Bile pigments
An important indicator when taking urine tests is bile pigments. An increased amount of urobilinogen in the analysis may indicate the cause of certain diseases of the body. This substance is formed as a result of the breakdown of hemoglobin, as well as other proteins in the body that contain it. This pigment is found in bile, which gives it its yellow color.
Among the analysis indicators, the most valuable is bilirubin, as well as the products of its transformation; they, in turn, are formed in the intestines under the influence of microflora (bilirubinoids). To detect them, urine is checked very carefully. Urobilinogen also plays an important role. The doctor must consider its significance, and if urobilinogen is detected in the urine, what this means must be explained to the patient. If necessary, send for further examination.
How could this be dangerous?
In medicine, the occurrence of urobilinuria is associated with several defining factors. The primary cause is the intensive breakdown of red blood cells. Hemoglobin is the material that forms bile, which determines the degree of urobilinuria.
Reference ! Among the most important characteristics is the ability of the liver to take the bulk of urobilinogen from the blood. When this property is impaired, the liver cannot cope with the uptake of a significant mass of urobilin. As a result, the part that is not captured passes into the urine.
Urobilinuria is also caused by:
- putrefactive processes in the intestines;
- the presence of various diseases, such as hemorrhagic diathesis, lobar pneumonia and others;
- early symptoms of liver cancer, developing cirrhosis;
- congestive liver, as an initial sign of cardiac decompensation.
Urobilinuria confirms the presence of infectious diseases (pulmonary tuberculosis and endocarditis). Basically, this diagnosis is associated with weakened liver function, which manifests itself in pulmonary emphysema.
Urobilinoids
Any healthy person has a certain amount of urobilinogens in their urine. After oxidation in urine, they are converted into urobilins. In order for urobilinogen to completely transform into urobilin, urine must stand in the light for at least a day. For this reason, the determination of urobilinogen in urine is carried out using fresh tests.
To determine the amount of urobilin, standing urine is examined. It has a yellowish tint, whereas urobilinogen has no color in urine. This explains the fact why, after standing in the light, urine darkens. These substances (urobilinoids) are derivatives of bilirubin, which, in turn, is excreted in bile. In terms of their chemical composition, urobilinoids have a similar structure. If bilirubin has not reached the intestines, then these substances are not detected. This happens for a number of reasons: hepatitis, blockage of the bile ducts, fistulas.
How does urobilin appear?
Before explaining exactly how urobilin appears in the urine, it is necessary to recall the elementary chemical transformations of the substance in the body. A biochemical chain of decay forms these cells, which are found in some quantities in urine submitted for analysis.
The normal life cycle of red blood cells in human plasma is 120 days (about 4 months). Subsequently, non-viable cells enter the spleen, which destroys them. As a result of the breakdown, a hemoglobin cell is obtained, which undergoes many chemical changes in its composition. The result of this process is unbound bilirubin and many other components not considered in this issue.
Due to the intensity of the blood flow, bilirubin is delivered to the liver, which, with its enzymes, transforms the bilirubin molecule into a bound form. In this form, the cell, along with bile, is sent through the ducts to the duodenum. After several stages of transformation in this system and acidic reactions, the substances are released along with feces (stercobilin is detected) and with urine (urobilin cells).
More on the topic: Causes of a weak stream during urination in men
If the substance is contained in the body in an amount less than normal, this indicates a neoplasm in the bile ducts in the form of stones, due to which bile cannot flow into the intestines. The condition of increased urobilin is called urobilinuria.
How are they formed?
Urobilinogen is formed from red blood cells (up to 80%), to be more precise, from bilirubin, which, in turn, is synthesized from hemoglobin. At its core, urobilinogen is nothing more than a product of red blood cell utilization. How does the process work? Having served their due period, hemoglobin molecules must be disposed of. First, indirect bilirubin is synthesized from them, and it enters the intestines with the flow of bile. Under the influence of microflora, bilirubin undergoes further transformations. Multiple complex biochemical reactions help form a series of intermediate substances. Some of them (mesobilinogen, stercobilinogen) are reabsorbed into the blood, and some are excreted in the feces. The part that enters the blood is recaptured by liver cells. Urobilinogen is again excreted with bilirubin in bile. A small part of the blood passes past the liver through hemorrhoidal anastomoses. Thus, part of the urobilinogen enters the urine. For various reasons, its quantity may be different. If urobilinogen is present in the urine, what does this mean, we will consider further.
Reasons for decreased urobilin
A complete absence of urobilin in the urine can be observed in situations where the direct bilirubin molecule does not reach the intestinal lumen, and, therefore, all further biochemical transformations do not occur.
This can be observed with complete obstruction of the biliary tract (stone, tumor, pathological kinks of the ducts), or with the formation of fistulous tracts through which bile exits into the abdominal cavity or other anatomical structures.
A sharp decrease or complete absence of the filtration capacity of the glomerular apparatus is manifested by the absence of urobilinoids in the urinary sediment (for example, with a “shock” kidney, severe glomerulonephritis, and others).
Norm
In a healthy person, the urine of urobilinogen contains a tiny amount, so when it is determined, tests show a negative result. From here it is clear that the numbers do not indicate urobilinogen in the urine (the normal reading is 5-10 mg/l), but simply put the result “+” in the value. A weakly positive reaction is “+”, “++” is positive and “+++” is strongly positive. Some conditions affect these indicators. If urobilinogen levels are elevated, a diagnosis of Urobilinuria is made.
When analyzing urine, it is very important to determine the level of urobilin. Based on these readings, the doctor can judge how the urinary system works. The normal color of urine is slightly yellowish and transparent. If dehydration occurs in the body, the amount of water in the urine decreases sharply, and urobilinogen becomes more concentrated. As a result, the urine becomes darker. Also, certain medications, various diets, and alkoptonuria (hereditary disease) can affect its color.
Tests to determine
Every technical laboratory requires a urine test. It refers to screening diagnostic methods.
If a deviation of indicators from the norm is detected, narrow specialists note the presence of pathological processes in the patient’s body. In this situation, the doctor sends feces and urine for an extended examination. When necessary, other diagnostic instrumental studies are performed. You can also determine the exact diagnosis and course of therapy after consultation with specialists.
You should consult a specialized doctor if small portions of urine are dark yellow or brown.
The hue of such urine may be similar to dark beer. In such a situation, it is necessary to clinically examine the urine for the presence of urobilinogen. Urine collection must be carried out in an opaque container with a hermetically sealed lid. It needs to be quickly delivered to the laboratory.
Attention! In cases where the laboratory is located far away, screening tests . Specially designed test strips are placed in a selected container of urine.
The impregnation consists of stabilized diazonium salt. This strip in an acidic environment under the influence of urobilin changes color from white to cream. Also changes to various shades of red.
The exact level of urobilinogen can be determined according to how intense the staining occurs:
- A specially designed scale will allow you to accurately determine this indicator associated with the presence of urobilin.
- If an increase above normal is detected, a clinical examination should be performed.
Based on the results, the specialist will prescribe an effective treatment regimen.
A general clinical blood test helps to indirectly understand that this parameter is higher than normal Based on its results, an increase in bilirubin is determined. It is assessed in different factions. Based on the degree of increase in indicators, we can talk about the level of severity of the disease.
How to use biochemical test strips for urine at home is described in the video:
Increased performance. What do they mean?
As we found out, normally the urobilinogen level is negative - its amount in the urine is so insignificant. In what pathologies can the level of this indicator in the blood increase, in which case does urobilinuria occur? First of all, urobilinogen in the urine is increased in chronic, acute liver pathologies; in those conditions when red blood cells are destroyed, the intestines do not function normally. Namely when:
- cirrhosis, hepatitis of the liver;
- malignant or benign tumor;
- congestion in the liver;
- hemolytic anemia, in this condition there is a complete breakdown of erythrocytes (red blood cells);
- poisoning with chemicals, when red blood cells also disintegrate, hemoglobin in this case appears freely in the blood plasma; this, in turn, increases the formation of bilirubin, and it is excreted in bile (as we have already found out, urobilinogen is formed from bilirubin).
The following factors also influence the increase in the indicator:
- Inflammatory, chronic bowel diseases.
- Chronic constipation.
- Parasites.
- Intestinal obstruction.
An increase in urobilin, as many doctors say, is not an obvious pathology, but only indicates the possibility of its presence. So, in some conditions, when excess waste is released into the intestines (for example, with diarrhea), the kidneys receive additional stress, as a result - the presence of urobilinogen in the urine. This only confirms that the kidneys are doing their job.
Mechanism of urobilinogen formation
Urobilinogen and urobilin belong to the group of urobilinoids (urobilin bodies). These are organic substances that are derivatives of one of the main components of bile - bile biochrome (pigment) bilirubin, formed during the breakdown of proteins. Biochemical transformations in the body occur in a certain sequence.
The initial basis is the protein hemoglobin, which is part of erythrocytes (red blood cells). Complex compounds (heme) are formed from it, then an intermediate breakdown product of hemoglobin (biliverdin) is formed, then bilirubin. The pigment accumulates in the gallbladder, from where it enters the intestine through the bile duct system.
Intestinal microflora, including enzymes and bacteria, converts bilirubin into urobilinoids (urobilinogen and stercobilinogen). 95% of urobilin bodies remain in the organs of the digestive system and are excreted in excrement. The rest is subject to reverse resorption (absorption) into the systemic circulation.
Partially, urobilinoids, along with the blood, return through the portal veins to hepatocytes (liver cells), where they again become participants in the exchange of bilirubin. Partial bile pigments move to the kidneys. During circulation, part of the urobilinogen is transformed into urobilin, so both substances are present in the final excreted product (urine).
Urobilin in urine gives the biofluid a characteristic yellowish tint. Under the influence of oxygen, mesobilirubinogen is oxidized and converted into urobilin. When the mechanism of formation and utilization is fully operational, bile pigments in the urine (mesobilirubinogen and urobilin) are contained in minute quantities.
An increase in their concentration or complete disappearance is abnormal for the body. Bilirubin is not determined when examining healthy urine, since it is excreted from the body through the intestines (without affecting the urinary system). Bilirubinuria (the presence of pigment in the urine) occurs against the background of its elevated level in the blood as a sign of diseases of the hepatobiliary system.
Reference! The normal level of total bilirubin in the blood for adults and children (excluding newborns) ranges from 8.5 to 20.5 µmol/liter.
All bile pigments are in close correlation. The development of pathological changes in the digestive system is reflected in the overall quantitative content of pigments in biofluids (urine and blood) and their ratio to each other.
Reasons for the increase
Summarize. What does urobilinogen show in urine? Either excess production of bilirubin by the liver, or slow utilization of it. Such symptoms appear in liver diseases (cirrhosis, hepatitis) or in hemolysis (the process of destruction of red blood cells).
What other reasons for the increase exist:
- severe pathological changes in the spleen;
- poisoning with poisons, toxins;
- blood transfusion of inappropriate group, Rh factor;
- alcoholic liver damage;
- liver failure as a consequence of myocardial infarction;
- enterocolitis, ileitis;
- thrombosis, hepatic vein obstruction;
- insufficient fluid intake, excessive excretion.
How is urobilinogen produced?
What bilirubin is in its pure form has been known to everyone since school; it is very dangerous for the body due to its toxicity. Albumin, aka protein, like bilirubin, is also found in the intestines. After combining bilirubin with proteins, the mass becomes non-toxic and penetrates the hematopoietic system. In this case, a number of biochemical processes are carried out in which protein in the urine is involved. It plays one of the main roles, since it is with its help that bilirubin is formed, and, accordingly, urobilinogen.
Partially it is washed out into urine; such traces in a volume of about 4 mg per day are considered an acceptable indicator. Some blood moves through hemorrhoidal anastomoses without filling the liver. Regardless of the patient’s age, such cells are found in urine, enlarged in liver diseases, inflammation of any organs, toxic lesions of the body and hemolytic jaundice. Also, exceeding its permissible levels can occur with gastrointestinal diseases, for example, with poisoning or prolonged constipation.
Urobilinogen in urine during pregnancy
This pigment becomes highly concentrated when liver function is impaired. This may be caused by a hereditary predisposition or diseases such as cholestasis, hepatitis. If a pregnant woman has increased urobilinogen in her urine, it darkens and takes on the color of dark beer.
Another reason for the increase in the concentration of urobilinogen in the urine may be toxicosis, which contributes to increased fluid loss. In this case, the indicator fluctuates between 20 - 35 µmol/l.
Many pregnant women, upon receiving the test result, are interested in what such a high indicator means. Only an obstetrician-gynecologist can give such advice at an appointment, and perhaps send you for additional examinations.
After carrying out diagnostic measures, the doctor will make a conclusion about whether elevated values indicate toxic damage to the body or the development of blood pathology.
If you are sure that darkening of urine is in no way connected with fluid deficiency, increased fluid losses, or the use of any medications, then be sure to consult a specialist; dark urine is an alarming signal.
Exceeding the norm, which is not a pathology
In some cases, the discrepancy between the results obtained and normal values is considered acceptable and does not indicate pathology. Typically these conditions are as follows:
- in a child under four months of age who is breastfed before the start of complementary feeding, urobilinoids are not observed in the tests, since they cannot be formed in the absence of intestinal-type bacteria;
- in a child who has just been born, an unprecedentedly high rate is recorded that is not associated with physiological jaundice;
- During pregnancy, some deviation from the normal values is possible, but only until the urine turns brown. It signals a dangerous disease;
- when the body is dehydrated against the background of a high concentration of urine, the amount of urobininoids can be high without the development of pathology. This can be easily corrected by drinking a lot of water;
- complex forms of dysbiosis provoke the death of bacteria needed by the body, which form bilirubin.
More on the topic: How are bladder polyps treated in men?
Urobilinogen in the urine of a child
The daily concentration of urobilinogen in the urine of an infant should not exceed 2 mg/l. If this figure is exceeded, the following diseases are suspected:
- hepatitis;
- cholelithiasis;
- cirrhotic liver damage;
- hemolytic anemia;
- severe colitis;
- other infections.
To find out the true cause, you should familiarize yourself with the characteristics of the infant’s developmental period. In infancy, the body mainly adapts to the surrounding world, the external environment. Jaundice is characteristic of newborns; it is caused by the breakdown of fetal hemoglobin (hereinafter referred to as red blood cells). As a result, an increased amount of urobilinogen is formed, which is found in the urine. The phenomenon of jaundice at this age is temporary, so increased urobilinogen in the urine is the norm for newborns.
Urobilinogen in children
Colorless urine in infants is an indicator of the norm, when urobilinogen is not formed in the urine and is absent from research results. The intestinal tract in children is not able to produce urobilin and bilirubin. If the levels of these substances in children are exceeded, this indicates some kind of pathology in the functioning of the body. Upon reaching the age of 1 year, the level of urobilinogen in the urine of a child is calculated in the same way as for an adult.
More on the topic: How to prepare for an ultrasound of the genitourinary system?
Reduced urobilinogen
What if urobilinogen is not present in the urine? What does this mean? Doctors do not consider the absence of urinobilinogen in the urine as a valuable indicator, but this cannot be classified as normal. If this substance is completely absent in the urine, but bilirubin is detected, this may indicate blocked bile ducts or subhepatic jaundice. This is also a characteristic symptom of hepatitis A.
If bile does not enter the intestinal lumen, this also causes a decrease in urobilinogen in urine. The pigment concentration may also decrease in large volumes of urine in cases where fluid intake is exceeded (with some fruits).
Deviations of indicators
Non-compliance with standard indicators, that is, an increase in the concentration of urobilinogen or its complete absence in the urine, is a clinical sign of pathologies. First of all, the attending physician prescribes an additional examination of the kidneys and liver, using ultrasound (ultrasound), a general clinical and biochemical blood test. If necessary, an enzyme-linked immunosorbent test (ELISA) is performed.
The reasons for the increase in bile pigments may be the following:
Urinalysis for creatinine
- infectious hepatitis (A, B, C) and hepatitis of other origins (autoimmune, alcoholic, drug);
- obstructive (mechanical) jaundice;
- cirrhosis of the liver;
- hepatosis of various etiologies;
- inflammatory, infectious diseases of the gastrointestinal tract (gastrointestinal tract);
- invasion of liver parasites (opistarchosis);
- malignant or benign formations in the organs of the digestive system;
- inflammation of the bile ducts (cholangitis);
- long-term intoxication of the body;
- changes in blood composition associated with the destruction of red blood cells (hemolytic anemia);
- disturbance of water balance in the body.
You can read more about the reasons for the increase in urobilinogen and methods for stabilizing indicators in this article. If urobilin is absent in urine, this indicates abnormal processes in the hepatobiliary system associated with the development of cholestasis (impaired outflow of bile).
During the examination, the following can be diagnosed: the presence of stones in the gallbladder (cholecystolithiasis), stones in the bile ducts (choledocholithiasis). Also, the causes may be renal pathologies: damage to the glomeruli (glomeruli of the kidneys), otherwise glomerulonephritis, chronic renal failure (chronic renal failure), neoplasms in the kidneys.
Important! Only laboratory microscopy of urine provides accurate results. If the doctor has written out a referral for tests, you cannot ignore the examination.
What do we have to do?
Urobilinogen found in urine - what does this mean? What should be done in this case? The first piece of advice is don't panic. Nervous stress and negative emotions cause stagnation in the body. If urobilinogen levels are elevated, you should definitely consult a doctor to find out the true reasons, you need to undergo additional examination.
Often those people who work at night and do not sleep have their biological clock disrupted. In this case, the reaction to the presence of urobilin bodies can be positive. In such a situation, restoring the regime can bring the body back to normal.
An active lifestyle, physical activity, and water treatments help the body get rid of toxins in a timely manner. A dairy-vegetable diet is also useful in such cases, as it will improve intestinal function. In this case, medicinal bitter herbs will not interfere: wormwood, immortelle, elecampane, tansy, milk thistle. They will restore the body and help remove excess toxins from the intestines. The infusion is prepared as follows: pour one tablespoon into 0.5 liters of boiling water and leave for half an hour. Take ¼ glass before meals.
Diagnostic methods
If urobilin is discovered completely by accident, during a routine examination, in a patient who does not present any complaints, then this condition does not cause any particular concern. As a rule, it is caused by disturbances in diet and normal fluid intake. Urobilinuria often occurs in women who are on a strict diet.
In such cases, a repeat urine test and examination of biochemical blood parameters, in particular the level of total bilirubin and its fractions (direct and indirect), are required.
A special group is represented by pregnant women who experience episodes of urobilinuria. They are recommended to take a urine test at every visit to the doctor in order to monitor the dynamics of the condition and, if necessary, begin appropriate treatment.
To determine the concentration of urobilin in urine, special indicator strips are used that change color as a result of a chemical reaction.
When the level of urobilin in the urinary sediment and the concentration of bilirubin in the blood exceeds normal values many times over, a thorough instrumental examination begins.
First of all, an ultrasound of the liver tissue is performed, thanks to which its structure, the presence of pathological foci, as well as stones in the biliary tract are assessed. If there is a suspicion that the cause of urobilinuria is a liver disorder, a CT scan or MRI is performed.
Intestinal diseases are excluded or confirmed using endoscopic diagnostic methods (FGDS, colonoscopy and others).
Urobilin components in pregnant women
Impaired liver function is indicated by a high level of the urobilin component in pregnant women identified as a result of test samples. This may be influenced by a genetic predisposition or the presence of a disease (such as hepatitis disorders or cholestasis). Exceeding the norm of the urobilin component can cause a decrease in fluid during pregnancy, which leads to an increase in the concentration of urobilinogenic substances in urine.
An indicator of this problem is the dark color of urinary secretions. If there is no dehydration, problems with nutrition or taking medications, diagnostic measures are carried out necessary to exclude diseases.
During pregnancy, doctors urge regular tests to understand how a woman tolerates stress and changes and to rule out health problems.
What analysis shows urobilinoids in urine
The level of urobilinogen is determined during a general clinical analysis (CCA). But you can suspect an increase or decrease in their number by visually assessing the color of the biological fluid. With a high content of urobilinoids, the color of urine changes - it becomes dark; with a low concentration of bile breakdown products, it becomes almost colorless.
Both phenomena should be a reason to see a doctor and undergo an examination. First you will have to pass the OAM. The result form will indicate the amount of urobilinogen (UBG, URO). Based on this, the doctor will prescribe further diagnostics or allay concerns regarding the patient’s health condition.
How to prepare and how the analysis is carried out
The urobilinogen test does not require preliminary preparation. The only thing doctors ask is that on the eve of urine collection, avoid foods that can change its color. These are beets, carrots, pumpkin. You should also not use medications (unless absolutely necessary) that give urine an unnatural color - analgin, acetylsalicylic acid, otherwise the analysis for urobilinogen will be biased.
To collect urine, prepare a disposable container purchased at a pharmacy or a well-washed dry jar with a volume of up to 200 ml with a lid. In the morning after sleep, you need to rinse the area of the external genitalia and dry it with a clean towel. Fill the container with 80-100 ml of urine.
The material is delivered for analysis no later than 2 hours after collection.
What is urobilinogen?
When explaining to patients what urobilinogen is in a urine test, doctors say that it is a simple bile pigment. The substance is a product of bilirubin metabolism. Urobilinogen itself gives the urine a golden (straw) color. As a result of the breakdown of erythrocyte hemoglobin, bilirubin is released, which is toxic. In the liver, it binds to glucuronic acid and loses the ability to negatively affect the body.
In this combination, bilirubin enters the intestine, where it undergoes fermentation, oxidation and metabolization (decomposition). As a result of such complex reactions, urobilinogen is formed. This bile pigment is partially sent along with the blood to the kidneys and excreted in the urine. The rest of the urobilinogen, moving into the large intestine, is transformed into stercobilin and in this state leaves the body along with the feces, giving the stool an intense brown color.
How to reduce pigment content
If a high urobilinogen value is detected, the analysis must be repeated. If he confirms urobilinuria, then the therapist, gastroenterologist or hepatologist prescribes a diagnosis. She should identify the cause of high urobilin. Based on the examination, treatment is prescribed.
In therapy they use:
- hepatoprotectors – Esliver, Essentiale;
- antiviral for hepatitis - Arviron, Zepatir, Baraklyud, Leukinferon;
- choleretic agents – Odeston, Allohol, Flamin;
- vitamin and mineral complexes;
- immunomodulators.
Inflammatory processes affecting the intestines require antibiotic therapy. For dysbacteriosis, medications containing live lactobacilli are prescribed. To reduce the degree of poisoning, which resulted in an increase in the concentration of urobilinogen in the urine, sorbents (Sorbex, Enterosgel) are prescribed. They must be taken in parallel with increasing the volume of fluid you drink.
Absorption of urobilinogen occurs with the participation of bacteria inhabiting the intestines. Changing the ratio of flora to the benefit of pathogenic microorganisms during dysbacteriosis reduces the flow of pigment into the bloodstream.
To reduce the concentration of pigment, doctors recommend eating lean boiled meat, fresh fruits, vegetables, and cereals. Fermented milk products with a low fat content will help improve intestinal function.
General urine analysis
General urine analysis
is a laboratory study of the physical, chemical properties of urine and microscopy of sediment.
A general urine test includes:
- study of physical properties: determination of color, transparency, specific gravity of urine;
- determination of protein, glucose, hemoglobin, bilirubin, urobilinogen, ketone bodies and nitrites by a semi-quantitative method;
- assessment of the composition of urine sediment.
The results of a general urine test are of particular importance in determining a number of pathologies in the human body.
For patients suffering from kidney pathology and diseases of the urinary system, the study is prescribed repeatedly to assess the condition and monitor therapy over time. The analysis is performed during preventive examinations. Indications:
- diseases of the urinary system;
- screening examination during medical examinations;
- assessment of the course of the disease, monitoring the development of complications and the effectiveness of treatment;
- Persons who have had a streptococcal infection (tonsillitis, scarlet fever) are recommended to take a urine test 1–2 weeks after recovery.
Preparation
On the eve of the test, it is not recommended to eat vegetables and fruits that can change the color of urine (beets, carrots, cranberries, etc.), or take diuretics.
Collect a strictly morning portion of urine, excreted immediately after sleep. Before collecting urine, it is necessary to perform a thorough hygienic toilet of the external genitalia. When urinating for the first time in the morning, release a small amount of urine (the first 1-2 seconds) into the toilet, then collect the entire portion of urine in a clean container without interrupting urination. Pour approximately 50 ml of urine into a sterile plastic container with a screw cap. When collecting urine, it is advisable not to touch the container to your body. The container with urine must be delivered to the medical office within 2 hours from the moment the biomaterial is taken.
Women are not recommended to take a urine test during menstruation.
Interpretation of results
Indicators in a general urine test are:
- Urine color
- Transparency
- Relative density
- pH
- Protein in urine
- Glucose in urine
- Bilirubin in urine
- Urobilinogen in urine
- Ketone bodies in urine
- Nitrites in urine
- Hemoglobin in urine
- Sediment microscopy
Urine color
The color of urine in an adult is straw-yellow. The shade can range from light to almost amber. Normally, the urine pigment urochrome gives the urine a yellow color of various shades, depending on the degree of saturation of the urine with it. With polyuria, urine has a lighter color; with a decrease in diuresis, it acquires a rich yellow tint. A change in the color of urine may be the result of the release of coloring compounds formed during organic changes or under the influence of dietary components, medications taken, or contrast agents.
Pathologically changed color of urine occurs when:
- discharge of blood in the urine - “a type of meat slop”;
- presence of bilirubin in urine (beer color);
- the presence of a large number of leukocytes (milky white color);
- presence of hemoglobin or myoglobin (black).
Urine transparency
Reference values: complete.
Cloudiness of urine can be the result of the presence of red blood cells, leukocytes, epithelium, bacteria, fat droplets in the urine, precipitation of salts (urates, phosphates, oxalates) and depends on the concentration of salts, pH and storage temperature of urine (low temperature promotes precipitation of salts) .
If you stand for a long time, your urine may become cloudy due to bacterial growth. Normally, slight turbidity may be due to epithelium and mucus.
Relative density
The relative density (specific gravity) of urine depends on the amount of excreted organic compounds (urea, uric acid, salts) and electrolytes - Cl, Na and K, as well as on the amount of water excreted. The higher the diuresis, the lower the relative density of urine. The presence of protein and especially glucose causes an increase in the specific gravity of urine.
A decrease in the concentration function of the kidneys in renal failure leads to a decrease in specific gravity. Complete loss of concentration function leads to equalization of the osmotic pressure of plasma and urine, this condition is called isosthenuria.
Reference values: 1003–1035 g/l.
Increased relative density (hypersthenuria):
- glucose in the urine in uncontrolled diabetes mellitus;
- protein in the urine (proteinuria) with glomerulonephritis, nephrotic syndrome;
- drugs and (or) their metabolites in the urine;
- intravenous infusion of mannitol, dextran or radiocontrast agents;
- low fluid intake;
- large fluid losses (vomiting, diarrhea);
- toxicosis of pregnant women;
- oliguria.
Decreased relative density (hyposthenuria):
- diabetes insipidus (nephrogenic, central or idiopathic);
- chronic renal failure;
- acute damage to the renal tubules;
- polyuria (as a result of taking diuretics, drinking too much).
Urine pH
Fresh urine from healthy people can have a different pH reaction from 4.5 to 8. Usually the urine reaction is slightly acidic, pH = 5–6. Fluctuations in the pH of urine are caused by the composition of the diet: a meat diet causes an acidic reaction in the urine; the predominance of plant and dairy foods leads to alkalization of the urine.
Changes in urine pH correspond to blood pH; with acidosis, the urine is acidic, and with alkalosis, it is alkaline. Sometimes there is a discrepancy between these indicators. In case of chronic damage to the kidney tubules (tubulopathies), hyperchloric acidosis is observed in the blood, and the urine reaction is alkaline, which is associated with a violation of the synthesis of acid and ammonia due to damage to the tubules. Bacterial decomposition of urea in the ureters or storage of urine at room temperature leads to alkalinization of urine.
The reaction of urine affects the nature of salt formation in urolithiasis: at a pH below 5.5, uric acid stones are more often formed, at a pH from 5.5 to 6.0 - oxalate stones, at a pH above 7.0 - phosphate stones.
Reference values:
- 0–1 month — 5.0–7.0;
- 1 month–120 years – 4.5–8.0.
Increase in urine pH:
- metabolic and respiratory alkalosis;
- chronic renal failure;
- renal tubular acidosis (types I and II);
- hyperkalemia;
- primary and secondary hyperfunction of the parathyroid gland;
- carbon anhydrase inhibitors;
- a diet high in fruits and vegetables; prolonged vomiting;
- urinary tract infections caused by microorganisms that break down urea;
- administration of certain medications (adrenaline, nicotinamide, bicarbonates);
- neoplasms of the genitourinary system.
Decrease in urine pH:
- metabolic and respiratory acidosis;
- hypokalemia;
- dehydration;
- starvation;
- diabetes;
- tuberculosis;
- fever;
- severe diarrhea;
- taking medications: ascorbic acid, corticotropin, methionine;
- diet high in meat protein and cranberries.
Protein in the urine ( proteinuria)
Protein in the urine is one of the most diagnostically important laboratory signs of kidney pathology. A small amount of protein in the urine may be present in healthy people, but the excretion of protein in the urine does not normally exceed 0.080 g/day at rest and 0.250 g/day during intense physical activity, after a long walk (marching proteinuria). Protein in the urine can also be detected in healthy people during strong emotional experiences or hypothermia.
Orthostatic proteinuria (in an upright body position) occurs in adolescents. Normally, most proteins do not pass through the membrane of the renal glomeruli, which is explained by the large size of protein molecules, as well as their charge and structure.
With minimal damage in the glomeruli of the kidneys, there is primarily a loss of low molecular weight proteins (mainly albumin), therefore, with a large loss of protein, hypoalbuminemia often develops. With more pronounced pathological changes, larger protein molecules also enter the urine. The renal tubular epithelium physiologically secretes a certain amount of protein (Tamm-Horsfall protein). Some of the urine proteins can come from the genitourinary tract (ureter, bladder, urethra) - the content of these proteins in the urine increases sharply with infections, inflammation or tumors of the genitourinary tract.
Proteinuria (the appearance of increased amounts of protein in the urine) can be:
- prerenal (associated with increased tissue breakdown or the appearance of pathological proteins in the plasma);
- renal (caused by kidney pathology);
- postrenal (associated with urinary tract pathology).
The appearance of protein in the urine is a common nonspecific symptom of kidney pathology.
With renal proteinuria, protein is found in both daytime and nighttime urine. According to the mechanisms of occurrence of renal proteinuria, glomerular and tubular proteinuria are distinguished:
- glomerular proteinuria is associated with a pathological change in the barrier function of the glomerular membranes. Massive urinary protein loss (> 3 g/L) is always associated with glomerular proteinuria;
- tubular proteinuria is caused by impaired protein reabsorption due to pathology of the proximal tubules.
Reference values: <0.140 g/l.
Presence of protein in urine (proteinuria):
- nephrotic syndrome; diabetic nephropathy; glomerulonephritis; nephrosclerosis;
- impaired absorption in the renal tubules (Fanconi syndrome, heavy metal poisoning, sarcoidosis, sickle cell disease);
- multiple myeloma (Bence Jones protein in urine) and other paraproteinemias;
- impaired renal hemodynamics with: heart failure, fever;
- malignant tumors of the urinary tract;
- cystitis, urethritis and other urinary tract infections.
Glucose in urine
Glucose in urine is normally absent or found in minimal quantities, up to 0.8 mmol/l, because in healthy people, all blood glucose, after filtering through the membrane of the renal glomeruli, is completely absorbed back into the tubules.
When the concentration of glucose in the blood is more than 10 mmol/l - the renal threshold is exceeded (the maximum ability of the kidneys to reabsorb glucose) or when the renal threshold is reduced (renal tubular damage), glucose appears in the urine - glucosuria is observed.
Detection of glucose in urine is important for the diagnosis of diabetes mellitus, as well as monitoring (and self-control) of antidiabetic therapy.
Method for examining general urine analysis using Bayer Multistix diagnostic strips (+ sediment microscopy)
The result is read automatically using a Clinitek 500 analyzer from Bayer (visual determination errors are excluded). The principle of the glucose determination method is glucose oxidase. The test strip step for a urine glucose test is as follows: first there is a “negative” result, the next step is “5.5” (traces). If the true glucose value is between these values, then due to this step of the test strip, the device displays it as a minimum positive value - 5.5. Since questions from doctors and patients about this threshold value of glucose concentration have recently become more frequent, the laboratory decided, when receiving such a result, to give out not a number, but to write “traces”. With such a response to glucose in the urine, we recommend additional studies, in particular, a determination of fasting blood glucose, a study of daily urine excretion (hexokinase method), or, if prescribed by a doctor, a glucose tolerance test.
Reference values:
- 0–1.6. "See comment":
- < 1.7 - negative;
- 1.7–2.8 — traces;
- > 2.8 - a significant increase in the concentration of glucose in the urine.
Increased levels (glucosuria):
- diabetes;
- acute pancreatitis;
- hyperthyroidism;
- renal diabetes;
- steroid diabetes (taking anabolic steroids for diabetics);
- poisoning with morphine, strychnine, phosphorus;
- dumping syndrome;
- Cushing's syndrome;
- myocardial infarction;
- pheochromocytoma;
- major trauma, burns;
- tubulointerstitial kidney damage;
- pregnancy;
- taking large amounts of carbohydrates.
Bilirubin in urine
Bilirubin is the main final metabolite of porphyrins excreted from the body. In the blood, free (unconjugated) bilirubin in plasma is transported by albumin; in this form, it is not filtered in the glomeruli. In the liver, bilirubin combines with glucuronic acid (a conjugated, water-soluble form of bilirubin is formed) and in this form it is released into the bile into the gastrointestinal tract. When the concentration of conjugated bilirubin in the blood increases, it begins to be excreted by the kidneys and found in the urine. The urine of healthy people contains minimal, undetectable amounts of bilirubin. Bilirubinuria is observed mainly with damage to the liver parenchyma or mechanical obstruction of the outflow of bile. With hemolytic jaundice, the urine reaction to bilirubin is negative.
Reference values: negative.
Detection of bilirubin in urine:
- obstructive jaundice, viral hepatitis, liver cirrhosis;
- metastases of neoplasms to the liver.
Urobilinogen in urine
Urobilinogen and stercobilinogen are formed in the intestine from bilirubin released in bile. Urobilinogen is reabsorbed in the colon and again enters the liver through the portal vein system, and then again excreted along with bile. A small part of this fraction enters the peripheral bloodstream and is excreted in the urine. Normally, in the urine of a healthy person, urobilinogen is determined in trace quantities - its excretion in urine per day does not exceed 10 µmol (6 mg). When urine stands, urobilinogen turns into urobilin. Reference values: 0–17.
Increased excretion of urobilinogen in urine:
- increased hemoglobin catabolism: hemolytic anemia, intravascular hemolysis (transfusion of incompatible blood, infections, sepsis), pernicious anemia, polycythemia, resorption of massive hematomas.
- increased formation of urobilinogen in the gastrointestinal tract: enterocolitis, ileitis, intestinal obstruction;
- increased formation and reabsorption of urobilinogen during infection of the biliary system (cholangitis);
- increased urobilinogen in liver dysfunction: viral hepatitis (excluding severe forms), chronic hepatitis and cirrhosis of the liver;
- toxic damage: alcohol, organic compounds, toxins during infections, sepsis;
- secondary liver failure:
- myocardial infarction, cardiac and circulatory failure;
- liver tumors;
- increased urobilinogen during liver bypass surgery: liver cirrhosis with portal hypertension, thrombosis, renal vein obstruction.
Ketone bodies in urine (ketonuria)
Ketone bodies (acetone, acetoacetic and beta-hydroxybutyric acids) are formed as a result of increased catabolism of fatty acids. Determination of ketone bodies is important in recognizing metabolic decompensation in diabetes mellitus. Insulin-dependent juvenile diabetes is often first diagnosed by the appearance of ketone bodies in the urine. With inadequate insulin therapy, ketoacidosis progresses. The resulting hyperglycemia and hyperosmolarity lead to dehydration, electrolyte imbalance, and ketoacidosis. These changes cause dysfunction of the central nervous system and lead to hyperglycemic coma.
Reference values:
- 0–0.4 — “See. comm.";
- <0.5 - negative;
- 0.5–0.9 — traces;
- > 0.9 - positive.
Detection of ketone bodies in urine (ketonuria):
- diabetes mellitus (decompensated - diabetic ketoacidosis);
- precomatose state; cerebral (hyperglycemic) coma;
- long-term fasting (complete refusal of food or diet aimed at reducing body weight);
- severe fever;
- alcohol intoxication;
- hyperinsulinism;
- hypercatecholaminemia;
- isopropranolol poisoning;
- eclampsia;
- glycogenosis types I, II, IV;
- lack of carbohydrates in the diet.
Nitrites in urine
Nitrites are absent in normal urine. In urine, they are formed from nitrates of food origin under the influence of bacteria, if the urine was in the bladder for at least 4 hours. Detection of nitrites in the urine (positive test result) indicates infection of the urinary tract. However, a negative result does not always exclude bacteriuria. Urinary tract infection varies among different populations and is dependent on age and gender.
Other things being equal, the following are more susceptible to an increased risk of asymptomatic urinary tract infections and chronic pyelonephritis:
- girls and women;
- elderly people (over 70 years old);
- men with prostate adenoma;
- diabetic patients;
- patients with gout;
- patients after urological operations or instrumental procedures on the urinary tract.
Reference values: negative.
Hemoglobin in urine
There is no hemoglobin in normal urine. A positive test result reflects the presence of free hemoglobin or myoglobin in the urine. This is the result of intravascular, intrarenal, urinary hemolysis of red blood cells with the release of hemoglobin, or muscle damage and necrosis, accompanied by an increase in plasma myoglobin levels. It is quite difficult to distinguish hemoglobinuria from myoglobinuria; sometimes myoglobinuria is mistaken for hemoglobinuria.
Reference values: negative.
Presence of hemoglobin in urine:
- severe hemolytic anemia;
- severe poisoning, for example: sulfonamides, phenol, aniline. poisonous mushrooms;
- sepsis;
- burns.
Presence of myoglobin in urine:
- muscle damage;
- heavy physical activity, including sports training;
- myocardial infarction;
- progressive myopathies;
- Rhabdomyolysis
Microscopy of urine sediment
Microscopy of urine components is carried out in the sediment formed after centrifugation of 10 ml of urine. Sediment consists of solid particles suspended in urine: cells, protein-formed casts (with or without inclusions), crystals, or amorphous deposits of chemicals.
Red blood cells in urine
Red blood cells (blood cells) enter the urine from the blood. Physiological erythrocyturia is up to 2 red blood cells/μl of urine. It does not affect the color of urine.
Hematuria is the appearance of red blood cells, formed elements, as well as hemoglobin and other blood components in the urine. The condition can be caused by bleeding anywhere in the urinary system. The main reason for the increase in the content of red blood cells in the urine is renal or urological diseases and hemorrhagic diathesis.
Reference values: <2 per field of view.
Red blood cells in urine – exceeding reference values:
- urinary tract stones;
- tumors of the genitourinary system;
- glomerulonephritis;
- pyelonephritis;
- hemorrhagic diathesis (with intolerance to anticoagulant therapy, hemophilia, coagulation disorders, thrombocytopenia, thrombocytopathies);
- urinary tract infections (cystitis, urogenital tuberculosis);
- kidney injury;
- arterial hypertension with involvement of the renal vessels;
- systemic lupus erythematosus (lupus nephritis);
- poisoning with benzene derivatives, aniline, snake venom, poisonous mushrooms;
- inadequate anticoagulant therapy.
Leukocytes in the urine
Leukocyturia is an increased number of leukocytes in the urine. Its presence is a symptom of inflammation of the kidneys and/or lower urinary tract. In chronic inflammation, leukocyturia is a more reliable test than bacteriuria, which is often not detected. With a very large number of leukocytes, pus in the urine is determined macroscopically - this is the so-called pyuria. The presence of leukocytes in the urine may be due to the presence of secretions from the external genitalia in the urine due to vulvovaginitis, or insufficiently thorough toileting of the external genitalia when collecting urine for analysis.
Reference values:
- men: <3 in visual field;
- women, children < 14 years: < 5 per field of view.
An increase in leukocytes in the urine is observed in almost all diseases of the kidneys and genitourinary system:
- acute and chronic pyelonephritis, glomerulonephritis;
- cystitis, urethritis, prostatitis;
- stones in the ureter;
- tubulointerstitial nephritis;
- lupus nephritis;
- kidney transplant rejection.
Epithelial cells in urine
Epithelial cells are almost always present in urine sediment. Epithelial cells originating from different parts of the genitourinary system vary (usually squamous, transitional and renal epithelium are distinguished). Squamous epithelial cells, characteristic of the lower parts of the genitourinary system, are found in the urine of healthy people and their presence usually has little diagnostic value. The amount of squamous epithelium in the urine increases with urinary tract infection. An increased number of transitional epithelial cells can be observed in cystitis, pyelonephritis, and kidney stones. The presence of renal epithelium in the urine indicates damage to the kidney parenchyma (observed in glomerulonephritis, pyelonephritis, some infectious diseases, intoxication, circulatory disorders). The presence of more than 15 renal epithelial cells in the field of view 3 days after transplantation is an early sign of the threat of allograft rejection.
Reference values:
- squamous epithelial cells: women - <5 per field of view; men - <3 in the field of view;
- transitional epithelial cells - < 1;
- renal epithelial cells are absent.
Detection of renal epithelial cells:
- pyelonephritis;
- intoxication (taking salicylates, cortisone, phenacetin, bismuth preparations, poisoning with heavy metal salts, ethylene glycol);
- tubular necrosis;
- kidney transplant rejection;
- nephrosclerosis.
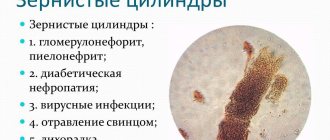
Cylinders in urine
Cylinders are elements of cylindrical sediment (a kind of cast of renal tubules), consisting of protein or cells, and may also contain various inclusions (hemoglobin, bilirubin, pigments, sulfonamides). Based on their composition and appearance, there are several types of cylinders (hyaline, granular, erythrocyte, waxy, etc.). Normally, renal epithelial cells secrete the so-called Tamm-Horsfall protein (absent in blood plasma), which is the basis of hyaline casts. Sometimes hyaline casts can be found in healthy people.
Granular casts are formed as a result of the destruction of tubular epithelial cells. Their detection in a patient at rest and without fever indicates renal pathology. Waxy casts are formed from compacted hyaline and granular casts. Erythrocyte casts are formed when red blood cells are layered on hyaline casts, and leukocyte casts are formed by leukocytes. Epithelial casts (rarely) are derived from renal tubular cells. Their presence in a urine test a few days after surgery is a sign of rejection of the transplanted kidney. Pigment cylinders are formed when pigments are included in the composition of the cylinder and are observed with myoglobinuria and hemoglobinuria.
Reference values: none.
Hyaline casts in urine:
- renal pathology (acute and chronic glomerulonephritis, pyelonephritis, kidney stones, renal tuberculosis, tumors);
- congestive heart failure;
- hyperthermic conditions;
- heavy physical activity;
- high blood pressure;
- taking diuretics.
Granular casts (nonspecific pathological symptom):
- glomerulonephoritis, pyelonephritis;
- diabetic nephropathy;
- viral infections;
- lead poisoning;
- fever.
Waxy cylinders:
- chronic renal failure;
- kidney amyloidosis;
- nephrotic syndrome.
Red blood cell casts (hematuria of renal origin):
- acute glomerulonephritis;
- kidney infarction;
- renal vein thrombosis;
- malignant hypertension.
Leukocyte casts (leukocyturia of renal origin):
- pyelonephritis;
- Lupus nephritis in systemic lupus erythematosus.
Epithelial casts (most rare):
- acute tubular necrosis;
- viral infection (for example, cytomegalovirus);
- poisoning with salts of heavy metals, ethylene glycol;
- overdose of salicylates;
- amyloidosis;
- kidney transplant rejection reaction.
Bacteria in urine
Isolation of bacteria in urine has significant diagnostic value. Bacteria remain in the urine for no more than 1–2 days after the start of antibiotic therapy. The first morning urine sample is preferable for testing. The type of bacteria can be determined and the level of bacteriuria can be assessed, as well as the sensitivity of microorganisms to antibiotics can be determined using bacteriological urine culture.
Reference values: negative.
Bacteria in urine:
- infections of the urinary system (pyelonephritis, urethritis, cystitis).
Yeast
The detection of yeast of the genus Candida indicates candidiasis, which most often occurs as a result of irrational antibiotic therapy.
Inorganic urine sediment (crystals), salts in urine
. Urine is a solution of various salts, which can precipitate (form crystals) when the urine stands. Low temperature promotes the formation of crystals. The presence of certain salt crystals in the urinary sediment indicates a change in the reaction towards the acidic or alkaline side. Excessive salt content in urine contributes to the formation of stones and the development of urolithiasis. At the same time, the diagnostic value of the presence of salt crystals in urine is usually small. Increased doses of ampicillin and sulfonamides lead to the formation of crystals.
Reference values: none.
Uric acid and its salts (urates):
- highly concentrated urine;
- acidic reaction of urine (during physical activity, meat diet, fever, leukemia);
- uric acid diathesis, gout;
- chronic renal failure;
- acute and chronic nephritis;
- dehydration (vomiting, diarrhea);
- in newborns.
Tripelphosphates, amorphous phosphates:
- alkaline urine reaction in healthy people;
- vomiting, gastric lavage;
- cystitis;
- Fanconi syndrome, hyperparathyroidism.
Calcium oxalate (oxaluria occurs with any urine reaction):
- eating foods rich in oxalic acid (spinach, sorrel, tomatoes, asparagus, rhubarb);
- pyelonephritis;
- diabetes;
- ethylene glycol poisoning.
Mucus in urine
Mucus is secreted by the epithelium of the mucous membranes. Normally present in urine in small quantities. During inflammatory processes, the mucus content in the urine increases. An increased amount of mucus in the urine may indicate a violation of the rules of proper preparation for taking a urine sample.
Reference values: insignificant quantity.
Additional tests required
Finding out the reasons for the increase in urobilinoids in the urine requires additional diagnostics, because a general urine test provides only indicative data and does not allow making a diagnosis, much less prescribing treatment.
If there is a pathological change in the level of urobilinogen, the patient will have to undergo:
- general blood analysis;
- biochemical blood test (content of bilirubin and other liver enzymes, creatinine, urea);
- general stool analysis (amount of stercobilin);
- Ultrasound of the liver, kidneys.