You are here: Blood test -
Lymphocytes -
T lymphocytes
- Education and development
- Main functions
- Kinds
- Norm
- Reasons for deviations
T-lymphocytes (t-lymphocytes) - cells, precursors of agranulocytes, are formed in the bone marrow. They take an active part in the functioning of the immune system and protect the body from pathogenic influences. A decrease or increase in the number of T cells in the blood may indicate the development of a certain pathological process.
There are no specific symptoms of the disorder: the deviation of the content of T cells in the blood from the norm can only be determined by diagnostic means. The common marker of T lymphocytes is CD3. The main subpopulations are represented by five species.
Education and development
Subpopulations of T lymphocytes are found in the bone marrow; organisms are formed from stem cells. Maturation of T-lymphocytes occurs in the thymus gland (thymus), after which the cells enter the spleen, lymph nodes and begin to circulate through the blood. At this stage, their full functioning begins - ensuring the protective functions of the body.
There are two main stages in the process of cell differentiation:
- antigen-dependent differentiation of T-lymphocytes - carried out in the peripheral organs of the immune system;
- antigen-independent differentiation of T-lymphocytes - carried out only in the thymus (thymus gland).
The life cycle of T-lymphocytes is different: some cells can live for several months, others for several years and even decades. It is possible that a T-lymphocyte can circulate in the blood throughout a person’s life if it is a memory cell. Such cells are located in different places in the body and provide lifelong or very long-term immunity to a person. The cell receives similar functions after meeting a foreign organism.
What are lymphocytes in a blood test?
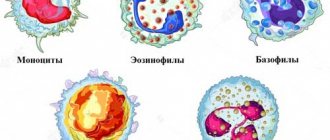
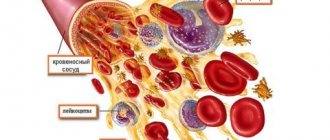
Lymphocytes are white blood cells (a type of leukocyte), through which the protective function of the human body is realized from foreign infectious agents and its own mutant cells.
Abs lymphocytes are the absolute number of a given type of cell, determined by the formula:
Total leukocyte count * Lymphocyte content (%)/100
Activated lymphocytes are divided into 3 subpopulations:
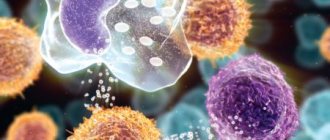
- T-lymphocytes - mature in the thymus, are responsible for the implementation of the cellular type of immune response (direct interaction of immune cells with pathogens). They are divided into T-helpers (take part in the antigen presentation of cells, the severity of the immune response and the synthesis of cytokines) and cytotoxic T-lymphocytes (recognize foreign antigens and destroy them due to the release of toxins or the introduction of perforins, which damage the integrity of the cytoplasmic membrane);
- B lymphocytes - provide humoral immunity through the production of specific protein molecules - antibodies;
- NK lymphocytes (natural killer cells) - dissolve cells infected with viruses or undergoing malignant degeneration.
It is known that lymphocytes in the blood are capable of synthesizing a number of antigens on their surface, and each of them is unique for its subpopulation and stage of cell formation. The functional activity of such cells is different. In most cases, they are targeted by other leukocytes at the immunophenotyping stage.
Cluster of differentiation and its types
Cluster designation is an artificially created nomenclature assigning numbers to various antigens that are produced on the surface of lymphocytes in the blood. Synonyms for the term: CD, CD-antigen or CD-marker.
During laboratory diagnostics, the presence of labeled cells in the general subpopulation of white blood cells is determined using monoclonal (identical) labeled antibodies (based on fluorochrome). When antibodies interact with strictly specific CD antigens, a stable antigen-antibody complex is formed, and it is possible to count the remaining free labeled antibodies and determine the number of lymphocytes in the blood.
There are 6 types of CD antigen clusters:
- 3 – characteristic of T-lymphocytes, takes part in the formation of a signal transduction complex along the membrane;
- 4 – identified on several types of leukocytes, helps facilitate the process of recognition of foreign antigens when interacting with MHC (major histoconscience complex) class 2;
- 8 – presented on the surface of cytotoxic T-, NK-cells, the functionality is similar to the previous type of clusters, only antigens associated with MHC class 1 are recognized;
- 16 – present on various types of white blood cells, is part of the receptors responsible for the activation of phagocytosis and cytotoxic response;
- 19 – a component of B-lymphocytes, necessary for their proper differentiation and activation;
- 56 - produced on the surface of NK and some T cells, necessary to ensure their attachment to tissues affected by malignant tumors.
Main functions
T lymphocytes, together with other blood cells, ensure the effective functioning of the immune system. In the human body, T cells perform a lot of extremely important tasks:
- synthesize antibodies;
- destroy foreign cells;
- responsible for immune memory;
- destroy their own mutant cells;
- provide increased sensitization of the body.
All cells of this type are morphologically identical inside, but the properties of surface receptors will differ.
Kinds
T lymphocytes come in five types, each of which performs important functions for the body. The following types of T-lymphocytes are distinguished:
- T-lymphocytes are helpers or “helpers” - present almost everywhere, “commanding” other cells that accelerate or suppress the immune response;
- cytotoxic T-lymphocytes or “killers” - kill a foreign organism due to the influence of a special substance (lymphokine), one cell can kill one pathogenic organism;
- regulatory T lymphocytes or suppressors - suppress the reaction;
- immunological memory cells - “remember” a foreign organism and when the latter enters the body again, the pathogen will be instantly identified, which will speed up the launch of the processes of its destruction.
In addition, B and T lymphocytes include null cells, which do not have the exact morphological structure and functions at birth, but can be transformed (depending on the circumstances) into B or T cells. The functions will be the same as “killers”, but their receptors are somewhat different, since the destruction of a foreign organism occurs without the development of an immune reaction. These types of T-lymphocytes do not have a certain norm in the blood of a child or an adult.
It is possible to determine which T-lymphocytes in the blood are normal and which are missing by conducting a laboratory detailed biochemical blood test.
The work of resident T cells: do not confuse tourism with emigration
In a normal situation, mouse resident tissue cells hardly move within non-lymphoid tissue and are quite firmly attached by adhesion molecules to the stroma of the organ. When resident macrophages of the same tissue initiate an inflammatory response by secreting cytokines, TRMs become more motile and patrol the nearby epithelium in search of infected cells.
If the inflammatory reaction intensifies, then the cells understand this as a signal for reinforcement: TCM and TEM cells newly arriving from the blood are connected to the work of patrol TRM. These blood cells are much more mobile and move better in the epithelium. Does this mean that it is in the blood that killer T-cells are ready to act among TEM, and CD8+ TRMs perform helper and regulatory functions in the tissue?
On the one hand, T-helpers are more tissue-specific in the spectrum of T-cell receptors, i.e. There is very little overlap between the TCR repertoires of cells taken from different tissues, while cells of the same killer T cell clone are found in different tissues among TEMs [6]. The range of functions and repertoire of antigen specificity of TRM remains to be studied, but TRM killers definitely have the ability to destroy infected tissue cells. Moreover, in a model of murine polyomavirus infection in brain tissue, the affinity of virus-specific T-cell receptors of resident killer cells is higher than that of virus-specific central memory cells [10].
However, the size of the T-cell population depends not only on the specificity of the TCR for infections that previously occurred in a given organ, but also on the homeostatic proliferation of T-cells - the proliferation of more successful cells to fill the organ's capacity according to the number of T-lymphocytes. By using the markers CD28 and CD127 on the cell surface, it is possible to distinguish cells recently and long ago activated through the TCR from those that received only a homeostatic signal to proliferation from the growth factor IL-7. As tissue ages, homeostatic cell proliferation begins to dominate over the proliferation of TCR-activated cells.
NKT cells, a type of liver-resident cell found in other tissues, often function independently of T-cell receptors. They can be activated by NK cell receptors through recognition not of individual antigens, but of general molecular patterns of danger and tissue stress. When activated, CD8+ NKT cells release cytotoxic granules and lyse suspicious tissue cells, for example, single tumor cells and virus-infected cells that express and display stress molecules on the outer membrane. With aging, the tendency of TRM to be activated without the T cell receptor, through NK cell receptors or cytokine signals, can lead to erroneous lysis of tissue cells, insufficient control of chronically infected or degenerating areas of the epithelium.
Pathological manifestations associated with the work of resident T cells include organ-specific autoimmune syndromes and chronic tissue inflammation syndromes. Examples of chronic inflammation maintained by resident T lymphocytes are contact dermatitis and psoriasis, and the mechanism is the release of inflammatory factors IL-17 by resident killer T cells and IL-22 by resident dermal helper T cells. CD8+ effector T killer cells located in the brain are similar in their set of membrane marker molecules to TRMs of the skin, intestines and lungs and are capable of promoting the development of intermittent multiple sclerosis with periodic releases of inflammatory cytokines. It is unclear, however, whether there is a normal TRM population in the brain or whether these are T lymphocytes remaining in the tissue after a neurotropic viral infection [8].
The functions of resident memory cells normally—in the absence of infection or chronic inflammation—may include cross-talk
(mutual regulation mainly through the secretion of cytokines and costimulatory molecules) with non-classical, poorly studied lymphoid cells.
They may be mucosal-associated γ/δ T cells, which carry an alternative variant of T-cell receptor assembly, or Innate Lymphoid
(ILCs), which share common features of the epigenetic landscape with T and B lymphocytes, but do not have T-/B- or NK-cell receptors [11, 12].
Drawing. 5. Proposed functions of resident T-lymphocytes of tissues.
Some functions can be performed in interaction with resident macrophages
Note ed .: γ/δT cells, making up about 5% of all T cells, are either CD8-positive or CD4-, CD5- and CD8-negative. Like natural killer cells, they are “innate” cytotoxic effector cells and do not require sensitization by antigen for activation. γ/δT cells have a tropic distribution and are found mainly in the red pulp of the spleen, the epithelium of the small intestine, and the skin. The distribution of these cells under normal conditions correlates with the localization of γ/δT-cell lymphomas. γ/δT cells are not restricted by the major histocompatibility complex (MHC – major histocompatibility complex), i.e. Antigen recognition by the T-cell receptor does not require contact on the cell surface with MHC molecules. They are the first line of defense against bacterial infections, particularly mycobacterial infections, and play an important role in the immune defense of the mucous membranes.
TRM cells come into contact with antigen-presenting tissue cells—dendritic cells of the skin and resident tissue macrophages. Resident myeloid cells in different tissues are differentiated and slightly similar to each other. For example, marginal zone macrophages of the spleen, liver macrophages, and microglia (brain macrophages) will differ greatly in both morphology and range of functions. In addition to detecting antigens in tissue, resident macrophages are involved in regulating the processes of aging and tissue self-renewal, in particular, they secrete growth factors and cytokines that stimulate the division of tissue stem cells. In adipose tissue, for example, macrophages stimulate the differentiation of new fat cells, but when they enter an activated M1 state, they trigger inflammation and, instead of differentiating, cause existing fat cells to enlarge and swell. Concomitant changes in adipose tissue metabolism lead to the accumulation of fat mass and in recent years have been associated with the mechanisms of development of obesity and type II diabetes. In the skin, cytokines released by macrophages and resident γ/δ T cells stimulate stem cell division during the regeneration of the epidermis and hair follicle stem cells [13, 14]. It can be assumed that helper TRM cells, when patrolling the epithelium and forming contacts with tissue macrophages, can modulate the spectrum and volume of growth factors secreted by the latter for stem cells, inflammatory cytokines and epithelial remodeling factors - and thereby participate in tissue renewal.
Norm
Normal values for the number of these cells in the blood will change with age - this is normal and is not considered a pathology. Until the age of six, lymphocytes will predominate in the blood, and then the function of these cells will mostly be performed by neutrophils. The decrease in the number of cells with age is due to a decrease in the size of the thymus gland, where T-lymphocytes develop and differentiate.
The norm will be the following indicators of T cells from the total number of lymphocytes by age group:
- newborns - 12–36%;
- first month - 40–76%;
- up to six months - 42–74%;
- up to a year - 38–72%;
- up to 12 years - 24–54%;
- 13-15 years old - 22–50%;
- after 16 years and throughout life - 19–37%.
A slight deviation in the indicators is not considered a pathology. Large discrepancies with the normal parameter will clearly indicate the development of a pathological process in the body. In this case, a repeat analysis is prescribed (to eliminate the possibility of error) and a comprehensive examination (to determine the cause of the development of the anomaly and prescribe the correct treatment).
How to distinguish resident tissue cells from admixtures of blood cells?
Resident T cells can be correctly, but inconveniently, determined each time by the ability of an individual cell to migrate to lymph nodes, so it is necessary to compile a list of characteristic features that can be used to identify membership in this subpopulation. Resident T lymphocytes in tissues that are the body's natural barriers (for example, in the lungs and small intestinal mucosa) are a bit like classical effector blood cells: they express the activated cell marker CD69, and the expression is stable throughout life during adulthood and aging and is characteristic of all non-lymphoid tissues. But in addition, CD69 colocalizes with the marker CD103, which denotes a group of adhesion molecules - integrins, which promote the attachment of resident T cells to the epithelium and to fibroblasts in the submucosa of the selected organ. For effector T cells in secondary lymphoid organs, the expression of CD103 integrins is completely uncharacteristic: TEM cells constantly maintain a motile phenotype.
The map compiled by Donna Farber's team has a major flaw: it is unclear how cleanly T-lymphocytes can be isolated from an organ, and what proportion of the analyzed cells are actually blood T-lymphocytes from capillaries inside the organ.
The issue of contamination by blood cells is especially acute for the lungs - it is no coincidence that the subpopulation composition of T cells in the lungs is unexpectedly similar to T cells in the blood and lymph nodes. The issue of blood cell contamination was elegantly solved for mouse T cells: experimental animals were infected with lymphocytic choriomeningitis virus after transplantation of a transgenic P14 T cell clone specific for this virus. As a result, during infection, the majority of circulating cells were represented by the virus-specific P14 clone, and its presence in tissues could be detected using fluorescent antibodies to TCR P14. Mice were injected into the blood with an anti-CD8 antibody to a marker of T-killer cells; it quickly spread through the bloodstream and bound to all T-killer cells in the blood (but not in tissues). By microscopy of organ sections, it was easy to distinguish resident killer TRMs from cells only recently released from the blood into the organ, labeled with anti-CD8 antibody []. The number of resident cells calculated by this method was 70 times higher than the number determined by flow cytometry; a difference of less than twofold was observed only for resident cells of the lymph nodes and spleen. It turns out that standard methods for isolating lymphocytes from organs are poorly suited for the analysis of killer resident cells and significantly underestimate the size of the population.
Possible reasons for deviation from the norm
Non-pathological reasons for an increase in the number of T cells in the blood:
- excessive physical activity;
- stress, emotional arousal;
- drinking alcohol;
- time period before and after menstruation (in women)
- pregnancy.
As for pathological factors that can cause deviations from the norm, the following should be highlighted:
- diseases of the central nervous system;
- autoimmune and systemic diseases;
- chronic pathological processes;
- endocrine disorders;
- some viral diseases;
- recovery period;
- infectious diseases;
- side effects of certain medications;
- oncological processes;
- secondary immunodeficiency;
- consequences of radiation and/or chemotherapy;
- acute or chronic circulatory failure;
- allergic reaction.
In such cases, there is an abnormality of not only T cells, but also other blood components. It is impossible to determine the cause of the disorder using only one biochemical analysis; a comprehensive examination is required.
There are no specific drugs that would affect the number of T-cells in the blood. Periodically you need to undergo a medical examination or at least take a blood test. Such simple preventive measures will allow you to timely diagnose the problem and begin treatment.
Resident T cells in aging human tissues
A map of the relationships between the presence of individual subpopulations of T cells in different human organs, oddly enough, was compiled only in 2014. Donna Farber's team from Columbia University Medical Center in New York compared the phenotypes of T cells isolated from the blood and tissues of organ donors of all age groups from 3 to 73 years (total 56 donors) [6]. Analysis of T cell subpopulations using flow cytometry confirmed many data obtained using methods with lower resolution and lower statistics, and some features of the description of the immune system transferred from mouse immunology to humans, for example, a decrease in the content of naive T lymphocytes in all organs during aging of the body .
The decline in the number of naive T cells with age is associated with the rapid aging of the thymus, in which future T cells undergo the stages of TCR assembly, testing its functionality, and selection for lack of autoimmune potential. It is important not only to reduce the absolute number of naïve T cells, but also to reduce the diversity of the T-cell receptor repertoire, and therefore the ability to form an adaptive immune response to a previously unfamiliar infection [7]. For naive killer T cells, a progressive decline in abundance in the blood and lymph nodes was confirmed, although for naive helper T cells the negative correlation of abundance with age in this study was significant only for secondary lymphoid organs, but not for the blood.
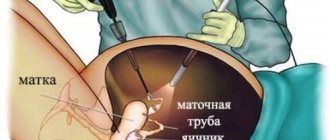
Drawing. 4. Circulation pathways of T-lymphocytes of various subpopulations [8].
Naive T cells, together with the TCM subpopulation, travel through blood vessels and enter the T-cell zone of various lymph nodes; they do not enter the tissues, although they are found in their capillaries ( red trajectory
).
Effector TEM cells move through the lymph and bloodstream, can enter the lymph node, but do not enter the T-cell zone ( purple trajectory
).
Resident TRM cells (shown in green
in the skin and
different colors
in the mucous membranes) move only within the tissue (
green trajectory
)
Isolation of memory T lymphocytes, memory effector cells and short-lived effector cells from the mucous membranes of the lungs, small and large intestines, inguinal and mesenteric lymph nodes of organ donors made it possible for the first time to assess the dynamics of these populations in human tissues during aging. The proportion of central memory cells expectedly increases over the course of life, in accordance with the increase in the number of infections that the body has encountered and entered the memory library of the immune system. TEM effector memory cells rapidly fill the T cell niche in the child's tissues, quickly displacing naïve T cells by about 12 years of age. The number of terminally differentiated effector T-killer cells (TEMRA) also increases, but only in the lymph nodes and spleen; in nonlymphoid tissues, TEMRA abundance decreases. Short-lived terminally differentiated killer T cells are most often found in the blood, spleen and mucous membranes of the lungs at any age, but among T helper cells this subpopulation is represented by a vanishingly small number of cells. Similarly, there are few central memory cells among T-killers; they are predominantly located in the mucous membranes of two barrier tissues: the lungs and intestines.
In broad strokes, the distribution map of human T-lymphocytes can be outlined as follows: naïve T-cells travel through the blood and periodically enter secondary lymphoid organs; TEMRA killers are found in the blood, spleen and lungs. Apparently, central memory cells are characterized by a more individual distribution across tissues than other subpopulations: in any case, patterns of dynamics during aging of different tissues could not be identified. Effector memory cells, including the TRM subpopulation, dominate among T cells of mucosal barrier tissues. In general, with aging of T-cell immunity, non-lymphoid tissues show greater stability of subpopulations, while lymphoid tissues show greater age-related dynamics of T-cell types [6]. The stability of tissue cells is easier to explain if we understand which of the TEM effector cells remain in the tissue, become resident TRMs, and what events their life consists of after they stop traveling throughout the body.