What is thyroglobulin and when does it appear in the blood?
The hormones produced by the thyroid gland are called thyroxine (T4) and triiodothyronine (T3).
These hormones, being in active connection with iodine, affect almost all tissues of the body. They are able to increase the level of basal metabolism, give a person wakefulness and vitality, and improve mental activity. Thyroid hormones regulate body temperature and increase the flow of glucose into the blood, which allows for increased muscle activity. We can say that the function of thyroid hormones increases the oxidative potential of the body, and if we compare the human body with the firebox of a furnace, then the effect of these hormones is reduced to increasing the supply of oxygen to this firebox. They are normally produced from a special protein precursor - thyroglobulin, and one of the key tests used in endocrinology is a blood test to detect antibodies to thyroglobulin, abbreviated AT TG.
In a healthy person, thyroglobulin is synthesized in special cells of the thyroid gland, which are called basal cells. After this, it is transported from the cells to the follicular tissue, and is stored there in the form of a special colloidal substance.
Thyroglobulin is a unique compound; there is no other molecule like it in the body. From a chemical point of view, it is a glycoprotein, that is, a protein molecule associated with carbohydrate residues. Its mass is very large - 600 kilodaltons. This means that such a large molecule cannot enter the blood unless special conditions are created. What is thyroglobulin in a blood test? It occurs only when the integrity of the follicular cells is disrupted and the molecule enters the general bloodstream.
Normal thyroid hormones, T3 and T4, are synthesized for a reason; they are assembled from various small structural subunits, but inside this large thyroglobulin molecule. After many hormone molecules are synthesized on one thyroglobulin molecule, it is broken down using proteolytic lysosomal enzymes. After this, newly synthesized thyroid hormones are released, and iodine also becomes free, which is again used to build hormones.
Every day, the thyroid gland, thanks to thyroglobulin, synthesizes up to 90 mcg of the T4 hormone and up to 9 mcg of the T3 hormone. The breakdown of thyroglobulin does not occur immediately after the synthesis of hormones, but as needed. In an adult healthy person, such a reserve of thyroid hormones in thyroglobulin is quite large, and it can ensure their normal supply to the blood for up to two months, thanks to such endogenous reserves. This unique situation does not occur in any other human endocrine organs.
In healthy people, the immune system accepts this compound as its own protein. However, due to some autoimmune disorders, the body begins to perceive its cells as foreign. In this case, antibodies to thyroglobulin (anti tg) are produced. When there is an excess amount of them in the tissues of the thyroid gland, autoimmune diseases occur, often causing hypothyroidism.
If the level of thyroglobulin is elevated, then this clearly indicates problems with the thyroid gland. But for the primary diagnosis of endocrine pathology, this method is rarely used; for this purpose, hormones are first examined.
Thyroglobulin itself is determined in patients with thyroid cancer, for whom it is a tumor marker. His study is a very convenient indicator of the effectiveness of surgical intervention for malignant neoplasms. If its level before surgery was high (which is most often detected), then after surgery its concentration quickly decreases. But if its concentration before surgery was normal, which is also possible in case of thyroid cancer, then it makes no sense to use it to monitor the effectiveness of treatment. But let’s return to the analysis of At to Tg
Now it becomes clear what harm are caused by antibodies that block and paralyze the work of such an important compound - thyroglobulin
Reasons for the increase and accompanying symptoms
Elevated antibody levels are most often diagnosed in the following cases:
- Hashimoto's thyroiditis (autoimmune thyroiditis);
- diffuse toxic goiter;
- malignant tumors in the thyroid gland;
- after resection of the gland.
These conditions are described in more detail below.
In addition, the concentration of antibodies increases in diseases such as:
- Myxedema. This pathology is an extreme form of hypothyroidism, or thyroid deficiency. The disease mainly affects women. Patients develop a peculiar appearance: thickened lips and nose, swollen eyelids and an indifferent facial expression. Among other symptoms, patients note an enlarged tongue (sometimes it does not fit in the mouth) and a feeling of dry mouth. The tissues of the larynx also swell, causing the patient's voice to become duller.
- Diabetes mellitus type I. With this disease, a deficiency of pancreatic beta cells develops, which are responsible for determining the need for insulin and its production. The pathology is characterized by a genetic predisposition, but it can occur not only in childhood, but also in old age. Risk factors for the manifestation of the disease are viral infections (including those of the upper respiratory tract), stress, poisoning with heavy metals and other toxic substances, consumption of foods containing soy, gluten, easily digestible carbohydrates, cow's milk proteins and unsaturated fats. Among the most characteristic symptoms are dry mouth, thirst, constant hunger, and increased urination.
- Non-toxic nodular goiter , developing with prolonged iodine deficiency in the body. It is non-tumoral in nature and manifests itself in the form of a single nodular formation.
- Other autoimmune diseases:
- Pernicious anemia , developing due to a deficiency of vitamin B12 and folic acid. Patients experience neurological damage due to irreversible death of nerve cells.
- Autoimmune hemolytic anemia. With this disease, premature destruction of red blood cells occurs under the influence of antibodies.
- Systemic lupus erythematosus – damage to connective tissue and blood vessels.
- Sjögren's disease is a connective tissue pathology accompanied by multiple lesions of the secreting glands.
- Rheumatoid arthritis is an inflammation of connective tissue affecting small joints.
- Myasthenia Gravis is a neuromuscular pathology accompanied by rapid fatigue of striated muscles.
Removal of the thyroid gland
Removal of the thyroid gland is usually performed if a malignant tumor is detected or the nodes in it reach a significant size, making it difficult for the patient to breathe. A study of the level of thyroglobulin and AT-TG is done six months to a year after removal of this organ. The patient receives hormone replacement therapy throughout the postoperative period.
Antibodies to thyroglobulin may be elevated after complete removal of the gland in women when the tumor producing thyroglobulin has reappeared, but in a different location. Additional diagnostics are necessary, and to prevent this condition, all patients after resection are recommended to donate blood annually to determine antibodies.
Thyroid cancer
One of the features of malignant tumors located in the thyroid gland is that they have the ability to produce thyroglobulin. As a result, its total level increases by 2 or more times.
The prevalence of this disease is on average 8 people per 100 thousand population among women. At the initial stage, the disease is most often asymptomatic; some patients complain of a nodule in the neck, hoarseness and difficulty swallowing food.
For diagnosis, the following types of studies are carried out:
- determination of the level of thyroid-stimulating hormone and calcitonin produced by thyroid cells;
- Ultrasound;
- aspiration biopsy under ultrasound control and subsequent cytological examination - determination of the characteristics of cellular elements;
- Neck scintigraphy is a radioisotope study at the preoperative stage to remove a malignant tumor.
Autoimmune thyroiditis
Autoimmune thyroiditis is one of the most common pathologies of the thyroid gland. In this disease, the human immune system perceives gland cells as foreign and attacks them, leading to the development of a chronic inflammatory process and destruction of organ tissue.
The prevalence of autoimmune thyroiditis in women is several times higher than among men. Patients over 60 years of age (up to 20% of the population) are especially susceptible to this pathology. Most often, this disease manifests itself in a familial (hereditary) form. Often the patient or his relatives have other autoimmune disorders.
Against the background of thyroiditis, hypothyroidism develops in 90% of cases, that is, the production of thyroid hormones decreases.
Risk factors for this disorder are:
- lack or excess of iodine in food;
- radioactive exposure;
- pregnancy and the postpartum period in women;
- presence of other autoimmune diseases;
- influence of unfavorable environmental factors.
At the initial stage, subjective symptoms may be completely absent.
As the disease progresses, the following signs appear:
- enlargement of the thyroid gland and tuberosity of its surface;
- increased fatigue;
- feeling hot and sweating;
- irritability;
- weight loss;
- drowsiness;
- chilliness;
- constipation;
- memory loss;
- hair loss;
- decrease in heart rate.
Diffuse toxic goiter
Antibodies to thyroglobulin are elevated in women also with diffuse toxic goiter. This disease is especially common in iodine-deficient areas. It is also autoimmune (the production of antibodies to the thyroid hormone TSH increases).
Its greatest prevalence occurs at the age of 20-40 years, and the provoking factors are:
- hereditary predisposition;
- chronic stress;
- infectious and inflammatory diseases;
- unfavorable environmental factors;
- bad habits (smoking).
The symptoms of this disease are primarily due to neurological disorders:
- increased physical activity;
- excitability and irritability;
- emotional instability, aggressiveness;
- tearfulness;
- worsening sleep;
- fast fatiguability;
- tremor (shaking) of the limbs;
- rare blinking of the eyes, their increased shine (“crystal” eyes) as a result of the wide opening of the palpebral fissures.
What is thyroglobulin
If a person is completely healthy, then the content of this protein in the follicles is mandatory. It is also produced exclusively by thyroid cells. That is why many patients are interested in the question, what is this indicator - ATTG?
In sufficiently small quantities, thyroglobulin itself can be quickly released from thyroid cells and almost immediately enter the bloodstream.
To this day, scientists and doctors cannot establish why thyroglobulin turns into an anti gene, which is autoimmune in nature.
In other words, a given protein can become a substance that can be isolated only under certain specific conditions. In this case, it will act as a foreign agent. In response to its appearance, the body begins to intensively produce antibodies to thyroglobulin.
If its indicator is elevated, this may indicate the presence of a pathological process in the body:
- Antibodies to thyroglobulin are determined precisely in order to determine whether a person has thyroid disease. They can block the thyroglobulin protein itself in a fairly short time. Because of this, some disturbances occur in the synthesis of one or several hormones produced by the thyroid gland.
- If processes occur in which antibodies to thyroglobulin increase, an inflammatory process in the thyroid gland begins. In this case, both its deficiency, that is, hypothyroidism, and excessive production of the hormone, called hyperthyroidism, can develop.
Indications
The AT-TG marker allows you to identify autoimmune lesions of the thyroid gland (Hashimoto's disease, diffuse toxic goiter, atrophic autoimmune thyroiditis, etc.). The analysis is also used for the differential diagnosis of endocrine pathologies in iodine-deficient areas and the treatment of children born to mothers with an increased concentration of antibodies to TG. In addition, testing for AT-TG is necessary to monitor the rehabilitation of patients with thyroid cancer. In this case, the purpose of testing is to prevent disease relapse and metastasis.
According to the statistics of AT to TG, the following are determined:
- 40-70% of cases in patients with chronic thyroiditis (inflammation of the thyroid gland);
- 70% - with hypothyroidism (lack of function);
- 35-40% for toxic goiter (increase in size and change in the functional state of the gland);
- less often in other cases (including with pernicious anemia).
According to a 2012 study by the British Association of Dermatologists, patients with vitiligo have a higher risk of autoimmune thyroid disease. 9.7% of the examined people with vitiligo had antibodies to TG.
Antibody levels can also be elevated in healthy people (for example, in 10% of cases in menopausal women).
Indications for the purpose of analysis are as follows:
- changes in the size, shape, structure of the thyroid gland;
- blurred vision, ophthalmopathy;
- sudden weight loss or gain without objective reasons;
- rapid heartbeat (tachycardia) or arrhythmia;
- increased weakness and fatigue, decreased performance;
- monitoring the effectiveness of treatment with thyroglobulin after removal of a tumor on the gland;
- systemic autoimmune processes (to determine the risk of thyroid damage);
- problems in the reproductive sphere in women;
- dense swelling of the lower extremities, which may indicate pretibial myxedema;
- for differential diagnosis of toxic and non-toxic (for example, iodine deficiency) nodular goiter;
- monitoring the condition of pregnant patients if they have a history of autoimmune diseases (analysis is carried out upon registration and in the 3rd trimester of pregnancy);
- to determine risk groups for the development of thyroid diseases among children born to mothers with pathology of the endocrine organs.
What is thyroglobulin
Thyroglobulin (TG) is a type of protein produced by the follicular cells of the thyroid parenchyma. It is deposited in the lipids of the follicle (the structural unit of the thyroid gland) as a colloid. Modern research suggests that TG is a depot of iodine and supplies this useful element to other organs
At the moment this has not been proven, but the importance of thyroglobulin cannot be denied. This protein is used by the body to generate the hormones thyroxine and triiodothyronine (T4 and T3, respectively)
In the blood of a healthy person, the protein is found in extremely low concentrations, since it is stored precisely in the follicles of the thyroid gland. An analysis for antibodies to TG will help identify an increase in the amount of the substance, which will allow doctors, after decoding, to diagnose a number of diseases.
What to do if antibodies to thyroglobulin are very elevated: principles of treatment
AT to thyroglobulin is not a disease, but an indicator of the ill health of the endocrine system. To determine the appropriate treatment strategy, patients are prescribed additional examination. To diagnose the disease, do:
- histological examination;
- immunogram;
- Ultrasound of the thyroid gland;
- analysis for T3 and T4.
There is no specific treatment for autoimmune thyroid diseases. Most often limited to symptomatic therapy. Medicines are prescribed that eliminate the consequences of autoimmune disorders - hypo- or hyperactive thyroid gland.
Principles of treatment of various diseases:
- Autoimmune thyroiditis. To reduce the titers of antibodies to thyroglobulin, take non-steroidal anti-inflammatory drugs - Almiral, Argette Duo, Indomethacin. For severe inflammation of the gland, glucocorticosteroids with prednisolone are used.
- Hypothyroidism. If T3 and T4 are insufficient, hormone replacement therapy with levothyroxine is performed. During treatment, patients should visit their doctor periodically to have their thyrotropin levels monitored.
- Thyrotoxicosis. To reduce the synthesis of T3 and T4, antithyroid therapy is prescribed. Patients take Metizol, Propicil, Tyrosol, etc. Women often experience complications in the form of thyrotoxic crisis. Therefore, if therapy is ineffective, they are prescribed thyroidectomy - excision of the thyroid gland.
- Thyroid cancer. Treatment options depend on the size and location of the tumor. Patients usually undergo surgical treatment and chemotherapy to prevent relapses. If surgery is contraindicated, radioactive iodine and hormonal drugs are taken.
Severe autoimmune aggression towards thyroid cells is an indication for taking immunosuppressants and cytostatics. They suppress the immune system, due to which the amount of antibodies to thyroglobulin in the blood decreases.
Tests for thyroid hormones are the main symptoms of the complaint, allowing one to suspect hyperthyroidism
- feeling hot and sweating;
- weight loss;
- constant thirst;
- excessive urination and diarrhea;
- rapid heartbeat and interruptions in heart function;
- eye symptoms: bulging eyes (exophthalmos), swelling around the eyes, inability to concentrate on an object, double vision;
- change of character. Patients become fussy, agitated, and often aggressive. The mood of patients with thyrotoxicosis also changes very quickly from euphoria to depression. Tearfulness often appears;
- hair change. The hair of patients becomes brittle, thin and may fall out rapidly.
How is the analysis done?
Blood is usually taken from a vein. Preferably in the morning on an empty stomach. Doctors recommend not eating in the evening. In addition to these requirements, there are a number of others:
- It is not recommended to smoke the day before the test. Avoid strenuous physical activity;
- To get a reliable result, along with determining the level of TG in the blood, it is necessary to check the amount of antibodies to thyroglobulin. A high level of antibodies, which is a pathology, leads to a low content of thyroglobulin;
- If a person takes hormones produced by the thyroid gland, such as thyroxine, they must be stopped three weeks before the test;
- After surgery to remove a thyroid tumor, it is advisable to check your TG levels at least three months later. In the case of using radioactive iodine - after six months.
There are times when the results turn out to be false. There are a number of reasons for this:
- Presence of antibodies to thyroglobulin. Therefore, their level must be checked, since because of them, the amount of TG in the blood is reduced;
- Taking hormonal medications, iodine supplements. Oral contraceptives taken by a woman to prevent pregnancy may also affect TG levels;
- The presence of infectious diseases, as well as genetic predisposition;
- If the person has been exposed to radiation or there are other toxic substances in the blood;
- Severe stress experienced;
- In elderly women, as well as in pregnant women, an increase in the amount of TG may be observed, when, as in men, as observations show, the level of thyroglobulin does not depend on age.
General information about thyroglobulin
Thyroglobulin is the largest glycoprotein (protein) that is stored in the colloid of the thyroid follicle.
The presence of this prohormone is a necessary condition for the synthesis of hormones such as thyroxine (T4) and triiodothyronine (T3).
The only source of thyroglobulin, which consists of iodine and the amino acids tyrosine, is the thyroid gland.
The production of this prohormone occurs in the cells of a healthy thyroid gland and in the cells of papillary and follicular adenocarcinoma of this organ (in malignant neoplasms).
Determining the level of thyroglobulin is one of the most effective methods for monitoring the appearance of malignant neoplasms in the thyroid gland.
The glycoprotein is stored as a kind of reserve in the lumens of the follicles until the body needs it.
When such a moment occurs, the thyroglobulin molecule is captured by the cells of the thyroid gland, passed through them, dividing into tyrosine and iodine, and in this “divided” form enters the blood.
Causes and symptoms of changes in the level of thyroglobulin in the blood
Low or high levels of thyroglobulin occur in most patients with thyroid dysfunction. But it is impossible to determine the type of disease based on the content of prohormone T3 and T4. To clarify the diagnosis, patients are referred for further examination. To confirm oncology, a chest x-ray, MRI, ultrasound or is prescribed.
Increased concentration
If thyroglobulin is elevated in patients with previously diagnosed adenocarcinoma, this indicates an exacerbation of cancer. In this case, there is a direct relationship between the concentration of TG and the size of malignant neoplasms. In patients of other groups, elevated thyroglobulin indicates:
- subacute thyroiditis;
- hyperthyroidism;
- endemic goiter;
- Hashimoto's syndrome;
- iodine deficiency conditions;
- tumors in the adenohypophysis;
- Graves' disease;
- nodular toxic goiter;
- benign adenoma.
Sometimes elevated thyroglobulin levels are caused by hormonal therapy or radioactive iodine. High TG is found in men and women who have undergone ethanol sclerotherapy for cystic nodular formations in the gland.
Most therapeutic and diagnostic procedures that affect thyrocytes lead to an increase in serum TG concentrations.
Elevated thyroglobulin during the treatment of cancer indicates the need to adjust the treatment regimen, increase the dose of chemotherapy, etc. Only a specialist can understand the test results. Sometimes an imbalance of T3 and T4 caused by pathologies of the adenohypophysis also affects the TG content.
Decreased concentration
A drop in TG in patients with adenocarcinoma in the thyroid gland indicates the effectiveness of treatment and the absence of secondary neoplasms. But even if thyroglobulin is lowered, this does not indicate complete recovery. Other reasons for a decrease in TG in the blood include:
- inhibition of secretory activity of the thyroid gland;
- errors when collecting biomaterial for analysis;
- congenital anomalies of the thyroid gland;
- chronic stress;
- iodine deficiency;
- exacerbation of toxoplasmosis or mononucleosis.
Biochemical analysis is carried out in combination with a test for antibodies (AT) to thyroglobulin. An increased level of AT indicates the autoimmune nature of the thyroid disease. Manifestations of pathology include:
- thickening of the thyroid gland;
- moderate pain in the throat area;
- labored breathing;
- reduction or enlargement of the thyroid lobes.
Symptoms of endocrine diseases increase slowly, so patients do not rush to see a doctor. The reasons for contacting an endocrinologist are:
- problems with conception;
- depression;
- difficulty falling asleep;
- menstrual irregularities;
- decreased libido, etc.
Most endocrine diseases are polysymptomatic, that is, thyroid dysfunction affects the functioning of many internal organs and systems.
It is recommended to undergo a preventive examination if close relatives suffered from autoimmune or oncological pathologies.
AT-TPO and AT-TG
Articles from all conferences.
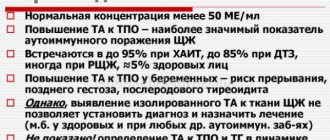
Dear patient! The creation of this topic was dictated by widespread recommendations for studying the level of antibodies to the thyroid gland without appropriate indications. The consequences of such recommendations are a waste of money (own or budgetary) and, often, inadequate clinical decisions. The material presents key aspects of the problem of antibodies to the thyroid gland and the most common errors associated with their definition and interpretation. —————————————————————————- What are antibodies (AT)? Antibodies are proteins synthesized by cells of the immune system. The main function of antibodies is to identify and neutralize foreign objects, such as bacteria and viruses. However, it happens that antibodies begin to be produced against healthy tissues of one’s own body. What antibodies can be produced to the thyroid gland (TG)? In the thyroid gland, the most popular targets for antibody production are the enzyme thyroid peroxidase (TPO) and the matrix for hormone synthesis, thyroglobulin (TG). Accordingly, AT-TPO and AT-TG are more often detected during examination. In clinical practice, the determination of not so common antibodies to the thyroid-stimulating hormone receptor (AT-rTSH), which stand apart from AT-TPO/AT-TG in diagnostic terms, is also used. What does an increase in AT-TPO and/or AT-TG levels indicate? The production of AT-TPO and AT-TG does not always lead to the development of autoimmune diseases. The detection of elevated AT-TPO and/or AT-TG in the blood serum does not allow establishing a diagnosis of autoimmune thyroid disease. According to epidemiological data, about 15-20% of the healthy population are carriers of thyroid antibodies. At the same time, elevated levels of AT-TPO and AT-TG often indicate autoimmune damage to the thyroid gland. Therefore, if thyroid function is impaired, testing the level of antibodies can help in diagnosing and confirming the autoimmune nature of the disease. In this case, it is sufficient to determine AT-TPO (a more sensitive marker of autoimmune thyroid pathology)
AT-TG acquires independent clinical significance only after treatment of highly differentiated thyroid cancer. Is it necessary to reduce and control the levels of AT-TPO and AT-TG? It is important to emphasize that antibodies to TPO and TG are not a key element in the pathogenesis of autoimmune thyroid diseases and begin to be produced in response to damage to the thyroid gland. Therefore, attempts to reduce the level of antibodies are devoid of any practical meaning (even if their concentrations exceed the standards hundreds of times!!!)
Assessing AT-TPO levels over time is also not recommended, because has no prognostic value. Monitoring AT-TG may be appropriate only after surgical treatment of differentiated thyroid cancer. To whom and when is the study of AT-TPO and AT-TG indicated? A SINGLE study of AT-TPO can be useful in the following situations: - when identifying hypofunction of the thyroid gland (TSH>4 mU/l) - with an increase in the thyroid gland (>18 ml in women, > 25 ml in men) against the background of reduced or normal thyroid function - before prescribing amiodarone, interferon and lithium drugs (since carriers of antibodies have an increased risk of developing thyroid pathology induced by these drugs) - if TSH is detected >2.5 mU/l during pregnancy (carriage of AT-TPO is an argument in favor of prescribing L-thyroxine and control thyroid function after pregnancy) - in the differential diagnosis of thyrotoxicosis (EXTREMELY RARE, only after determining the level of antibodies to the TSH receptor, which were mentioned at the beginning of the conversation) The study of AT-TPO in other situations can be considered redundant, and the interpretation of the results is meaningless. The diagnostic niche of AT-TG research is limited to monitoring patients after treatment for differentiated thyroid cancer.
—Copyright to this article belongs to the Rusmedserv website and MarinaAS personally. The original is available here: https://forums.rusmedserv.com/showthread.php?t=171173 At the first request of the copyright holder, if this follows, the article will be removed from this site. The publication is intended for educational purposes only.
Author of the article: Alexander
Proper preparation before the analysis of antibodies to thyroglobulin
To obtain a reliable result, before donating blood, it is necessary to eliminate all risks that can cause an imbalance in the endocrine system.
The correct approach before AT TG studies:
- Avoid taking hormonal medications for 6 weeks;
- stop taking thyroxine and its derivatives 3 weeks before;
- 3 days in advance, exclude fatty, fried, sour foods, alcohol, energy drinks;
- At least 8 hours must pass after the last meal;
- avoid physical and emotional stress per day;
- 3 hours in advance do not smoke, do not use mouth sprays or chewing gum.
Other causes of hyperthyroidism include
- Nodular diseases of the thyroid gland.
- Increased iodine consumption, which can also lead to thyrotoxicosis, especially against the background of an existing thyroid disease (the so-called “Iodine-Bazedov”)
- Postpartum thyroiditis, which occurs in every 20th woman after childbirth. It is discussed in more detail in the section “The Thyroid Gland and Pregnancy”.
- Overdose of thyroid hormones in the treatment of hypothyroidism and goiter. Some women take large doses of thyroxine to control body weight, causing drug-induced thyrotoxicosis.
- Increased function of the pituitary gland, leading to constant stimulation of the thyroid gland.
Possible complications
In the absence of timely correction of the thyroid gland, the patient develops serious complications against the background of progressive pathological changes:
- depression develops;
- attacks of suffocation occur periodically;
- severe shortness of breath appears;
- body weight decreases;
- a person is worried about insomnia;
- patients complain of angina pectoris;
- heart failure is diagnosed.
A complication of a high level of antibodies to thyroglobulin (AT-TG) is also toxic hepatosis, atrial fibrillation, limb tremors, and hypothyroid coma. The greatest danger to human life is a malignant tumor. Delayed treatment in most cases leads to death.
The functioning of all internal organs and systems of the human body depends on the proper functioning of the thyroid gland. If AT-TG is very elevated, then you need to go to the hospital and undergo an examination. Identifying any disease at an early stage will allow timely treatment to begin and prevent serious consequences for a person.
Article design: Vladimir the Great
Rules for donating blood and interpretation of test results for thyroglobulin levels
After removal of the thyroid gland, an analysis of the concentration of thyroglobulin in the blood is recommended only after 3 months after surgery or 6 months if a course of treatment with radioactive iodine was carried out.
Taking the test before these dates will not give a real picture and may show a false increase in thyroglobulin levels, which in turn makes one think about a recurrence of cancer.
In a situation where antibodies to thyroglobulin are highly elevated in the body, an analysis for thyroglobulin itself will not be of any value, since the antibodies will kill protein molecules and its concentration will not be significant.
An analysis of venous blood for TG, done against the background of a 3-week withdrawal from taking a thyroxine-based drug, is the most accurate marker of the reappearance of malignant neoplasms (carried out only in the absence of elevated antibodies to the glycoprotein).
In most cases, it is more important to see the dynamics of changes in thyroglobulin concentration than its value itself. This means that even with its increased level, treatment can be considered successful if there is a positive dynamics of its decline
This means that even with its elevated level, treatment can be considered successful if there is a positive trend in its decline.
Normal levels of AT-TG in the blood of women
The normal level of antibodies to thyroglobulin in the blood is in the range of 0-115 IU/ml. The upper limit may vary slightly between laboratories. The reference value must be indicated on the analysis form. Most often, the study is performed using electrochemiluminescent immunoassay.
Pregnancy
During pregnancy, the increase in the size of the thyroid gland is a physiological process. The level of hormones also increases, which is associated with increased excretion of iodine in the urine and an increase in the concentration of protein that binds thyroxine.
These processes ensure normal development of the fetus and the course of pregnancy. The average level of AT-TG during this period of life in women is 243 IU/ml.
Antibodies to thyroglobulin are elevated in women during gestation and can be up to 580 IU/ml. As pregnancy progresses, the concentration of AT-TG gradually decreases, which is explained by a natural decrease in immunity to prevent fetal rejection.
Sometimes the mechanism of hormonal changes can go beyond the norm. In these cases, pregnant women develop endocrinopathies - thyrotoxicosis, hypothyroidism and other pathologies.
Menopause
During menopause, women undergo active hormonal changes in the body. During this period, the likelihood of disorders in the thyroid gland increases. Its various pathologies are observed in 14-20% of cases. Most often, thyroiditis, hypothyroidism and nodular goiter develop.
Normally, the level of AT-TG during menopause can increase by 5-6% of the normal value, which is not a violation.
Increased levels of antibodies to thyroglobulin
The level of AT to TG increases in the presence of the following diseases:
- diffuse toxic goiter, which is characterized by excessive production of the hormone T3 or T4, as well as intoxication of the thyroid gland itself;
- nodular goiter - specific nodes form on the thyroid gland, and the formation of thyroid hormone increases several times;
- Autoimmune thyroiditis is a chronic disease: it occurs when the patient has a partial genetic defect of the immune system, it leads to irreversible structural changes in the organs of the endocrine system, then there is an increase in destructive phenomena in the thyroid gland, which leads to the appearance of hypothyroidism;
- granulomatous thyroiditis is characterized by a non-purulent inflammatory process in the thyroid gland: most often its occurrence is associated with a viral disease such as influenza, mumps or measles;
- idiopathic myxedema occurs due to incomplete supply of the body with thyroid hormones and is characterized by severe swelling of tissues and organs;
- diffuse connective tissue disease, lesions of small joints, Sjögren's disease;
- genetic diseases;
- postpartum failure of the thyroid gland in women;
- type 1 diabetes
Thyroglobulin and antibodies are of great diagnostic importance for thyroid diseases.
Therefore, in case of the slightest suspicion of any deviations in her work, the doctor prescribes an appropriate study.
It should be remembered that a blood test should be taken only according to strictly defined rules. After all, if they are not followed, the result of the study may turn out to be completely unreliable.
Only after carrying out all the necessary additional studies and tests will the doctor be able to make a final diagnosis, which in most cases will be the reason for the increase in the level of antibodies to the thyroid protein.
Only after determining the exact cause of this condition can the most adequate treatment of the pathological process developing in the body be prescribed.
You should always remember that only a specialist can prescribe treatment, since self-medication can only worsen the situation.
If the main cause of the disorder in the normal function of the thyroid gland is eliminated, the level of antibodies will also return to normal.
To monitor the condition of the thyroid gland, you need to be tested for antibodies to thyroglobulin every six months. It is this indicator that will change at the slightest disruption in the work of this body.
Reasons for increasing AT to TG
The release of an increased amount of thyroglobulin into the blood causes pathologies or destruction of thyroid tissue, which can be triggered by diseases or external influences:
- autoimmune disorders;
- inflammatory, purulent processes;
- surgical intervention;
- diagnostic scintigraphy using iodine;
- iodine or ethanol therapy;
- biopsy;
- radiofrequency ablation;
- laser destruction.
A referral for diagnostics is given by an endocrinologist or other specialized specialist. Based on a separate analysis, it is impossible to make a complete conclusion about the disease.
It is considered in conjunction with other indicators and the patient’s medical history.
Diseases in which the level of AT TG changes significantly:
- benign and malignant neoplasms of the thyroid gland;
- follicular or papillary carcinoma;
- relapses after treatment of neoplasms and carcinomas;
- autoimmune thyroiditis (Hashimoto's disease);
- diabetes;
- idiopathic myxedema;
- adenoma of glandular tissue;
- multinodular or endemic goiter;
- diffuse toxic goiter (Graves disease);
- hyperthyroidism.
The test is used to monitor the condition of patients who have undergone surgery (removal of the thyroid gland, tumors), radical thyroidectomy, or radioactive iodine therapy. An increase in the number of antibodies is one of the signs of cancer relapse.
Important information! To establish an accurate diagnosis, one analysis is not enough. Its results are taken into account together with other indicators.
A surge in the number of antibodies is mistakenly called a cancer marker, but the imbalance can be caused by reasons not related to neoplasms.
Diagnostics and tests
It should be noted that many patients are wary of antibody tests. But do not be afraid of the purpose of this analysis. It can be prescribed not only for suspected cancer. Thyroid dysfunction can also occur for other reasons.
Testing for antibodies to TG is often prescribed for diseases of an autoimmune nature, i.e. for disorders of the human immune system. In such diseases, the body perceives its own tissues as foreign, resulting in their damage. An antibody test allows you to identify serious pathologies at the initial stage of their development.
Similar situations arise in the following violations:
- When controlling the processes occurring in the thyroid gland.
- For systematic pathologies of an autoimmune nature.
- If any violations are detected after injuries.
- In case of disruption of the reproductive system in women.
- To monitor the behavior of the body after surgical interventions.
Often, a test for antibodies to thyroglobulin is prescribed based on the patient’s verbal complaints.
Such complaints may include:
- Apathetic mood.
- Fatigue and weakness.
- Increase in neck volume.
- The appearance of rashes on the skin, its dryness.
- Noticeable bulging of the eyes.
- Insomnia.
- Increased irritability and anxiety.
- Memory problems.
- Cycle disturbances, miscarriages, infertility in women.
- Decrease/increase in body weight from normal.
Frequently, antibodies to thyroglobulin should be tested for the following diseases or suspicion of them:
- Tumor diseases or diseases of an oncological nature,
- Down syndrome disease,
- Thyroid diseases
- Hemolytic anemia,
- Hashimoto's thyroiditis,
- Diffuse or toxic goiter.
What are the rules for donating blood for analysis to detect antibodies to thyroglobulin?
To obtain a more accurate and reliable analysis result, a number of conditions must be met.
- Blood for analysis must be taken from the ulnar vein.
- Blood sampling must be done before 11 o'clock in the afternoon, i.e. in the first half of the day, since it is at this time that hormone levels peak.
- Blood must be donated on an empty stomach; only clean drinking water can be consumed.
- Smoking is strictly prohibited several hours before the test (including the use of nicotine substitutes).
- About a day before the analysis, physical activity and psychological stress should be excluded, i.e. it is necessary to ensure the patient's rest. Half an hour before the analysis should be spent in absolute peace.
- It is necessary to interrupt treatment if it is in progress. You should also temporarily stop taking certain medications that may distort the test result.
- The analysis should be carried out separately from other studies. It is not advisable to undergo ultrasound, MRI and other examinations on this day.
The test should be postponed for some time if the patient has recently suffered from an infectious disease with an increase in body temperature.
Also, if minor deviations from the norm are detected, the analysis should be repeated after 7-10 days in order to compile a complete and correct picture of the pathology and its origin.
Preparing and conducting analysis
To carry out the analysis, you need to donate blood from a vein. Most often, antigens are determined by solid-phase chemiluminescent enzyme-linked immunosorbent assay (“sandwich” method).
Antibodies to thyroglobulin can be elevated if you do not properly prepare for a thyroid hormone test.
The sample to be analyzed is placed in the wells of the plate on which the fixed antigen is located. After adding special reagents, the optical density of the sample is measured and the results are interpreted. The unit of measurement for this parameter is IU/ml (international unit per milliliter).
Preparation for analysis is as follows:
- one day before the collection of biomaterial, it is recommended to avoid heavy physical activity and stress;
- the test is carried out on an empty stomach, so you cannot eat for breakfast, you can only drink still water;
- The analysis is carried out in the morning, before 11-00, when the level of hormones reaches its peak;
- 2-3 hours before visiting the laboratory you must refrain from smoking.
The blood sampling procedure is carried out in the following order:
- The nurse checks the patient’s personal data in the direction issued by the doctor and makes an entry in the registration journal.
- The patient is seated in front of the laboratory assistant's table (in some cases, blood sampling can be done in a lying position).
- An elastic tourniquet is applied above the vein puncture site.
- The puncture area is treated with a disinfectant composition.
- A vein is punctured and blood is collected into a test tube, the tourniquet is loosened.
- A special reagent is introduced into the test tube with the biomaterial, closed and placed in a stand.
- The needle is removed from the vein and the puncture site is pressed with a disposable napkin soaked in a disinfectant solution (alcohol).
Interpretation of results
The patient's blood serum is used for diagnosis. Specific solutions containing antigens are added to it. The formation of antigen-antibody complexes occurs (particles of solution and antibodies bind). Special luminescent particles are added to the complexes, which tend to glow when viewed under a photomultiplier tube. The indicators are calculated.
The answers are deciphered not by laboratory workers, but by the patient’s attending physician who ordered the analysis. Trying to interpret indicators on your own can lead to unnecessary worry and misinterpretation of the data. The subject receives a response the very next day.
There are several options for test results for antibodies to TSH receptors in women and men (indicators in IU/l):
- up to 1.5 – negative result, normal;
- 1.5-1.75 – intermediate result, antibodies are increased, but are within acceptable limits, requires additional research;
- above 1.75 – positive analysis response.
An antibody titer above 10 IU/l indicates a severe prognosis and unfavorable course of the disease. Indicators that reach 40 IU/l indicate that the patient may not expect the development of remission in the near future.
A decrease in indicators by less than 2 times during six-month therapy is evidence that the achieved remission will be short-lived.
There are cases of false negative test results. This means that the person is being treated with drugs that show a normal level of antibodies at the time of blood sampling or the patient was incorrectly prepared for the procedure.
Decoding the results
The analysis results are interpreted taking into account the reference values indicated above. Factors that can change the AT-TG value are listed in the table below.
| Result | Factors |
| False positive |
|
| False negative |
|
What is thyroglobulin?
What is thyroglobulin? This is one of the variants of globulins that are present in the body.
Thyroglobulin is a protein iodine-containing biologically active compound that reflects the presence of thyroid cells in the human body.
It is produced and accumulates exclusively in the follicular cells of the thyroid gland. The main thyroid hormones, T4 (thyroxine) and T3 (triiodothyronine), are formed from thyroglobulin.
The TG concentration in the blood is directly dependent on the mass of the gland and therefore can be considered a reliable indicator of its condition.
When the blood test for TSH is higher than normal, then with a high degree of probability it is possible to suspect the occurrence of tumor processes in the thyroid gland or its inflammation.
Important! The iodine-containing protein thyroglobulin is not a tumor marker for the unremoved thyroid gland. However, its inflated indicators may indicate an increased risk of oncological processes in the organ.
Thyroglobulin can be considered a tumor marker only if its concentrations are studied after removal of the thyroid gland.
If the thyroid gland is removed, such a blood test is required approximately once every 4 months. This allows you to diagnose a possible relapse at an early stage.
And in the presence of thyroid gland, a blood TG test to determine the primary tumor is meaningless.
Treatment
If indicators deviate from the norm, specific therapeutic regimens are not used. The presence of antibodies to thyroglobulin is a symptom of a particular pathology that needs to be identified and eliminated. Hormonal drugs in most cases do not reduce the number of immune cells. The same applies to plasmapheresis and hemosorption.
Treatment should be aimed at reducing the severity of autoimmune aggression; in this case, cytostatics and immunosuppressants become the most effective. Sometimes the only treatment is surgery - resection or removal of the thyroid gland.
How is the amount of antibodies determined?
The analysis is carried out using the enzyme immunoassay method for examining blood serum.
To do this, take venous blood in the morning, on an empty stomach. It is taken into a test tube with a gel containing a coagulation activator. The tube is centrifuged to separate the serum from the formed elements and fibrin.
The results are interpreted by a clinical laboratory diagnostics physician, and deciphered by the attending endocrinologist.
The study requires careful preparation to exclude false positive results. Therefore, before analysis you should:
- avoid fatty, spicy foods, alcohol and smoking,
- limit physical activity,
- stop taking medications two weeks before the test, hormonal medications - a month,
- in the morning do not have breakfast, do not drink tea, coffee, only water is allowed,
- it is better to take it in the first half of the day, since the indicators fluctuate throughout the day,
- eliminate stress and anxiety.
It is better not to get tested if you have recently had an infection with an increase in body temperature.
Watch a video on this topic
Thyroglobulin norm
The thyroglobulin level varies from 1.5 to 59 ng/ml. Such a large difference in rates depends on many factors, and each person may have different numbers. It all depends on the size of the thyroid gland and what the body’s need for this protein is. So, for example, if an operation was performed to completely remove an organ, then this protein is practically absent in the blood. The reason for this is that TG can only be produced by the thyroid gland, as well as cancer cells. It is impossible to judge the presence of thyroid dysfunction by the amount of TG only from a single analysis. Most often it is studied in dynamics. If the level exceeds 50 ng/ml for a certain time, experts can reliably speak about thyroid dysfunction.
Causes of changes in thyroid-stimulating hormone
Thyroid-stimulating hormone is produced by the anterior lobe of the pituitary gland and regulates the functioning of the gland. If not enough thyroid hormones enter the blood, the pituitary gland produces more TSH, increasing the production of thyroxine.
What the indicator says:
- a normal amount of thyroid-stimulating hormone indicates stable functioning of the pituitary gland;
- elevated TSH is a sign of a lack of thyroid hormones, which indicates primary hypothyroidism;
- TSH below normal indicates hyperactivity of the gland, in this situation hyperthyroidism is diagnosed.
TSH during pregnancy drops below normal in the first trimester. If a woman did not have pathologies in the thyroid gland before pregnancy, the process of decreasing thyroid-stimulating hormone in the first trimester (especially in multiple pregnancies) is the norm and does not require treatment.
Drug therapy
As a rule, if a high level of the hormone thyroglobulin is detected, drug therapy is not prescribed, since a complete examination of the thyroid gland should be performed before choosing treatment.
If there is a lack of thyroglobulin in the body, doctors prescribe hormone-containing drugs such as:
- Tiretoma,
- Thyroxine,
- Thyreokomba.
If patients have a disturbance in the functioning of the thyroid gland, then such drugs are prescribed, as a rule, for life.
It is worth noting that such drugs are only replenishers of hormone deficiency, and the very cause of inflammation of the thyroid gland should be treated with preventive or surgical methods, after which medications are prescribed.
Norm of total and free thyroid hormones (table)
| Study | Norm for women | Unit |
| TSH | 0,4-4,0 | honey/l |
| T3 general | 0,8-2,0 | ng/ml |
| T3 free | 2,5-4,3 | ng/ml |
| T4 general | 5,1-14,1 | ng/dl |
| T4 free | 0,93-1,7 | ng/dl |
| AT-TPO | < 5,6 | U/ml |
| AT-TG | 0-18 | U/ml |
What can affect the results of the analysis?
It is worth remembering that the hormone thyroglobulin will only be present in the blood if your thyroid gland is in place. If the operation to remove the thyroid gland is successful, this hormone is practically not detected, since it is not produced.
If you have been prescribed thyroglobulin control without first examining the thyroid gland, then an increased level of the hormone may indicate the presence of a thyroid tumor or its extreme enlargement. In this case, you should immediately contact an endocrinologist to establish all the details of the condition of the organ.
How can elevated levels be dangerous?
An analysis for an increased amount of antibodies to thyroglobulin is used in the early stages of any disease, when other methods are powerless. If antibodies to thyroglobulin exceed the norm, this may mean the presence of certain pathological diseases occurring in the body.
These include:
- inflammation of the thyroid gland;
- malignant thyroid tumors;
- benign adenomas;
- the body's reaction to damage to the thyroid gland;
- decreased production of thyroid hormones;
- chronic thyroiditis.
Quite often, pernicious anemia, thyroid surgery, or some genetic disease contributes to an increase in antibodies.
In addition, a woman's age may be a potential reason for the increase in the rate. Men suffer from this pathology much less frequently than women. You should also take into account recent illnesses or treatment of a disease that has not been completed.
What can influence the indicator
The level of autoantibodies to thyroglobulin is affected by taking oral contraceptives . These drugs significantly increase the level of ATTG in the blood. Previous infections can have the same effect, so it is recommended to donate blood 7-10 days after complete recovery.
Physical activity and severe stress on the eve of blood sampling are one of the reasons for a false increase in the level of AT to TG. But such an overestimation is usually insignificant.
When interpreting the results, it is important to take into account hormonal levels. In 10% of healthy women during menopause, antibodies to thyroglobulin are elevated.
Is thyroglobulin an indicator of cancer?
As described above, thyroglobulin as an indicator of the functioning of the thyroid gland can go beyond its normal range due to various factors. Accordingly, it is necessary to study all available information and not panic prematurely.
If thyroglobulin is very elevated, what does this mean?
- If, at the same time, other studies of the thyroid gland did not show any special abnormalities, most likely the body has suffered stress or another disease is developing that is in no way related to the cancer.
- Of course, it is the thyroglobulin level that is the main indicator of the possibility of developing thyroid cancer, but this does not mean at all that you have it. Before drawing any conclusions, you should undergo a full examination and consult with your doctor.
- If the thyroid gland has been removed, then the hormone, in principle, should not increase, which means that its elevated value may be false and the analysis should be repeated.
Read about the causes and consequences of elevated TSH hormone in women here.