From the article you will learn what a leukocyte blood formula is and a breakdown of test indicators in adults and children. What deviations mean and how to prepare for analysis.
Thanks to blood tests, the doctor can learn a lot of useful and important information about the health status of the patient being examined. The study of an indicator called the leukocyte formula is carried out in order to determine the type of disease, the nature of its course, the development of complications and the establishment of preliminary prognoses of the disease.
What is the leukocyte formula?
The leukocyte formula is an important indicator of the numerical ratio of all types of leukocytes, calculated as a percentage based on examination of a stained smear. The leukoformula is part of the common CBC analysis. It is determined in peripheral blood samples in several ways:
- Microscopy of blood from a finger - counting is done manually using microscopic examination.
- Studying blood from a vein - counting using automated methods.
Leukocytes, due to differences in cell size, have a specific location in the material under study: neutrophils, basophils and eosinophils are located at the edges, and lymphocytes with monocytes are in the central part of the smear.
Definition, general information
White blood cells, like other blood cells, are formed in the bone marrow. Their main function is to fight infection and respond to tissue damage.
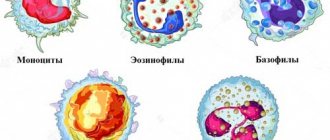
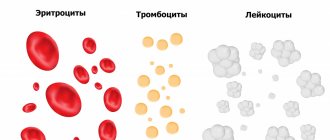
Unlike red blood cells, whose population is homogeneous, white blood cells have five types that differ in their functions and appearance: basophils, neutrophils, eosinophils, monocytes and lymphocytes.
White blood cells are formed from stem cells in the brain of the head. They do not live long, so they are constantly updated. White blood cell production in the bone marrow increases in response to any tissue damage, as part of the normal inflammatory response. Different types of leukocytes have their own functions, but they can coordinately interact by contacting the use of certain components - cytokines.
For a long time, manual calculation of the leukocyte formula was carried out.
Types of leukocytes in a leukogram
- Eosinophils are detected in allergies, parasitic infestations, infectious and autoimmune diseases, as well as in cancer.
- Neutrophils help fight acute infections by destroying the cell membranes of pathogenic microorganisms and their further phagocytosis (capture and destruction of foreign cells). They are divided into:
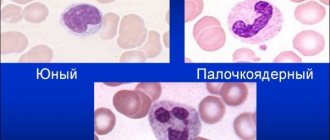
- Myelocytes (nascent) and metamyelocytes (young) cells - these should not be present in normal samples. They appear only in cases of severe infectious pathologies or blood diseases, accompanied by inhibition of the hematopoietic function of the bone marrow.
- Band neutrophils (young) - their number begins to increase during bacterial infections, when segmented neutrophils cannot cope with their task.
- Segmented cells (mature) are quantitatively superior to others. Needed for normal functioning of the immune system.
- Lymphocytes are a kind of cleaners: they find, identify and destroy antigens, and also promote additional production of antibodies by the body to ensure immune memory (remembering and quickly recognizing foreign agents).
- Monocytes - their main task is to absorb and process dead cells, bacterial, viral, etc. agents, atypical cells, fragments of own phagocytes, etc.
- Basophils - the exact functionality of these cells has not been reliably studied. It is known that they regulate allergic reactions and blood clotting processes. They are activated when a focus of inflammation occurs.
Plasma cells (plasmocytes) are necessary for the production of antibodies. Normally, they are allowed in the analysis in children, but they should not be present in adults. Plasmocytes appear only during acute pathology.
Leukocyte blood count: normal indicators and decoding of the leukogram in children and adults + video
Blood indicators characterize a person’s health status and can greatly facilitate diagnosis. By determining the leukocyte formula, one can guess the type of disease, judge its course, the presence of complications, and even predict its outcome. And deciphering the leukogram will help you understand the changes occurring in the body.
What does the leukocyte blood count show?
The leukocyte formula reflects the percentage of the five main types of leukocytes
The leukocyte formula of blood is the ratio of different types of leukocytes, usually expressed as a percentage. The study is carried out as part of a general blood test.
Leukocytes are white blood cells that represent the body's immune system. Their main functions are:
- protection against microorganisms that can cause health problems;
- participation in processes that occur in the body under the influence of various pathogenic factors and causing disturbances in normal functioning (various diseases, exposure to harmful substances, stress).
The following types of leukocytes are distinguished:
- Eosinophils. They appear in allergic, parasitic, infectious, autoimmune and oncological diseases.
- Neutrophils. Protects against infections and can destroy viruses and bacteria. Classified into:
- myelocytes (nascent) and metamyelocytes (young - derived from myelocytes) - are absent in the blood of a healthy person, they are formed only in extreme cases, in the most severe diseases;
- stab neutrophils (young) - their number increases in bacterial diseases if segmented neutrophils cannot cope with the infection;
- segmented (mature) - presented in the largest quantities, provide immune protection of the body in a healthy state.
- Lymphocytes. They are a kind of cleaners: they are able to detect, recognize and destroy antigens, and also take part in the synthesis of antibodies (compounds that can stimulate lymphoid cells, forming and regulating the body’s immune response), and provide immune memory.
- Monocytes. Their main task is to absorb and digest dead (dying or remains of destroyed) cells, bacteria and other foreign particles.
- Basophils. The functions of these cells are not fully understood. It is known that they take part in allergic reactions, in blood clotting processes, and are activated during inflammation.
Interpretation of LYM (lymphocyte) indicators in a blood test: https://krasnayakrov.ru/analizy-krovi/rasshifroa-lym-v-analize-krovi-norma.html
Plasma cells (plasmocytes) participate in the formation of antibodies and are normally present in very low quantities only in the blood of children; in adults they are absent and can appear only in the case of pathologies.
The study of the qualitative and quantitative characteristics of leukocytes can help in making a diagnosis, since with any changes in the body, the percentage of some types of blood cells increases or decreases due to an increase or decrease to one degree or another in others.
The doctor prescribes this test in order to:
- get an idea of the severity of the patient’s condition, judge the course of the disease or pathological process, find out about the presence of complications;
- establish the cause of the disease;
- evaluate the effectiveness of the prescribed treatment;
- predict the outcome of the disease;
- in some cases, to evaluate the clinical diagnosis.
To calculate the leukocyte formula, certain manipulations are performed on a blood smear, dried, treated with special dyes and examined under a microscope. The laboratory technician marks those blood cells that fall into his field of vision, and does this until a total of 100 (sometimes 200) cells are collected.
Leukocyte counting is carried out visually by a laboratory assistant using a microscope.
The distribution of leukocytes over the surface of the smear is uneven: the heavier ones (eosinophils, basophils and monocytes) are located closer to the edges, and the lighter ones (lymphocytes) are closer to the center.
When calculating, 2 methods can be used:
- Schilling method. It consists of determining the number of leukocytes in four areas of the smear.
- Filipchenko's method. In this case, the smear is mentally divided into 3 parts and counted along a straight transverse line from one edge to the other.
The quantity is noted on a piece of paper in the appropriate columns. After this, each type of leukocyte is counted - how many of which cells were found.
It should be borne in mind that counting cells in a blood smear when determining the leukocyte formula is a very inaccurate method, since there are many difficult to eliminate factors that introduce error: errors in drawing blood, preparing and staining the smear, human subjectivity in interpreting cells. The peculiarity of some types of cells (monocytes, basophils, eosinophils) is that they are distributed unevenly in the smear.
If necessary, leukocyte indices are calculated, which are the ratio of various forms of leukocytes contained in the patient’s blood; sometimes the ESR indicator (erythrocyte sedimentation rate) is also used in the formula.
Leukocyte indices show the degree of intoxication and characterize the state of the body's adaptive potential - the ability to adapt to the effects of toxic factors and cope with them. They also allow:
- obtain information about the patient’s condition;
- assess the functioning of the human immune system;
- study the body's resistance;
- find out the level of immunological reactivity (the development of immunological reactions by the body in response to exposure to parasites or antigenic substances) when various organs are affected.
The norms of the leukocyte formula depend on the age of the person. In women, the difference is also that the indicators can change during ovulation, after or during menstruation, during pregnancy, after childbirth. That is why in cases of deviations you should consult a gynecologist.
If there are deviations in the leukocyte formula in pregnant women, consultation with a gynecologist is necessary.
Possible deviations from the norm in the leukogram
An increase or decrease in the level of certain types of leukocytes indicates pathological changes occurring in the body.
Leukocyte formula shift
In medicine, there are concepts of a shift in the leukocyte formula, indicating deviations in the health status of patients.
A shift in the leukocyte formula indicates abnormalities in the human body
Shift of leukocyte formula left and right - table
To obtain data on the patient's condition, based on the results of the leukocyte formula, the shift index is taken into account. It is determined by the formula: IS = M (myelocytes) + MM (metamyelocytes) + P (band neutrophils)/C (segmented neutrophils). The norm for the leukocyte formula shift index in an adult is 0.06.
In some cases, there may be a phenomenon such as a significant content of young cells in the blood - metamyelocytes, myelocytes, promyelocytes, myeloblasts, erythroblasts. This usually indicates diseases of a tumor nature, oncology and metastasis (formation of secondary tumor foci).
Cross leukocyte formula
Leukocyte crossover is a concept that arises when analyzing a child’s blood.
If in an adult, changes in the blood are caused by diseases or significant exposure to harmful factors on the body, then in young children, changes occur due to the formation of the immune system.
This phenomenon is not a pathology, but is considered absolutely normal. The non-standard nature of the numbers is determined only by the development of immunity.
The phenomenon of leukocyte crossover is due to the formation of the immune system in children
The first cross-section of the leukocyte formula usually occurs towards the end of the first week of a baby’s life. At this time, the number of neutrophils and lymphocytes in the blood equalizes (they become approximately 45%), after which the number of lymphocytes continues to increase, and the number of neutrophils decreases. This is considered a normal physiological process.
The second cross-section of the leukocyte formula occurs at 5–6 years of age, and only by the age of ten do blood counts approach the normal level of an adult.
According to a number of medical authors, at present, children have an earlier crossover in the leukocyte formula, a tendency to eosinophilia, relative neutropenia and an increase in the number of lymphocytes.
The leukocyte formula can provide many answers to difficulties in diagnosing the disease and prescribing therapy, as well as characterize the patient’s condition. However, it is better to entrust the interpretation of the blood test to an experienced specialist. The doctor can give detailed explanations and adjust the treatment.
- Anatoly Kupriyanov
Source: https://krasnayakrov.ru/analizy-krovi/o-chyom-mozhet-rasskazat-leykotsitarnaya-formula.html
What does the leukocyte formula indicate?
This analysis is informative in diagnosing:
- Viral and bacterial infections (allows for differential diagnosis).
- Parasitic infestations.
- Diseases of allergic origin.
- Malignant neoplasms and leukemia (as an additional method of primary diagnosis).
- State of the patient's immune system.
Decoding the leukocyte blood formula in adults
When assessing a blood test for the leukocyte formula in an adult patient, specialists check certain indicators and their compliance with normal values.
The norm for deciphering the leukoformula in an adult is presented in the table:
| Index | Normal value | |
| % | X 109/l | |
| Band neutrophils | 1-6 | 0,04-0,3 |
| Segmented neutrophils | 45-72 | 2,0-5,5 |
| Eosinophils | 0,5-5 | 0,02-0,3 |
| Basophils | 0-1 | 0-0,065 |
| Monocytes | 3-11 | 0,09-0,6 |
| Lymphocytes | 19-37 | 1,2-3,0 |
Any recorded deviation from normal values is a reason for a more thorough examination. All results obtained are evaluated together with medical history, clinical symptoms, patient complaints and the results of other tests.
Decoding the leukocyte blood formula in children
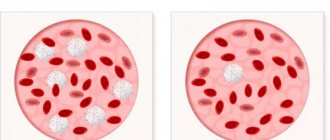
There are constant changes in a child’s tests, depending on the growth and development of the body, so the normal blood count in children will depend on age. Immediately after birth, neutrophils predominate in the baby’s tests (approximately 65-70% of the total number of cells). Lymphocytes account for 25-30%.
During the first five days, the level of lymphocytes increases and neutrophils decrease. On day 5, the first physiological crossover is observed - the level of lymphocytes reaches 50-60%, and neutrophils - from 35 to 47%.
Closer to one month of age, the child’s body produces more lymphocytes than neutrophils, creating a strong immune system to resist bacteria. In the entire leukocyte mass, lymphocytes themselves account for up to 65%, and neutrophils account for about 15-20%. This blood leukoformula in children provides a 1-year-old baby with a strong immune system, which is important for the period of active development.
After the first year, when the immune system is already fully formed, the amount of lymphocyte mass gradually decreases.
By the age of four, another crossover occurs, during which lymphocytes are again compared with neutrophils, forming a barrier to the penetration of pathogenic microorganisms. After it, the number of neutrophils continues to increase, and lymphocytes decrease.
Closer to the sixth year, deciphering the leukocyte formula of a child’s blood increasingly resembles the analysis of an adult, in which the bulk falls on neutrophils and lymphocytes.
NEUT - decreased, LYM - increased
The reasons for a decrease in neutrophils and an increase in lymphocytes in a general blood test can be physiological and pathological. Let us consider in more detail the possible reasons for the simultaneous development of neutropenia and lymphocytosis.
Physiological reasons
The immune system of children is still preparing for birth in utero - the total number of all types of leukocytes increases. At the same time, their percentage approximately corresponds to adults and teenage children.
From the first day after birth until 2 weeks of age, neutrophils begin to decline rapidly in a newborn baby.
At the age of 1-12 months, their level is minimal - only 17-30%. Neutrophils continue to be reduced until the end of the child's first year of life. Then gradual growth begins.
Lymphocytes, against the background of a decrease in neutrophils, are increased. This is not an absolute increase, because... absolute numbers remain almost at the same level (approximately 4.5-6.0*109/l). This is exclusively a percentage increase against the background of a decrease in the total number of leukocytes (mainly due to neutrophils).
Pathological causes
An increase in the number of lymphocytes and a decrease in the number of neutrophils during an infectious-inflammatory process is due to the characteristics of the functions they perform:
- Neutrophils are “close combat” immune cells that come into direct contact with infection and die during this confrontation. The greatest effect of neutrophils is manifested against bacteria and fungal flora, which they successfully phagocytose and destroy. With a viral infection, the effectiveness of neutrophils is low - they cannot always destroy them, but they effectively present their antigenic information to lymphocytes.
- Lymphocytes are long-range immune cells. They perform their functions of destroying pathogenic microorganisms through antibodies. During the immune response, they do not die like neutrophils.
Due to these features, long-term viral infections and chronic diseases lead to a decrease in neutrophils and an increase in lymphocytes.
What is a leukocyte formula shift?
In the standard leukocyte formula, young neutrophils are indicated from left to right, followed by more mature cells. The first step is to take into account the relationship between these two categories. The shift is classified into 3 types: left, with rejuvenation and right.
Shift in leukocyte formula
What is a shift in the leukocyte formula to the left?
A condition indicating the predominance of young cells in the bloodstream over mature ones, but due to their weak biological activity, they are not capable of normal maintenance of immunity. The reason for this phenomenon is often:
- Blood loss.
- Diseases accompanied by inhibition of the hematopoietic function of the bone marrow.
- Aseptic inflammatory processes.
- Malignant neoplasms.
- Infection with a purulent nature.
- Intoxication of the body.
When a shift in the leukocyte formula to the left with pronounced rejuvenation is detected, the result may indicate blood diseases (leukemia).
Read further: ESR in oncology - the norm and the relationship with cancer
What is a shift in the leukocyte formula to the right?
A condition that occurs when a growth of mature white blood cells is detected, with a predominance over all other types of cells. Such decoding is possible in the following conditions:
- Liver disorder
- Kidney dysfunction.
- Exposure to ionizing radiation.
- Regular blood transfusions.
After the analysis, the laboratory technician calculates the so-called shift index, which reflects the level of the total number of new leukocytes to more mature ones.
The leukocyte blood count allows for differential diagnosis between infections of viral and bacterial origin, as well as to suspect the presence of parasitic infestations and the presence of malignant neoplasms.
What is included in the leukogram
The leukogram, also called the leukocyte formula, the leukoformula of the blood, includes the following indicators: neutrophils, basophils, eosinophils, lymphocytes, monocytes. All of them belong to white cells, that is, leukocytes. In general, they reflect the state of the immune system, but each indicator also has its own clinical significance. Their role in the blood is shown in the table.
| Name | What processes are they involved in? |
| Neutrophils | Microphagocytosis, absorption of parts of destroyed cells (one’s own, microbial), toxins; upon destruction, they release substances that increase inflammation, stimulating the influx of new leukocytes into the lesion |
| Eosinophils | Inflammatory, allergic, absorb immune complexes (antigen-antibody), destroy parasites (roundworms, giardia) |
| Basophils | Inflammation, immediate type allergy, stimulate the influx of neutrophils and eosinophils into the area where a foreign protein or allergen enters; they can live outside the vessels - in the tissues, where they cause burning, itching, redness (they release histamine) |
| Lymphocytes | Recognize foreign proteins, kill cells infected with microbes, viruses, cancer, transmit information about the introduction of antigens, produce protective proteins - immunoglobulins (antibodies) |
| Monocytes | Phagocytosis - absorption and removal from the blood of dead cells, remnants of microbes, viruses, large protein altered molecules, immune complexes, hold a “mark” of destruction on the membrane, it is recognized by lymphocytes |
The leukocyte formula reflects the number and percentage ratio between different types of cells. The laboratory technician also points out the appearance of young, immature neutrophils. They, unlike band and segmented ones, may normally be absent. There should be no myelocytes or promyelocytes in the smear; in healthy people they are found in the bone marrow and do not pass into the blood.
We recommend reading the article about a general blood test. From it you will learn about the indicators of a general blood test, what the leukocyte formula is, what the main erythrocyte indices and hematocrit mean, as well as about the norms and deviations in a general blood test. And here is more information about eosinophils in the blood.
Deviations from the noma in adults
Lymphocytosis, manifested by an increase in the concentration of lymphocytes in the bloodstream, can indicate the development of one of the following pathologies:
- Chicken pox.
- Syphilis.
- Rubella.
- Leukemia.
- Lymphoma.
- Tuberculosis.
- Measles.
Low lymphocyte counts may occur due to:
- Immunosuppressive conditions.
- Autoimmune diseases.
- Kidney dysfunction.
- Deficiency of nutrients and microelements.
- Radiation therapy.
- Treatment with corticosteroids.
An increase in the number of neutrophils is an important indicator of the following diseases:
- Acute hemorrhage.
- Intoxication.
- Development of diseases of bacterial etiology.
- Myocardial infarction.
- Vasculitis.
- Malignant neoplasms.
- Autoimmune pathologies.
If the analysis shows a low concentration of neutrophils, doctors may suspect the following pathologies:
- Immunosuppressive conditions.
- Effect of ionizing radiation.
- Progressive infectious disease.
An increase in monocytes indicates the following conditions:
- Infections that occur due to the influence of bacteria.
- Progression of rheumatoid arthritis.
- Infectious mononucleosis.
- Parasitic infestations.
- Hemoblastoses.
A low concentration of monocytes in the lymphocyte formula helps to suspect pulmonary tuberculosis. If a high level of basophils is detected, one may think about the presence of chronic myeloid leukemia or erythremia. Deciphering the leukocyte formula in adults may show an increase in eosinophils, which is often detected during:
- Allergies.
- Scarlet fever.
- Parasite infestations.
- Skin pathologies.
- Eosinophilic leukemia.
A decrease in eosinophils in an adult can be triggered by progressive typhoid fever or adrenal hyperactivity. Deciphering the leukogram is performed with an assessment of nuclear shifts, where special attention is paid to the ratio of mature and immature neutrophils.
At the moment, the leukocyte formula is considered one of the most important indicators in diagnosis. Carrying out a CBC with an assessment of the leukogram makes it possible to discuss the presence of acute pathological conditions, the effectiveness of the prescribed therapeutic course, as well as possible prognoses for the future.
Biological role
Leukocyte changes are a natural reaction of the child’s immune system. The newborn's immune system experiences stress and begins to develop to effectively combat future threats. Formation takes time, so during the first year of life a child is at risk of developing many diseases.
It is important to know! Due to imperfect immunity, infants more often suffer from bacterial and viral infections. The cross indicates that the immune system is being rebuilt and adapted.
The situation with the formula in healthy children
In healthy children, the leukocyte formula changes in accordance with the average values. Physiological processes in the absence of negative manifestations are considered normal. However, you need to remember that the formula of newborns when affected by infection also changes.
In a healthy child, all test results correspond to age standards, there is no discomfort
If the child is not bothered by any manifestations, the change in the formula for the ratio of different types of leukocytes occurs in accordance with the reference data, there is no reason for concern.
Changes in lymphocytes
Changes occur quite quickly. Every baby goes through them. The doctor warns parents that all this is normal.
During crossover, the number of lymphocytes increases significantly and persists for up to 5 years. As the child gets older, the rate slowly decreases. The normal value for a person over 16 years of age is 19 – 37%.
It is important to know! If in childhood the number of lymphocytes has increased too much or decreased below normal, a detailed diagnosis is required.
Functions of lymphocytes
Lymphocytes are an important part of leukocytes. There are 3 types of cells in the blood: T-, NK- and B-lymphocytes. They recognize antigens, participate in cellular immunity, and help eliminate viral infections.
NK cells help fight tumors. They form an early immune response, preventing the development of cancer. If lymphopenia occurs, a number of diagnostic examinations are required. Occurs with insufficient blood supply, oncology, secondary immunodeficiency.
Change in the number of basophils
Basophils are cells involved in inflammatory and allergic processes. The content in the blood is approximately the same in adults and children. Norm – value up to 1%. An upward change in the indicator indicates the following pathologies:
- allergy;
- blood damage;
- endocrine disorders;
- low-grade inflammation of the gastrointestinal tract;
- ulcerative inflammation of the intestines.
Basophils decrease with hyperfunction of the thyroid gland, radiation exposure and stress conditions.
A high level of basophils may indicate endocrine diseases
Basophils do not participate in the leukocyte formula change. When analyzing blood, the value should be approximately the same.
Possible deviations from the norm in children
Any changes in the leukogram, be it a shift in the leukocyte formula to the left or right, as well as an increase or decrease in the leukocyte index of intoxication in a child, always indicate the onset or progression of various pathologies.
A high concentration of lymphocytes (lymphocytosis) is diagnosed when the body is affected by an infection of any etiology:
- Whooping cough.
- Flu.
- Rubella.
- Measles.
- Tuberculosis, etc.
In addition to the above, an increase in the concentration of cells can be caused by diseases such as asthma, autoimmune pathologies, and allergic reactions. A significant deficiency of leukocytes at this age (lymphocytopenia) indicates pathological damage to the bone marrow.
A large number of neutrophils (neutrophilia) or a neutrophil shift to the left in the first days of life is a physiological condition. Subsequently, a crossover of the leukocyte formula occurs.
Pathological neutrophilia may indicate inflammation of the umbilical wound (omphalitis), enterocolitis, streptococcal infection, etc.
An increase in the number of monocytes is characterized as a condition (monocytosis) that occurs due to fungal or viral infection. In this situation, the symptoms need to be judged by some visual signs:
- Lymphadenopathy.
- Inflammation in the nasopharynx and larynx.
- Hepatomegaly and pain in the right hypochondrium.
In addition, a shift in the leukocyte count to the right or left is often associated with a deficiency of monocytes (monocytopenia). A similar condition can develop with a lack of B vitamins and folic acid. This problem is often accompanied by iron deficiency or B12 and folate deficiency anemia.
An increase in the number of basophils (basophilia) is a fairly rare condition. The cause may be the patient’s tuberculosis, lymph node damage, or myeloid leukemia.
Eosinophils can also cause a shift in the leukocyte formula to the left or right. Eosinophilia may be due to allergies or the presence of parasitic worms.
Segmented neutrophils, lymphocytes: how do they change during crossover?
The crossover of the formula occurs due to the fact that in a small child the formation and maturation of immunity occurs. Different forms of cells are formed in greater or lesser quantities, all this changes over time... This is where the natural changes in blood tests come from.
Now about why this phenomenon is called crossover. The thing is that with it, the indicators of neutrophils and lymphocytes “cross” each other. First, neutrophils (segmented) are decreased, neutrophils are increased. Then everything changes: segmented neutrophils are increased, lymphocytes are decreased. In more detail, this happens as follows...
A newly born child has “normal” lymphocytes and neutrophils, there is no increase or decrease, and the indicators of these cells resemble those in adults: the first 30-35%, the second 60-65%.
However, by the age of one week, changes occur: the indicators “approach” each other. As a result, it turns out that segmented cells are decreased and lymphocytes are increased relative to the values that the little man had quite recently. Both parameters “occur” at a value of 45% - by the age of 4-7 days in the child’s blood they become equal.
Then each of them continues to change in the same direction, but at a different “speed”. By 10-14 days, a person has rather low segmented neutrophils, while lymphocytes increase and reach a content of 55-60%. In addition, at the same time, the level of monocytes in the blood increases slightly, up to 10%.
The subsequent months and years do not bring such dramatic changes in the composition of the blood as the first days of life. However, gradually segmented neutrophils increase, and lymphocytes decrease again. At 5-6 years old, their number becomes equal again. This is the second and last crossover of the leukocyte formula. Then some more changes occur, and everything turns out in such a way that, as a result, neutrophils are increased, and lymphocytes are decreased relative to that “average” 45%.
At approximately 10 years of age, the leukocyte formula stops changing, and all values approach the norms that were described at the beginning of the article.
Indications for analysis
Collection of biomaterial for subsequent assessment of the leukogram is advisable in one of the following cases:
- Passing a medical examination.
- Pregnancy planning.
- Preparing for surgery.
- Diagnosis of any pathology (leukocyte formula refers to one of the main types of walking OAC).
- Exacerbation of chronic pathology.
- Acute abdominal pain, increased sweating at night, weight loss, shortness of breath, diarrhea, enlarged lymph nodes.
Clinical indications for prescribing OAC with leukogram:
- Hyperthermia.
- Feverish condition.
- Pain in the joints.
- Body aches, general malaise.
- Headache.
- The need for differential diagnosis between viral and bacterial infections.
- Enlarged lymph nodes.
- Increased bleeding.
- Pustular rash on the body.
- Taking immunosuppressive drugs.
- Carrying out chemotherapy or radiation therapy.
- Night sweats.
- Routine examination during hospitalization.
- Routine examination of pregnant women.
For what reasons does the leukocyte formula change?
The blood leukogram may change due to various pathologies. There may be many reasons, but doctors have identified patterns of increases or decreases in the number of different types of cells.
Each type of leukocyte helps to identify the cause of the disease. If we are talking about a general increase in lymphocytes in the blood, then doctors call this condition lymphocytosis. It can be observed with viral, bacterial infections, lymphoma, lymphocytic leukemia, arsenic, lead poisoning, etc.
The number of neutrophils may increase due to endogenous intoxication of the body, bleeding, tissue necrosis, infections, taking corticosteroid hormones, and after abdominal surgery.
The level of monocytes increases in hemoblastoses, subacute and chronic infectious diseases. This indicator is especially important when diagnosing tuberculosis.
The percentage of neutrophils may decrease, which is also a deviation from the norm. This condition can be caused by acute viral infections (chickenpox, measles, rubella), thyrotoxicosis, anaphylactic shock, and hematological diseases.
The percentage of basophils increases with chickenpox, myxedema, chronic myeloid leukemia, nephrosis, and Hodgkin's disease. Decreases during pregnancy.
An increased level of eosinophils should be expected with allergies, parasitic diseases, during the acute period of any infection, with malignant tumors and inflammatory processes (rheumatism, scleroderma, etc.). This indicator decreases in the acute period of myocardial infarction, during severe purulent infections.
Preparing for analysis
To obtain the most reliable analysis results, the patient must prepare for the blood sampling procedure:
- Blood is taken in the morning, strictly on an empty stomach (you must wait more than 10 hours from the moment of eating to the analysis). Some time before the procedure, you can drink a glass of plain water.
- You need to exclude fatty, smoked, spicy foods and tonic drinks (coffee, strong tea, energy drinks), as well as any alcohol from your daily menu 3-4 days before the procedure.
- 1-2 hours before the scheduled time of blood sampling, you should not smoke (cigarettes, hookahs), you should not lift weights, or be nervous.
Immediately after collection, the test tube with the biomaterial is sent to the laboratory for testing. The laboratory assistant, using a microscope, determines the ratio of all visible leukocytes and calculates the leukogram. In addition, an automatic analyzer can be used for more accurate and faster results.
Read further: How long does alcohol last in a person’s blood (table)?
Why and how is material collected for the UAC?
A complete blood count (CBC) is a mandatory stage in the diagnosis of any disease, since the percentage of blood components changes in the presence of inflammatory processes. The number of some increases, while others decrease. A general blood test with a leukogram helps to see both the presence of inflammation and the body’s ability to overcome it.
Doctors recommend taking blood tests to:
- assess the severity of the patient’s condition, the course of the disease, possible complications;
- try to determine the cause of the disease;
- assess the correctness of the prescribed therapy;
- make a prognosis of the course of the disease and its possible outcome;
- confirm the diagnosis of the disease.
The total number of leukocytes in the analysis can only predict the presence of inflammation, and the detailed percentage of each type of cell gives a clear and detailed picture of the course of the disease in the body.
A leukocyte analysis is carried out using blood taken from a vein. To do this, an adult or child should not eat any food 3-4 hours before taking tests. Active physical activity and emotional stress should be avoided. All this can change the percentage of components at the time of analysis.
Analysis technique
Calculations of the leukocyte formula are carried out by qualified health workers using the method of studying smears under a microscope.
In addition, a hematology automatic analyzer is often used. If certain deviations are detected, an additional microscopic assessment of the smear is carried out, with a description of the clear morphology of visible cells and clarification of the leukogram.
Automatic devices make it possible to obtain better results: with technology, it is possible to examine more than 2000 cells, and under a microscope only 200. During a blood test on an analyzer, the result will be more informative.
Automatic counting also has a number of disadvantages, because it is not able to distinguish neutrophils into segmented and band types.
What leukocytes are included in the formula?
The calculation formula shows the percentage of the five types of white blood cells. Each indicator has its own norm, and it is different for different ages.
Red blood cells, platelets and different types of leukocytes
To understand the importance of the tests, it is worth learning more about the individual functions of each type of leukocyte:
- Eosinophils. This type of white blood cell appears if the body experiences an infectious, parasitic, allergic, autoimmune or cancerous disease.
- Neutrophils. Their main task is to eliminate pathogens of infectious diseases (viruses or bacteria). This is a large group of leukocytes, so it is divided into subtypes:
- myelocytes and metamyelocytes (the appearance of these bodies in the blood indicates a serious illness that lasts a long time);
- rod-nucleus (responsible for fighting bacteria, they come to work if the segmented ones are not able to overcome the infection);
- segmented (responsible for the constant maintenance of immune defense in the body, therefore they are present in the blood of healthy people).
- Lymphocytes. The purpose of lymphocytes is to promptly detect and destroy antigens that provoke various diseases in the body. synthesize antibodies, providing long-term protection in the form of the body's immune memory.
- Monocytes. These blood elements absorb destroyed and dying cells, foreign particles and foreign elements.
- Basophils. This type of leukocyte has not been thoroughly studied, but scientists were able to find out that basophils help the body fight allergic reactions by increasing their number during inflammation. Basophils also participate in the process of blood clotting.
- Plasmocytes. These are cells that take an active part in the process of producing antibodies. Normally, they are present in small quantities only in children. In adults, plasma cells appear only as a result of pathological processes.
What is ESR?
The general table of blood tests is supplemented by the ESR indicator. This is another characteristic that is assessed when there is a suspicion of:
- infectious diseases;
- renal failure;
- malignant tumors;
- rheumatological diseases.
ESR (erythrocyte sedimentation rate) is a general clinical indicator that shows the ratio of different protein fractions in the liquid part of the blood. Red blood cells are dense and heavy cells. If you deprive the blood of the opportunity to clot, then gradually the red blood cells will precipitate, and the plasma with lighter elements will float on top.
When there is a focus of inflammation or malignant formations in the body, lymphocytes begin to intensively produce protein components. Because of this, red blood cells stick together and precipitate faster.
Important! The ESR norm for males is 1-10 mm/hour, and for females – 2-15 mm/hour.
During a blood test, deciphering ESR may not always be objective, since this indicator is influenced by many factors:
- sometimes the indicator may not rise at all (this condition is observed in 2% of patients);
- elevated ESR after illness can persist for another 2-3 weeks or months;
- To decipher this indicator correctly, the patient should not eat for 3-4 hours before the analysis, it is contraindicated to smoke at least 30 minutes before collecting the material and to drink alcoholic beverages the day before.
Two methods recognized by WHO help analyze the ESR rate. Innovative medical institutions often use the Westergren method. This technique involves mixing blood in a test tube with an anticoagulant, and after an hour the sedimentation rate is assessed using a special scale. This approach makes it possible to measure the exact distance in a test tube between plasma and red blood cells. Anticoagulants prevent blood from clotting.
The second method of analyzing ESR is the Panchenkov method. This technique is considered traditional; it is still used in ordinary hospitals and clinics. To carry it out, blood is taken from a finger, and not from a vein. The calculation is carried out according to the same principle as in the Westergren method. Blood and sodium citrate are gradually added to the test tube in a ratio of 1:4. Everything is mixed in one glass capillary and after an hour, when the red blood cells settle, measurements are taken.
So, a leukogram is the basis of any diagnosis, since this analysis provides great opportunities to make an accurate diagnosis. Using such an analysis, a qualified doctor can not only predict the course of the disease, but also adjust the prescribed treatment.
Only a qualified physician should interpret the results. There is no point in drawing independent conclusions, since for various blood pathologies the indicators may be far from normal. If the analysis reveals serious blood pathologies, then such a patient should be treated by a hematologist. This is a highly specialized specialist who studies the hematopoietic organs, possible pathologies and diseases in this area.
LEUKOCYTE CROSSING
(RULE OF FOUR FOURS)
65% lymphocyte blood profile 44% blood 4 days 1 year 4 years age lymphocytes neurophils
Figure 12. Leukocyte crossover.
In a newborn, the percentage of neutrophils and lymphocytes is the same as in an adult. Subsequently, the content of neutrophils decreases, and the content of lymphocytes increases, so that by 3-4 days their number is equalized (44%). This phenomenon is called the first physiological (leukocyte) crossover. Subsequently, the number of neutrophils continues to decrease and by 1-2 years reaches 25%. At the same age, the number of lymphocytes is 65%, that is, at this age a lymphocytic blood profile is observed. Over the following years, the number of neutrophils gradually increases, and the number of lymphocytes decreases, so that in 4-year-old children these indicators are equalized again (44%) - the second physiological (leukocyte) crossover. The number of neutrophils continues to increase, and the number of lymphocytes continues to decrease, and by the age of 14 these indicators correspond to those of an adult, that is, a neutrophilic blood profile is observed.
Lymph
(from the Greek lympha - pure moisture, spring water) - a biological fluid formed from
interstitial (tissue) fluid,
passing through the system of lymphatic vessels through a chain of lymph nodes (in which it is cleansed and enriched with formed elements) and through the thoracic duct entering the blood .
Mechanism of lymph formation
associated with the filtration of plasma from the blood capillaries into the interstitial space, resulting in the formation of interstitial (tissue) fluid. In a young man weighing 70 kg, the interstitial space contains about 10.5 liters of fluid. This fluid is partially reabsorbed into the blood and partially enters the lymphatic capillaries, forming lymph. The formation of lymph is facilitated by increased hydrostatic pressure in the interstitial space and differences in oncotic pressure between blood vessels and interstitial fluid (ensuring the daily flow of 100-200 g of proteins from the blood into the tissue fluid). These proteins are completely returned to the blood through the lymphatic system.
Lymph volume
in the human body is, on average, 1-2 liters.
· peripheral lymph
(flowing from tissues);
· intermediate lymph
(passed through the lymph nodes);
· central lymph
(located in the thoracic duct).
Main functions of lymph:
1. Homeostatic –
maintaining the constancy of the cell microenvironment by regulating the volume and composition of the interstitial fluid.
2. Metabolic –
participation in the regulation of metabolism through the transport of metabolites, proteins, enzymes, water, minerals, molecules of biologically active substances.
3. Trophic –
transport of nutrients (mainly lipids) from the digestive tract into the blood.
4. Protective –
participation in immune reactions (transport of antigens, antibodies, lymphocytes, macrophages and APCs).
Lymph consists of a liquid part ( plasma
) and
formed elements
. The closer the lymphatic vessel is to the thoracic duct, the higher the content of formed elements in its lymph. However, even in the central lymph, formed elements make up less than 1% of its volume.
Lymph plasma
in concentration and composition of salts it is close to blood plasma, has an alkaline reaction (pH 8.4-9.2), contains less proteins and differs from blood plasma in their composition.
Formed elements of lymph.
The concentration of formed elements varies within the range of 2-20 thousand/μl (2-20´10 9 /l), changing significantly during the day or as a result of various influences.
Cellular composition of lymph:
90% lymphocytes, 5% monocytes, 2% eosinophils, 1% segmented neutrophils and 2% other cells. Red blood cells are normally absent from the lymph, entering it only when the permeability of the blood vessels of the microvasculature increases. Due to the presence of platelets, fibrinogen and other clotting factors, lymph is able to coagulate to form a clot.
1. Almazov V.A. Physiology of leukocytes. – L., Nauka, 1979.
2. Bykov V.L. Cytology and general histology (functional morphology of human cells and tissues). – St. Petersburg: SOTIS, 1998.
3. Vashkinel V.K., Petrov M.N. Ultrastructure and functions of human platelets. – L., Nauka, 1982.
4. Volkova O.V., Eletsky Yu.K. and others. Histology, cytology and embryology: Atlas: Textbook. – M.: Medicine, 1996.
5. Histology (introduction to pathology) / Ed. E.G. Ulumbekova, Yu.A. Chelysheva. – M.: GEOTAR, 1997.
6. Mayansky A.N., Mayansky D.N. Essays on the neurophile and the macrophage. – Novosibirsk, Nauka, 1983.
7. Protsenko V.A., Shpak S.I., Dotsenko S.M. Tissue basophils and basophilic granulocytes of blood. – M., Medicine, 1987.
8. Reusch A. Fundamentals of immunology. Per. from English – M., Mir, 1991.
9. Sapin M.R., Etingen L.E. Human immune system. – M., Medicine, 1996.
10. Semchenko V.V., Samusev R.P., Moiseev M.V., Kolosova Z.L. International histological nomenclature. – Omsk: OGMA, 1999.
11. Willoughby M. Pediatric hematology. Per. from English – M., Medicine, 1981.
What is the need
This is necessary for diagnosing acute or chronic diseases, cancer infections. However, this type of analysis is carried out in combination with others, since it does not give an accurate answer to the type of origin of the disease, its development and outcome.
Indicated for monitoring infectious, oncological and autoimmune diseases. And also in combination with a leukocyte blood count or a general blood test.
A clinical blood test can provide many answers to complex diagnoses and diseases, as well as describe a person’s condition. However, decoding should be done by an experienced specialist who can give an accurate description and correct the treatment process.
Carrying out analysis
Before you do a blood test for the leukocyte formula, you need to undergo simple preparation. You just need to refuse food 3-4 hours in advance, and also not be subjected to physical and emotional stress.
The material is blood from a vein. Next, it is placed on a special glass plate under a microscope. The laboratory technician fishes out several hundred cells to determine the number and level of white blood cells. The next step is to distribute the blood over the entire glass surface, but not evenly. The heavy bodies are located at the edges, and the light ones in the center. The heavy ones include: monocytes, basophils and eosinophils, and the light ones include lymphocytes.
When counting white bodies in the blood, two options are used:
- Schilling method. Counting occurs conditionally in 4 areas of the smear.
- Filipchenko's method. The laboratory technician divides the smear into 3 parts and determines the quantity along a straight transverse line.
However, there are clinics equipped with new equipment and the counting of leukocytes is done by a special device - an analyzer. And if the result deviates sharply from the norm, then a person intervenes. It should be noted that the quantity error error exists in any case. Factors include errors in blood collection, smear preparation, and others.
The transcript of the blood test will be ready in a few days. The attending physician analyzes the obtained values.
Analysis transcript
A specially trained specialist is responsible for deciphering the leukocyte formula of blood. However, you can also compare the result with the norms. To do this, you need to know what indicators are the maximum permissible for a healthy person in accordance with his age.
There are leukocyte blood formula standards for adults:
Table of normal leukocyte formula for adults
- neutrophils - 55%;
- lymphocytes - 35%;
- monocytes - 5%;
- eosinophils - 2.5%;
- basophils - 0.5%.
Leukocyte formula norms by age:
- hemoglobin is a protein found in red blood cells. It is needed to transport oxygen throughout the body, as well as carbon dioxide. For men: 130 - 160g/l, for women: 120 - 140g/l, for children from 0 to 6: 100 - 140g/l, and up to 12: 120 - 150g/l.
If the indicators in the leukocyte formula deviate, for example, in a decreasing direction, the possible development of various types of anemia or leukemia is detected. If increased, it indicates the presence of diabetes mellitus, dehydration or diseases of the hematopoietic system.
- red blood cells . The norm for men is 4.0-5.0 × 1012 / l, for women: 3.6 - 4.6 × l, in children from 0 - 6 years old: 5 - 15.5 × l, in children from 0 - 6 years: 5.0-15.5×l, up to 12 years – 4.0 – 13.5×l.
An increase in red blood cells is possible with drug allergies, sinusitis, bronchitis, and leukemia. If the indicators are less than normal, then this indicates the initial stage of inflammation, the development of viral or infectious diseases.
- neutrophils. The normal amount of segmented neutrophils for adults is from 50 to 70%, for children from 0 to 6: 28 - 55%, up to 12 years: 43 - 60%. As for stab diseases, in adults it is 1-3%, and in children under 16 it is 1-5%. A deviation from the norm shows that not everything is in order in the body. So, if the amount is exceeded, then this is mainly during bronchitis, sinusitis, and inflammation of the organs. Reduces this indicator of diseases that are infectious or blood diseases.