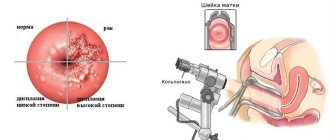
Colposcopy is a diagnostic method in which the cervix is examined in the vaginal part. The procedure is performed using a binocular microscope called a colposcope. In order to obtain the most accessible examination results during the examination, specific tests are additionally carried out.
If such a procedure is prescribed, do not panic. For the doctor, after a gynecological examination, this procedure is a confirmation of the identified diagnosis or dysfunction. Before the event, it is necessary to properly prepare, because the accuracy of the examination depends on this.
What is the cervix?
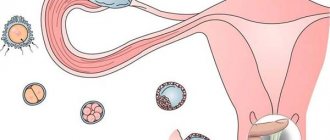
The cervix is one of the constituent parts of the female genital organs. It is not only an important functional, but also an anatomical element. This is primarily due to the presence of cellular composition.
In the area of the cervix there is a junction of several epithelial layers at once. Among them, the main ones are stratified squamous epithelium and columnar epithelium. The joint can be located in different parts of the cervical canal.
The cervix has a cylindrical shape, the dimensions should reach 3-4 cm in length. Its structure is homogeneous, without additional inclusions, and has a dense elastic consistency.
The cervix is divided into two main sections:
- External os. The external os is that part of the cervix that is the border with the vaginal cavity.
- Internal os. The internal os is the area that communicates with the uterine cavity.
Another component of the cervix is the cervical canal , which is the cavity for communication between the external and internal genital organs. It is through this area that infection and sperm can penetrate, and the fetus can also pass through at birth.
The cervical canal is the cavity in which epithelium meets in different areas. Normally, it is filled with thick mucus, which serves as a protective barrier.
Rating of the best gynecological colposcopes for 2020
Video colposcope Slv-101
A distinctive feature of this device is that it was created under the supervision of gynecologists. The device has many functions: convenient functionality, excellent optical capabilities, image magnification 250 times, clear image on the monitor, the design is quite flexible, it is unlikely to break. The examination is very thorough; even the slightest pathologies of the organs will be visible. By connecting to the monitor, the device archives all received data.
Video colposcope Slv-101
Characteristic:
- Colposcope type: digital/video.
- Allowable working distance: 7-9 cm.
- Image magnification: 25 times.
- Working time: 8 hours.
- Video camera: built-in.
- Illumination: 25000 Lux.
- Focusing: auto and manual.
- Average price: 330 thousand rubles.
Advantages:
- Multifunctionality;
- Clear image on the monitor;
- Excellent camera quality;
- Large working distance.
Flaws:
- High price.
Alscope
A binocular apparatus equipped with a video camera, a green filter for better contrast, an excellent optical system, a high-quality examination of the genital organs. This is one of the most popular models on the European market. This device is also multifunctional: a video camera, image recording, a good optical system, data processing on the monitor is possible. The monitor is large enough, images are shown in high quality, thanks to the green film, the contrast is seen better and even minor pathologies are visible.
Alscope colposcope
Characteristic:
- Type of colposcope: binocular.
- Allowable working distance: 7 cm.
- Image magnification: approximately 15 times.
- Working time: 8 hours.
- Video camera: built-in.
- Illumination: 25000 Lux.
- Focusing: auto and manual.
- Average price segment: 470 thousand rubles.
Advantages:
- There are useful additional functions;
- Good optical system;
- Clear image on the monitor.
Flaws:
- High price.
Dafina
Quite a popular model in the field of medicine. The producers did their best. Multifunctionality, high-quality materials, convenient use, image clarity. This device will help examine the cervix, lower third of the cervical canal, vagina and vulva. Good illumination, represented by a fiber-optic LED light source. If you have a disease in the lower third of the cervical canal, you should be examined with this particular device, because its accuracy is quite high. It is possible to connect to a computer to save and process data. The company has added many useful features that make work easier and more convenient. Reviews from gynecologists are positive.
Dafina colposcope
Characteristic:
- Type of colposcope: digital video colposcope
- Allowable working distance: 20-40 cm.
- Image magnification: 5-7 times.
- Working hours: 8 hours.
- Camera: built-in.
- Illumination: 3000 Lux.
- Focus: auto, manual.
- Average price segment: 120 thousand rubles.
Advantages:
- Low price;
- The price corresponds to the quality;
- Positive feedback from customers;
- Many useful functions;
- Convenient to use.
Flaws:
- Not identified.
KN-2000-C
The brand has released a whole series of gynecological devices, including this colposcope model. In general, this company released 3 models of this device, and each of them is unique and individual in its own way. Sturdy tripod, easy to set up. During the diagnosis, the patient will not feel any discomfort; on the contrary, he will feel comfortable. When diagnosing diseases, it is never superfluous to check the vessels so that you can see them; the device has a special green filter that will help with this. The binocular stereoscopic head will help you variably magnify the image.
KN-2000-C colposcope
Characteristic:
- Type of colposcope: video colposcope.
- Allowable operating distance: 10 cm.
- Magnification of the picture: approximately 12 times.
- Working time: 8 hours.
- Video camera: built-in.
- Illumination: 2500 Lux.
- Focus: Varies by model.
- Average price segment: 100 thousand rubles.
Advantages:
- Low price;
- The product is made of quality materials;
- The patient feels comfortable;
- Ease of use.
Flaws:
- Not identified.
Vesta C-3100
This digital video colposcope has the ability to connect to a local network. All received information can be transferred to an electronic medium and the data can be archived on it. All data obtained from patient research histories will be saved, but in a certain quantity, the limit is about 3000 stories. This device is also capable of connecting to the Internet and transmitting data. Ease of use lies in the fact that the device will tell you how to use and what to press. Of course, the device has a green filter, image processing and video recording. The program for the device will come with it, as well as a video camera and a fairly strong tripod. To archive, view or process data, you will need to connect to a computer.
Vesta C-3100
Characteristic:
- Type of colposcope: digital.
- Allowable working distance: 7-10 cm.
- Magnification of the picture: 21 times.
- Video camera: built-in.
- Illumination: 2500 Lux.
- Focusing: auto and manual.
- Average price segment: 380 thousand rubles.
Advantages:
- Many useful functions;
- Ease of use;
- Positive feedback from customers.
Flaws:
- High price.
Colposcope KS-01
According to buyers, this is the best colposcope. The device was made in Russia and was distinguished by its quality, accuracy and good illumination. Good illumination will help improve the quality of research and diagnostic efficiency; it is represented by a halogen light source. The big advantage is that the doctor can easily and simply use it during the operation. The device weighs quite little, so it will be easy to move in the office. When connected to a computer, you can record all patient histories, archive the received data and further process them. But over time, the memory will fill up, we must take this into account. Upon purchase, the company will provide all documents for the device.
Colposcope KS-01
Characteristic:
- Type of colposcope: digital.
- Allowable working distance: 7 cm.
- Magnification of the picture: 31 times.
- Video camera: built-in.
- Illumination: from 2500 – 6000 Lux
- Focusing: auto and manual.
- Average price segment: from 140 – 175 thousand rubles.
Advantages:
- Despite the low price, the quality is excellent;
- Customer reviews are positive;
- High diagnostic accuracy.
Flaws:
- Not identified.
KS-02 mod. 051
Another Russian-made model. A distinctive feature of this device is its compact size. The device has maximum diagnostic accuracy. It doesn’t matter which genital organ or part of it needs to be examined, the colposcope KS-02 mod. 051 will be able to find any problem, for example, with diseases of the vagina or with diseases of the cervix. Often, when using a device, a lot of energy is consumed, but this model is more economical; it does not consume as much energy, unlike previous models. The device can also connect and work with a camera. The device has high optical characteristics. To view all received data, you will need to connect to a computer for analysis, archiving and processing. The model can be fixed in place using special clamps so that it cannot roll away anywhere. All documents and certificates are publicly available on the official website.
NKS-02 mod. 051 colposcope
Characteristic:
- Type of colposcope: binocular.
- Allowable working distance: 30 cm.
- Image magnification: more than 30 times.
- Power: 150 Volts.
- Illumination: 3500 Lux.
- Focusing: auto and manual.
- Average price segment: from 150 thousand rubles.
Advantages:
- The price corresponds to the quality;
- Positive feedback from customers;
- Excellent characteristic;
Flaws:
- Not identified.
Indications for colposcopy
Colposcopy is prescribed in the following cases:
- The main indication for colposcopy is a change in the cytological composition of cells. According to smears for oncocytology, changes in various types of dysplasia can be detected. These may be minor changes, or precancerous, or the presence of atypical cells.
- Inflammatory processes in the cervix, such as nonspecific or infectious cervicitis. It can be caused by a sexually transmitted infection, such as chlamydia, mycoplasma, ureaplasma, gonococcus, etc. As well as an inflammatory process that is caused by dysbiosis or inflammation in the vagina.
- The phenomena of endometriosis in the cervix or lower segment of the uterus, as well as transition to the vagina.
- The presence of condylomatous formations in the cervix.
- Detection of polyps in the area of the external os or cervical canal.
- in the cervical area that are suspicious or difficult to explain during a routine examination Conditions suspicious for malignant lesions of this area of the genital tract.
- Control examination after treatment.
- Examination of a woman as part of a medical examination.
- The presence of cases of spotting or contact bleeding after a gynecological examination, sexual intercourse or other conditions and the absence of changes in the uterine cavity.
Procedure and purpose of its implementation
Colposcopy is necessary for diagnosing gynecological diseases, in which the cervix is examined using a special optical device (colposcope), which magnifies the image several times. In this way, the doctor receives the most accurate information about the condition of the mucous membranes of the reproductive system.
Colposcopy is prescribed for erosion in cases where, as a result of a cytological examination, deviations from the norm were detected or anomalies were identified during examination on a gynecological chair.
Thanks to a colposcopic examination, it is possible to identify various diseases:
- erosive formations;
- endometriosis;
- endometrial dysplasia;
- the process of replacing multilayer epithelium with cells of the cervical canal;
- erythroplakia;
- HPV;
- changes in the structure of the cervix;
- cancerous and precancerous conditions.
Contraindications for carrying out
Colposcopy is a non-invasive method and carries few side effects. Among all contraindications, there are two main groups, including absolute and relative.
Relative
Relative side effects represent temporary removal from the procedure. This is due to the fact that at the moment the result obtained may not be sufficiently informative and lead to deliberately false results. After eliminating this factor, the procedure can be performed.
These include:
- The appearance of bloody discharge from the cervical canal. They may be associated with discharge from the uterine cavity or from the cervix. This can be either a disease or a condition of menstruation, as well as its residual effects.
- Clinic of acute inflammatory process in the cervix or vagina.
- Pronounced clinical manifestations of the strophic process in the mucous membrane of the external pharynx.
- Also, colposcopy cannot be performed within two months after natural childbirth . If delivery was carried out by caesarean section and there was no deciduosis clinic, then colposcopy can be performed a little earlier.
- Within a month after a medical abortion , as well as intervention in the uterine cavity.
- Within three months after surgical interventions on the cervix. This may be cryodestruction or diathermocoagulation. Vaginal examination, especially with speculum, is not recommended for several weeks. Within three months, complete tissue epithelization must occur, and a premature examination may result in a false result.
Absolute
Currently, absolute contraindications to colposcopy are:
- Cases of allergic reactions to any substances from the constituent components of the reagents.
- Adhesions in the vaginal area, preventing the removal of the cervix.
- Conducting radiation therapy to the lesion.
Possible consequences and complications after the procedure
Normally, after the procedure, a woman does not experience any unpleasant consequences.
However, sometimes after the end of the diagnosis the patient may experience the following conditions:
- Minor vaginal discharge. Not everyone experiences changes in vaginal discharge, but some women note an increase in vaginal discharge and an unusual color. The discharge is caused by the treatment of the mucous membrane with reagents, the remainder of which comes out of the vagina within a few days after the examination. There is no need to be alarmed if the discharge has a brown tint: its color is due to the reaction of the mucous membrane to chemical reagents. Such discharge usually goes away on its own and does not require additional treatment.
- Bloody discharge after examination. In rare cases (especially if there was an examination for erosion and a smear taken for oncocytology or a cervical biopsy), after the end of the procedure, blood may begin to be discharged from the genital tract. It is caused by damage to the vessels of the cervix. If the bleeding is minor and lasts for several hours, additional measures are usually not required. Bloody discharge is collected using a pad. However, if there is excessive bleeding after colposcopy, it is recommended to immediately consult a doctor.
- Discomfort or pain in the vagina and lower abdomen. Minor aching or nagging pain in the lower abdomen after colposcopy is normal. Usually they have virtually no effect on a woman’s well-being and do not limit her activity. But if after colposcopy your stomach hurts severely and the pain is sharp, acute or cramping, you need to consult a doctor.
- Mild vaginal discomfort that persists for 1-2 days after the examination is also normal. To cope with it, you can use the Gynocomfort restoring gel. This remedy eliminates irritation of the mucous membrane and promotes the rapid regeneration of microtraumas that appeared during the gynecological examination. The gel contains active components that have a pronounced antiseptic, antimicrobial, regenerating and anti-inflammatory effect. Thanks to this, when using the restoring gel “Ginocomfort”, vaginal discomfort is reduced, microflora is normalized, and damaged areas of the mucous membrane are quickly regenerated. According to clinical studies conducted at the Department of Dermatovenerology of St. Petersburg State Medical University named after. I.P. Pavlova, the product is well tolerated and does not cause allergic reactions. Gel “Ginocomfort” has the necessary quality certificates.
- Increased body temperature. This complication after colposcopy is quite rare. However, if you notice that your temperature has risen after the procedure, this may indicate the presence of an inflammatory process in the vagina or cervix. To avoid dangerous health consequences, you should consult a doctor.
What does colposcopy show?
Every woman needs to remember that colposcopy is not the final conclusion of the diagnosis. It can only serve as an additional diagnostic measure for subsequent invasive procedures.
Diseases:
- Consequence of the inflammatory process.
- Development of dysplastic changes.
- Suspicion of an oncological process.
- The presence of space-occupying formations, such as polyps or condylomatous growths.
There are two types of epithelium, based on changes in which the condition of the cervix is assessed:
- Cells of stratified squamous epithelium. These are cells that in their structure belong to epithelial tissues. They normally cover areas such as the vagina, as well as the outer part of the cervix. During extended colposcopy, these cells are not stained with iodine or vinegar.
- Cells of the glandular epithelium or, as it may also be called, columnar epithelium. Normally, these are cells of the mucous membranes located in the area of the uterine cavity and internal pharynx.
Much attention is paid to the junction of these sections.
What can the research “tell”?
In a normal state, the cervix has a smooth, even structure, with a shiny pink surface, under which evenly spaced blood vessels are visible. In the first half of the ongoing menstrual cycle, this surface is fixed in a pale pink tone, after which it acquires a cyanotic, bluish tone. In a nulliparous girl, the external pharynx has a round structure, while in a girl who has given birth, it is represented by a small slit.
The examination allows you to diagnose pathological processes in the cervix
Under the influence of acetic acid, the healthy upper layers of the epidermis become even lighter for a short period of time. After just 2 minutes it acquires a normal tone. When iodine is applied, the mucous membrane normally takes on a brown tint. In such a situation, these parameters are normal for healthy epithelium.
With the help of diagnostics, ectopia of the cervix can be detected. It is indicated by small bleeding after intimacy with a partner or by strong mucous discharge from the vaginal cavity. In the absence of such signs, there is no reason for treatment.
When identifying erosion, such a procedure allows you to accurately determine the possibility of developing precancerous processes. Colposcopy is necessary after treatment of erosion, to determine the effectiveness of the course of therapy.
If deviations from the norm appear during the examination, they are strictly recorded.
After a colposcopy, a woman receives results telling about the analysis performed and the general condition of the cervix. When describing the results, standard verbal forms can be used, as well as a drawing that shows the foci of inflamed areas.
The description may contain the following points indicating the normality or abnormality of the condition of the cervix:
- Shape – conical or irregular.
- Size – not hypertrophied, increased in volume or reduced (atrophied).
- The transformation zone is not visible or normal, large with closed or open glands, large cysts.
- The junction of flat and columnar epithelium is clear or blurred.
- Vessels – typical, atypical (short, twisting, comma-shaped, corkscrew-shaped).
- Vascular anomaly – no, rough or soft mosaic is present.
For certain criteria, the positions “Yes” or “No” are simply highlighted. These signs include: endometriosis, iodine-negative zone, ectopia, keratosis and mucosal atrophy. Based on the diagnosis, the doctor makes a decision on prescribing medications or further therapy.
Types of colposcopy
Currently, there are several types of colposcopy, they differ in the technique of execution, as well as the possibility of visualizing pathology.
Simple colposcopy
There are two types:
- Non-targeted colposcopy , which is performed during a routine vaginal examination. In this case, when examining the vagina and cervix, you can evaluate the integrity of the mucous membrane, its color, estimated size, as well as the condition of the external pharynx. In this case, we can only assume the presence of a possible pathology, take biological material for examination, and also outline a plan for further examination and management.
- Targeted simple colposcopy . It is performed, as a rule, during an examination when pathological elements are detected that may alert to the presence of pathology. Most often, this is the initial stage of performing an extended colposcopy. To do this, the cervix is exposed in the speculum and is processed to remove mucus and discharge from the canal or vaginal cavity. In this case, the area can be observed under magnification. This makes it easier to distinguish or refute the presence of pathology. If pathological elements are detected, then a simple colposcopy will transition to an extended one.
Extended colposcopy
This type of colposcopy is performed using any type of colposcope.
In this case, a distinctive feature is the use of special reagents:
- Initially, a solution of acetic acid in a small concentration is applied to the cervix without unnecessary impact .
- Inspections can be carried out for a certain period of time until the exposure time has expired. As a rule, this time does not exceed 3 minutes.
- After this, without cleansing the cervix, Lugol's solution is applied to it. It contains iodine, which penetrates the surface cells of the mucous membrane.
Why is a colposcopy prescribed?
Colposcopy in gynecology is a frequently prescribed test. Its essence lies in examining the cervix using a colposcope - a special binocular microscope equipped with illumination. Colposcopic examination involves studying the structure of the mucous lining of the vulva, vagina and cervix under magnification.
Women undergo colposcopy of the cervix in order to identify oncopathologies, as well as precancerous diseases or benign conditions.
Also, during colposcopy, smears are taken from the cervix and a biopsy is taken for subsequent cytological examination. In addition, the procedure allows you to obtain photographs of the foci of the pathological process under the necessary magnification.
Using a colposcope, you can achieve an image magnification of 6-40 times. At low magnification, the specialist determines the presence of foci of pathology, evaluates their color, surface, location, and shape. Then, with high magnification, the doctor examines suspicious areas of the mucosa. If it is necessary to better visualize the vessels of the microvasculature, the specialist uses a green filter. This approach is necessary to detect invasive cervical cancer.
Doctor adjusting colposcope
The colposcope consists of optical and lighting systems. The device is adapted for carrying out the procedure using a non-contact method. The design of the colposcope includes an optical head, a tripod and a base. This is necessary for ease of installation and use of the device. The optical head includes prismatic binoculars equipped with eyepieces that allow viewing of the tissues being examined. The head also contains an illuminator that creates the lighting necessary for work.
Colposcopic examination of the cervix can be simple or extensive.
- During a simple procedure, the mucous lining of the cervix is directly studied without the use of any additional reagents.
- Extended cervical colposcopy involves examining the cervix after treatment with a 3% acetic acid solution. This manipulation is necessary to more clearly identify pathological changes in tissue structure. This is explained by the fact that acetic acid causes short-term swelling of the mucous membrane and vascular contraction.
Interpretation of the results of colposcopy of the cervix.
Also, with expanded microscopy, treatment with Lugol's solution can be carried out to determine glycogen in the cells. This manipulation is called the Schiller test. In precancerous conditions, mucosal epithelial cells contain little glycogen, and therefore are not stained with Lugol's solution. When examined, they look like whitish spots against the background of healthy tissue, uniformly colored brown. Treatment with Lugol's solution facilitates the selection of a site for subsequent cervical biopsy.
Preparation for the procedure
Typically, performing a colposcopy does not require any significant preparation. But for the reliability of the data obtained, you should prepare and adhere to several rules regarding lifestyle, care, etc. on the days of the upcoming appointment.
Such measures can lead to disruption of the integrity of the mucous membranes of the cervix, which will obviously cause a false result.
Among them are:
- Material for cytological examination should be collected no later than 2 days before colposcopy.
- At least one day before the test, you should avoid sexual contact , especially if it is accompanied by the use of a condom or the release of sperm into the woman’s genital tract.
- During the day, you cannot perform an ultrasound examination using a transvaginal sensor, or perform colposcopy.
- Do not use topical medications for less than 24 hours.
- Also, colposcopy should be performed no less than 2 weeks after intrauterine intervention (regardless of the indication for which it is performed).
Contraindications
All medical procedures have their contraindications that must be observed. Violating them can cost a person his life.
There are no particularly serious contraindications to the procedure we are considering.
We can only say that, for obvious physiological reasons, a woman cannot be examined during menstruation.
Note that even pregnancy is not a contraindication, since the procedure does not pose any danger or mechanical damage to the female genital tract during its implementation.
When is the procedure performed?
- The study should be carried out any day, especially if there is a suspicion of an oncological process, as well as acute complaints from the cervix.
- Colposcopy is most informative in the initial days of the menstrual cycle, but there should be no discharge from the genital tract. The optimal time is considered to be 7-10 days of the menstrual cycle.
- If endometriosis is suspected, colposcopy should be performed on the 10-15th day of menstruation.
- During pregnancy, colposcopy can be performed at any time.
- During menopause, colposcopy is also performed at any time, in the absence of contraindications.
The essence of the disease
Cervical erosion occurs due to changes in this area. This process can be triggered by hormonal disorders, damage to the mucous membrane, inflammatory and infectious diseases. In this case, normal cells in a certain area are modified. Visually, the affected area appears as a red spot.
The pathology is most often asymptomatic, due to which certain difficulties arise in the diagnostic process. The absence of visible signs of the development of the disease leads to the fact that a woman is in no hurry to seek help from a gynecologist, and treatment of erosion begins in an advanced form.
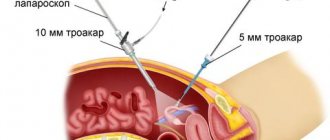
Conducting a survey
Colposcopy is performed on an outpatient basis, usually in any gynecological department or antenatal clinic. A prerequisite for compliance is the sterility of the room.
Examination stages:
- It is carried out on a regular gynecological examination chair.
- To visualize the cervix, a speculum must be inserted.
- After the cervix is removed, it is treated with a solution of acetic acid and the reaction of the cells is observed.
- After waiting for the exposure time, an iodine solution in the required concentration is then applied to the cervix. After this, the reaction is assessed again.
- As the procedure is completed, the mirror is removed and, if necessary, excess solution is removed.
- After the doctor performs a colposcopy and writes a report, the woman can go home.
Advantages of the method
Colposcopy is a modern diagnostic method that allows you to accurately see the condition of the cervical tissue and begin treatment on time.
What other advantages:
- The ability to diagnose early stages of cancer development or precancerous stages with erosive changes in the cervix.
- Diagnosis can be made without additional preparation - at the first examination by a doctor.
- Colposcopy can be done several times without harm to the patient’s health.
- The method is safe and painless.
- Can be used during surgery, which guarantees the success of the operation to remove damaged areas of the cervical canal.
- With the help of colposcopy, even the smallest fragments of malignant neoplasms are visible, which means treatment of cervical cancer is possible without surgery.
Colposcopy during pregnancy
Many women at the stage of pregnancy planning may be faced with such a question that the doctor prescribes a colposcopy.
Due to their condition, many are afraid of having it performed, believing that it can harm the fetus or cause miscarriage, as well as premature birth.
In fact, in some cases a colposcopy will be absolutely necessary:
- Most often, it is prescribed without fail to women at various stages of pregnancy if a malignant process is suspected. This is usually carried out after a woman registers and a smear is taken for oncocytology. In such a case, colposcopy allows you to assess the condition of the cervix, as well as exclude a possible malignant process.
- In addition, with complaints about the appearance of bloody discharge and the absence of pathology on the part of the fetus, as well as the presence of pronounced defects in the mucous membrane of the cervix, some doctors begin to confuse the presence of cervical erosion with the physiological state of deciduosis. Outwardly, it may resemble an erosive defect or the presence of multiple papilomatous formations, which begin to bleed upon contact with instruments. Normally, deciduosis goes away in a woman some time after the birth of the child.
The procedure is carried out using a standard algorithm of actions. It is no different from what is performed on women outside of this condition. Standard reagents are applied to the cervix, which contribute to the staining of the cellular composition.
Colposcopy of a pregnant woman should only be performed by an experienced specialist, as in some cases it may be difficult to see it in the mirror. In most cases, it turns out to be harmless to the woman and the fetus.
Contraindications during pregnancy
It is not recommended if:
- There is a risk of miscarriage or the woman has complications during pregnancy.
- The condition of isthmicocervical insufficiency or obvious threat deserves special attention.
- You should also refrain from performing it in cases where allergic reactions to the components of the reagents are detected, as this can lead to a deterioration in the woman’s condition and require the administration of medications.
Preparation
If the doctor has prescribed colposcopy for cervical erosion, you need to prepare:
- refrain from intimacy for 2-3 days;
- Do not use any vaginal products for 3-5 days, including tampons and antiseptic suppositories for erosion;
- refrain from douching for a week, even if clean water is used for this;
- Before performing colposcopy, it is necessary to perform hygiene procedures without using soap solutions that can affect the microflora of the genital tract.
No anesthesia is used during diagnosis. For the vast majority of patients, the procedure is absolutely painless.
Only some women report discomfort when applying the reagent. If the sensitivity threshold is reduced, the doctor recommends taking a painkiller in the form of a tablet, which a woman usually uses for menstrual pain.
Consequences
Currently, the design of the devices and the solutions used are safe for use in women, so the risk of complications or side effects is minimal.
Only in extremely rare cases may situations arise that will lead to complications in carrying out this manipulation.
Among them are:
- Discomfort or minor pain associated with the difficulty of removing the cervix in the speculum . This may be due to the location of the organs, as well as the patient’s insufficiently comfortable position or an unemptied bowel.
- The appearance of bloody discharge after manipulation. To a greater extent, this is due to trauma to damaged mucous membranes; in some cases, especially when the malignant process of the cervix is affected in the stage of decay, bleeding may develop.
- Allergic reaction to the use of solutions. These include burning, itching in the vaginal area, redness of the mucous membranes or a systemic allergic reaction.
- When carrying out a procedure with the presence of contraindications to it, as well as complications during pregnancy , if the procedure is carried out without comparing the possible risks and benefits.
What is colposcopy and how is it done?
This diagnostic method is carried out in clinics and diagnostic centers. It is an examination of the vaginal walls, vaginal cervix, and vulva. This diagnostic procedure is performed using a colposcope - an optical or video device resembling a microscope, equipped with a powerful magnifying lens and a lamp. With its help, the doctor receives an image of tissue magnified tens of times. If a digital device is used, the high-resolution image is transferred to a computer, after which (at the patient’s request) it can be recorded on a digital medium.
Expert opinion
During the procedure, the doctor thoroughly examines the condition of the mucous membrane and blood vessels, assesses the presence of possible formations, and also (if necessary) performs a biopsy - excision and collection of a small fragment of tissue or a smear for oncocytology for laboratory tests. If a biopsy is necessary, it is recommended to perform it in the first phase of the menstrual cycle.
Obstetrician-gynecologist of the highest category Oksana Anatolyevna Gartleb
How is the procedure performed in gynecology?
The patient is in a gynecological chair, the colposcope lens is located opposite the entrance to her vagina at a distance of about 15 centimeters. To ensure sufficient visibility, the vagina must be dilated; for this, a Cusco gynecological speculum is inserted into it. Its insertion is usually painless, but may cause minor discomfort. Next, the doctor examines the organs of interest. The examination time is usually 10-20 minutes.
The results must be deciphered by a specialist, because the patient will not be able to do this correctly on her own. Also, at the woman’s request, images and transcripts obtained during the examination can be recorded on electronic media.
Among the indications for this diagnostic method, in addition to preventive examination, are:
- pain of unknown etiology in the lower abdomen;
- vaginal discharge that has a strange smell and consistency;
- any vaginal discomfort (feeling of dryness, burning);
- painful intimacy;
- the appearance of spotting after sex;
- menstrual irregularities, represented by the appearance of bloody discharge not associated with menstruation.
Decoding the results
Results in gynecology may be as follows:
- Ectopia. This is a condition that is characterized by the fact that the cylindrical epithelium extends beyond the cervical canal, moving to the vaginal part of the cervix. This condition may be congenital and does not always require treatment. In some cases, it may go into the uterine cavity on its own after the birth of the child. Normally, it can appear after the use of oral contraceptives, as well as during pregnancy or adolescence.
- Presence of acetowhite epithelium. This is a condition in which the cervical epithelial cells change color to white. More often it characterizes the condition of dysplasia or viral infection. An area of bright white discoloration is found on the cervix. This condition requires mandatory further examination and treatment. A mandatory laboratory test is to identify the human papillomavirus.
- Presence of iodine-negative areas. When performing colposcopy and using Lugol's solution, the exocervix is incorrectly stained in a light color, compared to nearby dark areas. Characterize dysplastic conditions, as well as the phenomena of atrophy and leukoplakia. To clarify the diagnosis in this case, a mandatory biopsy is required.
- Presence of atypical vessels. During the examination, a violation of changes in the vascular pattern is noted; they can not only have a characteristic appearance for any disease, but also a violation of the reaction to the use of reagents.
- Mosaic and punctuation detection. Such conditions characterize the manifestations of vascular pathology. Moreover, they can occur with viral carriage, as well as long-term inflammatory diseases and a possible malignant process.
- Identification of cystically dilated glands. Formations represented by changes in surface cellular elements associated with hormonal imbalances. Most often, the use of conservative therapy is sufficient.
- Leukoplakia. A condition that is associated with increased production of epithelial cells. As a result, an area of increased keratinization is observed. This is a variant of the pathology, since normally the cells of the mucous membrane should not become denser. Leukoplakia requires a mandatory biopsy.
- Presence of condylomas. The appearance of areas of horny epithelium, which can extend beyond the mucous membrane. Most often they resemble cabbage-shaped formations that can reach large sizes. In some cases, it manifests itself as bleeding or the development of infertility. They require effective antiviral treatment and removal of emerging lesions.
How is the research result determined?
Colposcopy in gynecology is considered one of the simplest and most effective methods for diagnosing gynecological pathologies. As a result of this procedure, it is possible to determine the nature of the disease and its location. During the examination, the doctor assesses the appearance and structure of the mucous membranes.
Normally, the shell has a pale pink color, changing to bluish in the second phase of the cycle. Lugol paints it brown, against which all the anomalies are clearly visible.
If, during a colposcopic examination, smooth, fine-grained areas of a reddish tint were found, then a diagnosis of cervical erosion is made. Small papillae of rich red color indicate the presence of pseudo-erosion.
Papillomas are detected by applying a vinegar solution to the tumor. In this case, there is a contraction of blood vessels and blanching of the affected areas. The diagnosis of “endometriosis” is made if pink or bluish-purple formations of irregular shape are detected, the color of which changes during the examination.
If compactions of the mucous membranes are detected in the form of rough spots or thin light plates that separate from the surface without much effort, leukoplakia is diagnosed.
Colposcopy can also determine the presence of cancer. These are swollen, glassy areas with protrusions and clearly visible vessels that do not respond to reagents.
What should you not do after a colposcopy?
If colposcopy was performed in an extended version, then no special recommendations are required after it is performed. The woman can go home, minor discomfort is acceptable.
After the procedure, it is recommended to carry out hygienic measures, since acetic acid and iodine solution can cause discomfort, an unpleasant odor and a slight burning sensation if there are defects in the mucous membrane in the vagina and vulva.
If the procedure was performed with a biopsy:
Sexual activity should be avoided for a month.- Use douching and sanitary tampons.
- Use medications based on anticoagulants. These may be acetylsalicylic acid preparations.
- It is required to limit physical exercise, weight lifting, etc. for two weeks.
- Overheating, the use of saunas, baths, and baths should be completely avoided for a month. For a while after this procedure, it is recommended to take a shower with water at room temperature.
Recommendations after colposcopy
After an extended colposcopy, during which a biopsy was performed, the woman is advised to observe certain restrictions. Thanks to them, the surface of the cervix, on which a small abrasion remains, will have time to regenerate. What should you remember after the procedure?
- Sex after colposcopy is prohibited for 2 days.
- It is advisable to reduce physical activity.
- You will also have to temporarily abandon the use of vaginal tampons and douching.
- For 1-2 weeks, it is recommended to refrain from swimming in the pool and open water, from visiting the sauna and bathhouse. You should also not take a bath - hygiene procedures should be limited to washing and taking a shower.
Following these simple rules will reduce the recovery time of the cervix after colposcopy with biopsy and help avoid possible unpleasant consequences - in particular bleeding and inflammation.
Sources:
- COLPOSCOPY AS AN EXPERT METHOD FOR DIAGNOSIS OF CERVICAL PATHOLOGY. Ulyanova I. O., Makarenko T. A., Nikiforova D. E., Domracheva M. Ya. // Siberian Medical Review. – 2020. – No. 6. – P. 99-.
- ROLE OF COLPOSCOPY IN DIFFERENTIAL DIAGNOSIS OF INFECTIOUS DISEASES OF THE CERVIX. Kulinich S.I., Sverdlova E.S. // Far Eastern Medical Journal. – 2009. – P. 48.
- Diagnosis of HPV-associated lesions of the cervix // Handbook of the head of the clinical laboratory. – 2012.
- 16 Immunohistochemistry in Colposcope-Directed and Random Cervical Biopsies of CIN2 and CIN3. Arvizo S., Chen Q., Du H. // Journal of lower genital tract disease. – 2020. – Vol. 20, No. 3. – R. 197-200.
- Practical colposcopy. Rogovskaya S.I. // M.: GEOTAR - Media, 3rd ed., revised. and additional - 2013. - P. 240.
- https://www.medicinenet.com/colposcopy/article.htm
- https://www.emedicinehealth.com/colposcopy/article_em.htm
- https://www.cigna.com/individuals-families/health-wellness/hw/medical-tests/colposcopy-and-cervical-…
- https://www.brown.edu/campus-life/health/services/promotion/general-health-reproductive-health-sexua…
Cost of the procedure
This question will largely depend on the location of the colposcopy.
If the procedure is carried out in the antenatal clinic department or in any hospital of a state medical institution, regardless of the main profile (in most cases this is a gynecological department, but it can also be an obstetric department, as well as an oncology clinic), then as a rule the woman does not pay anything for it funds.
If colposcopy is performed in a private medical center or commercial department, the price of the procedure. will depend on the level of the institution and the approximate pricing policy.
The average cost is 500-2000 rubles. It does not depend on the indication for which a woman is sent for colposcopy, as well as her current condition.
Does it hurt
Almost all women are afraid to undergo this procedure because they have misinformation about the pain that can be caused. Such thoughts must be dispelled.
Colposcopy is not an entirely safe procedure, but it still does not cause any pain. But, it should be noted that pain can be provoked by acid during a more open examination of the uterus. This is another type of this procedure, which the woman will, of course, be warned about. It is when the acid and mucous membrane react that discomfort can occur. But they won't last long.
There are also a number of complications that occur rarely, but still occur among women:
- Bleeding.
- Infection.
- Nagging pain in the lower abdomen.
Bleeding in the first few days is an absolutely normal positive sign indicating rapid tissue healing.
But along with positive signs, there are negative symptoms:
- Increase in basal body temperature.
- Change in human condition. Throws you into cold or heat.
- Nagging pain in the lower abdomen.
Gynecologists recommend calling an ambulance if you experience unusual sensations after the procedure. In this case, the woman needs immediate examination by a female doctor.
All negative symptoms may appear 2-3 days after this type of intervention.
Let us repeat once again, negative symptoms can appear only after an extended procedure, since during it the gynecologist uses a number of substances to impregnate the epithelial tissues. Symptoms are a kind of reaction to such substances.
Features of the recovery period
Usually, after colposcopy, the patient does not experience any unpleasant conditions. Your lower abdomen may hurt for several days. Due to the effect on erosion, a woman may experience bloody discharge. Normally, they should not last more than 5 days.
If a simple colposcopy was performed, the patient is not given any additional recommendations. For an extended type of diagnosis involving taking a biopsy, you will have to adhere to the following rules:
- do not take a bath or visit the pool;
- do not expose your body to thermal procedures;
- reduce physical activity and avoid lifting heavy objects;
- exclude intimacy;
- do not use vaginal products or sanitary tampons.
These rules must be followed until the end of the next menstrual bleeding.
What is it - diagnostic, difficult
Colposcopy or colposcopy is a diagnostic method for visual assessment of the exocervix (the vaginal part of the cervix in contact with the vaginal microflora). To carry it out, you need a colposcope, which is equipped with optical equipment that allows you to visualize structures under multiple magnification.
The study is performed by an obstetrician-gynecologist in most medical institutions for the purpose of a detailed examination of the exocervix and cervical canal, identifying precancerous changes, as well as monitoring the effectiveness of treatment of the neoplastic process.
Types of research for detailed investigation
Several types of colposcopy are used in clinical practice, each of which differs in purpose and technique.
Simple colposcopy
This type is the most common and technically simple. It aims to visually assess the exocervix. During this procedure, the nature of the discharge, the configuration of the cervix and changes in the structure are assessed. The initial task is to search for abnormalities in organs and tissues. Inflammatory foci, erosions, polyps and tumor processes are visually detected.
Extended
Advanced colposcopy (sometimes abbreviated as ECC) refers to a more in-depth method of evaluating the cervix by applying reagents and assessing changes in cell staining. The main substances include Lugol's solution, iodine and acetic acid.
Chromocolposcopy
This option is based on examining the cervix using special dyes. The method involves changing the color of different cells with different substances.
A green or blue reagent, as well as a special light filter built into the colposcope, allows you to identify a suspicious area on the exocervix.
Chromocolposcopy is most valuable in identifying a malignant process. Application of a luminescent dye followed by interaction with pathological cells leads to the emission of luminescence in ultraviolet rays.
Videocolposcopy
Video colposcopy refers to a type of advanced digital colposcopy, which is performed using modern equipment equipped with a special photo or video camera.
The equipment allows you to record the image you see, as well as the reaction of cells in response to the application of reagents. Using the saved information, the doctor can evaluate the dynamics of treatment, as well as the rate of progression of the disease.
results
Visual results of cervical colposcopy, regardless of its type, are given immediately after the procedure. If areas stained with the solution are detected, a biopsy may be performed, as this may indicate a precancerous condition.
The biopsy is done with surgical forceps, which can make the procedure slightly uncomfortable. The doctor splits off the fragment needed for research, placing it in a test tube for subsequent histological analysis. A small wound remains at the biopsy site, which heals in just a couple of days.
If a woman is about to begin her period, the procedure is postponed so that the damaged tissue can heal unhindered. The results of the histological examination come in a week or two. The doctor himself sets the time for the patient’s next visit to establish an accurate diagnosis.
How is the colposcopy procedure performed?
The patient does not feel pain. Perhaps the unpleasant sensations due to the gynecological speculum being in the vagina throughout the entire process. Moreover, it does not last long, only 10-20 minutes.
How does all this happen? The patient is located on a gynecological chair, next to which there is a colposcope. After a speculum is installed in the vagina, the study of the epithelium and blood vessels begins. This is done using diagnostic tests. The doctor lubricates the cervix with iodine solution (Lugol) and vinegar solution. At this moment, a short-term burning sensation is possible. Lugol is neutral. This is done in order to get a good look at the desired area, since the solution provokes “swelling” of the cells for a short time. After this, a detailed inspection is carried out.
Unpleasant pain occurs when tissue samples are taken for analysis. Afterwards there is mucous or bloody discharge. Don't be afraid of them; they will disappear over time.
Colposcopy is safe and available even to nulliparous women. However, it is contraindicated if:
- less than 8 weeks have passed since birth;
- less than 4 weeks have passed since the abortion;
- the woman is bleeding or menstruating;
- there is a pronounced inflammatory process.
If necessary, vaginoscopy and colposcopy are performed on virgin girls, without breaking the hymen or causing pain. For this purpose, special children's gynecological speculums are used. Sometimes only with the help of such an examination can a foreign object be detected in a girl’s vagina and removed.
The cost of colposcopy depends on the type and purpose of the examination. In addition, the price of tissue analysis (histology) is taken separately. On average, the examination will cost from 1000 rubles. Plus about 2000 rubles for a histological report. Remember, an ultrasound of the cervix performed vaginally cannot replace colposcopy.
Back to contents
Purpose of the event
First of all, colposcopy is a diagnostic research method applicable in the presence of the following symptoms:
- itching, burning in the vagina;
- acyclic uterine bleeding;
- painful sensations, possible bleeding before or during sex;
- dull pain in the lower abdomen, which is constant and increasing in nature.
If a woman discovers a rash around her external genitalia or the smear result is unsatisfactory, then colposcopy is indicated first.