FGS stands for fibrogastroscopy (or simply gastroscopy), perhaps the most effective method for studying the digestive organs. Let us consider in detail in this article what FGS of the stomach is, how it is done and how long the procedure lasts, what indications and contraindications it has, as well as how an adult can prepare for its safe, most comfortable implementation.
In medicine, FGS is the “gold standard” for examining people with pathologies of the digestive system. But this is unlikely to inspire “feat” in the name of their health in patients leaving the gastroenterologist’s office for the first time with a referral for FGS or FGDS. Many are lost, not knowing what to expect from this “execution” and how best to prepare for it, even if the doctor has given instructions.
After reviewing the information presented below, you will be able to expand your understanding of this procedure, get rid of prejudices that give rise to fear of the study, and prepare properly for it.
Table of contents
- FGS of the stomach - what is it, how does it differ from FGDS
- What does gastric FGS show?
- Indications and contraindications
- FGS of the stomach - how the procedure works
- How long does FGS last?
- How soon can you eat after the examination?
- How to prepare in the morning What you need to take with you for the procedure
- How to behave correctly during FGDS and FGS
- Is it possible to drink water during gastroscopy?
- Taking pills before the procedure
- Is it possible to smoke before and after FGS?
- What can you eat before FGS of the stomach?
What you can and cannot do after the procedure
It is better to stay in the medical facility for the first couple of hours after the examination, especially if sedative medications were used. In case of complications (which is extremely rare), doctors will be able to provide assistance in a timely manner. You can take an accompanying person with you to help you get home if you are not feeling well.
Anesthetics used during FGDS cause numbness in the root of the tongue and pharynx, so you should not eat or drink until their effect wears off. If sensitivity is restored, you can safely eat.
It is strictly forbidden to drink alcohol on the first day after the procedure.
It is better to refrain from driving, especially when using sedatives. You will be able to drive after 12 hours.
More detailed information about behavior after FGS will be provided by the specialist conducting the study.
FGS of the stomach - what is it, how does it differ from FGDS
Visual examination of the mucous membrane of the stomach and esophagus using an endoscope (a flexible tube with a video camera and a light source at its end), which is inserted through the oral cavity (less often through the nose), is called gastroscopy - FGS (fibrogastroscopy).
FGS is a modern, accessible, fairly informative and popular diagnostic method for assessing the condition of the mucous membrane of the esophagus and stomach in order to make the correct diagnosis.
In many cases, to obtain the most accurate information about the state of the organs of the digestive system, the flexible endoscope probe moves further than the stomach - into the lumen of the duodenum. Then another letter appears in the abbreviation of the name of the study, replacing it with FGDS (fibrogastroduodenoscopy).
FGDS is a method that allows you to closely examine not only the condition of the esophagus and stomach (as with FGS), but also the initial part of the small intestine - the duodenum. This is the only difference between these two procedures. Preparation for the procedures is the same.
FGS or FGDS is prescribed by a gastroenterologist, and the procedure itself is performed by an endoscopist.
Important!
Today, bulky gastroduodenoscopes with thick hoses have been replaced by innovative devices that have high technical and optical characteristics, and, most importantly, a minimum thickness of the flexible tube.
These factors provide a number of benefits:
- no pain;
- easy tolerability of the procedure;
- high security;
- high information content.
If necessary, during the procedure, medical and surgical manipulations are performed, a portion of gastric juice, bile is taken, or a fragment of mucosal tissue is taken (biopsy) for laboratory testing.
What does improper preparation and standard complications lead to?
If the patient’s preparation for fibrogastroduodenoscopy was incorrect, the result may be erroneous. In addition, nausea and vomiting, belching and bloating may occur. In case of low visibility, due to improper preparation, injuries to the mucous membranes of the esophagus and stomach are possible.
The most severe and rare complications include asphyxia, but this occurs mainly if the patient took drugs that, together with anesthesia, caused a severe allergic reaction.
Standard complications include:
- Pain in the larynx. This occurs due to mechanical damage to the organs by the tube, especially when breathing improperly and ignoring doctor’s advice. Unpleasant sensations may occur during swallowing for several days. To speed up healing, it is better to avoid irritating foods.
- Bleeding in the esophagus, stomach, intestines in places of injury to the walls.
- Perforation. Occurs rarely.
- Laryngotracheitis, hoarseness.
- Allergic reactions.
- Jaw injuries are a very rare occurrence.
- Pain at the biopsy site.
- Injury to the gastrointestinal tract. May occur with sudden movements of the patient.
What does gastric FGS show?
During FGS (FGDS), even the slightest changes in the mucous membrane of the stomach, esophagus and duodenum are visible and diagnosed. A more detailed picture can only be provided by a biopsy of neoplasms (for oncology), but this is already a study at the cellular level.
FGS of the stomach in adults can show:
- condition of the mucous membrane and walls of the stomach and esophagus;
- diameter of the lumen of the esophagus (possible narrowing);
- degree of reflux (reflux of stomach contents into the esophagus);
- detect neoplasms, erosions, ulcers and bleeding.
Important!
Very often, in the early stages, dangerous diseases of the gastrointestinal tract are “silent”. Not only polyps and tumors, but also erosions and ulcers sometimes occur without symptoms. Their timely detection, as is known, is the basis for successful recovery.
Now endoscopic equipment has been so improved that anyone can be examined painlessly and comfortably for prophylaxis (without any complaints, at their own request).
Description of the procedure
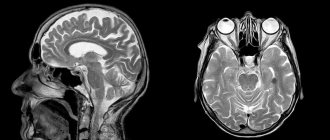
Fibrogastroduodenoscopy (FGDS) is a technique for endoscopic examination of the upper digestive system
(stomach, duodenum, esophagus). To carry it out, a special probe is used, which is equipped with a miniature camera and a manipulator.
In modern endoscopy, the image is displayed on a special screen. Acidity is also constantly monitored. FGDS usually includes a test for the presence of Helicobacter pylori infection
.
If necessary (for example, long-term existence of an ulcer, the appearance of neoplasms, chronic inflammatory processes), the examination is supplemented by a tissue biopsy with cytological examination
in a specialized laboratory.
An FGDS certificate is the basis for diagnosing diseases of the stomach, duodenum or esophagus.
It allows you to visualize changes in the mucous membrane that are difficult to see on CT or MRI. It is based on the results of FGDS that one can distinguish gastritis, peptic ulcer or malignant process
.
The study is of particular importance for highly specific rapid diagnosis of Helicobacter pylori infection.
Fibrogastroduodenoscopy is prescribed if the patient has the following symptoms:
- aching pain in the upper abdomen, which intensifies after eating or drinking (especially alcoholic or carbonated);
- sensations of discomfort in the epigastrium ;
- the occurrence of nausea, single vomiting;
- burning behind the breastbone or heartburn;
- decreased appetite and subsequent loss of body weight;
- tendency to constipation or diarrhea.
Typically, FGDS is carried out after the patient is examined by a doctor and undergoes basic laboratory tests.
FGS of the stomach - how it is done
The FGS procedure is performed in a specialized gastroscopy room and consists of several stages.
Let's look at how gastric FGS works:
- The patient is given local anesthesia: the throat or root of the tongue is treated with a solution of Lidocaine or Dicaine (used as a spray or given to drink).
- After a feeling of numbness appears (about 5 minutes), the patient is placed on his left side.
- A mouthpiece (a plastic ring-mouthpiece) is inserted into the subject's mouth, which must be clamped with the teeth and lips.
- The doctor will carefully insert the flexible endoscope hose through the mouthpiece to the root of the tongue. Then he will ask you to swallow or inhale, and the endoscope will move into the esophagus.
- The doctor will slowly advance the device from the esophagus to the stomach and examine its walls. From this moment, the image of the mucous membrane can be seen on the monitor (if necessary, video or photo recording is carried out on a digital medium). Air is supplied through the endoscope to straighten the lumen of the esophagus and the stomach cavity. While advancing the gastroscope probe, the doctor can perform therapeutic and diagnostic manipulations.
- After the probe enters the stomach, the doctor examines the condition of its walls for several minutes.
- After completing the examination of the stomach (and other manipulations), the doctor carefully removes the device - the procedure is completed (with FGDS, the endoscope is first advanced into the duodenum). The results are recorded.
How to prepare for FGS of the stomach in the morning
In the morning before the FGS, in the first half of the day you are allowed to brush your teeth, but not eat. Only preparation for FGS of the stomach and duodenum, carried out in the afternoon, allows a light breakfast.
What should you bring with you to the procedure?
Before the gastroscopy procedure, you need to take from home:
- drinking water and medicine, which should be taken immediately after the examination;
- food, preferably kefir, yogurt (if necessary);
- towel.
In addition, you need to prepare and take with you to the FGDS:
- referral for research;
- outpatient card;
- protocols of previous studies.
How to behave during FGDS (FGS)
You should definitely notify your doctor if you are allergic to drugs for local anesthesia (for example, lidocaine).
People wearing glasses or dentures are asked to remove them.
The best advice for well-bearing and surviving FGS of the stomach is to relax as much as possible and take slow and deep breaths through your nose and mouth. Also listen to your doctor and follow his breathing recommendations.
Is it possible to drink water before FGS of the stomach?
It is not advisable to take a lot of liquid on the day of the procedure. You can drink before FGS no later than 3 hours before the test and no more than half a glass. This can be mineral water (still), weak tea. It is not recommended to drink coffee.
Taking pills before the procedure
It is allowed to take medications that do not require swallowing (dissolve in the mouth). The remaining tablets are not taken before the FGS or FGDS procedure.
Is it possible to smoke before and after FGS?
Many years of practice have proven that smoking contributes to the appearance of nausea and other unpleasant sensations during endoscopy. It can also increase the duration of the procedure due to irritation of the mucous membrane.
3 hours before the test, smoking must be stopped before FGS (nicotine and tar activate the production of gastric juice and mucus).
For the same reasons, it is also necessary to maintain an hour-long period without smoking after the examination.
Moral preparation for the procedure
It is very important to learn to control your emotions before and during the procedure. The calmer the patient is, the easier it is for the doctor to work. In addition, if the patient is relaxed, the probe advances easier and the pain of the manipulation is reduced.
Those who go for examination for the first time experience many fears, including for their lives. There is an opinion that you can suffocate while the endoscope is in the digestive tract. This is a completely incorrect and baseless judgment.
The tube does not border the respiratory tract at all, and therefore FGDS does not pose any danger.
Discomfort is largely associated with the process of pumping air to straighten the walls and obtain a clear picture. There is no way to avoid this, but understanding these simple truths, you can go through the procedure with confidence and without a grain of doubt.
It is very important to remember that this is only a momentary discomfort; usually the period between insertion and removal of the endoscope is no more than 2 minutes . Therefore, you need to endure this moment, listening carefully to the doctor’s recommendations in order to find out about the state of the digestive tract and promptly prevent more dangerous procedures.
Some patients are advised to administer local anesthesia to quell panic. In fact, the procedure is completely painless and there is no need to use the drug. On the contrary, after using it, it is difficult for the patient to swallow and breathe, as the treated surface becomes numb.
Diet before FGS of the stomach
Diet recommendations should not be neglected, since even a minor error can lead to difficulties during the study. The diet before FGD of the stomach, first of all, takes into account the intake of warm food with a soft consistency and small portions.
What can you eat before FGS of the stomach?
The final meal before gastroscopy should be 19 hours (in the most extreme case - 12 hours before the start of the procedure).
If the diagnosis is carried out in the afternoon, then 8 hours before it you can allow yourself a light breakfast. The liquid can be drunk 3 hours before FGS, but its amount should not exceed 100 ml.
However, nutrition before FGS of the stomach is a purely individual topic. And what you can and cannot eat, how much not to eat before gastroscopy, the attending gastroenterologist should say exactly at the stage when the patient is preparing for the study.
Example of a light dinner
In the evening you can eat, for example: steamed vegetables with boiled fish or rabbit (serving no more than 350 grams). For the next 12 hours, fasting is observed.
A light dinner before FGS of the stomach means that in 12 hours the stomach has time to process the food eaten.
FGS of the stomach under anesthesia
The use of anesthesia during gastroscopy is possible not only if there are indications, but also at the request of the patient (if there are no contraindications for it).
FGS of the stomach with anesthesia is recommended:
- during surgery;
- children from 3 to 6 years old;
- sensitive and receptive people.
After gastroscopy with the use of drugs for anesthesia, the patient requires a recovery period and several hours to be under medical supervision, therefore, the length of stay in the institution and the cost increases.
There is an alternative option for the procedure under anesthesia - this is FGS with sedation (i.e., during sleep). Sedation (putting the patient into a half-asleep state exactly for the duration of the procedure using “laughing gas”) eliminates the moral and physical inconveniences of gastroscopy: salivation, gag reflex, etc. After it, you cannot immediately get behind the wheel of a car.
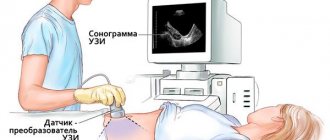
How to check the stomach without FGS in an adult?
When examining the hollow organs of the digestive system (without swallowing the tube), the following are used:
- X-ray;
- Ultrasound;
- computed and magnetic resonance imaging.
These methods have one significant drawback - a limited list of diagnosed diseases of the esophagus, stomach and duodenum. They do not provide a visual picture of the mucous membrane of the esophagus, stomach and intestinal wall (except in cases of large ulcerative lesions).
An alternative to FGS can only be capsule endoscopy - an innovative method that uses a capsule with a video camera to examine the digestive tract.
However, it also has its drawbacks - it is an expensive procedure, there is no way to take a biopsy sample, the camera is not controlled (dangerous lesions can be missed), if bleeding is detected, you will still have to resort to invasive manipulations, sometimes the capsule is removed using an endoscope.
Unfortunately, to the question: “What can replace FGS?” – there is only one answer: It is not possible to check the condition of the esophagus, stomach and duodenum with the provision of adequate therapy without FGS or FGDS.
Important recommendations: how to prepare for gastric FGS
Proper preparation for the examination is the most important condition for effective gastroscopy!
Attention!
Errors at the stages of preparation for FGS complicate the procedure, reduce its comfort and information content!
To avoid mistakes, you need to carefully listen to the recommendations of a gastroenterologist, who will explain how to prepare for FGS of the stomach, what you should not eat, and also how to go through this procedure comfortably.
Step-by-step preparation for the FGS is divided into general and local events.
General preparation for FGS is the doctor’s area of responsibility:
- Identification of possible contraindications to FGS.
- Assessing and weighing possible risks.
- Drug correction of conditions potentially dangerous for the procedure (severe angina, arrhythmia, arterial hypertension, respiratory failure, bleeding after minor operations with low platelets in the blood test, etc.). Corrective therapy is prescribed several days before the procedure.
- Elimination of possible allergic reactions to local anesthetics. Be sure to report any allergic reactions to medications.
- Identification of diseases that may affect the choice of drug preparation for the study (for some pathologies, the use of certain medications is contraindicated). Provide the doctor with all required medical documentation.
- Psychological preparation consists of developing an optimistic attitude. This will reduce discomfort during insertion of the gastroscope. If a person cannot overcome fear, the doctor prescribes sedatives and sedatives.
Effective preparation for FGDS includes the following steps:
- Report all medications you take. Due to the procedure, your medication regimen may change or temporary discontinuation may be necessary.
- If the patient has esophagitis or inflammatory diseases of the upper respiratory tract, appropriate therapy is prescribed. Sanitation of these pathways is important for smooth insertion of the endoscope.
- 2-3 days before the test, completely eliminate alcohol, fried and fatty foods, and foods that cause flatulence should be removed from your diet. To prevent flatulence and disturbances in the passage of food, enzyme preparations and sorbents are prescribed. For example: Creon, Espumisan, Enterosgel, etc.
- Dinner the night before the FGS should be no later than 18.00-19.00 hours.
- On the morning of the test, you should not eat anything (if the test is scheduled before lunch).
- You cannot drink sparkling mineral water.
- In the morning you can: brush your teeth, take lozenges in your mouth.
- To undergo the procedure, prepare comfortable clothes in which you can lie down, bend your legs and not be embarrassed.
- There is no need to paint your eyelashes and lips before the procedure. Makeup can deteriorate and cause inconvenience to the doctor during manipulations.
By undergoing FGS or FGDS, you give the attending physician the opportunity to make a diagnosis as accurately as possible and create an effective treatment regimen for the identified pathology. Remember that proper preparation is a responsibility shared by two people: the patient and the doctor.
© The material was prepared with the participation of doctor, candidate of medical sciences Stepura V.P.
What to take with you
Typically, people undergoing FGS need to have:
- the direction in which the patient’s data and the presumed diagnosis are indicated. The signature of the doctor and the seal of the medical institution are required;
- medications for regular use;
- outpatient card;
- conclusions of previous studies so that it is possible to compare results and monitor the effectiveness of treatment;
- towel, disposable diaper;
- shoe covers or replacement shoes.
Blood pressure-lowering medications and sedatives are also allowed.