Literally, the name of this enzyme-linked immunosorbent test can be translated as follows: complete, or total (total) antibodies (anti) to the human hepatitis C virus (human C virus, HCV). Currently, this test is a screening test. This means that it is taken from a wide range of populations and is the first type of laboratory test to diagnose hepatitis C, allowing the diagnosis of the disease in its acute or chronic form.
How to interpret these tests, and what can be learned from a positive and negative result? Simple logic dictates that if HCV is positive, then the person is infected with the hepatitis C virus, and if the test is negative, then this person is healthy, and you can “breathe easy.” This is true in most cases, but in reality everything is far from so simple. Surprisingly, in the case of a positive result, a person can be healthy, and in the case of a negative result, a person can be sick. How is this possible? Let's figure out what confirms this or that result.
What exactly is anti-HCV total?
First of all, this is a laboratory indicator confirming that specific antibodies are found in human blood plasma, which are produced in the body to the virus. This indicator is general, that is, based on it, it is impossible to say which class of antibodies or immunoglobulins (they are different) led to a positive result.
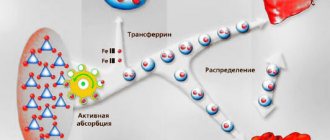
It is known that during infectious diseases, including viral hepatitis, antibodies of classes M and G are produced. Some of them are rapid response antibodies (M), and appear in the acute form of the disease, when the body first encounters the virus, but compounds class G are “long-lasting” and remain in the blood plasma for a long time after the infectious process has either ended or continues in a chronic form.
Rapid response antibodies (M) appear in the blood within a month after infection, and their titer, or concentration, increases quite quickly. After about six months, their concentration gradually decreases in the blood plasma, and they are activated again only if the infection worsens again during a chronic course. This process is called reactivation.
But antibodies of the slow type, class G, appear much later, 3 months after infection. Their maximum concentration in the blood plasma is indicated six months after the virus enters the body, and then remains constant throughout the illness, as well as during the period of convalescence, that is, recovery and the subsequent period. Therefore, this analysis - the total level of antibodies - has diagnostic value only within 4-5 weeks from the beginning of the suspected infection. Currently, new generation test systems are being introduced into laboratory practice, which make it possible to determine the level of antibodies much earlier, already 10-15 days after infection, and compete in this with the best method, or PCR.
Now let’s consider what results can be obtained after receiving the results of this analysis, without even looking at the symptoms and without asking the patient anything, especially since in most cases this viral hepatitis does not manifest itself in any way, and only after 20 years it transforms into liver cancer, or hepatocellular carcinoma. That is why this disease is called the “gentle killer.”
Who needs to get tested?
People at risk for hepatitis C include residents of disadvantaged countries, drug addicts, employees of the medical industry, and people with promiscuous sex.
Traveling to a country with a high incidence rate and being with an infected person requires careful prevention and testing. This type of infectious hepatitis is characterized by incidence at a young age. The percentage of people infected with the virus increases every year. More than half of those infected with the hepatitis C virus are drug addicts who inject drugs.
Viral cells are found in blood, saliva, and semen. When the virus enters the body of a healthy person, it infects liver cells and leads to tissue destruction. A small amount of infection does not lead to infection - the body independently copes with the penetrated antigens. With a high concentration of the virus and weakened immunity, infection occurs.
Anti-HCV total analysis is prescribed:
- if you suspect hepatitis C;
- for sexual diseases;
- pregnant women and newborns if the mother is infected;
- drug addicts;
- persons with HIV;
- before operations and before blood transfusions;
- people working in beauty salons and medical institutions;
- in case of disturbances in the level of bilirubin in the blood.
Also, for hepatitis C, patients at different stages of treatment are prescribed this test. Anti-HCV analysis indicators help to adjust the initiated treatment course in case of a protracted nature of the disease.
The presence of Anti-HCV antibodies in the blood and previous hepatitis do not provide immunity to this disease. Secondary infection is possible even with a moderate concentration of antibodies in the body. A vaccine against this form of hepatitis has not been developed.
In some cases, the chronic form develops without severe symptoms. Prolonged development of the disease without the necessary treatment leads to significant damage to the liver and increases the likelihood of complications.
When the test is positive
It would seem that in this case everything is simple: if a person has antibodies to the hepatitis C virus, then this result indicates the presence of hepatitis and the patient must be sick. But sometimes there are false positive results. It is known that every laboratory test has both sensitivity and specificity. And each research result cannot be both highly sensitive and highly specific, since these are different “sides of the coin.”
If the method is highly sensitive, it may falsely react to foreign substances that generally have nothing to do with the research question. And if it is very highly specific, then the sensitivity may be low. This leads to the fact that the fairly highly sensitive enzyme immunoassay method sometimes produces errors. Therefore, if a patient has a positive HCV blood test for the first time, then according to the law, it is retaken in the same laboratory, but using a different method. And only if it is repeatedly positive is it considered truly positive. But what does it mean?
- The patient has hepatitis C. It is impossible to understand whether this process is acute or chronic, since we do not know whether the presence of which antibodies was detected: M or G,
- The patient is recovering from acute hepatitis C, and due to the “trail” of G antibodies, the result came out positive,
- The patient recovered from the acute illness a long time ago (this is also rare, but it does happen), and he also had G antibodies as a marker of a long-standing infection.
Naturally, with such a “diverse interpretation”, a confirmatory analysis is necessarily necessary. This can be PCR, which directly determines whether the virus is in the body or not. Finally, this may be a determination not of total antibodies, but of separate ones, by class. Thus, the detection of only class G antibodies will confirm whether the patient has a chronic form of the disease, or has had acute hepatitis, or is recovering. In any case, the presence of class G antibodies alone excludes the diagnosis of acute hepatitis, especially in the early period.
Interpretation of blood test results
Ideally, Anti-HCV decoding is carried out by a specialized specialist. But when taking a test in a private laboratory, the patient receives the results of treatment even before visiting the doctor. It’s a rare person who will be able to wait for a doctor’s consultation and not ask whether the indicators go beyond physiologically acceptable values.
Normally, Anti-HCV Total is negative, which means that no antibodies to the causative agent of hepatitis C are detected in the human blood.
The basic principles for interpreting various options for the results of a serological study are given in the table. The purpose of the test being performed is also indicated.
It is the basis for diagnosing hepatitis C.
Possible results:
- antibodies detected (indicating the titer) – with a high degree of probability the person is infected;
- antibodies were not detected - in most cases, the result indicates that the person is not infected with HCV or the test was taken within the “diagnostic window”
It can be performed both instead of Anti-HCV Total, and when total antibodies are detected.
Possible results:
- there are no immunoglobulins - the person is healthy (except for the possibility of false positive results);
- Anti-HCV IgG detected - a chronic form of hepatitis C or a previous disease:
- Anti-HCV IgM was detected - this type of immunoglobulin indicates an acute course of a viral infection
| Name of analysis | Possible result and description |
| Anti-HCV total (total) | |
| Differential analysis for antibodies to HCV | |
| HCV Ag At ELISA | The study is carried out to detect virus antigens (usually the nuclear core protein) or structural proteins (NS3, NS4, etc.). In routine clinical practice, the test is rarely prescribed. Analysis for the core antigen has been successfully replaced by faster and easier-to-perform PCR, and testing for antibodies to antigens of other structural proteins is advisable in complex cases when it is necessary to find out the cause of resistance, etc. But the detection of any of the listed antigens for hepatitis C is unambiguous a sign of infection |
Like any other test, ELISA tests for antibodies to HCV are associated with the risk of obtaining erroneous results.
In addition to a technical error in the analysis, false positive or negative data are possible when:
- pregnancy;
- autoimmune diseases (especially autoimmune hepatitis);
- leukemia and other types of oncology;
- HIV;
- previously suffered hepatitis C (both after antiviral therapy and during independent recovery, which is noted in 10–15% of cases of infection);
- severe systemic infections, when a large amount of antibodies are constantly released into the blood, which is the cause of error in the analysis;
- any conditions associated with serious immunodeficiency (including drug-induced).
Another reason for a false result is the so-called “diagnostic window”. This is the period from the moment of infection until the accumulation of antibodies in the human blood in the amount necessary for laboratory diagnosis. The time frame for detecting HCV by ELISA varies from person to person, but on average is 6–8 weeks.
Conducting a serological test is not practical for diagnosing pathology in a child born from a sick mother. If the probability of intrauterine and intrapartum transmission of the virus does not exceed 5–7% (the exception is women with HIV, their risk is about 20–25%), then IgG passes through the placenta and is found in the child’s blood. Therefore, in this case, testing for HCV is always carried out using PCR.
Considering the possibility of obtaining false results, doctors always prescribe a confirmatory test using a high-quality PCR method.
ELISA remains the main recommended method for rapid diagnosis of hepatitis C. This test is performed everywhere. But in order to avoid mistakes with the test results, it is better to consult a doctor for a more comprehensive examination (especially if the ELISA is negative against the background of deteriorating health).
Quite often we have to take biochemistry tests (from a vein) during a routine medical examination, before surgery or during pregnancy to identify any diseases or abnormalities of the body. As a rule, the most basic components of the study are HIV or hepatitis antibodies, which can be used to establish the fact of infection. Hepatitis C antibodies are called in medicine “Anti-HCV”, that is, “against hepatitis C” and are divided into two groups: “G” and “M”, which in test results are designated as “IgG” and “IgM”, where “Ig” ..." - immunoglobulin. Anti - HCV total - markers for which a test is carried out to detect hepatitis C diseases. Anti-hcv can be detected after 5 weeks of the incubation period in acute or chronic types of the disease. Anti-hcv total is most often determined in those who have had the disease “on their feet”. In this case, antibodies can be detected for 5-9 years after infection. A positive result of the anti-HCV test does not provide 100% grounds for making a diagnosis, since in an infectious disease - hepatitis C - which occurs in a chronic form, total virus antibodies with a reduced content of titers are detected.
It is worth noting that the presence of antibodies in the body does not prevent re-infection with HCV infection, nor does it provide any immunity.
The test for the detection of hepatitis C is carried out in the laboratory, on an empty stomach (at least 8 hours before meals) and is examined within 1-2 working days.
The most common reasons for prescribing such an analysis are:
- cholestasis;
- pregnancy;
- donation;
- drug addiction (intravenous drug use);
- prerequisites for infectious hepatitis;
- upcoming surgery;
- detection of STIs;
- a sharp increase in ALT and AST levels.
There are antibodies that belong to certain hepatitis C proteins - the anti-HCV spectrum and determine the degree of viral load, the type of infection and the affected area. Anti-HCV are created from non-structural, for example, NS5, and structural (core) proteins (proteins).
Antibodies of class “G” - “IgG” belong to nuclear proteins and are detected 10-12 weeks after infection. The highest rate is observed six months after the onset of the disease. In the chronic form of the virus, such bodies are determined throughout life. If a person suffered this disease “on his feet,” then the “G” titer will decrease.
What if the test is negative?
We concluded that if a patient has a condition in which antibodies to HCV are positive, then the result can be, to put it mildly, ambiguous. And if anti-HCV total is negative, what does this mean?
In this case, we again have to choose from three possible answer options:
- The patient does not have hepatitis C. Most likely, he never had it, and the patient is absolutely healthy,
- the patient may also be sick and became infected only recently. He is in the first month of his illness, even the first weeks, and the antibodies have not yet had time to develop in the human body in such quantities that this technique can “feel”,
- Finally, viral hepatitis C can occur, but only in the seronegative form. This is a special type of disease in which antibodies practically do not appear in the peripheral blood, or appear in significant concentrations that it is impossible to detect them and interpret them. This type of course occurs in 5% of cases, or in every 20 patients. Agree that this is a fairly high probability of missing the diagnosis using only this one method.
HCV RNA test
HCV (viral hepatitis C) is an RNA infection from the group
"Flaviviridae", which gives rise to the liver. Testing for the presence of the virus is carried out using real-time polymerase chain response (RT-PCR), determining the presence of hepatitis C genetic material (RNA) in the body and its viral load on the body. The linear concentration criterion, in which the sum of pathogens is calculated, should be equal to 7.5x102 - 1.0x108 copies/ml.
A quantitative method for analyzing HCV RNA detects infection in 1 ml of blood, which includes:
- chain reaction (PCR and RT-PCR) in reality;
- branched DNA - that is, R-DNA;
- TMA—transcriptional amplification.
If the concentration of infection is less than 8x105 IU/ml, then the prognosis for treatment is favorable, in which you can completely get rid of the disease, and, in the minimum possible, place it in a state of remission.
What to do?
Precisely because this inexpensive method allows only to hint to the patient that he may have “problems” with viral hepatitis C, it is a screening method, exactly the same as determining the HBs antigen when testing for viral hepatitis B.
No infectious disease doctor will be able to make a diagnosis based solely on deciphering the test results. PCR is required, as well as separate determination of immunoglobulins by class. But even this full-fledged type of diagnosis, which allows one to determine the presence of a virus in the body and make an accurate diagnosis, still cannot say anything about whether the patient will develop liver cancer after many years or not. Comprehensive diagnostics with determination of prognosis is only possible with all biochemical tests, ultrasound results, and liver biopsy.
ALT, AST - blood test
A biochemical blood test allows doctors to detect the presence of serious diseases and infections in the human body. AST is an enzyme that catalyzes the conversion of oxaloacetate to aspartame. In addition to AST, biochemical analyzes include indicators of ALT - alanine aminotransferase, which is a protein catalyst in the metabolism of amino acids (a cell-based enzyme).
If the content of ALT and AST in the blood is too high, then this indicates painful human ailments, for example, cirrhosis of the liver, hepatitis. The more complex the course of the disease, the higher the enzyme level will be. If, nevertheless, the ALT and AST indicators are underestimated, then this indicates a lack of vitamin B6 or necrosis (ALT is underestimated, AST is increased).
With timely medical care and therapeutic procedures, AST returns to normal within a month after the rehabilitation course of treatment. In order for ALT and AST levels to always be normal, it is necessary to exclude long-term use of any medications that destroy liver tissue or disrupt the general functionality of a vital organ. If this is not possible due to, for example, chronic hepatitis, then AST and ALT analysis should be carried out frequently and periodically for the timely detection of abnormalities caused by drug intoxication or the appearance of a chronic form of the disease.
It is also necessary to remember that during the period of elevated enzyme levels, the liver is weakened and should not be exposed to any risk. Therefore, WHO recommends herbal-based drugs such as: “Karsil”, “Essentiale N”, “Tykveol”, which have a positive effect on the liver and take on part of its functions: participation in metabolism and disinfection - destruction of toxins.
But under no circumstances should you self-medicate. If you find any signs of hepatitis in yourself, or see the words “Detected” in the test results, immediately consult a doctor for a comprehensive examination and an accurate diagnosis. The sooner you do this, the better it will be for you. You can’t joke with your health!
At-risk groups
The risk group is numerous:
- doctors and nurses who perform blood collection, transfusions, and surgeries;
- drug addicts, prostitutes, homosexuals;
- patients who need donor blood;
- patients with irreversible kidney damage;
- people who have promiscuous sex.
Blood with the HCV virus can be transmitted through promiscuity, infected syringes, during childbirth, and poorly treated instruments in salons and hospitals. The pathogen is not transmitted in everyday life with dishes, during breastfeeding, or through the air.
Treatment regimens for hepatovirus
If there is no doubt about the presence of a diagnosis such as HCV, the patient is prescribed a specific treatment regimen, which depends on the following factors:
- Age of the patient (for example, antiviral drugs are not recommended for children under 12 years of age);
- The general condition of the patient’s body, the presence of other chronic diseases;
- Course of the disease, presence of complications.
Until recently, only one treatment regimen for hepatovirus was used - Ribavirin in combination with Interferon-alpha. This method has many disadvantages, including many serious side effects and poor effectiveness. In addition, due to the duration of therapy, renal failure may occur, and the combination of drugs itself negatively affects blood biochemistry. If the white blood cell count rises sharply, treatment should be stopped.
The Interferon Ribavirin regimen is significantly outdated and is used only in cases where treatment with other drugs is not allowed. Most often, when treating a viral disease of this type, innovative antiviral drugs made in India are used based on the original American formulation.
Modern antiviral treatment regimens necessarily contain Sofosbuvir, an inhibitor of viral RNA polymerase, and a substance that inhibits the pathogenic NS5A protein, depending on the HCV genotype:
- Ledipasvir – for hepatovirus genotypes 1, 4, 5 and 6;
- Daclatasvir - used for genotypes 1, 2, 3 and 4. Most effective in gen 3 therapy;
- Velpatasvir is a universal substance that is used in the treatment of absolutely all genotypes of the pathogen.
The course of treatment depends on the severity of the disease. If the course of the disease is standard, the therapeutic course lasts no more than 12 weeks. For repeated therapy, as well as in the presence of severe complications, a 24-week therapeutic regimen may be prescribed. In this case, Ribavirin and various hepatoprotectors can be added to the main medications.
Why might the result be wrong?
An indeterminate result of an enzyme immunoassay is the presence in the biomaterial of a small amount of antibodies to the pathogen, in which it is impossible to refute or confirm infection. Doubtful data guides the hepatologist to further monitor the patient.
https://www.youtube.com/watch?v=https:accounts.google.comServiceLogin
Reasons for an indeterminate anti-HVC test result:
- early stage of hepatitis;
- insufficient sensitivity of the test system;
- non-compliance with the rules for collecting biomaterial.
Medical literature data on the presence of genetic material in the blood with weakly positive ELISA are contradictory. Additional tests are performed to confirm infection.
It is possible to obtain false-positive ELISA results for rheumatoid factor in the blood of patients suffering from systemic lupus erythematosus, Sjogren's syndrome, rheumatoid arthritis or parasitic infections.
The HCV test may be incorrect. This is possible if:
- the studies were carried out in different laboratory conditions;
- contaminated materials were used: biological materials were not sterile;
- improper storage of the test sample;
- incorrect processing.