Ultrasound for women is one of the main examinations necessary to diagnose the disease. If there are suspicions of problems in the pelvis, with timely diagnosis the disease can be successfully cured.
Examination of the female reproductive system requires a special approach
The need for the procedure
Ultrasound of the internal female organs is prescribed to:
- detect diseases of the female reproductive system at the initial stage;
- assess the anatomical structure of the uterus;
- assess the condition of the cervix;
- monitor the therapy being carried out;
- accurately diagnose a disease when it is difficult to define.
A doctor using an ultrasound scan checks the anatomical structure of the uterus
What does a vaginal ultrasound show?
This examination allows you to evaluate the following parameters of the reproductive system organs:
- Dimensions of the uterus. In normal condition, it should be about seven centimeters in length, six in width and 4.2 in diameter. If it is significantly less or more, then this indicates the presence of pathology
- Echogenicity. The structure of the organs must be homogeneous, uniform, have clearly defined, clearly visible edges
- General picture of internal organs. The uterus should be slightly tilted forward. And the fallopian tubes may be slightly visible, but should not be clearly visible without the use of a contrast agent
How to prepare for the procedure
It is worth noting that gynecological ultrasound for women can be performed in two ways: usually (through the peritoneal wall) and transvaginally. To conduct the study in the first way, a woman should prepare. Firstly, you must come to the procedure with a full bladder. To do this, it is recommended to drink approximately a liter of still water. Thanks to a full bladder, the uterus and ovaries are visualized more clearly, which simplifies the examination.
If the bladder is not filled enough, the image will not be as informative, which is why the diagnosis may be carried out a second time.
For a transvaginal examination, filling the bladder will not be necessary - the image will still be clear. Diagnosis is carried out if a detailed examination of the uterus and ovaries is necessary, or if there is interference with examination through the peritoneum. Often such an obstacle is excessive fat deposits. In this case, the sensor is inserted through the vagina and the image on the monitor is formed from the middle. Transvaginal diagnosis is often used in the early stages of pregnancy, including suspicion of an ectopic pregnancy.
Using the device, the doctor can check the condition of organs
Features of preparation
All of the above types of ultrasound in gynecology have their own distinctive features in preparation for the procedure:
- For the transabdominal method, it is important to prepare the intestines and bladder so that they do not block the necessary organs and structures. To do this, 2-3 days before the study, a diet is prescribed aimed at eliminating gas-forming foods (legumes, pasta, white bread, cabbage, cucumbers, rice, carbonated water, etc. are removed from the diet). The use of antifoam agents (Espumizan, Smecta) is justified. In this case, the last meal should not be later than 8 pm on the eve of the examination. The bladder begins to fill 1.5-2 hours before the first urge to go to the toilet.
- Preparation for a gynecological ultrasound through the rectum involves careful bowel movements using physical or pharmacological methods. In the evening and morning on the day of the study, a cleansing enema is prescribed, as an alternative - laxatives (Picolax, Duphalac) or suppositories. You also follow a diet and fill your bladder (drink 1-1.5 liters of regular clean water about an hour before the procedure).
- In order to perform a gynecological ultrasound through the vaginal cavity, there is no need for special preparation. The bladder does not fill, and the ultrasound diagnosis itself is carried out on the 3rd or 4th day of the new menstrual cycle.
Diagnostic methods
Such diagnostics are carried out by three methods:
- Transvaginal. Used to more accurately diagnose pathologies of the genital organs. It is carried out by introducing a specialized device into the patient’s vagina.
- Transabdominal. This method is used to examine a virgin or to detect gross pathology in the pelvic organs. The examination is carried out through the abdominal wall.
- Transrectal. The examination is carried out by inserting a sensor into the anus. The method is as informative as transvaginal examination. Rarely used, only for virgins.
Prevention of labia cancer
Regular gynecological examinations help prevent the development of labia cancer, which not everyone can avoid. It is also advisable to follow the recommendations of oncologists to reduce the risk of getting sick. Increased immune status protects well from cancer, for which it is recommended to lead a healthy lifestyle, which includes:
- • moderate physical activity, hardening;
- • absence of bad habits (alcohol consumption, smoking, drug addiction should be excluded);
- • diet and proper diet with foods rich in vitamins, microelements, and plant fiber;
- • proper sleep and rest (it is better to avoid stressful situations and overwork, which, according to psychosomatics, provoke cancer);
- • genital hygiene;
- • maintaining normal weight;
- • absence of promiscuity.
Carrying out the procedure
Transabdominal diagnosis is carried out as follows:
- The woman lies face up on the couch.
- The doctor applies a special gel product to the skin.
- Then the doctor moves the device along the abdominal wall.
Different sensors are used for different types of ultrasound
Transvaginal examination is carried out as follows:
- the patient is positioned on the couch with his legs slightly spread;
- the doctor places a condom on the examination device;
- the sensor is inserted into the woman's vagina.
To carry out such diagnostics, you can purchase a special sterile condom.
Transrectal examination is carried out by analogy with transvaginal examination. The only difference is that the examination device is inserted into the woman’s anus. In this case, the patient should lie on the couch on her side.
During the diagnostic process, the nurse keeps a protocol, which records all the information voiced by the doctor.
Treatment of labia cancer
Surgery allows you to defeat labia cancer and stop the oncological process. During surgery, the surgeon’s actions are aimed at resecting the lip and surrounding tissues. Contraindications to resection are the detection of secondary lesions in distant organs and the serious condition of the woman.
Surgery is supported by radiation and chemotherapy, the purpose of which is to slow down metastasis. In case of advanced cancer, combined operations are used with removal of the uterine appendages, after which cytotoxic drugs are prescribed that affect cancer cells throughout the body. This approach allows you to achieve good results at stages 1–2. Recurrence of cancer, or relapse, is observed in 30% of women after clinical remission.
Recovery at stages 3–4 is observed in only 18–20% of cancer patients. To help alleviate the patient's condition if labia cancer is incurable, the prescription of symptomatic medications and pain relief helps. Effective painkillers, narcotic and non-narcotic analgesics, should be taken continuously.
Standard indicators on ultrasound
To begin with, the transcript of the ultrasound of the female genital organs indicates the size of the uterus. The standard distance between the fundus of the uterus and the internal os of the cervix is 5-8 cm. On average, this distance in a healthy nulliparous woman is 60-71 mm. In female representatives who have given birth, the uterus enlarges slightly; in this case, its size is determined by the number of births.
After studying the ultrasound readings, the doctor can draw a conclusion about the woman’s health
The thickness of the uterus should be 30-40 mm, and the width - 45-60 mm. A few years after reproductive function fades away, the uterus may decrease in size to 40-50 mm. When assessing the health of a woman’s genital organs, it is important to take into account the location of the uterus.
The normal location is in the center of the pelvis with a slight deviation towards the peritoneum. Such a position in the act of research is designated as “anteflexio”. “Retroflexio” is a physiological anomaly in the location of the uterus (the uterus deviates backwards), namely “bending”. The term “lateroflexio” refers to the deviation of the body of the uterus in relation to the center of the body.
When assessing the location of the uterine body, it is necessary to take into account that due to a full bladder, it may deviate slightly from the norm.
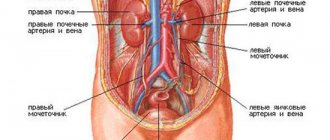
Condition of the appendages
The cervix on the echogram is determined as a formation of 2-3 cm, in the shape of a cylinder, the echogenicity is similar to the uterus. Normally, the width of the cervical canal should be 0.3-0.4 cm. The ovaries on an ultrasound image are visualized as an oval-shaped formation located on both sides near the uterus. The ovaries should be 27-37 mm in length, 21-29 mm in width, and 17-21 mm in thickness.
During an ultrasound, the doctor examines the ovaries very carefully
The ovaries can vary in size, since when the follicles grow, the ovaries also enlarge. When a dominant follicle is released, which is determined during the first phase of the cycle and continues to grow vigorously until days 12-14 of the cycle, the others become smaller again, and the ovaries return to normal size.
By the time of ovulation, follicles can grow to 15-29 mm, so they can be easily identified by ultrasound examination. When visually assessed by size, one ovary should be no more than 1/2 the size of the uterus in width. It is impossible to determine normal sized fallopian tubes using ultrasound. At the end of ovulation, the corpus luteum, a temporary hormone-producing gland, begins to form, the main purpose of which is to ensure implantation of the embryo and maintain pregnancy.
The corpus luteum is visualized as a small formation with a heterogeneous thick wall and fluid inside.
The endometrium in the uterus during the first days of the cycle is determined in the form of a heterogeneous structure with different thicknesses (3-8 mm). By the end of menstruation (4-5 days of the cycle), the endometrium is 2-4 mm thick, so it is almost invisible on ultrasound. During the early stage of proliferation (6-7 days of the cycle), a slight increase in the size of the endometrial layer is determined up to 6-9 mm, and in parallel the echogenicity decreases.
The doctor pays special attention to the condition of the endometrium
At the same time, it is easy to determine the emerging thin echo-negative contour up to 0.1 cm in thickness. By day 10, the endometrium increases in thickness to 10 mm. During the secretory phase (15-27 days), and during menstruation, the endometrial layer thickens significantly (in some cases up to 15 mm), this is visualized on an ultrasound image as a thickened reflective surface inside the uterus.
It should be noted that the detected corpus luteum and thickened endometrial layer in the first days of menstruation, if there is no embryonic egg in the uterus, may indirectly indicate an ongoing ectopic pregnancy.
Diseases and gynecological ultrasound
When a doctor suspects a woman has a certain disease, he needs visual information about the location of the pelvic organs, their size and defects. Ultrasound examination allows you to identify a number of diseases quickly, efficiently and informatively. The uterine cavity and ovaries are in a special risk zone for the female internal organs of the small pelvis.
Endometriosis is one of the most common women's health problems. With this disease, the tissue of the uterine cavity, the endometrium, grows into it and spreads to other organs. The danger of endometriosis is that in 30% of cases it leads to infertility. Endometriosis can also cause the appearance and growth of adhesions, and cause uterine fibroids. Usually, to identify the problem using ultrasound, the study is carried out in the second part of the menstrual cycle. It is at this time that the uterus increases in size and its defects become more noticeable. During the development of endometriosis, women often experience bleeding between periods, chaotic menstrual cycles, pain during sexual intercourse, and pain during urination. But at the initial stage of development, the disease does not manifest itself in any way. That is why ultrasound can promptly detect foci of proliferation and endometriotic formations in the form of ovarian cysts.
Uterine fibroids are the second most commonly diagnosed disease of the female genital organs. This is a benign neoplasm that appears in the uterine cavity. Large fibroids can have an extremely negative impact on the development of other pelvic organs.
The main symptoms appear during the menstrual cycle in the form of long and heavy bleeding. In this case, an ultrasound examination is performed immediately after menstruation. An ultrasound will show the doctor the number of fibroids, their size and location. Diagnosis of a benign tumor should be carried out at the first suspicion of it, because if the tumor reaches a large size, then the only way out will be surgery. Sometimes the uterus is completely removed along with the fibroids.
Diseases detected by ultrasound
Ultrasound of the genital organs determines the presence of:
- pregnancy – uterine, tubal, abdominal;
- deviations in the formation of the uterus and appendages;
- inflammatory processes in the uterus and appendages;
- endometriosis;
This method helps diagnose the presence of cysts in the ovaries
- hemo-, hydro- and pyosalpinx (accumulation of inflammatory or purulent fluids, blood in the fallopian tubes), and there is no precise differentiation of the form of abnormal fluids;
- complications after the birth of a child and abortion (for example, when parts of the fetus or its membranes remain in the uterus);
- neoplasms in the pelvic organs;
- polyps in the endometrial layer;
- fibroids in the uterus, its stages, what condition the myomatous nodes are in, how they affect uterine patency;
- cysts in the ovaries;
- torsion of the cyst stalk in the ovary;
- pathological fluid in the pelvic organs.
When using IVF, such diagnostics are used for dynamic monitoring of the condition of the uterus and ovaries, and during pregnancy it helps to monitor the formation of the child and the health of the mother’s organs.
In this video you will be told about the features of gynecological ultrasound:
Purposes of performing ultrasound of internal female organs
Using ultrasound scanning, it is possible to identify the following diseases and pathologies:
- uterine fibroids;
- oncological formations;
- cervical or ovarian cancer;
- pathological changes in the uterine tubes;
- formation of cysts in the ovarian area;
- formations of a benign nature.
Interpretation of ultrasound results is carried out by a gynecologist or obstetrician-gynecologist. The price of an examination in Moscow at the clinics of the Vash Doctor Group of Companies is calculated taking into account the method of diagnosis. You can check the cost yourself on our website or seek advice from specialists by phone.
Make an appointment
Factors leading to developmental disorders of the genital organs
In addition to abnormal levels of sex hormones (especially a large amount of testosterone in girls and a lack of it in boys) and chromosomal defects, the development of the genital organs in the fetus can be affected by hereditary and external factors. Anomalies occur due to certain genetic faults. The cause may also be infectious diseases of a woman during pregnancy.
Also factors affecting the development of the genital organs include:
- diseases of the endocrine system;
- unbalanced diet;
- taking certain medications.