Methods for examining the human body are constantly evolving: new types of diagnostics are appearing and old ones are being improved. But in some cases, the help of long-proven techniques such as radiography is needed. In maxillofacial medicine and otolaryngology, radiography of the temporal region is still successfully used. This examination reflects the structure of the bone quite informatively, on a par with such progressive studies as computed tomography and magnetic resonance imaging. It is used to determine diseases of the ear, vestibular and masticatory apparatus, and has its own characteristics and results.
Why do you need an X-ray of the temporal lobe?
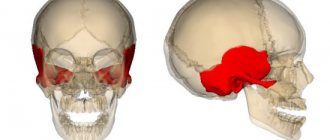
Radiography appeared in the 19th century and made it possible to make diagnoses without surgical intervention. This type of diagnosis is especially significant in otorhinolaryngology and maxillofacial medicine, where doctors have to deal with very important and sensitive organs, and errors in diagnosis are very expensive. Thus, radiography of the temporal bone is intended for examining the middle ear, masticatory apparatus, and pathologies of the facial part. The temporal lobe regulates all three functions of the human skeleton: supporting, protective, and motor.
Timely and correct diagnosis of the pathology of this area of the skull is extremely important for successful treatment. Using X-rays, the doctor obtains images of the temporal bone, establishes the affected area, and finds inflammatory processes in the hearing or chewing apparatus. A repeat procedure is prescribed to monitor the therapy and evaluate its effectiveness. X-rays play an equally important role in identifying malignant and benign tumors in the ear canal; in the image, the doctor can see bone destruction and suggest a diagnosis.
It is worth noting that radiography remains important for examining the bone part of the skeleton, as it reflects them better. To diagnose soft tissues, more informative methods are prescribed - magnetic resonance imaging or computed tomography.
When is an x-ray needed?
An x-ray of the ear and temporal bone is usually necessary in the case of:
getting injured, be it a bruise or a fracture;
Ear pathologies, mainly otitis and other disorders of the vestibular apparatus;Suspicion of the occurrence of tumor processes in the temporal zone.
Considering the presence of harmful radiation during the procedure, as well as the development of safer and more informative research methods (meaning MRI and CT), x-rays of the temporal bone are performed much less frequently. Currently, the reason for prescribing the procedure may be:
the need to identify air cavities in the mastoid process - pneumatization;
Study of the location of intra-ear implants.
If it is not possible to conduct an MRI or CT scan, an x-ray of the ear and temporal bone is necessary for acute or chronic inflammatory processes of the middle ear, cholesteatoma or mastoiditis. Otitis occurs in approximately 50% of cases. When we talk about the middle ear, we mean the area just behind the eardrum. The inner ear is the area closest to the brain that is responsible for balance.
What can be seen in the photographs
On an x-ray, it is possible to track only otitis media of the middle ear, with a noticeable compaction in the soft tissues, which looks like a grayish opaque mass. Periodically, the disease is accompanied by vascular sclerosis and bone growth, and it can reach both the temporal lobe and the temporomandibular joint.
Where, how and who should undergo the procedure
Typically, such a procedure is prescribed by otolaryngologists, oncologists or traumatologists. If there is a referral, the study is carried out either at the place of residence or in another medical institution that has the ability to carry out the procedure.
It must be taken into account that X-ray examination of the temporal bone is contraindicated:
pregnant women, regardless of term;
If the patient has metal implants in the temporal zone.
How photographs are taken and decrypted
There are two ways to obtain images - one-time and two-time. At the same time, more complete information is provided by two snapshots. A comparative analysis is made by examining x-rays of the right and left bones. Pictures can be obtained by projections:
oblique;
Lateral;Axial.
The most commonly used is a lateral radiograph. As for decoding, it is carried out immediately after the x-ray. The condition of all visualized components of the temporal bone is assessed. If tumors and other formations are detected on the image, their location and size are assessed.
X-ray examination is used in otorhinolaryngology to assess the condition of the structures of the inner, middle and outer ear. A plain X-ray of the head does not provide a complete picture of these structures. Specialists in the field of radiation diagnostics use targeted X-rays or magnetic resonance and computed tomograms for this purpose.
Currently, the indications for radiography of the temporal bones are gradually narrowing. This is due to the low resolution of the method, the imposition of extraneous shadows, the complexity of installation, as well as the introduction of more informative research methods into clinical practice.
Indications for use
Radiation diagnostics of the temple is prescribed to check the condition of the organs located in this area. X-rays show congenital bone destruction, inflammation, and tumors. This technology remains indispensable in emergency cases, such as head injuries. Also, such an examination is necessary after operations, implantation, to adjust treatment.
X-ray of the temporal bone is prescribed in the following cases:
- if tumors or other neoplasms are suspected;
- after head injuries;
- to establish the causes of hearing impairment or complete disappearance;
- for pathologies of the temporomandibular joint;
- to study congenital anomalies of the bones and organs of the temple;
- in case of malfunction of the vestibular apparatus, loss of a sense of balance and orientation in space.
With the development of computer diagnostics, the scope of radiography is increasingly narrowing. However, in some cases, even CT and MRI cannot replace conventional x-rays. For example, in case of choleastomy and mastoiditis, the most informative research method is considered to be a regular x-ray. It is also often prescribed when filling the mastoid process with air. In dentistry, during a purulent-inflammatory process in the teeth, the doctor must make sure that the exudate has not penetrated into other parts of the head; this also requires an x-ray.
Indications for diagnosis
An MRI examination procedure is prescribed if the patient complains of the following symptoms:
- hearing loss or complete loss;
- dizziness and loss of orientation;
- external signs of inflammation of the ears;
- pain, noise, ringing in the ears, itching;
- bloody, purulent, or watery discharge from the ears.
Middle ear diseases can manifest themselves in loss of balance and decreased tone of the facial muscles.
Constant tinnitus may indicate nervous disorders, dysfunction of the vascular system, diseases of the spine, and abnormalities in the functioning of the brain. An MRI of the ear is required to exclude the listed diseases.
Contraindications for the procedure
Radiography is an almost universal diagnostic method. Contraindicated during pregnancy, when in most cases such examination is replaced by other types of diagnostics. But in emergency situations and if it is impossible to conduct a study that is safe for the fetus, such as an MRI, pregnant women still undergo an X-ray examination. To protect the fetus from radiation, the patient’s body, except for the head, is covered with a special reflective apron.
People with metal implants are more often prescribed a CT scan because such parts in the body cause shadows in the photo, which makes diagnosis difficult. However, in rare cases, this problem is solved in the same way as with pregnant women - the body is covered with a lead apron. In other cases, this type of study is prescribed for both adults and children. To minimize the radiation dose, such a procedure is prescribed only when absolutely necessary.
Types of X-ray examination
X-rays of ENT organs can be classified according to the area of interest and the purpose of diagnosis. There are two main types of x-rays:
X-ray examination
- Survey radiography;
- Sight radiography.
The first type is usually prescribed for complaints of unclear pain and discomfort, the cause of which was not determined by examination in the ENT office. A specific part of the body is examined - this could be the frontal lobe, nasal sinuses and other parts. Survey radiography, therefore, only sets the boundaries of further research, although in some cases the information obtained through it is sufficient.
Sight radiography is often carried out after survey radiography. For example, the maxillary sinuses were examined for the first time and compaction or swelling was found in one of them. A targeted x-ray of the diseased sinus is prescribed to clarify the cause of swelling or compaction.
Where can I get an X-ray of the temporal lobe?
Pictures of the temple structure are taken using a conventional X-ray machine or a digital one. The first, as a rule, is available in any hospital or clinic, and such a service in government institutions should be free for every patient under a compulsory health insurance policy. You may have to wait a few days for the images and their transcripts and then give them to the doctor who referred you for the study.
Digital equipment is usually available in private clinics. This method is characterized by the speed of obtaining images and greater accuracy. In addition, the doctor can view the structure of the temporal region already during the process, since the image is immediately transmitted to the monitor. Results can be obtained after 30-40 minutes. The price of such a service ranges from 15 to 80 dollars. The cost will depend on the pricing policy of the medical institution, the equipment itself, and the qualifications of doctors.
X-ray examination
The main role in diagnosing congenital hip dislocation belongs to x-ray examination. We cannot support those doctors who keep a child with symptoms of hip dysplasia or dislocation from X-ray examination until 3 months of age (in the absence of an ultrasound method), explaining this by the negative impact of radiation on the baby. However, late diagnosis of the disease has an even worse impact on the child’s health.
| Schemes for diagnosing VVB |
| X-ray anatomy |
An x-ray is taken with the child in the supine position with the legs extended and parallel. I would like to emphasize that in no case should you bend the limbs at the hip joints (which is also encountered during this study), since this changes the relationship in the hip joint in the frontal plane and, as a result, can complicate the correct interpretation of the main x-ray indicators.
As is known, most of the skeleton in young children consists of cartilage, and therefore the contours of the femoral head and acetabulum remain invisible on the x-ray image. In this regard, certain schemes are used to decipher radiographs.
It can be difficult to decipher a radiograph in newborns and young infants, since it is quite difficult to distinguish a moderately severe disorder of joint development from a lower variant of the norm. Therefore, auxiliary lines are drawn on the radiograph, with the help of which the distance and angles are measured.
The X-ray method of research plays a significant role in the diagnosis of dysplasia of the hip joint in newborns. During radiography, the child lies on his back with his legs extended and adducted in a position of some inward rotation, strictly symmetrically. The pelvis should fit snugly against the cassette. It is necessary to protect the genitals with a lead plate, which, if positioned correctly, does not interfere with radiography. When X-ray diagnosing diseases of the hip joints, it should be taken into account that newborns do not have ossification nuclei of the femoral heads and the acetabulum is also cartilaginous and does not provide a contrasting shadow. When reading radiographs, particular importance is attached to the condition of the upper edge of the acetabulum, the relationship of the upper end of the femur and the acetabulum. For this purpose, special diagrams are used, which, using special lines, establish the normal arrangement of the elements of the hip joint and, accordingly, make it possible to determine the displacement of the hip in relation to the socket and its degree. Various schemes have been proposed for early radiological diagnosis of congenital hip dysplasia.
Schemes for diagnosing VVB
Hilgenreiner scheme
Rheinberg circuit
Ombredan Scheme
Calvet and Shenton scheme
Rheinberg circuit
| Used for reading radiographs of hip joints in infants. Horizontal line A, drawn through the Y-shaped cartilages, crosses the middle or upper part of the ossification nucleus of the femoral head. Then line B and the midline are drawn through the superolateral protrusion of the acetabulum. |
The distance between the midline and line B is measured, and line B1 is drawn at the same distance from the midline. In case of unilateral hip dislocation, a vertical line is first drawn on the healthy side and then on the diseased side.
With congenital dislocation of the hip, the proximal end is located outward from the vertical line B and above the horizontal line A. Another identifying feature is the lower edge of the femoral neck, the contour of which in the medial direction should smoothly intersect the lower contour of the horizontal branch of the pubic bone and form the correct line - Shenton's line.
Ombredan Scheme
| A perpendicular, lowered from the outermost edge of the acetabulum to a horizontal line, divides the hip joint into 4 parts. Normally, the ossification nucleus of the femoral head is located in the lower internal quadrant. In case of subluxation - in the outer lower quadrant. In case of dislocation - in the outer upper quadrant. |
Calvet and Shenton scheme
| Calvet Line | Shenton Line |
| 1. Calvet's line is a line connecting the outer edge of the ilium and the upper edge of the femoral neck. Normally it forms a regular continuous arcuate line. With subluxation or dislocation in the hip joint, the line becomes discontinuous and irregular. 2. Shenton’s line is a line connecting the lower edge of the femoral neck and the upper edge of the obturator foramen. Normally, a smooth arched line is formed. With subluxation and dislocation, the femoral neck moves upward and the arcuate line is interrupted. |
Hilgenreiner scheme
In our opinion, Hilgenreiner’s scheme is quite informative and at the same time simple. In our practice, to read radiographs we use a special transom grid proposed by Ter-Egiazarov G.M., Yukina G.P.
First of all, the value of the acetabular angle is calculated, which is normally less than 300 in children under 3 months of age and decreases to 20 degrees by the age of one year. The acetabular angle is the angle of the roof of the socket, formed by the intersection of a line drawn through the Y-shaped cartilages and a tangent running along the upper edge of the glenoid cavity. The value h, which tells us about the vertical displacement of the head relative to the acetabulum, is the distance from the horizontal Hilgenreiner line to the middle of the metaphyseal plate of the proximal femur. Normally, this value is the same on both sides and ranges from 9 to 12 mm. A decrease in this indicator and its difference on the right and left indicate the presence of pathology. Value d, indicating the lateral displacement of the femoral head relative to the acetabulum - the distance from the bottom of the acetabulum to the vertical line (value h). With normal development of the hip joints, it is also the same on both sides and should be no more than 15 mm. Hilgenreiner's scheme is convenient, reliable, gives an objective view of the hip joint, and is quite simple if you know how to read radiographs. Its great advantage is that it allows early detection of minor displacements of the femur outward and upward.
Preparation and methodology
No special preparation is required. Before the procedure itself, the subject must remove all jewelry, even if it is on the wrists or fingers. Metal accessories produce artifacts in images, which can lead to incorrect diagnosis. Dentures, if any, are also removed. The doctor must be warned if there are implants in the body. If the patient has already undergone such a diagnosis, be sure to bring pictures of previous studies with you. They will be needed to compare and track the development of the disease - its dynamics.
There are more than 10 ways to obtain X-ray images; they differ in the position of the head during the examination, and at the same time, in the reflected areas in the image. The most common are three types, which are called styling and are assigned for different purposes.
Laying according to Mayer
Often this projection is needed to examine the middle ear and detect pathologies in it, to study the antrum - mastoid cave. With her help:
- establish the causes of hearing loss;
- detect tumors and inflammations;
- after a head injury, such an image shows a lesion in the structure of the middle ear and fractures of the pyramid.
To carry out this procedure, the patient lies down on the table, stretches his arms along his body, and slightly pulls his chin towards his chest. The doctor or laboratory assistant turns the subject’s head so that the median plane forms 45 degrees with the plane of the table. A cassette is inserted behind the ear and a series of images are taken. This completes the installation according to Mayer; the patient will only have to collect the data.
Laying according to Schüller
Performed in an oblique projection. This type of diagnosis is used in dentistry and maxillofacial medicine. The subject lies on his side and turns his head so that the side of the skull of interest is exposed. The hand clenched into a fist should be placed under the head so that it remains motionless, the other hand should be extended along the body. The health worker monitors the patient’s position and controls the process. The cassette is placed behind the ear and the examination is performed.
The images obtained in this way show the structure of the mastoid process and reveal abnormalities of the organs in the temple area. The doctor can evaluate the condition of the temporomandibular joint and identify fractures in the temporal bone. Due to the fact that the mastoid process can be of individual shape, the study is done on both sides for comparison.
Laying according to Stenvers
The picture is taken in transverse projection. The technique for carrying out such a procedure differs only in the position of the subject. The patient lies down on the table with his stomach down, bends his head so that the upper edge of the eye socket and cheekbone are adjacent to the table. The doctor will strictly ensure that the head is turned in the right direction and creates the correct angle, explaining to the patient how to do this. The cassette is placed under the cheekbone and eye socket. A series of photographs according to Stenvers clearly shows the structure of the pyramid, the inner ear, and the mastoid process. This is how tumors, injuries, and pyramidal fractures are diagnosed.
General characteristics of the examination
Diagnosis of the temporal bone is a complex radiographic task. There are many ways to study specifically the area where the hearing organs are located using this device and tomography. The procedure is considered one of the effective methods for determining ear pathological processes and injuries. To have a complete clinical picture of the structure and different variants of the development of the disease, this method is quite suitable. Due to the complex location of the temporal zone, there are some difficulties in studying the ear areas. X-rays for otitis media in the ears are performed using several methods.
- Diagnosis according to Mayer. The patient should lie on his back, with the inflamed auditory organ pressed against the cassette. The image makes it possible to examine the walls of the bony hearing zone, the tympanic meatus and the area around it.
- Shot according to Schuller. An examination of the hearing organ along with the mastoid process is carried out. During the procedure, the patient must place his head with the inflamed part down. The X-ray beam acts in such a way that, together with the cassette, it creates an angle of 35 degrees. As a result, there is a coincidence of the auditory department, which appears in the picture as a dark circle. Such a study helps determine the type of process, the location of the sinus and various inflammations and changes.
- According to Stenvers. The study is a snapshot of the pyramid. The patient is placed on his stomach, the cassettes should be in contact with the tip of the nose. The image shows the internal part of the hearing organ and the apex of the pyramid.
X-ray examination of the ear area and canal is suitable for determining changes in the temporal bone due to inflammation. For otitis media, this examination is considered an effective way to determine the condition of the auditory department.
X-ray of the ear.
Decoding the results
An oncologist, dentist, otorhinolaryngologist (ENT), or therapist can refer you for an x-ray of the temporal bone. The diagnosis is carried out by an x-ray technician, and a radiologist interprets the results of the study. Based on the images, he draws up a protocol in written form or electronically if a digital device was used. The duration of decoding also depends on the technology used and the workload of the hospital. The fastest way to provide data is in private clinics; in public clinics it will take 1-3 days if the procedure is not an emergency. The radiologist should not give any recommendations regarding treatment. The patient collects the data at the appointed time and takes it to the doctor who referred him for the study. Based on these results, the doctor will judge the patient’s condition and determine further treatment tactics.
Is this dangerous for health?
During an X-ray examination, a person receives a dose of radiation. In this case, it is approximately 3-4% of the annual norm. Every day we encounter sources of radiation and receive a dose of radiation; for example, in one hour on the beach we receive the same 4% of the annual radiation rate. That is, radiography of the temporal bones does not pose a health hazard, but it is not recommended to overuse such diagnostic methods. The opinion of experts is that the acceptable norm is 7 sessions per year.
In what cases is an x-ray of the larynx prescribed?
The need for a diagnostic procedure will be determined by an otolaryngologist. Direct indications for the study are the following conditions:
- trauma to the neck area;
- possible presence of a foreign object;
- suspected injury during tracheal intubation;
- assessment of the condition of the organ after a chemical or thermal burn;
- visualization of the state of the vocal folds during their paresis;
- the likelihood of having cystic and other types of neoplasms;
- whooping cough, laryngitis and other types of infectious processes localized in the larynx.
Regarding contraindications, diagnosis has no absolute restrictions. It is not recommended for use during pregnancy, in particular in the early stages. If necessary, it is carried out during lactation. After the procedure, it is recommended to express breast milk.
Alternative Methods
In addition to X-rays, other types of examinations are also used. Computed tomography is increasingly replacing conventional radiography. It uses an even lower dose of radiation, but the information content is higher. During a CT scan, the doctor receives a three-dimensional model of any part of the body, including the temporal regions. Moreover, this method displays both bones and soft tissues equally well, which makes it possible to immediately examine the structure of the skull and brain.
Another alternative is magnetic resonance imaging. Its advantage over the two previous options is that the patient is not irradiated at all, since MRI does not use X-rays. The principle of this diagnostic procedure is the phenomenon of nuclear magnetic resonance. The effectiveness of this method is comparable to CT, as it also transmits a detailed image to a monitor in real time.
However, conventional radiography also has an advantage over progressive methods. It provides enough information when examining bones, although it is inferior in diagnosing soft tissues. In case of destruction of the temporal areas, this examination will be sufficient at the initial stage of diagnosis. It is easy to perform and results can be obtained quickly if the situation requires it. The level of radiation, although it remains the highest among other studies, is safe for the patient’s health, provided that safety precautions and time intervals between studies are observed. Moreover, among all other options, this is the most affordable, including economically, which makes research possible for all segments of the population.
2. In 2020, by decision of the examination committee at the private institution of additional professional education “Institute for Advanced Training of Medical Personnel”, she was admitted to carry out medical or pharmaceutical activities in the specialty of radiology.
Experience:
general practitioner – 18 years, radiologist – 2 years.
> MRI (magnetic resonance imaging) of the inner ear
This information cannot be used for self-medication! Consultation with a specialist is required!
Why is the inner ear examined using MRI?
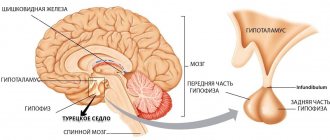
Located deep in the temporal bone of the skull, the inner ear is an organ inaccessible to visual examination. And its proximity to the brain, important blood vessels, and the organ of vision precludes the use of radiation diagnostic methods and invasive diagnostic operations. Therefore, magnetic resonance imaging, which does not have any harmful effects on the body, is the most informative method of examining the inner ear. Based on the use of the phenomenon of magnetic resonance, it makes it possible to obtain images of this complex organ taken in various planes.
Where can I get an MRI of the inner ear?
MRI of the inner ear can be done in clinics and diagnostic centers that are equipped with appropriate equipment and therefore provide this service. As a rule, an otorhinolaryngologist, neurologist or, less commonly, a therapist gives a referral for this examination. Hospitalization to a hospital is not required.
What are the indications for performing an MRI of the inner ear?
MRI of the inner ear is prescribed in cases where the patient has certain clinical symptoms, and the doctor needs to either confirm or exclude the presence of a pathological process in the hearing aid.
Persons with severe hearing loss or complete loss, with symptoms of inflammation (swelling, redness) in the outer ear, with complaints of pain or itching, noise or ringing in the ears, as well as frequent dizziness, are referred for this examination. Tinnitus is most often a symptom of vascular disorders, diseases of the brain or cervical spine. But the first priority when a patient complains of tinnitus is to exclude the presence of a pathological process in the inner ear. In addition, indications for MRI of the inner ear are pain in the nasopharynx and discharge from the external auditory canal.
How to prepare for an MRI of the inner ear?
No special preparation is required before MRI. But you should know that during its execution there should be no metal objects on the subject’s body or on his clothing (zippers, pins, hairpins, jewelry, hairpins, metal implants in the oral cavity, joint and other metal prostheses, etc.). Their presence may not have the best effect on the quality of the pictures. And they themselves can shift and even heat up to a high temperature.
The doctor giving the referral for MRI should be informed about the presence of electronic devices in or on the body (insulin pump, electronic implants, pacemaker, hearing aid, etc.). Under the influence of a magnetic field, their operation may be disrupted.
Women should not hide pregnancy, if any, from the doctor.
What does an MRI of the inner ear reveal?
In the photographs obtained as a result of the examination, taken in different projections, it is possible to detect even the smallest pathological changes in the inner ear. MRI makes it possible to create a three-dimensional model of an organ, which can not only be enlarged and reduced, but also viewed from different angles, adjusting the clarity of the image. The photographs show deformations of the labyrinth, areas of bone tissue destruction, and inflammatory processes affecting the auditory nerve. The consequences of previous otitis media, tumors and other tissue growths, metastases of tumors located in other organs, changes in the structure and density of bone tissue will not go unnoticed.
The advantage of MRI of the inner ear over all other examination methods is its safety and absolute information content. No part of the inner ear remains obscured or invisible.
Select a category Adenoids Sore throat Uncategorized Wet cough Wet cough In children Sinusitis Cough Cough in children Laryngitis ENT Diseases Folk methods of treating Sinusitis Folk remedies for cough Folk remedies for the runny nose Runny nose Runny nose in pregnant women Runny nose in adults Runny nose in children Review of drugs Otitis Medicines for cough Treatments for Sinusitis Treatments for cough Treatments for the runny nose Symptoms of Sinusitis Cough syrups Dry cough Dry cough in children Temperature Tonsillitis Tracheitis Pharyngitis
- Runny nose Runny nose in children
- Folk remedies for runny nose
- Runny nose in pregnant women
- Runny nose in adults
- Treatments for a runny nose
- Cough in children Dry cough in children
- Traditional methods of treating sinusitis
- Pharyngitis
To establish an accurate diagnosis of a specific type of ear pathology, otolaryngology often resorts to x-ray examination.
An x-ray of the ear with otitis media makes it possible to examine in detail the structure of this organ. Similar manipulations include CT and MRI. The article explains what research is and how to prepare for it. Diagnosis of the temporal bone is a complex radiographic task. There are many ways to study specifically the area where the hearing organs are located using this device and tomography. The procedure is considered one of the effective methods for determining ear pathological processes and injuries. To have a complete clinical picture of the structure and different variants of the development of the disease, this method is quite suitable. Due to the complex location of the temporal zone, there are some difficulties in studying the ear areas. X-rays for otitis media in the ears are performed using several methods.
- Diagnosis according to Mayer. The patient should lie on his back, with the inflamed auditory organ pressed against the cassette. The image makes it possible to examine the walls of the bony hearing zone, the tympanic meatus and the area around it.
- Shot according to Schuller. An examination of the hearing organ along with the mastoid process is carried out. During the procedure, the patient must place his head with the inflamed part down. The X-ray beam acts in such a way that, together with the cassette, it creates an angle of 35 degrees. As a result, there is a coincidence of the auditory department, which appears in the picture as a dark circle. Such a study helps determine the type of process, the location of the sinus and various inflammations and changes.
- According to Stenvers. The study is a snapshot of the pyramid. The patient is placed on his stomach, the cassettes should be in contact with the tip of the nose. The image shows the internal part of the hearing organ and the apex of the pyramid.
X-ray examination of the ear area and canal is suitable for determining changes in the temporal bone due to inflammation. For otitis media, this examination is considered an effective way to determine the condition of the auditory department.
X-ray of the ear.
Which is better: CT or MRI of the inner ear?
Only the attending physician will help determine the effectiveness of computed tomography and magnetic resonance imaging. Different pathologies require different diagnostic methods, so MRI cannot always help determine the cause of hearing disease. MRI will help identify the causes of pathologies that lead to the appearance of noise or ringing in the ears. In this case, CT is a more informative diagnostic method, as it will help determine changes in bone structures and their density.
To diagnose tumor processes, MRI is used with the introduction of a contrast agent, which will appear as a light spot on the image. It is impossible to say about the unambiguous effectiveness of one or another method, because everything depends on the type of disease being diagnosed.
The cost of CT and MRI in Moscow clinics without contrast differs significantly from the price of an X-ray image, but the information content of such studies is much higher. On average, the cost of an MRI of the inner ear varies between 3000-6000 rubles. If diagnostics of the inner ear is included in an MRI of the brain, then such a procedure will cost an order of magnitude more – from 9,000 rubles.
X-ray image of the temporal bones
can be obtained simultaneously by taking photographs of the base of the skull on one film or using other survey projections. However, these images, despite their important advantage - the same projection and technical conditions, do not provide an isolated image of the most important parts of the temporal bone: the attic, aditus ad antrum, antrum, labyrinth, sinuses and other anatomical details.
This is achieved
other methods, which we proposed to call two-stage, since obtaining images of the right and left temporal bones requires two separate procedures. Radiographs of the diseased and healthy ear are needed to obtain comparative radiological data. Methods for two-stage radiography of the temporal bone can be divided into three main groups: lateral, oblique and axial projections.
The best representatives
These groups should be considered the lateral projection of the temporal bone, proposed in 1905 by A. Schiiller, the oblique projection proposed in 1917 by N. Stenvers, and the axial projection of Mayer (E. J. Mayer) (1923) .
Lateral radiograph of the temporal bone
(according to Schüller) should be considered a review and used first when examining the ear for any clinical indication. From a lateral photograph, one can best judge the prevalence and size of the cells of the mastoid and squamous parts, the position of the sigmoid sinus, the severity of the emissary and other smaller sinuses, such as sinus petrosquamosus and sinus petrosus superior, the antrum mastoideum, the size of the external and partly the internal auditory openings and the walls of the external auditory canal, the zygomatic process and details of the temporomandibular joint, etc.
Stenvers method
was proposed to study some details of the petrous part, namely the labyrinth, the internal auditory canal and the apex of the pyramid. The temporal bone oblique technique is the most difficult, partly because of the difficulty of obtaining identical x-ray images of the right and left ears. The oblique image is of great value for the study of the deep-lying cellular system of the temporal bone: perianthral cells, retro- and translabyrinthine cells and cells of the very apex of the pyramid. Thus, the oblique projection can also serve for the purposes of a detailed study of the development of pneumatization of the temporal bone.
Axial radiograph of the temporal bone
(according to Mayer) is used in many cases and is mandatory for chronic ear diseases, traumatic injuries, tumors, etc. This method, like the Stenvers method, is complementary to the lateral image and is superior to it in terms of better identification of the few, but important for studying the anatomical details of the temporal bone.
These include
: opening and walls of the external auditory canal, attic and auditory ossicles, antrum and sigmoid sinus. The technique of axial ear photographs is more complex than that of lateral ones. Incorrect positioning of the patient's head, even with minor deviations from the rules, leads to projection distortions and gross diagnostic errors. In the technique of radiography of the temporal bone, both in axial and in other projections, it is very important to have an idea of the causes of errors in head positioning and methods for eliminating them in order to obtain repeated typical images.
In addition to the methods described
, it is much less common to resort to other methods of ear radiography to clarify the localization of the pathological process. These include an isolated (tangential) image of the mastoid process, a lateral image with a downward displacement of the labyrinth (according to Lysholm) and a lateral image with an anterior displacement of the labyrinth (according to Lange-Sonnenkalb). All these projections are two-stage, with the first image being a modification of the Stenvers oblique projection, and the second and third ones resembling the lateral projection of the temporal bone according to Schuller.
Description of the X-ray examination
The study of the temporal bone cannot be considered exhaustive without mentioning the diagnostic value of stereography and tomography. Stereoradiography can be performed in all of the projections listed above, but is usually limited to the typical lateral and axial ones. The ear stereography technique is relatively simple, but it still requires some devices for precise centering when moving and converging the X-ray tube, which include centralizers with an optical device. Stereoradiograms, when viewed in a special stereoscope, give good spatial representations of the location of the cells of the mastoid process and the state of their septa, the size of the antrum, the position of the sinuses, etc. With the development of the method of layer-by-layer research, the practical importance of stereography is significantly reduced.
Indications for the procedure
If the slightest suspicion of disease in the jaw and face area is detected, it is recommended to conduct an examination of the temporal bones or the extended protection - X-ray according to Schüller. Mayer's X-ray is usually recommended if it is necessary to view the mastoid cave or antrum. This method is a narrower method of examination. The examination is performed at an angle of 45 degrees, since the analysis represents axial protection of the auditory organ.
When is it necessary to conduct an X-ray examination of the temporal bones (X-ray according to Schüller):
- inflammatory process of the middle auditory region in an advanced phase;
- acute otitis with consequences;
- trauma to the auditory organs;
- cholesteatoma;
- benign or malignant formations;
- inflammatory process of mastoid cells.
Doctors advise carrying out this research method after surgical resolution of diseases of the auditory organs. The procedure will help to identify changes in the ear and assess their condition after the intervention.
Purulent otitis.
When is the examination scheduled?
X-rays of the temporal bones may be prescribed if the following indications exist:
- bruises, blows, injuries, temporal bone fractures;
- ear diseases: acute otitis with complications, chronic inflammation of the middle ear, cholesteatoma and others;
- suspicion of tumor growths in the temple area.
Today, CT and MRI are more effective and safe techniques than x-rays. This is why there is such a narrow range of indications for x-rays. However, this study helps to reliably identify the presence of pneumatization in a patient (in other words, cavities filled with air), as well as to study the position of intra-ear implants.
X-rays are also prescribed for other indications, when CT and MRI machines are not available in the medical institution.
How the research works
Before carrying out an x-ray examination, it is important to find a professional specialist. Usually people do this based on the advice of relatives and friends. Many people believe that in an expensive clinic, X-rays are done better than in a municipal medical institution. This judgment has logical confirmation, since private hospitals have better and more modern equipment. But this does not affect the professionalism of the staff. Sometimes doctors in city clinics are more competent than in expensive hospitals.
How is an X-ray examination performed?
- The patient lies on his stomach.
- Turns his head in the direction that will be examined.
- The hand should be clenched into a fist and placed under the chin (thanks to this position, the head will be clearly fixed).
- Place your free hand along your body.
- During exposure to x-rays, the person should not move.
Before the event, you should remove all accessories consisting of metal. The event lasts on average 2-3 minutes. This stage of diagnosis should not be postponed, since thanks to its results it is possible to promptly identify the presence of pathology and begin to eliminate it.
X-ray of the ear with otitis.
How is an ENT x-ray performed?
X-ray examination of the ENT region is carried out in a special diagnostic room using an X-ray machine. The designated area is examined according to the same rules as other parts of the body. The patient is asked to take a sitting or reclining position. The picture is taken in two projections (frontal and lateral). Less often, it is necessary to take a picture with additional overhead projections.
The procedure itself requires very little time. Preparation for the image lasts no more than 20 seconds (positioning the patient, fixing the installation). It takes even less time to take a photo (2-5 seconds). It takes a specialist a few minutes to print and decipher the result.
X-ray is a very quick, painless and informative way to diagnose serious pathologies.
Diagnostic quality and safety
It is no secret that the latest generation of medical equipment models compare favorably with the medical equipment of previous years.
Modern X-ray machines allow you to obtain highly accurate results and minimize the harmful effects of X-rays on the human body.
Thanks to the use of top-level medical equipment, the study in question was completely safe and effective.
Today, X-ray examination of the ENT organs does not cause any concern for patients and is considered one of the best diagnostic methods among specialists at various levels.
Decoding the results
X-ray images are prepared within 1 day. If the result is high-quality, the doctor determines the pathological conditions that have arisen.
What diseases are detected using x-rays?
- If the patient has acute otitis, the transparency in the area of the middle ear, as well as the cells of the mastoid process, will be reduced.
- In acute mastoiditis, pneumatization of the mastoid cells will be reduced or completely absent.
- Foci of bone tissue destruction signal advanced otitis media.
- If the mastoid areas are darkened, this may indicate purulent inflammation.
- Cholesteatoma is determined by the enlargement of the cave area.
- Large-scale formations are visible on their own in the image.
X-ray examination is recommended for all patients. This method accurately identifies pathological changes and conditions in the ear.
Indications
X-rays of the nose and paranasal sinuses are prescribed if the child has:
- Headache.
- Increased body temperature.
- Nasal congestion, impaired nasal breathing, especially in children, and associated changes in voice.
- Disturbance in the growth of the facial skull ─ with difficulty in nasal breathing and a constantly open mouth, a peculiar appearance of the child is formed: the face is elongated, the upper jaw is elongated, the upper teeth protrude forward, the mouth is half-open.
Typical signs of adenoid face in a child
- Snoring, sleep disorders.
Contraindications to the procedure
X-ray examinations are scary for many people, usually because the person receives a small amount of radiation - 0.12 m3v. It is susceptible to the same irradiation when exposed to the sun for one hour. On average, the radiation dose a patient receives during testing is within normal limits. Even such exposure is contraindicated for some patients. This is one of the contraindications to the procedure.
Who should not undergo X-ray examination:
- pregnant women (even a small dose of radiation can affect the development of the fetus);
- patients with cancer;
- open tuberculosis;
- pathology of the thyroid gland;
- liver diseases.
The only absolute contraindication to x-ray examination is pregnancy. The analysis is prescribed to pregnant women only when absolutely necessary. In other cases, the procedure is carried out with extreme caution.
Pregnancy.