, immediately removing a sterile swab from the test tube by the stopper with his right hand.
- A smear is taken with this swab, which is passed along the arches of the oropharynx and palatine tonsils, without touching the mucous membranes on the sides.
- The swab is removed and placed in a test tube, the test tube is placed in a stand, and the spatula is disinfected.
For the procedure, wooden or metal knitting needles can also be used, on which cotton or gauze swabs are wound. Before taking a smear, the latter are moistened in 9% saline solution.
Indications for testing
- Microscopic examination gives a general idea of the condition of the patient’s skin, assesses the degree of development of the inflammatory process, and visually assesses damage to the mucous membranes.
- If the microorganism is often found in dermatological diseases, then direct microscopy is the final diagnostic test option.
- Less common pathogens require further diagnosis by culture.
In particular, one cannot do without diagnostics for anthrax carbuncle, bullous dermatitis, most types of cancer, incl. cervix.
This video will tell you how to prepare a bacterial culture smear for bacterioscopy:
Carrying out analysis
All types of tests are carried out using a cotton swab soaked in the secreted pus and other secretions. Unpleasant sensations may occur during vaginal and urethral examinations.
Purulent inflammatory processes in the urogenital organs cause aggravation of pain when rotating a tampon or moving a spatula. The intensity of pain in such cases is reduced by deep breathing and efforts to relax the muscular system.
About the norm and interpretation of tests for bacterioscopy of sputum, smear, etc. for women and men, read below.
Nasal swab collection technique
Before the procedure, the patient’s nose is cleared of mucus and crusts using cotton swabs or gauze, cotton flagella soaked in saline solution. This is done carefully so as not to injure the mucous membrane, since if blood gets into the sample, the results of the study will be distorted.
The biomaterial is taken according to the following algorithm:
- The patient sits with his head thrown back.
- The physician takes a sterile tube marked “N” (nose) in his left hand and removes a swab from it with his right hand.
- Having lifted the tip of the patient’s nose, the specialist inserts a tampon with his right hand, first into one nasal passage to a depth of 1.5-2 cm, then into the other.
After removing the swab from the nose, it is placed in a test tube, being careful not to touch its walls.
Decoding the results
Smears, depending on their type, are stained with different dyes in the laboratory. Test results are prepared within 1, less often – 2 days.
The number of pathogenic bacteria is calculated differently for different laboratories, so different numbers of bacteria are considered the norm. The presence of an inflammatory process is indicated by the detection of cocci. There are 4 degrees of smear purity:
- In the first degree, a smear shows the absence of pathogenic bacteria, which is considered very rare when taking pus from skin scabs.
- The second degree indicates minor disturbances during remission of inflammation.
- The third degree diagnoses an acute inflammatory process.
- The dangerous purity of a smear is the fourth degree . Pathogenic bacteria exceed permissible limits several times. It is often a parameter of a running chronic process.
You already know about the bacterioscopic method of examining smears, its decoding, let's talk and about the prices for the procedure.
Decoding the smear
The healthy microflora of the female genital organs consists of symbiont bacteria. No pathogenic microorganisms should be detected during the analysis.
The smear contains some of the body's own cells. This is due to the fact that epithelial tissues are quickly renewed and dead cells come out along with secretions.
If local inflammatory processes are observed, cells responsible for fighting microbial invasion (leukocytes) can be found in the smear.
Bacterioscopy indicators:
- Leukocytes. Normally, their number should not exceed 10 units in the field of view for the urethra, and 30 units for the cervix. If these parameters are exceeded, this indicates inflammatory processes.
- Squamous epithelial cells. This parameter significantly depends on the phase of the menstrual cycle. If cells are not detected, this indicates degeneration of the epithelial layer. Exceeding the indicators occurs during inflammatory processes.
- Lactobacilli. They usually make up the bulk of bacteria in the healthy microflora of the vagina and cervix (up to 90% of bacterial bodies). If their number is reduced, this may be a sign of bacterial vaginosis. “Foreign” bacteria inhibit “their” normal microflora and cause inflammation.
- Yeast fungi. Normally, their number is minimal (on the verge of detection). Found in the acute phase. In the latent phase, their spores are observed in the smear. If this indicator is exceeded, this is a sign of candidiasis.
- Epithelial (key) cells. If their number is significant (20% or more), this is an indicator of inflammatory processes (bacterial vaginosis).
- Leptothrix. Normally absent, present in candidiasis.
- Trichomonas. It is the causative agent of trichomoniasis. Should not be present in the sample.
- Chlamydia. Pathogenic agents that cause chlamydia.
- Cocchi. Usually present in small quantities, their excess indicates inflammatory processes.
- Gonococcus. If it is detected, gonorrhea is diagnosed.
- Staphylococcus aureus is normally either absent or present in extremely small quantities. If its quantity is significant, inflammatory processes are observed in the vagina and uterus, the causative agents of which it is.
Based on the results of bacterioscopy, a number of diseases can be identified or excluded. For an accurate diagnosis, the results must be interpreted by a gynecologist.
Concept of smear purity
According to microscopic examination of the smear, the result is conventionally divided into four “degrees of purity”:
- First. It only happens to absolutely healthy women. All indicators are normal, there are no foreign cells, bacterial or fungal infection.
- Second. Still considered normal. Pathogenic pathogens are not detected. There are slight deviations in the vaginal microflora.
- Third. The smear reveals an excess of leukocytes, and conditionally pathogenic cocci are detected.
- Fourth. A significant deviation of the microflora from the norm is detected. Causative agents of diseases or sexually transmitted infections are identified. The number of epithelial cells and leukocytes is significantly higher than normal. This is a state of acute illness.
An ideal analytical result, such as first degree purity, is practically unattainable. It is rare in young, healthy women.
Small deviations that are observed with the second degree of purity are easily corrected. This is exactly the result of the study that most women who come for a preventive examination receive. This result is considered normal.
If the third, and especially the fourth degree of purity of the smear is observed, treatment is necessary.
A smear test must be taken before planned surgical interventions. If the degree of purity is not lower than the second, elective surgery is allowed. In the third and fourth cases, surgical intervention is postponed until the parameters are corrected.
Deviation from the norm and possible diseases
The technique is very effective - by analyzing the main indicators, diagnostic conclusions can be drawn:
- If there is not enough squamous epithelium in the smear, there is likely a decrease in estrogen or an excess of male hormones in women. The result of hormonal imbalance is atrophy of the epithelial layer.
- If the number of leukocytes exceeds the norm, then inflammatory processes are occurring in the woman’s body. The number of leukocytes is directly proportional to the strength of the inflammatory process: the more leukocytes, the stronger the inflammation.
The results of bacterioscopy are sometimes not enough. Then the doctor prescribes a bacterial culture. This study is necessary to determine the causative agent of the disease and its sensitivity to antibiotics. This will help you choose the most effective drugs.