April 26, 2020 mrt Home page » MRI and CT of joints Views: 4356
The hip joint is the largest joint in the body and bears a very large load of a person's weight. Due to constant stress and traumatic influences, degenerative-dystrophic, inflammatory and tumor processes can develop.
CT scanning of the hip joints is an informative and reliable diagnostic method that allows doctors to visualize and evaluate changes and pathologies in this area. The CT method is based on layer-by-layer scanning with X-rays, the results of which, after computer processing, specialists obtain images of the area under study in longitudinal and transverse projections. Thanks to this opportunity, it is possible to obtain data on the condition of difficult-to-diagnose areas of the body.
What does a CT scan of the hip joint show? Computed tomography of the hip joints makes it possible to obtain images not only of the joint itself, but also of all the tissues surrounding it. On CT scans of the hip joint you can see:
- upper part of the femur
- ilium
- surrounding soft tissues.
When performing a computed tomography scan of the hip joints, specialists are able to measure the circumference of the joint, the distance between its articular surfaces, determine the location of bone fragments in comminuted fractures, and detect foreign bodies. Obtaining such data helps to prescribe the optimal treatment method.
CT scan of the pelvic bones allows us to detect the presence of various pathologies and changes:
- tumor formations of various nature (benign or malignant) of bones and tissues
- degenerative changes
- consequences of injuries and damage (fractures, sprains, bruises, hematomas, ruptures of ligaments and tendons)
- inflammatory processes
- arthrosis with thinning of cartilage tissue
- arthritis
- osteomyelitis.
In cases where the changes in the joint are minor and it is difficult to distinguish normal from pathology, tomography of both joints is performed to compare them.
Patients are referred to a CT scan of the pelvic bones before surgical interventions, for subsequent assessment of the dynamics of the disease and to determine the effectiveness of the prescribed treatment.
Detectable pathology
Traumatic changes
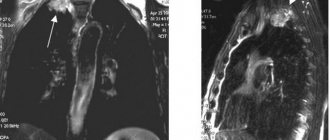
There are fractures of the neck, head of the femur, pertrochanteric fractures, and fractures of the roof of the acetabulum. CT allows one to evaluate the location of the fracture line, displacement, size and number of bone fragments, and the presence of complications.
Injuries are sometimes observed in the context of osteoporosis or the presence of space-occupying lesions that weaken the bone structure. These are cysts, hemangiomas, metastases and other tumors.
Inflammatory changes
Most often, osteomyelitis is a complication of injury and (or) surgery.
- An area of rarefaction of bone tissue (a cavity filled with pus) is detected, against which dense bone inclusions - sequestra - are visible.
- Often fistulous tracts are detected that open in the muscles, subcutaneous tissue, and skin.
Other changes are osteosclerosis, hyperostosis, linear (layered) periosteal reaction. In the soft tissues near the inflammatory area in the bone, hypodensity zones (abscesses) may be detected.
Degenerative changes
Manifestations of arthrosis include uniform or uneven narrowing of the joint space, sclerosis of the subchondral bone, subchondral cysts, and osteophytes. Sometimes concomitant exudative synovitis is detected - excess fluid in the joint cavity.
Arthrosis is divided into 4 stages according to Kellgren or 3 stages according to Kosinskaya. Stage 1 - minimal changes, stage 4 according to Kellgren or stage 3 according to Kosinskaya - final degenerative changes.
Arthrosis and injuries are often combined with aseptic necrosis - the death of bone tissue due to impaired blood flow.
Structure violations
Osteoporosis is a serious pathology manifested by bone loss:
- the number of trabeculae per unit volume decreases;
- the partitions become thinner;
- cortical plates become thinner.
Causes of osteoporosis: old age, hormonal imbalance, malnutrition, immobilization (bed rest, immobilization).
Osteochondropathies
Legg-Calvé-Perthes disease is typical for children during the growth period, especially against the background of regular physical activity.
- The basis is a violation of blood flow in the ossification nucleus of the femoral head, its necrosis and impression fracture.
- In the acute phase, heterogeneity in the structure of the nucleus is detected. During the fracture phase, the height of the core decreases—it “flattens.”
- In the phase of structural restoration, fusion begins, the formation of new bone tissue. The head of the femur becomes deformed to take the shape of a club.
Tumors of cartilage and (or) bone tissue
- Tumors of bone tissue: osteoma, osteosarcoma.
- From cartilage tissue: chondroma, chondroblastoma, chondrosarcoma.
- Mixed: osteochondrosarcoma, osteochondroma.
Secondary tumors (metastases) also occur. Osteoma, chondroma are benign formations. Sarcomas are malignant.
For example, consider osteochondroma, a mixed tumor.
- Occurs near the articular surface of the tibia, fibula, or femur.
- It has a mixed structure.
- The shape of the tumor is irregular; in many cases, a stalk and a cartilaginous “cap” are found.
- Size from a few millimeters to 10 cm or more.
Post-operative changes
Patients with femoral fractures undergo osteosynthesis. Cervical screws, L-shaped plate, intramedullary nail, and gamma nail may be detected. It is important to assess the integrity of metal structures and determine the presence of areas of bone tissue destruction against the background of metal.
Hip replacement can be partial or complete. In the first case there is only a femoral component, in the second there is a two-component prosthesis. The femoral component of the prosthesis is always made of metal, the acetabular component is always made of metal or plastic.
Contrasting
Contrast, intravenous or intra-articular, is used very rarely. Most often, in practice, the introduction of contrast is not necessary.
Even bone tumors appear obvious and do not require contrast to confirm the diagnosis. Intravenous contrast can sometimes be used to differentiate soft tissue abscesses.
Preparing for the study
Best materials of the month
- Why you can't go on a diet on your own
- 21 tips on how to avoid buying stale food
- How to keep vegetables and fruits fresh: simple tricks
- How to curb your sweet cravings: 7 unexpected products
- Scientists say youth can be extended
Specific preparation is needed only when conducting contrast diagnostics. The patient must refrain from eating food 6 hours before the CT scan. This is necessary to minimize side effects. Moreover, the contrast agent will spread faster and more efficiently through the “clean” gastrointestinal tract. In addition to refusing to eat, the patient must choose comfortable and safe clothing. These should be simple pants/T-shirt made of natural or synthetic fabric without metallic decorative elements. Metal particles can distort the image, leaving empty white spots in the final 3D image.
How the research works
All metal objects are removed from the scanning area.
- The patient is placed on the tomograph table with his feet or head facing the gantry.
- Tomograms necessary to mark the study area are performed.
- Then a helical or incremental scan is started.
- During the examination, various voice commands may be given and must be followed.
- The data is transmitted to the radiologist's station, where it is processed using software.
The doctor analyzes the data obtained and makes a conclusion about normality or pathology.
How is the diagnosis carried out?
During a CT scan of the pelvis, the patient lies on the machine table. The area to be examined is located under a scanning ring, which rotates and sends pulses through the body. There will be some noise from the equipment during the procedure.
The examination progress is observed through glass by staff in the next room. There is also a computer there that receives data from the tomograph. The doctor can see what the device shows and assess the condition of the joints and blood vessels during the process.
With contrast, diagnosis takes about 20 minutes, without the drug - no more than 5.
Decoding the results
The conclusion is written by a radiologist. It consists of a narrative, a short summary, and recommendations. Along with the conclusion, a disk with the original data recorded on it is issued. Film may also be dispensed.
Having received the conclusion, you need to follow the recommendations of the radiologist. For example, with severe arthrosis, it is necessary to visit an orthopedic traumatologist to prescribe treatment (including completing documents for prosthetics).
Benefits of CT
Of course, this diagnostic technique is quite effective and allows you to examine the most inaccessible areas and areas. In this case, each area is viewed at high magnification, which does not affect the clarity of the image.
Another advantage of this method is that it is possible to examine with maximum accuracy not only bone structures and joints, but also the soft tissue surrounding them.
The advantages also include patient comfort; everything is painless for the person and does not cause him any inconvenience.
If this procedure is performed once, it is safe and cannot harm human health.
Possible complications
There are complications associated with exposure to ionizing radiation and the use of contrast.
- In the first case, there is a risk of developing tumor pathology in children and a negative impact on the fetus in pregnant women.
- In the second - the risk of allergies, shock, swelling of the respiratory tract, renal failure, extravasation, phlebitis.
Execution frequency
The study can be performed as often as required. Radiation exposure during pelvic examination is on average 2-5 mSv. A dose of 1 Gy (1000 mSv) is required to cause acute radiation sickness. At the same time, the younger the patient, the higher the risk of delayed development of cancer.
Attention: the risk of developing pathology from radiation during diagnostic procedures in adults is almost zero.
CT scan of the hip joints in children
Children, especially younger ones, are most susceptible to radiation. They need significant reasons to carry out the research. These are trauma, tumors, inflammatory lesions, osteochondropathy. Radiography is better suited for diagnosing congenital dislocation.
Caution: Young children need to be distracted. Bring toys, a tablet or phone with cartoons.
Contraindications
If the examination is carried out without the use of injections with contrast, then there is only one contraindication - pregnancy. However, in some situations, even a pregnant woman may be prescribed hip imaging. In this case, the specialist will cover the abdomen with a lead blanket to provide maximum protection to the fetus and maternal body from x-ray radiation.
If the disease is carried out with contrast, then there will be more prohibitions on the examination. CT scanning is not recommended for patients with the following pathologies:
- Heart failure.
- Kidney failure.
- Allergy to iodine.
- Endocrine system disruption.
Other Imaging Techniques
Most often used:
- radiography: diagnosis of bone trauma, arthrosis, congenital hip dislocation;
- sonography: diagnosis of joint diseases in children and adults;
- MRI - the information content is generally higher compared to CT;
- nuclear medicine - in oncopathology, to search for tumors.
CT or MRI?
Computed tomography is an X-ray method that best shows the pathology of bones, then soft tissues. The method is associated with radiation exposure, as a result of which its use is limited in children and pregnant women.
MRI is more suitable for visualizing ligaments, muscles, and other soft tissues. On MRI, trabecular edema is clearly visible, which is why this method can also be used to diagnose bone injury.
General principle: CT is more suitable for emergency patients with trauma in a hospital, MRI is more suitable for diagnosing chronic diseases (arthrosis) in a clinic.
Operating principle of CT and MSCT
It is not easy to see the femurs, as on a regular x-ray, but the computed tomography technique allows you to examine them layer by layer.
Parts of the human body located in the area of influence of the tomograph absorb X-rays, which is recorded by the device. Tissues that differ in density and structure (bones, muscles, cysts, tumors) will appear differently in the resulting images.
By entering the human body from different angles, ionizing radiation makes it possible to build an accurate layer-by-layer model of the area under study. After computer processing, the data turns into a full-fledged image.
On the display that subsequently appears on the monitor of the unit, each type of tissue, bone, cartilage, ligaments, etc. is a separate entity from others. The picture is printed on X-ray film or recorded on a disk, with which the patient will go to an appointment with the doctor who scheduled the examination.
Thanks to advances in technology, the images obtained from tomography are merged into a three-dimensional model of the individual patient's joint. She provides invaluable assistance to surgeons preparing for surgery.
Stages of CT diagnostics of the hip joint
The joint area is scanned using a tomograph. The device is located in a separate office, one wall of which has a glass window. Through it, the progress of the procedure is monitored by the specialists responsible for the tomography. The examination takes place in several stages:
- the patient is positioned on the tomograph couch;
- for complete immobility, the hip joint area is fixed with belts;
- the couch with the patient smoothly moves into the device so that the joint area falls under the “sight” of the tomograph;
- if necessary, contrast is administered intravenously (single or bolus - through a syringe injector in which the rate of constant supply of the drug is adjusted);
- staff leaves the room and observes the procedure remotely;
- the doctor turns on the tomograph, the ring of which begins to rotate;
- The doctor controls the filming process; two-way communication is provided for contact between him and the patient;
- if the patient's condition worsens or there is a suspicion of an allergic reaction after the administration of contrast, the scan is stopped and medical attention is provided;
- the result of the examination is a tomogram, which is deciphered by a radiologist or a functional diagnostics doctor.
Indications
Computed tomography of the hip joint allows us to identify anomalies and pathologies at the earliest stages of their maturation. It is prescribed for suspected cases of the following diseases:
- formation of cracks in the bone area;
- arthrosis of the hips;
- arthrosis of the hip joint;
- fractures (inside the joints or in the femoral neck);
- any ligament damage;
- tumor formation.
As a result of the examination, the disease will be confirmed or refuted, the affected area and the stage of development of the disease will be identified. Depending on what the CT scan shows, the specialist can decide on the treatment method for the patient.