Ultrasound of peripheral nerves
is one of the predominant methods for studying diseases in neurological practice. Ultrasound diagnostics allows, without any harm to the body, to assess the state of the peripheral nervous system in order to timely identify pathological processes.
Moreover, this technique, in case of detection of damage, allows us to determine its cause and location, as well as the nature of the changes occurring. This is an undoubted advantage over other types of examinations. The advantages also include the safety and painlessness of the procedure, the absence of contraindications and a reasonable price.
In the paid services department of our clinic, ultrasound of the peripheral nerve
It is carried out using modern high-tech equipment, which, together with extensive experience and highly qualified doctors, guarantees you a competent examination and an accurate diagnosis.
When is it prescribed?
At the beginning of a pathological process occurring in the peripheral nervous system, studies are not always effective.
Reference! Some violations do not reveal themselves for a long time and appear only during examination using high-precision medical equipment.
Other pathologies, for example, shooting of the ulnar or sciatic nerve, are rarely taken seriously by the patient until the pain becomes unbearable and regular.
What symptoms are determining for a doctor who prescribes an ultrasound of peripheral nerves? There is a whole list of them:
- feeling of numbness in the limbs, disruption of their function;
- shooting pains;
- detected neoplasms in the projection of the trunks;
- foot paresis;
- burning sensation;
- any injuries that negatively affect the sensitivity of individual parts of the body or general motor activity;
- for visual assessment of the degree of dissection of the suspensory ligament of the carpal tunnel, if there is no improvement for a long time after decompression surgery;
- with benign fibrous tissue growths, for example, with Morton's neuroma;
- experiencing any extremely traumatic situations, including accidents;
- suspicion of tumors of any etiology.
Symptoms
The main symptom of a pinched sciatic nerve is pain. It begins in the buttocks and spreads along the back of the thigh all the way to the knee and ankle. Depending on the location and degree of pinching, the sensations can be sharp and sudden or aching that does not subside for a long time.
If the pinching occurs in the area of the spinal column or hip joint, the pain is aching in nature and intensifies when walking, squatting, or bringing the legs together.
When pinched in the piriform aperture, a person notes:
- dull pain over the entire surface of the thigh;
- a feeling of chilliness or burning of the skin in the affected area;
- decreased sensitivity in the back of the thigh and in the Achilles tendon area;
- sweating of the feet, feeling of heat in the toes.
If one of the large arteries passing through this area is pinched along with the nerve, the patient will experience a symptom of intermittent claudication. When walking for a long time, pain occurs in the leg, accompanied by numbness of the fingers and pale skin in this area. The sensations go away on their own with rest. Mild dysfunction of the pelvic organs often develops, in particular, a pause before urination.
Symptoms intensify when walking, as well as in a sitting position.
What are they watching?
Ultrasound examination allows you to examine in detail the peripheral structures, and, first of all, the key nerves of the upper extremities:
- trunk and fibers of the radial nerve;
- median and brachial nerve bundles;
- carpal, musculocutaneous and axillary nerves;
- finger flexors.
In addition, with great difficulty, one can obtain information about the nerves of the lower extremities. For example, determine the structure and localization of the following nerve endings:
- ischial and femoral;
- lower and upper gluteal;
- obturator and genital;
- iliogastric and inguinal;
- greater and fibula;
- plantar and medial cutaneous nerve of the foot.
Reference! The difficulty of examining individual nerve structures (for example, femoral, sacral and lumbar nerves) lies in their deep location.
These groups of nerves are deepened into soft tissues and hidden by bone elements. Therefore, an ultrasound sensor cannot always provide high-quality visualization.
Preparation
When preparing for sonography of the peripheral nervous system, there are no specific preparatory measures. However, before the procedure, you should discuss your symptoms in detail with your doctor. .
Important! Based on the patient's complaints, the doctor may prescribe additional examinations, including laboratory tests, for example, neurological tests or tests.
If there are skin lesions at the site of the proposed examination, the procedure should be postponed until they are completely healed.
Prevention
To prevent pinching of the sciatic nerve, doctors recommend:
- normalize body weight;
- avoid carrying heavy objects;
- avoid hypothermia;
- watch your posture;
- regularly engage in sports at an amateur level to strengthen muscles, swimming has a particularly good effect;
- minimize stress;
- eat properly and balanced without overusing fatty, smoked, spicy and canned foods.
If you experience discomfort and pain in the lower back or any other area, it is important to immediately consult a doctor and undergo an examination. Osteochondrosis and other pathologies are much more amenable to correction at an early stage of development.
How do they do it?
In order to obtain a clear and accurate image, the sonologist applies a gel to the skin that enhances the conductivity of the sensor. To examine the sciatic nerve, the doctor sets the frequency to 3-5 MHz. For the radial, ulnar plexuses and other peripheral nerve structures, the frequency changes and becomes equal to 7 - 15 MHz.
Ultrasound of peripheral nerve fibers takes place in several stages:
- First, the exact location of the object under study is determined.
- Secondly, the desired nerve is examined in the transverse and longitudinal planes. Moreover, assessing large nerve trunks is much simpler than searching and examining small branches. The fact is that during motor functional tests, small nerves may not be visible to the doctor.
general information
The sciatic nerve is the largest in the body. It is formed by branches of the spinal roots emerging from the spine at the level of 4-5 lumbar and 1-3 sacral vertebrae. The nerve passes through the piriformis foramen in the gluteal muscles and runs down the back of the buttock and thigh to the knee.
Most often, pinching occurs at the level of the lumbar spine, which is especially susceptible to the formation of hernias due to the high load when walking and sitting. Slightly less common is compression in the area of the piriform opening, which develops against the background of a sharp muscle spasm.
Make an appointment
Decoding
During the examination, the condition of the nerve trunk, its integrity and structure, the condition of the adjacent tissues and the clarity of the contours are determined.
All these parameters must be reflected in the study protocol.
If negative changes are detected in the structure of nerve fibers, the doctor indicates:
- what type of damage;
- compression zone and its degree;
- cause of stenosis and reduction in nerve diameter.
If a neoplasm is found, the doctor supplements the protocol with its description, which indicates the contours, structure, blood flow (or lack thereof), and interaction with adjacent tissues.
It is more advisable to begin examining the peripheral endings from the point of greatest identification of the nerve trunk. Then, moving in the near and far directions, assess the condition and functional characteristics of the nerve along its entire length.
Characteristic signs of nerves
There are several characteristic features that distinguish the image of a nerve from images of other anatomical structures:
- The transverse projection presents the nerve as a round or oval structure with a smooth contour, increased echogenicity and a heterogeneous internal component.
- The longitudinal projection demonstrates it as a linear formation with a smooth echogenic contour and regular alternation of stripes of different echogenicity. The thickness of the peripheral nerve structures can vary from 1 to 8 mm.
Examination of a healthy nerve reveals a homogeneous formation with high echogenicity . Therefore, normal nerve tissue is not clearly visible on ultrasound. But pathological changes in the nerves are accompanied by a decrease in echogenicity and thickening of the trunk. As a result, the changed area is identified by measuring basic parameters and detailed examination of the fibers.
Dynamic tests - studies of nerves under load - also Such procedures are often performed in conjunction with Doppler studies of blood flow in the area under study.
This is necessary to obtain a detailed picture of the work of the nerves and the participation of blood vessels in this work.
During these tests, movements should be unimpeded and free.
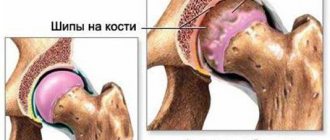
This is necessary so that if certain pathologies are detected, it does not cause pinched nerves (for example, with osteophyte).
Determining the location of compression
One of the tasks of ultrasound of peripheral nerves is to determine the location of nerve compression. To do this, several basic parameters are used:
- The degree of thickening in the place where compression is recorded. This parameter is calculated by dividing the maximum width of the nerve by its thickness. The normal value is 3.3 - everything that exceeds this figure is considered pathological.
- The area of the site with increased thickness. If it exceeds the accepted standard value, then this also indicates a pathological process.
- Reduced echogenicity and fibrousness of the nervous structure.
- Changes in the structure of the nerve, an increase in the thickness of its individual bundles.
Pathologies
During an ultrasound examination, the doctor examines the structure of the nerve bundles and can detect deviations from the norm, which may be a sign of a pathological process. For example:
- Inflammation - ultrasound can reveal inflamed areas of nerves that cause pain, numbness, decreased sensitivity and other unpleasant symptoms.
- Injuries to nerve endings - when dislocated or sprained, there is a risk of injuring the fibers. You can find out about the presence of an injury of this kind only with an ultrasound examination of the problem area.
- Post-traumatic conditions are diagnosed during the treatment of an injury associated with a bone fracture. Often a fracture is accompanied by a rupture (stretch) of the nerve. If we are talking about a rupture, then neuromas appear at the ends of the torn fiber - thickenings formed due to cell regeneration. Changes in the nerve structure can also appear due to the cutting of fibers during incised wounds or pinched nerves during a fracture.
- Pinching – unsuccessful movements, diseases of the musculoskeletal system or injuries of any kind can cause the formation of a compression area. Over time, the bone tissue in such an area is deformed, which is fraught with the formation of osteophytes - pathological growths on bone tissue. Pinching can also occur due to the development of a tumor - soft tissues can pinch the nerve structure.
- Tumors of various etiologies primarily affect the sheath of the nerve bundle, in this case they speak of the formation of a schwannoma or neurofibroma.
- Morton's neuroma is characterized by thickening of the interdigital endings due to the activity of the tumor process.
- Compression of nerve fibers - often caused by the placement of abnormally located vessels and muscles in the tunnels. It manifests itself as severe deformation of the nerve, the development of neuromas, and atrophy of altered fibers. On an ultrasound, the doctor observes thickening of the nerve structure and the development of carpal tunnel syndrome.
- Tunnel-type neuropathy – it is characterized by compression of nerve endings by tendons and bones. Typically found in people whose work involves computers.
- Diseases that cause pathologies of the nervous system. This includes a wide group of pathologies, from cysts and hematomas to injuries and thrombosis. Provocateurs are any conditions that can lead to compression of peripheral endings.
For any pathology of the peripheral nerves, an additional examination will be prescribed to clarify the final diagnosis. In addition to ultrasound, Doppler scanning and neuromyelography are often used.
Conducting functional tests is an important part of diagnosing neural structures.
For example, they make it possible to analyze the displacement of the sciatic nerve and surrounding tissues.
Based on similar tests, dislocation of the sciatic nerve is determined.
It is important to understand that this nerve can be constantly injured by nearby bones.
Causes
The list of causes of pinched sciatic nerve includes:
- osteochondrosis of the lumbar and sacral spine, protrusion and herniation of intervertebral discs; as a result, there is a narrowing of the spinal canal and compression of the roots that form the nerve;
- spinal injuries;
- postural disorders, scoliosis of the lumbar spine;
- diseases of the hip joint, especially arthrosis;
- myofascial pain syndrome: a sharp muscle spasm associated with severe pain, for example, due to a bruise or an unsuccessful injection;
- prolonged excessive stress on the pelvic muscles (for example, being in an uncomfortable position);
- inflammatory diseases of the pelvic organs, accompanied by a reflex spasm of muscle fibers;
- hypothermia;
- space-occupying formations in the area of the sciatic nerve: benign and malignant tumors, abscesses;
- pregnancy: infringement occurs against the background of pressure from the enlarged uterus on nearby structures.
The risk of developing entrapment increases significantly:
- against the background of excess body weight;
- with insufficient intake of minerals from food;
- for acute or chronic intoxication (salts of heavy metals, alcohol, drugs);
- with herpes zoster, which is localized in the area of the sciatic nerve.
pros
Ultrasound of peripheral nervous structures is a diagnostic method that is widely in demand in modern medical institutions. This method of examination has a number of positive aspects:
- financial inclusion;
- no radiation exposure;
- safety for all categories of patients;
- absence of contraindications and preparatory measures;
- the possibility of dynamic assessment of the condition of the problem area;
- the possibility of complex diagnostics in combination with other examination methods;
- good visualization of nerve fibers and endings;
- the ability to conduct examinations as many times as necessary and as often as the patient needs.
Advantages of the clinic
Energy of Health clinics offer each patient high-quality and affordable medical care, including:
- comprehensive screening programs to identify acute and chronic diseases;
- consultations with specialists of a wide and narrow profile;
- full range of laboratory diagnostics;
- modern methods of instrumental and functional examination;
- all types of drug and non-drug treatment;
- preventive measures to maintain the health of the body.
A pinched sciatic nerve can cause severe pain that interferes with normal movement and self-care. Do not try to treat it at home, seek help from Health Energy.
Minuses
Despite the fact that the diagnostic method of ultrasound has a lot of advantages, it is not without its disadvantages.
Undesirable aspects of ultrasound examination include insufficient passage of nerve impulses with an inconvenient location of the nerve for examination.
Therefore, it is not always possible to qualitatively examine the area of the peripheral nervous system that interests the doctor.
Thus, examination of the radial nerve trunk will be much more informative than examination of the tibial trunk. Inspection may be difficult:
- heavy weight of the patient;
- deep location of the nerve;
- the location of the bone structures covering the object of study.
In addition, ultrasound is a rather subjective method and this is its main drawback. The interpretation of the data obtained depends too much on the experience and qualifications of the personnel, as well as on the quality of the equipment.
What can untimely treatment lead to?
- It depends on the disease. If we are talking about banal back pain, then untimely treatment will lead to nothing, because 80% of back pain disappear spontaneously within 4 weeks. Another 10% disappears in 8 weeks, and only the remaining 10% will not disappear on its own.
I would say that incorrect treatment is more harmful here, that is, “dumb” pain relief, when instead of finding and removing the cause, a person takes painkillers. Pain is a defense mechanism developed by nature, and when we think that we are smarter than nature, it begins to take revenge on us.
Pain management increases the rate of destruction of our body, that is, we do not feel pain and do not protect our tissues.