Home » Methods » Study of external respiration functions: indications and methods
March 18, 2020 Methods
Patients with diseases of the respiratory system are often prescribed a pulmonary function test (RPF). Despite the fact that this type of diagnosis is quite simple, accessible, and therefore widespread, few people know what it is and for what purpose it is carried out.
What is FVD and why measure it?
Breathing is a vital process for a person of any age. During the respiratory process, the body is saturated with oxygen and releases carbon dioxide formed during metabolism. Therefore, impaired breathing function can lead to a number of health problems.
External respiration is a medical term that includes a description of the processes of air circulation through the respiratory system, its distribution, and the transfer of gases from inhaled air to the blood and back.
The study of respiratory function, in turn, allows you to calculate the volume of the lungs, assess the speed of their work, identify dysfunctions, diagnose diseases of the respiratory system and determine effective treatment methods. Therefore, doctors use FVD for various purposes:
- For diagnostic purposes. In this case, the state of health, the effect of the disease on the functionality of the lungs and its prognosis are assessed. Also, the risk of developing pathology is determined (in smokers, people working in hazardous conditions, etc.).
- For dynamic monitoring of the development of the disease and assessment of the effectiveness of therapy.
- To issue an expert opinion, which is required when assessing suitability for work in special conditions and determining temporary disability.
Also, diagnostics of external respiration function is carried out within the framework of epidemiological studies and for the purpose of carrying out a comparative analysis of people’s health in different living conditions.
FVD and spirometry: what is the difference?
During spirometry, the patient will sit with a mouthpiece in front of the equipment. It is important that the mouthpiece fits tightly and that all consumed air enters the device.
Spirometry measures the amount of air inhaled: it measures only the speed of air flow and estimates the size of the lungs.
Also, the procedure involves using a nose clip so as not to inhale air through it. The doctor will ask you to inhale and exhale as deeply as possible, or to breathe faster for a few seconds. The doctor may also ask you to inhale a medicine that opens the airways. You will then need to breathe into the breathing machine again to see if the medicine affects your lung function.
In medicine, pulmonary function tests determine a general and detailed analysis of the quality of lung function.
For example, lung capacity tests are the most accurate way to measure how much air your lungs can hold. This test determines the amount of gas in the lungs, known as lung capacity.
The diffusion capacity of the lungs determines how well oxygen gets into the blood of inhaled air. Pulse oximetry assesses the level of oxygen in the blood. Fractional exhaled nitric oxide tests measure the amount of nitric oxide in the air you exhale. Other tests may be needed to evaluate lung function in infants, children, or patients who are unable to perform spirometry and lung volume tests.
https://youtu.be/uXBGEulzSK4
Indications and limitations for diagnosis
The reason for studying pulmonary function and assessing respiratory function are many diseases of the respiratory system. Such diagnostics are prescribed for:
- chronic bronchitis;
- asthma;
- infectious inflammatory process in the lungs;
- chronic obstructive pulmonary disease;
- silicosis (an occupational disease resulting from regular inhalation of dust with a high content of silicon dioxide);
- idiopathic fibrosing alveolitis and other pathologies.
Contraindications to FVD include:
- age less than 4 years – if the child is not able to correctly understand and follow the instructions of a health worker;
- development of acute infections and feverish conditions in the body;
- severe angina and myocardial infarction;
- stable increase in blood pressure;
- a stroke suffered shortly before the proposed study;
- congestive heart failure, which is accompanied by breathing problems even with low exertion and at rest.
Important. Also, this type of diagnosis is not carried out in patients suffering from abnormalities in mental or mental activity that do not allow them to adequately respond to requests from medical staff.
Positive Ventolin test: what does it mean?
The Ventolin test is a quick, simple and painless method for assessing respiratory function. It takes about 60 minutes and is done for:
- detecting and confirming asthma, and monitoring the course of the disease.
- to distinguish asthma from COPD.
Ventolin is a medicine that is distributed in the respiratory system.
As a result of this test, an improvement is considered normal if the FEV1 value has increased by ≥200 ml and by ≥12% of normal (or the original value). In current protocols for the treatment of asthma and COPD, the result of Ventolin tests has no prognostic value, either with a long-term response to anti-inflammatory treatment or due to the progression of these diseases.
As a matter of practicality, the cardinal test result is a normal post-drug FEV1/FVC, excluding a diagnosis of COPD. Obstruction after the drug can occur in both COPD and asthma. In patients, the value of the Ventolin test may change over time. Having received the sample result, you need to analyze the data, drawing a conclusion about a possible pathology.
A healthy patient should have good basic indicators of the spirogram: forced vital capacity, air force and ventilation of the lungs at least 80% of the average values. If the indicators have decreased to 70%, then this is accepted as a pathology.
Pulmonary function testing is sometimes necessary after inhalation of drugs that are distributed in the respiratory system, for example, FVD with Methacholine. It can also be a spirometric study using medications, such as a bronchodilator test, for example, FVD with Salbutamol. If a test with Salbutomol has a questionable result, use a bronchodilator test with the drug Formoterol.
Spirometry
Currently, there are various methods for studying the function of external respiration. One of the most common is spirometry.
For studies of this kind, a dry or water spirometer is used - a device consisting of two components. The spirometer sensor records the volume of air inhaled and the speed at which the person inhales and exhales it. And the microprocessor processes information.
Spirometry allows you to assess:
- the functionality of the organs involved in breathing (including the vital capacity of the lungs);
- airway patency;
- complexity of changes in the respiratory system, their type.
In addition, it can be used to detect bronchospasms and determine whether changes in the respiratory system are reversible.
Other methods of studying FVD
Other methods included in the complex are performed less frequently and are prescribed in cases where spirometry cannot obtain a complete picture of the disease.
Pneumotachometry
This study allows you to find the speed of air flow through various parts of the respiratory system.
It is carried out while inhaling and exhaling. The patient is required to take a deep breath or exhale into the device. Modern spirographs immediately create a recording of spirometry and pneumotachometry readings. It allows you to identify diseases accompanied by a deterioration in the passage of air through the respiratory system.
Spirometry cannot detect hidden respiratory deficiency. Therefore, in the case of an incomplete picture of the disease, FVD with a test is prescribed.
It involves the use of bronchodilators after measurements are taken without the product.
The interval between measurements depends on which medicinal substance is used. If it is salbutamol, then after 15 minutes, ipratropium - Thanks to testing with bronchodilators, it is possible to find pathology at the earliest stage.
This option for checking the respiratory system is carried out if there are signs of asthma, but the bronchodilator test is negative. The provocation consists of administering methacholine to the patient by inhalation.
The concentration of the product is constantly increasing, which causes difficulty in the conduction of the respiratory tract. Symptoms of bronchial asthma occur.
Bodyplethysmography
Body plethysmography is similar to previous methods, but it most closely reflects the picture of the actions occurring in the respiratory system. The essence of the study is that a person is placed in a sealed chamber. The actions that the patient must perform are the same, but in addition to the size, the pressure in the chamber is regulated.
Ventolin test
This product belongs to the selective β2-adrenergic receptor agonists, the active substance is salbutamol.
When introduced after 15 minutes, it provokes dilation of the bronchi. In the diagnosis of asthma, it is essential: the patient is subjected to spirometry, measuring air circulation characteristics before and after the product. If the 2nd test indicates an improvement in ventilation by 15%, the test is considered positive, from 10% - doubtful, below - negative.
Stress tests
They consist of measuring the characteristics of the respiratory system at rest and after physical overload. This test allows you to detect stress disease, in which coughing begins after exercise. This is often observed in athletes.
Diffusion test
The main function of breathing is gas exchange; a person inhales oxygen needed by cells and tissues and removes carbon dioxide.
In some cases, the bronchi and lungs are healthy, but gas exchange, that is, the process of exchanging gases, is disrupted. The test indicates this: the patient closes his nose with a clip, inhales the consistency of gases through the mask for 3 s, exhales for 4 s. The equipment immediately measures the composition of exhaled air and interprets the acquired data.
Survey process
During the diagnostic study, the patient is asked to inhale as deeply as possible and then exhale into the spirometer. Initially, measurements are taken in a calm state, and then during forced breathing. The process is repeated several times with short breaks. When assessing the result, the highest indicator is taken into account.
To determine the reversibility of the process of narrowing of the bronchi, spirometry is performed with a bronchodilator - a drug that dilates this respiratory organ.
Features of the FVD method in a child
To test the functioning of the respiratory system, the respiratory function test system includes several types of samples. During the study, the patient must perform several actions. A child under 4-5 years old cannot fully fulfill all the requirements, so FVD is prescribed after this age. The child is explained what he must do, using a playful form of work. When deciphering the results, you may encounter unreliable data. This will falsely declare pulmonary or upper system dysfunction.
Conducting research in children differs from adults, since the anatomical structure of the respiratory system in the pediatric population has its own characteristics.
The initial establishment of contact with the child comes to the fore. Among the methods, you should choose options that are closest to physiological breathing and do not require significant effort from the child.
FVD (spirometry) indicators in normal and pathological conditions - meduniver.com
Preparing for the study
All studies are usually carried out in the morning on an empty stomach, or two hours after a small breakfast.
In order for spirometry readings to be most accurate, the patient must prepare for it in advance. As part of the preparation, doctors recommend:
- quit smoking one day before;
- do not drink strong tea, coffee and alcoholic drinks;
- half an hour before the examination, exclude vigorous physical activity.
In some cases, medications that affect the functioning of the respiratory system are also stopped.
During diagnosis, the patient should wear loose clothing that does not interfere with breathing deeply.
Research during pregnancy and breastfeeding
When diagnosing diseases, the question always arises whether pregnant and lactating women can be examined. Disturbances in the functioning of external respiration and the system as a whole can be detected during gestation for the first time. Deterioration of the conductivity of the pathways leads to the fact that the fetus does not receive the required amount of oxygen.
The norms prescribed in the tables do not apply to pregnant women. This is due to the fact that to provide the required volume of air to the fetus, the rate of minute ventilation gradually increases, by 70% by the end of the gestational period. Lung volume and expiratory speed are reduced due to compression of the diaphragm by the fetus.
When examining the function of external respiration, it is important to improve the patient’s condition, so if a bronchodilator is required, it is carried out. Tests make it possible to establish the effectiveness of therapy, prevent the development of complications, and begin timely treatment. The method is performed in the same way as in non-pregnant patients.
If the patient has not previously taken medications for the treatment of asthma, then during lactation it is not advisable to use a test with a bronchodilator. If this is necessary, the child is transferred to artificial nutrition for the period of drug removal.
Decoding the results
The average rate of breathing for a healthy person is:
- volume (DO) – from 0.5 to 0.8 liters;
- frequency (FR) – 10-20 times/min;
- minute volume (MOV) – 6-8 liters;
- expiratory reserve volume (ERV) – 1-1.5 l;
- vital capacity of the lungs (VC) – from 3 to 5 l;
- forced vital capacity (FVC) – 79-80%;
- volume of forced output for 1 second. (FEV1) – from 70% FVC.
In addition to these indicators, the instantaneous expiratory volumetric flow rate (IEF) is also determined. It is traced at different % filling of the lungs.
Important! Indicators of breathing volume and speed depend on the patient’s gender, age, weight and physical condition (training). Slight variability is allowed in each individual category of subjects (no more than 15% of the norm).
Significant deviations from normal readings allow the doctor to determine which pathologies are occurring in the patient’s respiratory system. So, if the vital capacity indicator is 55% of the norm, and FEV1 is equal to 90%, then this indicates the development of restrictive disorders characteristic of pneumonia, alveolitis.
Evidence of chronic obstructive pulmonary disease, in turn, is considered to be a slight decrease in vital capacity (up to 70%) against the background of a sharp decrease in CVF1 (up to 47%). Other respiratory dysfunctions also have characteristic indicators.
A little about our breathing
Respiration is a vital process as a result of which the body receives oxygen from the air, necessary for life, and releases carbon dioxide, which is formed during metabolism. Breathing has the following stages: external (with the participation of the lungs), the transfer of gases by red blood cells and tissue, that is, the exchange of gases between red blood cells and tissues.
Gas transfer is studied using pulse oximetry and blood gas analysis. We will also talk a little about these methods in our topic.
The study of the ventilation function of the lungs is available and is carried out almost everywhere for diseases of the respiratory system. It is based on measuring lung volumes and air flow rates during breathing.
Tidal volumes and capacities
Vital capacity (VC) is the largest volume of air exhaled after the deepest inhalation. In practice, this volume shows how much air can “fit” into the lungs during deep breathing and participate in gas exchange. When this indicator decreases, they speak of restrictive disorders, that is, a decrease in the respiratory surface of the alveoli.
Functional vital capacity (FVC) is measured like vital capacity, but only during rapid exhalation. Its value is less than vital capacity due to the collapse of part of the airways at the end of a rapid exhalation, as a result of which a certain volume of air remains “unexhaled” in the alveoli. If FVC is greater than or equal to VC, the test is considered as incorrectly performed. If FVC is less than VC by 1 liter or more, this indicates a pathology of small bronchi that collapse too early, preventing air from leaving the lungs.
While performing the rapid exhalation maneuver, another very important parameter is determined - forced expiratory volume in 1 second (FEV1). It decreases with obstructive disorders, that is, with obstructions to the exit of air in the bronchial tree, in particular with chronic bronchitis and severe bronchial asthma. FEV1 is compared with the proper value or its ratio to vital capacity (Tiffenau index) is used.
A decrease in the Tiffno index of less than 70% indicates severe bronchial obstruction.
The indicator of minute ventilation of the lungs (MVL) is determined - the amount of air passed through the lungs during the fastest and deepest breathing per minute. Normally it is 150 liters or more.
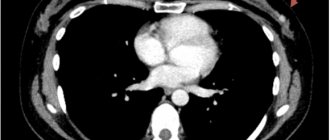
Bodyplethysmography
This test is similar in functionality to spirometry, but provides detailed and complete information about the state of the human respiratory system.
Body plethysmography helps to assess not only the patency of the bronchi, but also the volume of the lungs, as well as to recognize air traps that indicate pulmonary emphysema.
Such diagnostics are carried out using a body plethysmograph - a device consisting of a body camera (in which the subject is placed) with a pneumotapograph and a computer. The latter's monitor displays the study data.
Who is necessary and who is prohibited
The procedure is not only recommended, but also necessary in the following cases:
- diagnosing pathologies of the respiratory system, accompanied by prolonged cough, shortness of breath, sputum production and pain in the chest area;
- examinations of people from high-risk groups: smokers, people working in hazardous enterprises;
- preparing a person for operations on the lungs or bronchi;
- control of the body's response to physical activity (for athletes).
It is prohibited for people to carry out FVD analysis:
- with complex airway obstruction;
- myocardial infarction (its acute form or within 3 months after the illness);
- pregnant women;
- epilepsy;
- acute failure of cerebral blood circulation;
- aortic aneurysm;
- acute respiratory infections.
Peak flowmetry
A diagnostic method that allows you to determine the rate of inhalation/exhalation, and thereby assess the degree of narrowing of the airways.
The study is of particular importance for those who suffer from bronchial asthma, as well as patients with obstructive pulmonary disease in the chronic stage - it makes it possible to analyze the effectiveness of the chosen therapy.
Diagnostics is carried out using a special device - a peak flow meter. The first such apparatus in history was quite large and heavy, which significantly complicated research. Modern peak flow meters are mechanical (in the form of a tube, on which divisions with colored markers are applied) and electronic (computer), which are easy to use and compact. Moreover, the methodology itself for conducting and evaluating the results is so simple that it can be carried out at home.
But, despite this, the device should be used only on the recommendation of the treating doctor, and even better under his supervision (you can set up the peak flow meter together with the doctor, and then use it yourself, recording the readings). This approach will allow you to correctly take measurements and interpret the indicators.
Using a peak flow meter:
- changes in bronchial patency at different times of the day are determined;
- the necessary treatment is planned, the correctness and effectiveness of previous prescriptions is assessed;
- periods of exacerbation of asthmatic disease are predicted.
In addition, factors are identified that increase the risk of exacerbation (in cases where attacks occur frequently in some places and do not occur at all in others).
What is spirography and how is it performed?
This assessment method involves determining the volume of air that is inhaled and exhaled, as well as the speed of movement of air masses during breathing. When describing spirography - what kind of procedure it is, it is worth pointing out that it is very informative. To carry it out, you need specialized devices - spirographs. They can be with closed or open circuit. The technical operation of the device is based on recording changes in the filling of a certain container after the patient exhales. The device has sensors that monitor the amplitude of vibrations of the bellows.
What does spirography show?
During the study, the device records changes in the volume of air and the speed of flows that pass through it. Interpretation of spirometry begins with a visual assessment of the shape of the resulting curves. After this, the specialist conducts a quantitative analysis of the result, for which the obtained numerical indicators are compared with existing standards. As a result, a spirometric conclusion is drawn up. Spirometry with Salbutamol deserves attention - it is a bronchodilator drug that helps to draw more accurate conclusions.
Spirography - indications
The point of the study is to determine how lung volume changes during normal and increased breathing. Spirography is performed for bronchial asthma and other pathologies. In addition, with the help of such procedures, the effectiveness of the chosen treatment is established. Spirography is prescribed for the following symptoms:
- prolonged cough;
- frequent respiratory diseases;
- chest pain;
- shortness of breath and a feeling of incomplete inspiration;
- acute allergic reactions.
Spirography - contraindications
Not everyone is allowed to undergo such a procedure, so it is important to take into account existing contraindications. FVD spirography is prohibited in the presence of the following factors:
- sepsis;
- pneumothorax;
- acute myocardial infarction;
- exacerbation of bronchial asthma;
- tuberculosis;
- increased hemoptysis;
- serious mental disorders;
- other serious health problems.
How the study is conducted and the results are evaluated
Before starting regular measurements, the peak flow meter is adjusted taking into account the normal values of peak expiratory force (PEF), which depends on the gender, age group and height of the patient. When setting up, according to special tables, the boundaries of the areas (normal, alarming and unsatisfactory) are calculated.
For example, the norm for PSV in a man of middle age and height (175 cm) is 627 l/min. The normal area (it is marked in green on the device) is at least 80% of the norm, that is, 501.6 l/min.
The alarming level (yellow color) includes indicators from 50 to 80% (in this case, from 313.5 to 501.6 l/min).
All values below the alarm area limit will be marked as unsatisfactory (red).
Important. As an option for setting the peak flow meter, the patient's spirometry readings can be used (the best study indicator is taken as the basis).
Will FVD indicate asthma in a child and how?
The patient's main indicators are measured, then their relationship to the norm is determined.
A patient with obstructive diseases has a decrease in values below 80% of normal, and the ratio of FEV to FVC (Hensler index) is below 70%. Asthma is characterized by reversible obstruction of the upper airways. This means that the FEV/VC ratio increases after salbutamol administration. To diagnose asthma, in addition to the respiratory function indicators indicating pathology, the patient must have clinical signs of the disorder.
FVD in children. FVD study at the InetgraMedService clinic. Dr. Kuleshova Yu.A.
Terms of use
To obtain the most complete picture, peak flowmetry is carried out twice a day - in the morning and in the evening. Special preparation for diagnosis is not required, but there are a number of rules that require strict adherence:
- diagnosis is carried out before taking medications;
- before starting the study, the pointer slider is set to the beginning of the scale;
- During measurements, the patient stands or sits (the back is straight);
- the device is held in a horizontal position with both hands (hands do not cover the slider and holes);
- First, inhale deeply and hold your breath for a short time, after which you exhale as quickly as possible.
Important. Each measurement is performed three times, with short breaks. The maximum reading of the device is recorded and noted in an individual chart, which the doctor subsequently becomes familiar with.
What equipment and devices are used in medicine to carry out analysis?
To conduct different types of FVD studies, different devices are used:
- Portable spirometer with thermal printer SMP 21/01;
- Spirograph KM-AR-01 “Diamant” – pneumotachometer;
- “Schiller AG” analyzer, it is convenient to use for samples with bronchodilators;
- The Microlab spiro analyzer has a touch screen; functions are switched by touching the function icon;
- Portable spirograph "SpiroPro".
This is only a small part of the devices that record external respiration functions. Medical equipment manufacturing companies offer institutions portable and stationary devices. They differ in capabilities, each group has its own advantages and disadvantages. For hospitals and clinics, it is more important to purchase a portable device that can be moved to another office or building.
Additional Research
In addition to the basic research methods, doctors often use additional tests to clarify the diagnosis or assess the effectiveness of treatment.
So, during spirometry tests are prescribed with:
- salbutamol;
- physical activity;
- methacholine.
Salbutomol is a drug with a bronchodilator effect. A functional test with it is carried out after control studies and allows you to determine whether the narrowing in the bronchi is reversible or not. It also gives a more accurate picture of the state of the respiratory system and makes it possible to clarify the diagnosis. So, if FEV1 improves after taking a bronchodilator, this indicates asthma. If the test gives a negative result, this indicates chronic bronchitis.
Methacholine is a substance that provokes spasms (hence the name of the test - provocative test) and allows you to determine asthma with 100% accuracy.
As for exercise tests, in this case the second study is carried out after exercise on a bicycle or treadmill and allows you to determine exercise asthma with maximum accuracy.
A diffusion test is often used as an additional study. It allows you to assess the speed and quality of oxygen supply to the blood.
Reduced indicators in this case indicate the development of lung disease (and in an already quite advanced form), or possible thromboembolism of an artery in the lungs.
Tags: Measurement
Pulmonary function test
It is used to determine lung volumes and velocities. Additionally, functional tests are often prescribed to record changes in these indicators after the action of any factor.
Indications and contraindications
The study of respiratory function is carried out for any diseases of the bronchi and lungs, accompanied by impaired bronchial obstruction and/or a decrease in the respiratory surface:
- Chronical bronchitis;
- bronchial asthma;
- pneumonia;
- chronic obstructive pulmonary disease;
- silicosis;
- idiopathic fibrosing alveolitis and others.
The study is contraindicated in the following cases:
- children under 4–5 years of age who cannot correctly follow the nurse’s commands;
- acute infectious diseases and fever;
- severe angina pectoris, acute period of myocardial infarction;
- high blood pressure, recent stroke;
- congestive heart failure, accompanied by shortness of breath at rest and with slight exertion;
- mental disorders that do not allow you to correctly follow instructions.
External respiration function: how the study is carried out
The procedure is carried out in a functional diagnostics room, in a sitting position, preferably in the morning on an empty stomach or no earlier than 1.5 hours after a meal. As prescribed by the doctor, bronchodilators that the patient is constantly taking can be discontinued: short-acting beta2 agonists - 6 hours, long-acting beta2 agonists - 12 hours, long-acting theophyllines - a day before the examination.
Pulmonary function test
The patient's nose is closed with a special clip so that breathing is carried out only through the mouth, using a disposable or sterilizable mouthpiece (mouthpiece). The subject breathes calmly for some time, without focusing on the breathing process.
Then the patient is asked to take a calm maximum inhalation and the same calm maximum exhalation. This is how vital capacity is assessed. To assess FVC and FEV1, the patient takes a calm, deep breath and exhales all the air as quickly as possible. These indicators are recorded three times at short intervals.
At the end of the study, a rather tedious registration of MVL is carried out, when the patient breathes as deeply and quickly as possible for 10 seconds. During this time, you may feel slightly dizzy. It is not dangerous and goes away quickly after stopping the test.
Many patients are prescribed functional tests. The most common of them:
- test with salbutamol;
- exercise test.
Less often a test with methacholine is prescribed.
When conducting a test with salbutamol, after recording the initial spirogram, the patient is asked to inhale salbutamol, a short-acting beta2 agonist that dilates spasmodic bronchi. After 15 minutes, the study is repeated. You can also use inhalation of the M-anticholinergic ipratropium bromide, in which case the test is repeated after 30 minutes. Administration can be carried out not only using a metered dose aerosol inhaler, but in some cases using a spacer or nebulizer.
The test is considered positive when the FEV1 indicator increases by 12% or more while simultaneously increasing its absolute value by 200 ml or more. This means that the initially identified bronchial obstruction, manifested by a decrease in FEV1, is reversible, and after inhalation of salbutamol, bronchial patency improves. This is observed in bronchial asthma.
If, with an initially reduced FEV1 value, the test is negative, this indicates irreversible bronchial obstruction, when the bronchi do not respond to drugs that dilate them. This situation is observed in chronic bronchitis and is not typical for asthma.
If, after inhalation of salbutamol, the FEV1 indicator decreases, this is a paradoxical reaction associated with bronchospasm in response to inhalation.
Finally, if the test is positive against the background of an initial normal FEV1 value, this indicates bronchial hyperreactivity or hidden bronchial obstruction.
When conducting a load test, the patient performs an exercise on a bicycle ergometer or treadmill for 6–8 minutes, after which a repeat test is performed. When FEV1 decreases by 10% or more, they speak of a positive test, which indicates exercise asthma.
To diagnose bronchial asthma in pulmonology hospitals, a provocative test with histamine or methacholine is also used. These substances cause spasm of the altered bronchi in a sick person. After inhalation of methacholine, repeated measurements are taken. A decrease in FEV1 by 20% or more indicates bronchial hyperresponsiveness and the possibility of bronchial asthma.
How are the results interpreted?
Basically, in practice, the doctor of functional diagnostics focuses on 2 indicators - vital capacity and FEV1. Most often they are assessed according to the table proposed by R. F. Clement et al. Here is a general table for men and women, which shows percentages of the norm:
| Options | Normal limits | very light | Lung | moderate | significant | very significant | sharp |
| Vital. | 78,2 – 113,3 | 72,0 | 65,8 | 59,6 | 53,4 | 47,1 | 40,9 |
| FEV1. | 77,4 – 113,8 | 72,0 | 66,6 | 61,2 | 55,8 | 50,4 | 45,0 |
For example, with a vital capacity of 55% and an FEV1 of 90%, the doctor will conclude that there is a significant decrease in the vital capacity of the lungs with normal bronchial patency. This condition is typical for restrictive disorders in pneumonia and alveolitis. In chronic obstructive pulmonary disease, on the contrary, vital capacity may be, for example, 70% (slight decrease), and FEV1 – 47% (sharply decreased), while the test with salbutamol will be negative.
We have already discussed the interpretation of tests with bronchodilators, exercise and methacholine above.
Pulmonary function: another way to assess
Another method of assessing external respiration function is also used. With this method, the doctor focuses on 2 indicators - forced vital capacity (FVC) and FEV1. FVC is determined after a deep breath with a sharp full exhalation, lasting as long as possible. In a healthy person, both of these indicators are more than 80% of normal.
If FVC is more than 80% of normal, FEV1 is less than 80% of normal, and their ratio (Genzlar index, not Tiffno index!) is less than 70%, they speak of obstructive disorders. They are associated primarily with impaired bronchial patency and the exhalation process.
If both indicators are less than 80% of the norm, and their ratio is more than 70%, this is a sign of restrictive disorders - lesions of the lung tissue itself that prevent full inspiration.
If the values of FVC and FEV1 are less than 80% of normal, and their ratio is less than 70%, these are combined disorders.
To assess the reversibility of obstruction, look at the FEV1/FVC value after inhalation of salbutamol. If it remains less than 70%, the obstruction is irreversible. This is a sign of chronic obstructive pulmonary disease. Asthma is characterized by reversible bronchial obstruction.
If irreversible obstruction is identified, its severity must be assessed. For this purpose, FEV1 is assessed after inhalation of salbutamol. When its value is more than 80% of the norm, we speak of mild obstruction, 50–79% – moderate, 30–49% – severe, less than 30% of the norm – severe.
Pulmonary function testing is especially important to determine the severity of bronchial asthma before treatment. In the future, for self-monitoring, patients with asthma should perform peak flow measurements twice a day.