In some cases, after examination of a man and woman planning to conceive a child, no abnormalities in their reproductive health are revealed, and the desired pregnancy never occurs. In such situations, reproductive specialists may recommend that the couple undergo a test such as a test for the compatibility of partners for conception (or a post-coital test). This laboratory examination method allows us to identify immunological infertility, in which, due to certain features in the functioning of the woman’s immune system, conception cannot occur. In this article you will become familiar with the essence, indications, methods of preparing and taking an analysis for the compatibility of partners for conception. This information will help you get an idea of this method of diagnosing infertility, and you will be able to ask your doctor any questions you may have.
This type of infertility is called immunological, because for some reason a woman’s immune system produces antisperm antibodies (AST or antibodies to sperm), which cause their immobility and death. When they are detected, they speak of the immunological incompatibility of the couple.
The postcoital test detects the presence of antisperm antibodies in the cervical mucus, through which sperm pass from the vagina to the uterus. The purpose of such a study (or such modifications as the Kurzrock-Miller or Shuvarsky test) is to clarify the interaction between cervical secretion and sperm.
How the phase of the menstrual cycle affects the state of cervical secretion
Cervical mucus during the period of ovulation ensures that the healthiest sperm enter the uterine cavity as quickly as possible. Before answering this question, let's consider the functions of cervical mucus during ovulation - the most favorable period for fertilization of an egg.
Normally, during ovulation, cervical mucus performs the following functions:
- provides favorable conditions for the advancement of sperm into the uterine cavity and fallopian tubes;
- protects male reproductive cells from the acidic environment of vaginal secretions;
- “selects” the strongest and most viable sperm;
- helps selected male reproductive cells accumulate energy;
- ensures the launch of the capacitation reaction, which allows sperm to transform and become capable of conception (i.e., penetration into the egg).
Before and after the ovulation period, cervical secretion becomes more viscous, and its main function is to protect the uterus from infectious agents. In addition, viscous mucus retains sperm.
The secretion of the cervical canal is produced by the cylindrical epithelium located in the cervix. Depending on the level of sex hormones, cervical mucus changes its properties throughout the cycle:
- Follicular phase. During this phase, starting from the 1st day of monthly bleeding before the onset of ovulation (from 1 to 13-14 days in a standard cycle of 28 days), estrogen levels gradually increase. As long as it remains low, cervical mucus has a viscous consistency.
- Ovulation phase. In a standard cycle, the release of the egg from the ovary occurs around day 13-14. The level of estrogen and luteinizing hormone increases in the body. Under their influence, the secretion becomes more liquid and watery. In its thickness, peculiar pores appear, which enable sperm to enter the uterine cavity. In addition, the secretion acts as a filter that filters out weakened male reproductive cells. Once in the cervical mucus, sperm remain viable for several days and during this time accumulate the energy necessary for further movement.
- Corpus luteum (or luteal) phase. This period begins after the completion of ovulation and ends on the first day of menstruation. The composition of cervical mucus at this time is influenced by androgens, progesterone and estradiol. These hormones increase its viscosity and density, the number of cellular elements in it increases, and sperm cannot enter the uterine cavity.
The above-described features in the composition of mucus are important when conducting a postcoital test, since failure to perform the analysis in a timely manner can give false positive results.
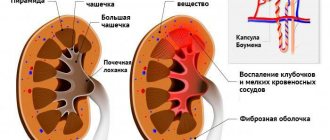
About HLA
All cellular structures of the human body have a specific type of receptor - antigenic proteins of a large region of the genome or a large family of genes, which are the most important for the immune system (major histocompatibility complex (MHC)). These receptors themselves are unique; their task is to ensure the reliable functioning of the immune system according to the “friend or foe” rule. If the receptor composition is changed (a foreign organism is detected or the cellular structure has been transformed into a malignant one), then the antigen binds to immune cellular structures, and thanks to the HLA complex, a response of the immune system occurs.
Basic properties of cervical secretion
The possibility of fertilization can be influenced by various properties of cervical mucus:
- Viscosity. This parameter depends on the concentration of proteins and ions, molecular composition, and the number of cellular elements. Before the release of the egg from the follicle, the viscosity of the secretion decreases significantly, and before the onset of menstrual bleeding it reaches its maximum.
- Extensibility. This parameter reflects the elasticity of cervical secretion. During ovulation, this figure is 12 cm, and in other phases it is less than 4 cm.
- Crystallization. This parameter can be examined after the selected material has dried on the slide. Before ovulation occurs, the secretion forms images on it that resemble fern leaves.
The above parameters are assessed using another special analysis - the cervical mucus index.
Immunization
When, after consultation with a doctor, a couple decides to continue trying to conceive a common child, an active or passive immunization procedure may be recommended.
Active immunization of the mother is carried out with a concentrated culture of lymphocytes from a partner or donor, and allows one to overcome the problem of similarity of partners in HLA antigens. The procedure should “teach” the female body to recognize the partner’s cells. Typically, the procedure is carried out in three stages using a drug that is made from the blood of a partner or donor. To date, the opinions of geneticists and immunologists on the effectiveness of immunotherapy with lymphocytes are divided in half. On one side, this method is considered a means of salvation, while on the other, its entire meaning is completely denied.
Some data indicate that a carefully selected and timely prescribed method of active immunization is 60% effective. Unfortunately, the procedure for immunization with lymphocytes can now only be completed in some large cities.
Passive immunization is more accessible and does not require a long preparation period, but data on its effectiveness are conflicting. This method consists of immunizing the mother using immunoglobulin preparations. The drug is prescribed exclusively by a doctor, usually intravenously, in three stages.
The importance of these tests is that they provide the couple with the opportunity to make an informed choice when weighing the risks of continuing to try to conceive or opting for egg and sperm banking. Therefore, before making such a serious decision, it is necessary to have the relevant information and enlist the opinion of several immunologists and geneticists.
How to properly prepare for analysis
How to determine the test date
Measuring a woman's basal temperature every day will help determine the days of ovulation.
The phases of the menstrual cycle affect the properties of cervical mucus and therefore a compatibility test for conception should be performed 1-2 days before ovulation. With a standard cycle, such a test is usually performed on days 12-13 of the cycle.
In order to accurately determine the date of expected ovulation, and therefore the day the analysis is performed, it is necessary:
- find out the date of the first day of the last menstrual bleeding (more than half of women ovulate on the 13th day);
- measure basal temperature and draw up a schedule for 3-4 cycles - rectal temperature before getting out of bed in the morning begins to be measured from the first to the last day of the cycle, according to the chart, the day of ovulation is determined (when it occurs, the temperature rises to 37 ° C);
- carry out ovulation tests - the analysis allows you to determine the day of a sharp increase in the level of luteinizing hormone, which indicates the approach of ovulation;
- conduct an ultrasound of the ovaries to study the condition of the follicles - with visualization, a specialist can determine the maturity of the egg in the follicle and its readiness for opening.
Additional Research
3-4 days before the post-coital test, the couple should undergo a series of diagnostic tests:
- tests for sexually transmitted diseases (STDs) - these studies are necessary for a woman, because such infections can affect the quality of cervical secretion and make it unsuitable for sperm;
- spermogram - this analysis allows you to determine the number and mobility of male germ cells in a man’s sperm and their suitability for conception.
How to prepare for the test
Before taking the test, the woman must be completely healthy, since the reliability of the results can be affected by recent viral or infectious diseases (for example, ARVI), stress, changes in climatic conditions or dietary patterns. These factors can trigger earlier or later ovulation. Untreated sexually transmitted infections can have a particularly negative effect on the results of the analysis, since sloughed endometrial or vaginal cells make the mucus of the cervical canal more viscous.
You need to start preparing for the test to determine the compatibility of partners for conception 3-4 days in advance (i.e., from the 10th day of the cycle):
- Avoid sex 3-4 days before the test.
- Do not take medications that can affect the onset of ovulation (Tamoxifen, Anastrazole, Clostilbegit, etc.).
- Do not use forms of medications inserted into the vagina (suppositories, suppositories, pellets, tablets or creams).
- Avoid vaginal contraceptives and do not use lubricants.
- The day before, 4-6 hours before the test, sexual intercourse should take place. After sex, you should not immediately get out of bed. You need to stay in a lying position for about 30-40 minutes. After sexual intercourse, you should not wash yourself, take a bath, douche, or use tampons. To prevent the leakage of sperm, you can use a panty liner.
What causes the incompatibility of spouses at the genetic level?
In the human body, all cells contain special proteins on their surface that help them recognize foreign substances and fight them to protect the body.
Having recognized a foreign object, the cell sends a signal to produce protective antibodies (immunoglobulins of different classes). They move towards the object and destroy it.
The embryo carries two genetic components: half from the mother and half from the father. When these data do not match, the woman’s body recognizes a condition such as pregnancy and produces protective antibodies for the fetus and placenta. This is what avoids natural rejection of the embryo and allows the child to grow and develop normally in the womb.
When the genotype of the father and mother are too similar to each other, the woman’s body does not understand that pregnancy has occurred. He perceives the embryo as his own, but modified cells. Considering this a pathology similar to a cancerous tumor, the body begins to produce antibodies against the embryo, which prevents the fetus from settling in the uterus or contributes to its rejection and miscarriage.
There are no people with the same set of genes.
How material is collected for analysis
Typically, material collection for a postcoital test is carried out in the morning:
- The woman undresses and lies down on the gynecological chair.
- The doctor inserts a speculum into the vagina to provide access to the cervical canal.
- The material is collected using a special pipette or a disposable syringe without a needle. Mucus is taken from the cervical canal and posterior vaginal fornix.
- The resulting sample is applied to glass and covered with a second glass. Their edges are filled with paraffin to ensure sealing.
- The glasses are sent to the laboratory.
What factors can negatively affect the reliability of the results?
Unreliable test results for the compatibility of a man and a woman for conception can be observed in the following cases:
- the test was not taken during the ovulation phase;
- more than 4-24 hours have passed since sexual intercourse;
- the presence of inflammatory diseases of the genital organs or urogenital infections in a woman;
- hormonal imbalance, manifested by a decrease in the level of estrogen, affecting the viscosity of cervical secretions;
- hormonal drugs or spermicides were used;
- a small amount of sperm or decreased sperm motility during the last sexual intercourse.
Immunological incompatibility associated with blood factors and methods for its study
This type is related to blood factors such as blood type and Rh. This type cannot be called a complete discrepancy. There is no combination of blood groups that would prevent pregnancy. The same applies to rhesus. But if there are other reasons that make it difficult to conceive or bear a child, certain combinations may affect the process of pregnancy. For example, a Rh conflict is possible if the expectant mother is Rh negative, and the fetus inherited the presence of the Rh factor from the father. Group incompatibility can arise if a woman has blood type I, and her baby has any other (such a conflict is possible, but it does not occur often). These factors can cause pregnancy failure at a period of up to a month, which is mistakenly considered by couples to be an inability to conceive a baby, and at a later stage, when pregnancy failure is obvious. The study, aimed at determining the blood type and Rh factor of each of the partners of the couple, requires blood sampling from both partners.
results
The results of the analysis for the compatibility of partners for conception may be as follows:
- positive - in the selected sample, 25 sperm with sufficient motility were identified and the woman has a very high chance of pregnancy;
- satisfactory - in the selected sample, 10 or more sperm with straight motility were identified and the woman has a high chance of pregnancy;
- doubtful - in the selected sample, from 5 to 10 sperm with low motility were detected and the woman has a low chance of pregnancy or the test was not performed before ovulation;
- bad - only immobile sperm were detected in the selected sample, i.e. the probability of pregnancy is extremely low or absent;
- negative – no sperm are found in the cervical secretion (for example, due to a violation of the entry of sperm into the vagina or ejaculation).
There are many factors that can influence the reliability of the results of this analysis. That is why experts recommend not limiting yourself to passing only one test. A single negative or poor result of a postcoital test is not yet a reason for making a diagnosis of “immunological infertility.” This final diagnosis can only be made after receiving 3 negative results from a fertility compatibility test indicating the presence of sperm-killing antisperm antibodies in the cervical mucus. Tests are performed in different menstrual cycles at intervals of 2-3 months.
Analysis of the compatibility of partners for conception: indications, preparation, methodology
In some cases, after examination of a man and woman planning to conceive a child, no abnormalities in their reproductive health are revealed, and the desired pregnancy never occurs. In such situations, reproductive specialists may recommend that the couple undergo a test such as a test for the compatibility of partners for conception (or a post-coital test). This laboratory examination method allows us to identify immunological infertility, in which, due to certain features in the functioning of the woman’s immune system, conception cannot occur. In this article you will become familiar with the essence, indications, methods of preparing and taking an analysis for the compatibility of partners for conception. This information will help you get an idea of this method of diagnosing infertility, and you will be able to ask your doctor any questions you may have.
This type of infertility is called immunological, because for some reason a woman’s immune system produces antisperm antibodies (AST or antibodies to sperm), which cause their immobility and death. When they are detected, they speak of the immunological incompatibility of the couple.