Are HSG and ultrasound the same thing?
HSG and ultrasound are two different procedures. An ultrasound examination involves an overview of the patient’s internal organs and detection of possible pathology by changes in their structure and density. The picture is displayed on the monitor. To perform an ultrasound, there is no need to perform any additional procedures. It is enough to simply lubricate the surface being viewed with a special gel.
HSG involves injecting a contrast fluid into the uterus. After its distribution, the doctor performs a series of images using an X-ray machine (but it is possible to examine the internal organs using an ultrasound machine). The introduction of a contrast agent makes the study more informative. In addition, the doctor can diagnose tubal obstruction, which cannot be done during a regular ultrasound examination.
Since two devices can be used to perform HSG: X-ray and ultrasound, there is a difference in the diagnostic process. If the pictures are taken using X-ray equipment, the procedure is called “x-ray hysterosalpingography”. When an ultrasound machine is used to perform the examination, the technique is called “echohysterosalpingography”. Because of the similarity in name, many people believe that these procedures are identical; in fact, their essence and diagnostic significance differ.
Is it possible to get pregnant and give birth with fluid in the fallopian tubes?
Since there are several types of hydrosalpinx, not all of them lead to complete infertility. With some types of fluid accumulation in the fallopian tubes, pregnancy is possible. This applies to the case when the pathology is one-sided.
If the examination shows that the hydrosalpinx is bilateral, then there is no talk of pregnancy yet. After successful treatment with medications and surgery, about 50-70% of all women suffering from this pathology are able to become pregnant and give birth to a child naturally.
In cases where treatment is unsuccessful and both tubes are obstructed, the woman is diagnosed with infertility. She won't be able to get pregnant on her own.
To avoid such a terrible diagnosis, consult a doctor promptly if you experience any discomfort in the female organs.
Checking the patency of the tubes using hysterosalpingography requires preliminary preparation. A week before the procedure, you should avoid examinations and the use of sprays, vaginal suppositories, tablets and other intimate hygiene products.
To improve the quality of the examination, an X-ray examination of the uterus should be carried out before menstruation, since the mucous membrane of the uterus is thick, and in the first weeks of menstruation it is rejected, which makes it difficult for the contrast agent to pass through.
Quite often situations arise when pregnancy does not occur for a long time. If the test results are normal, it is recommended to undergo additional examination and check the condition of the fallopian tubes for their patency.
Sometimes a complete obstruction forms in one pipe, and a partial obstruction in the second. In such a situation, it becomes possible to become pregnant, but there is a high probability of ectopic pregnancy. The same risk occurs when partial obstruction affects both tubes.
In these cases, the egg does not reach the uterus after fertilization, since continuous division and growth occur during movement. Because of this, it can stop in a narrow lumen of the pipe, blocked by adhesions.
If an ectopic pregnancy is detected, you should immediately contact a specialist.
Which is better: X-ray or HSG?
A standard x-ray examination will not reveal obstruction of the fallopian tubes or other pathologies of the pelvic organs, so it is never used for this purpose. HSG, on the contrary, is the method of choice for suspected tubal obstruction, endometrial polyps, uterine fibroids, endometriosis and other pathologies of the female reproductive system. Therefore, HSG is definitely better than x-ray.
However, it is worth understanding that HSG is performed either using an X-ray machine or using an ultrasound diagnostic device. A woman's internal genitalia become visible after a special contrast agent is injected into the uterus and fallopian tubes. Many specialists use the term “X-ray” to refer to the procedure for examining the fallopian tubes using an X-ray machine, and the term “HSG” refers to conducting a study using an ultrasound machine. If we consider the issue from this point of view, then GHA will be better than X-ray.
The fact is that Echo-GHA has the following advantages over RGHA:
- A woman will not have to use contraceptive methods that protect her from pregnancy if she is prescribed an ultrasound HSG.
- There are no contraindications for conceiving a child in the month when Echo-HSG was performed.
- During and after the procedure, there is no risk of an allergic reaction to the contrast agent, which contains iodine.
- The patient's body will not be irradiated by the X-ray machine. Moreover, this negatively affects the number of eggs that are present in the ovarian follicles (ovarian reserve).
Checking the patency of the fallopian tubes
There are three ways to check the patency of the fallopian tubes.
The main one is hysterosalpingography. This study consists of an X-ray examination of the fallopian tubes.
First, a rubberized tip is inserted into the uterine cervix, and with its help a thin rod called a cannula is inserted. A dye solution (blue) is injected into the cavity through a cannula.
After which, using X-ray radiation, an image is taken. Which displays the general condition of the uterine body and tubes.
Other methods of researching the reproductive sphere include:
- Sonohysterosalpingography (similar methods - echohysterosalpingography, sono-, echo-, hydrosonography). This is a method with less severe pain than with HSG of the uterine tubes. The method is carried out by introducing a warm saline solution into the cavity of the uterine cervix using a catheter, and then visually examining the penetration of the solution through an ultrasound machine.
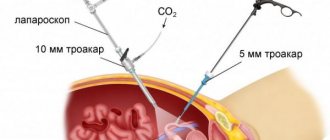
- Laparoscopy. As for diagnostic laparoscopy, this is the most inhumane and traumatic method for studying problems in the fallopian tubes. Almost always involves getting rid of adhesions, and for this reason is not performed only for testing. It is carried out by puncturing the abdominal tissues in order to introduce a special instrument that makes it possible to visually examine the organs and tissues of the reproductive system. Carrying out laparoscopy or blowing out the uterine tubes. It is used if a woman is allergic to the contrast component. It is carried out by artificially creating air pressure into the uterus through a soft tube and a pressure gauge.
- Echohysterosalpingography. Ultrasound diagnostics, which makes it possible to accurately determine the condition of the uterine body and the permeability of the fallopian tubes. Today, this method often becomes the initial step in establishing the tubal root cause of infertility, since ultrasound hysterosalpingography is characterized by a fairly good percentage of information content, along with HSG using X-ray radiation (80-91%), and is also acceptable in terms of pain and less invasive event. Echohysterosalpingography is performed in a hospital setting, in the initial phase of the menstrual cycle (when menstruation passes). A gynecological catheter is inserted into the uterine cavity, after which a contrast solution of approximately 10 to 20 ml is introduced. (saline solution, liquid glucose, furatsilin, echovist, levovist, etc.). The substance, being in the cavity, provides a visual inspection of the uterine body and makes it possible to evaluate the features of its structure much more definitely. The subsequent introduction of contrast implies its penetration into the pipes, and then into the abdominal location, which may indicate the presence of lumen and patency of the pipes. If there is impermeability of the fallopian tubes, the introduced fluid is not able to penetrate into the abdominal cavity, or accumulates in the tubes. A distinctive feature of ultrasound HSG is its auxiliary therapeutic effect. The fluid injection generated during the procedure destroys minor adhesions located in the pipes, thereby ensuring their permeability. Due to this, conception after tubal HSG becomes a very common result.
- X-ray The peculiarity of this method of study is that the woman is injected with contrast into the uterine cavity through a very thin tube. In the current realities, only components that dissolve in water are used for fallopian tube HSG: verografin, urotrast, cardiotrust. They have no side effects and are absolutely harmless to the mucous membranes of all organs of the reproductive system. After which 3 x-ray photographs are taken: Initial - immediately after the injection of the first 2-4 ml of contrast solution. It displays the shape of the uterine cavity and what its mucous membrane is like;
- The next one is immediately after additional pressure with another 3-4 ml of solution. Under the forming pressure, the contrast is directed through the pipes and, when they are permeable, appears in the abdominal location;
- Third , this image is not at all necessary; it can be performed in situations where it is necessary to study in more detail the features of the structure of the genital organs. It is carried out after half an hour from the start of the procedure.
HSG of the fallopian tubes under X-ray fixation lasts about 40 minutes. During this examination time, 10-20 ml of contrast liquid is infused into the total volume.
Using X-rays or HSG, the fallopian tubes are studied exclusively in women who are not pregnant, since radiation is always harmful for the embryo. In such circumstances, other possible methods are used, i.e. echography.
An X-ray examination can provide more information, and it is much easier to assess the current picture of the state of the reproductive organs.
However, the analysis also has some disadvantages. They are expressed in: radiation, albeit in a very small dose; possible allergic reactions to contrast liquid; physical violations of the integrity of the tissue surface, leading to bleeding.
Indications for HSG
Fallopian tube HSG is performed by gynecologists and gynecological oncologists.
Indications for the procedure are as follows:
- Tubal infertility;
- Adhesions of the pelvic organs;
- Anomalies in the development of reproductive organs;
- Sexual infantilism;
- Fibroma of the uterus, located in its submucosal layer;
- Endometrial cancer;
- Endometriotic growths in the uterine cavity;
- Polyps;
- Endometrial hyperplasia.
Hysterosalpingography is a method that will confirm that a woman has pathology of the fallopian tubes or uterus, but does not always make it possible to assess the severity of the disease and its nature. If we look at statistics, then in 98% of cases it is possible to identify an existing disorder, but a correct diagnosis can be made only in 35% of cases.
Where to do HSG of fallopian tubes in Russia
Saint Petersburg:
- SM-Clinic, a federal network of clinics for adults and children from 8600;
- SMT clinics from RUB 6,500;
- Leningrad Regional Clinical Hospital - from 4510 rubles;
- Clinical Hospital named after Peter the Great Northwestern State Medical University named after I.I. Mechnikov from 2700;
- BaltMed Ozerki, multidisciplinary clinic from 11,500 rub.
Moscow:
- Invitro diagnostic centers from RUR 8,000;
- Nixor clinic, medical center from 9,000;
- Halsmed, medical center from 2000;
- Endocrinological Research Center of the Russian Academy of Sciences from 10,000;
- Scandinavian health center from 8000 rub.
Also, HSG of the fallopian tubes can be done in large cities of Russia, namely Yekaterinburg, Nizhny Novgorod, Tula, Ulyanovsk, Omsk, Novocherkassk, Murmansk, Smolensk, Irkutsk, Krasnoyarsk, Bryansk, Novosibirsk, Sochi, Angarsk and others.
Contraindications for HSG
X-ray hysterosalpingography may not always be performed.
There are certain contraindications to the procedure, including:
- Intolerance to iodine preparations. This contraindication is due to the fact that the contrast agent, which is injected into the uterine cavity, contains iodine.
- Inflammation of the ovaries, uterus, appendages.
- Colpitis, cervicitis, bartholinitis.
- Acute infectious diseases of the body, for example, acute respiratory infections, ARVI, influenza, tonsillitis, sinusitis, etc.
- Blood clotting disorder.
- Heart diseases.
- Kidney failure.
- Severe disturbances in liver function.
- Pathologies of the thyroid gland.
- Pregnancy. A pregnancy test is required before undergoing the procedure.
- Menstrual bleeding.
- Lactation.
- Increased ESR and leukocytosis.
Why and when is HSG of the fallopian tubes prescribed?
Fallopian or fallopian tubes (oviducts) are peculiar canals connecting the uterus to the abdominal cavity. The length of the pipes is approximately 10–12 cm, their diameter is 2–4 mm.
The canals are located on both sides of the uterus, with one side of the oviduct connected to the ovary, the other to the uterus.
The fertilized egg moves through the oviducts into the uterine cavity. If an obstacle gets in her way, pregnancy does not occur.
Photo:
If the oviduct is partially patency, a fertilized cell can attach to its wall, which will cause an ectopic pregnancy.
An X-ray of the uterine tubes allows us to determine the level of patency of these canals, so hysterosalpingography is most often prescribed for women who cannot become pregnant and give birth to a child for a long time.
Today, X-ray examination of the patency of the oviduct is considered a common procedure.
Photo:
At least 2% of patients planning to become pregnant agree to undergo it, but, according to doctors, this figure increases every year.
Most likely, this fact is associated with the category of women who want to get pregnant and give birth to a child after 30–35 years.
Preparation for the procedure
Preparing for the procedure is simple, but following the recommendations given by the doctor is a prerequisite. Otherwise, you can harm your own body.
So, a woman must follow the following rules in order to properly prepare for hysterosalpingography:
- 1-2 days before the proposed test, you need to avoid intimacy.
- 7 days before the procedure, you should not douche or use intimate hygiene products inserted into the vagina.
- 7 days before the study, it is prohibited to use vaginal tablets, suppositories and ointments for treatment.
- 2-3 days before the test, you need to change your diet, refusing to eat foods that cause excess gas formation. This applies to cabbage, legumes, bread, dairy drinks, and carbonated water.
- 7 days before the procedure you should stop using tampons.
- After the end of the next menstruation, partners should use a condom to avoid conception.
It is equally important to undergo a high-quality examination before carrying out GGS. It necessarily includes the following tests:
- UAC.
- OAM.
- TANK.
- Blood test for syphilis, HIV, hepatitis.
- Vaginal and cervical smears.
Before going for the procedure, you need to remove all hair from the external genitalia and wash it thoroughly. The bladder and intestines should be empty. If you were unable to go to the toilet, you should do an enema. The procedure must be carried out on an empty stomach.
As for self-administration of painkillers, it is prohibited to use medications without consulting a doctor. If prescribed by a doctor, you can take an antispasmodic, for example, No-shpa, 30 minutes before the HSG.
When is HSG performed?
Most often, hysterosalpingography is performed within 2 weeks after the next menstruation. This is explained by the fact that during this period the mucous membrane of the uterus is small in thickness, which means it does not block the entrance to the fallopian tubes.
Although, depending on the purpose of the study, it may be scheduled at other times. To assess the patency of the fallopian tubes, it is carried out in the second half of the menstrual cycle. If there is a suspicion of internal endometriosis, it is recommended to perform HGS on days 7-8 of the cycle. Myoma in the submucosal layer of the uterus can be detected at any time, but only if the woman does not menstruate.
How is the patency of the fallopian tubes checked?
At the time of HSG, the patient is positioned on the couch.
When the procedure is carried out using x-rays, the equipment is located above it. When an ultrasound is performed, the specialist uses a vaginal sensor.
Before inserting the catheter, the doctor applies an antiseptic to the vulva, vagina and cervix.
As usual, HSG is performed without pain, but the woman will still have to feel minor inconveniences: during insertion of the tube into the vaginal cavity and while achieving fluid pressure.
The painful sensation is very similar to the nagging symptoms in the early days of menstruation. The examination is more difficult for nulliparous patients, since their uterine cervix is still dense, which may impede the insertion of the catheter.
Tests for HSG
Before the examination, you must provide biomaterials (blood, urine) for analysis and, in addition, a smear for microflora. If pathogenic microorganisms are present, performing HSG can be dangerous, since the disease can “rise” into the uterine body.
Preparation for GHA
Hysterosalpingography is best performed in the first part of the cycle, preferably in the first few days, immediately after the end of menstruation.
At this time, the endometrium of the uterus is still very thin, the cervix is more pliable, for this reason the gynecologist has a greater overview and the introduction of a fluid supply device is not difficult.
For this procedure, vaginal discharge must be completed, otherwise blood clots may change the image seen by the specialist.
Preparatory actions for fallopian tube HSG are related to the method by which the test will be performed.
HSG with x-ray
This examination is performed in the first part of the cycle of critical days, while the endometrium is quite thin and does not change the visual image. The most appropriate time is the interval between the first “clean” days immediately after menstruation and ovulation. With a 28-day cycle, this is 6-12 days.
When a referral for HSG is issued in advance, the woman is informed that from the time of the first bleeding until the day of the study, restrictions on sexual intercourse (exclusion) are required.
To carry out the procedure, the patient needs to prepare and undergo the following tests:
- General blood analysis;
- Blood for diseases such as AIDS, jaundice, gonorrhea.
- In addition, a general urine test is provided to determine the level of cleanliness of the vaginal cavity.
The day before the morning when the study is performed, it is necessary to do an enema and empty the intestines using Fortrans.
On the day of the HSG, you need to wash yourself very clean and shave your pubic hair. The examination is carried out in the morning. You cannot eat anything; you are allowed to drink no more than 1 glass of water 1.5 hours before the test.
Preparation for fallopian tube HSG right before the procedure involves the woman emptying her bladder and removing all metal objects and clothing that fall into the X-ray image area.
How is HSG performed?
If the doctor's office is equipped with a special X-ray chair, then the woman is seated on it. If there is no such chair, then the patient will be placed on a regular gynecological chair, and an X-ray machine will be brought to her.
After treating the external genitalia with an antiseptic composition, the doctor inserts speculum into the vagina and wipes the vaginal walls, first with dry cotton wool and then with cotton wool soaked in an alcohol solution. The next step is to install a tube with fixation in the cervical canal. The tube is secured with bullet pliers. When this manipulation is completed, the mirrors are removed. A contrast agent is supplied through the tube using a syringe, which must first be heated to approximately the woman’s body temperature (up to 37 °C).
When the contrast agent is evenly distributed throughout the uterine cavity and fallopian tubes, the doctor begins to take pictures. As a rule, the doctor takes from 4 to 6 pictures during the procedure. To begin with, the condition of the uterus (its relief) is recorded. Then another 4 ml of contrast agent is supplied into the cavity, which allows the appendages to be more clearly visualized. If this volume of liquid is not enough, then inject as much as necessary.
After all the pictures have been taken, the patient is transferred to the couch and left in a horizontal position for another hour. The fluid that was introduced during the procedure is absorbed into the blood and eliminated from the body by the liver and kidneys.
Examination technique
During the procedure, the patient lies on a couch or a special gynecological chair. The X-ray machine is located above it, and if echohysterosalpingoscopy is planned, the doctor uses a special vaginal sensor.
Before inserting a catheter into the genitals, the doctor disinfects the cervix, vagina and external genitalia with an antiseptic solution. The catheters and devices used in the process must be strictly sterile, and a special condom is placed on the ultrasound sensor.
Before inserting the catheter, the doctor examines the patient using a speculum. After this, a soft catheter is inserted into the cervix, through which a contrast agent is injected with a syringe. The substance enters directly into the uterine cavity and gradually passes into the fallopian tubes. At this time, the doctor takes a series of x-rays.
USEFUL INFORMATION: Causes and symptoms of ovarian dysfunction, impact on pregnancy, treatment and consequences
Echohysterosalpingoscopy of the uterine cavity follows a similar pattern: the doctor injects a saline solution into the uterine cavity, after which he carefully inserts the ultrasound device sensor.
The procedure usually does not cause severe pain or discomfort. The sensations during it are reminiscent of the pain syndrome in the first few days of menstruation. In this regard, most often, the use of anesthesia is not required. However, if the patient knows that the first days of her menstruation are very painful, and if there are no contraindications to the use of anesthesia, the doctor may administer local anesthesia before starting the diagnosis. General anesthesia is not used for this procedure.
If there is a possibility of spasms of the fallopian tubes or uterus, the doctor suggests taking antispasmodics, for example, the drug “No-shpa”. Most often, in such cases, an injection is given so that the active substance enters the blood faster.
What contrast agent is used for HSG?
To carry out the procedure, the introduction of a contrast liquid, which has the ability to block x-rays, is indicated. These are drugs such as:
- Cardiotrust. This is a contrast agent that can contain 50% and 30% iodine.
- Urotrast, Triombrast and Verografin. These are three analogues belonging to the group of radiopaque agents, which can contain 60% and 76% iodine.
Interestingly, hysterosalpingography was first attempted with Lugol's solution in 1909. But due to irritation of the peritoneal cavity and uterus, this attempt was unsuccessful. A year later, the Lugol's solution was replaced with bismuth paste, and then with argyrol and collargol. However, it was not possible to achieve the desired effect using these substances. In addition, all of them entailed inflammatory processes of the peritoneum.
It was only in 1925 that the scientist Heuser first used Lipiodol (a drug containing iodine) for hysterosalpingography. This substance made it possible to clearly visualize the condition of the uterus and fallopian tubes, and also did not harm the woman’s health. Since then, the procedure has been introduced into medical practice.
About the types of gynecological x-ray diagnostics
To understand the essence of examination methods, let's start by considering what tubal salpingography is. This terminology combines a group of gynecological studies that diagnose tubal infertility, pathology of the female reproductive system and neoplasms of various natures. For this we use:
- air purging during pertubation, kymopertubation;
- contrast agents when radiographic or ultrasound hysterosalpingography (HSG) is performed.
For the first option, the uterine cavity is filled with gas, which exits through the uterus if they are patent.
In the second case, through a cannula tube, the uterine cavity with fallopian tubes is gradually filled with X-ray contrast liquid, while X-rays are taken in parallel.
As a contrast, iodine-containing drugs cardiotrast, urotrast, and verografin are used.
Metrosalpingography to check the patency of the fallopian tubes with X-ray images takes 40 minutes.
Ultrasound HSG is performed transvaginally with contrast saline solution under the supervision of a physician in real time.
Indications and contraindications for hysterosalpingography
Depending on the purposes of the HSG examination, the appointment is made by both gynecologists and oncologists. X-ray for tubal patency is indicated for the following conditions:
- with anomalies in the development of female organs, tubal infertility (when a hormonal factor is excluded);
- with adhesions in the pelvic organs, polyps and growths of the endometrium in the uterus;
- with uterine fibroids in the submucosal layer;
- for hyperplasia and malignant tumors of the endometrium;
- if you suspect tuberculosis of the female organs, sexual infantilism;
- as a postoperative control of MT.
X-ray examination of the fallopian tubes is not carried out in a number of cases, which include:
- periods of pregnancy and breastfeeding;
- intolerance to iodine preparations;
- acute and chronic inflammation of any nature;
- liver disease, heart disease, kidney failure;
- pathology of the thyroid gland;
- suspected ectopic pregnancy;
- inflammatory diseases of the Bartholin gland, which produces a secretion that moisturizes the vagina (bartholinitis), a segment of the cervix (cervicitis), and the vaginal mucosa (colpitis);
- problems with blood clotting.
Consequences and complications of HSG
A woman should use sanitary pads for 2-3 days after the procedure. This need is due to the fact that residual contrast material may leak from the vagina. If a small amount of blood is found in the discharge, then you should not worry about this, since such a phenomenon is a variant of the norm.
Mild painful sensations, reminiscent of those that occur during the next menstrual cycle, should not frighten a woman. After HSG, such discomfort does not indicate any complications.
Also, the patient should be prepared for the fact that during or several hours after HSG, a metallic taste in the mouth, dizziness, and increased heart rate may occur. This is a normal reaction of the body to the injection of a contrast agent.
A woman should not visit a sauna or steam bath, or take a hot bath for 3-4 days after undergoing HSG.
You should be concerned and immediately consult a doctor if your body temperature rises, heavy bleeding or severe pain in the lower abdomen.
Extensive blood loss, infection, perforation of the uterus and fallopian tubes during the HSG procedure are extremely rare in modern gynecological practice, as an exception.
A woman should avoid pregnancy for the next 3 months. For protection, you should use a condom.
As a rule, the procedure is well tolerated, but only on condition that the preparation for it was carried out efficiently: inflammatory processes were identified in time, and there are no other contraindications to HSG.
When is the best time to perform X-ray and HSG using ultrasound?
Most often, X-rays of the tubes are performed immediately after the end of the next menstrual bleeding. During this period, the layer of the uterine epithelium is the thinnest, which allows you to examine the uterine cavity in detail. In addition, in the first few days after menstruation, the cervix is still very soft, which means it will be easier to insert a catheter into it to inject contrast or saline solution. But the exact date of the study must still be set by the doctor, based on specific clinical indications. Most often, X-ray HSG is performed between the first day of the end of menstruation and expected ovulation. With a 28-day cycle, the best time for HSG is from days 6 to 12.
The time frame looks a little different if hysterosalpingography is planned to be performed using ultrasound. In this case, it all depends on the expected diagnosis:
- if uterine endometriosis is suspected, echo-HSG is prescribed on days 7-8 of the cycle;
- if tubal obstruction and/or isthmic-cervical insufficiency is suspected - in the second phase of the cycle, that is, after ovulation;
- if submucosal uterine fibroids are suspected, an ultrasound can be performed on any day of the cycle. The only limitation is that neither x-rays nor ultrasound are ever done directly during menstruation.
Evaluation of results
The doctor must interpret the results based on the images obtained.
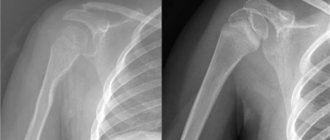
Signs of various diseases on an x-ray picture are as follows:
- Noticeable asymmetry of the uterus is a diagnosis of “unicornuate uterus.”
- An elongated cervix and a pronounced decrease in the volume of its cavity is a diagnosis of “infantile uterus.”
- Short, long, or asymmetrical fallopian tubes are diagnosed as “congenital tubal obstruction.”
- The presence of a flask-shaped expansion in the tubes is a possible diagnosis of “tubal adhesions”, or “sactosalpinx”, or a combination of these two diagnoses.
- The presence of light areas in the tubes is “fallopian tube adhesions.”
- The shape of the fallopian tubes, reminiscent of the shape of smoking pipes, the presence of flask-shaped extensions in them, a decrease in the volume of the uterine cavity - the diagnosis of “genital tuberculosis”.
- Uneven contours of the uterus, detection of oval or other shaped defects - diagnosis of “uterine polyps” or “endometrial hyperplasia”.
Of course, only the most obvious and common signs of certain diseases were listed. Only the attending physician can make a final diagnosis, assessing the entire range of results obtained in the course of various studies.
Reasons contributing to the occurrence of exudate
Tubal obstruction is a condition where an obstruction occurs that prevents the passage of an egg. In these cases, as a rule, the normal anatomical structure of the pipe is disrupted, and kinks or adhesions are formed.
In the presence of functional obstruction, there are no organic defects, but the advancement of the egg is impossible due to spasms of the fallopian tube, possible adhesion of the walls to each other, and impaired peristalsis.
Obstruction occurs, first of all, in the presence of inflammatory processes in the mucous membrane of the uterus or fallopian tube. In the future, they may be complicated by the formation of adhesions. The occurrence of inflammation itself is quite possible after an abortion, by curettage of the uterine cavity.
Adhesions in the lumens of the tubes or at the points of their connection with the uterine cavity are most often formed under the influence of chronic inflammation that lasts for more than six months. They replace the dead normal tissue with a film or cords consisting of connective tissue.
In some cases, adhesions cause the pipes to become kinked or misaligned. Because of this, their functioning deteriorates, the ability of the walls to contract decreases, and peristalsis is disrupted. The chances of an egg reaching the uterus are significantly reduced.
Timely diagnosis helps to quickly eliminate the root cause of the disease. When a mechanical obstacle in the form of a formed filled cavity is present in one tube, then the chances of getting pregnant always remain.
- abnormalities in the development of the reproductive organs (for example, sexual infantilism, manifested by thinning and tortuous fallopian tubes);
- diseases of the appendages (ovaries) in the form of salpingitis, adnexitis;
- inflammatory processes in the uterine cavity (endometriosis);
- inflammation in the cervix and cervical canal (ectropion, erosion, endocervicitis);
- infection with pathogenic flora (bacteria, viruses and fungi) as a result of frequent changes of sexual partners;
- sexually transmitted diseases (existing or present in the past);
- infection with Mycobacterium tuberculosis;
- surgical intervention on the pelvic organs, provoking inflammatory reactions and the development of adhesions;
- use of intrauterine contraceptives (spiral, cap);
- the presence of myomatous nodes in the uterine cavity and tubes;
- long-term inflammatory diseases of the vagina, changing its flora;
- previous abortions, miscarriages;
- ectopic pregnancy;
- curettage of the uterine cavity for diagnostic or preventive purposes;
- the presence of systemic diseases of the pelvic organs;
- general hypothermia of the body and pelvic organs;
- stress factor.
As stated above, hydrosalpinx is a consequence of the course of a disease. The longer a certain disease develops in a woman’s body, the more difficult it will be for her to tolerate the accumulation of fluid in the fallopian tubes. What leads to such a pathology?
- Inflammations such as salpingoophoritis, adnexitis.
- Infections living in the genitals. For example, Trichomonas, chlamydia, gonorrhea, syphilis.
- Various tumors of the uterus and appendages. This means both benign and malignant.
- Operations that were performed in the pelvic organs and subsequently resulted in mechanical damage.
Cons of GHA
The disadvantages of the procedure are the following:
- A woman receives a dose of radiation, albeit a small one.
- The likelihood of an allergic reaction to the administered contrast agent. Particular caution should be exercised by women with a history of bronchial asthma, as well as allergic patients.
- There is a risk of mechanical damage to the epithelial layer of the uterus, which leads to the appearance of bloody discharge.
Advantages of conducting HSG at the Doctor Nearby clinic
HSG must be carried out by an experienced specialist who strictly follows all the rules for its conduct. This will eliminate the risk of complications and unpleasant symptoms. Specialists from the Doctor Nearby clinic network have successfully carried out this procedure hundreds of times. They have everything they need to make it successful and effective.
You can find out the price of hysterosalpingogography in our clinic on this page of our website or by calling us by phone. Trust your health to professionals, contact Doctor Nearby!
Pros of GHA
In addition to the fact that X-ray HSG is highly informative, it has another important advantage. The fact is that hysterosalpingography is not only a diagnostic, but also a therapeutic method of influencing the female body. It has been established that approximately 20% of women who suffered from infertility successfully become pregnant after undergoing HSG.
Doctors explain this fact by the fact that during the procedure it is possible to improve the patency of the fallopian tubes, since the injected substances “wash” them, eliminating small adhesions.
Author of the article:
Lapikova Valentina Vladimirovna |
Gynecologist, reproductive specialist Education: Diploma in Obstetrics and Gynecology received from the Russian State Medical University of the Federal Agency for Health and Social Development (2010). In 2013, she completed her postgraduate studies at NIMU named after. N.I. Pirogova. Our authors
Why is hysterosalpingography needed?
This study helps to identify a wide range of uterine diseases, as well as assess the patency of the fallopian tubes. X-rays using contrast can detect:
- Developmental anomalies: duplication of the uterus, the presence of an intrauterine septum, etc. Normally, the uterine cavity looks like an isosceles triangle, facing downward.
- Neoplasms: polyps, fibroids, cancer. On x-rays they are visible as filling defects, that is, areas not filled with contrast. An uneven, “corroded” contour indirectly indicates the malignancy of the process. However, cancer can only be reliably diagnosed based on the result of a biopsy.
- Endometriosis of the uterus (a pathology in which cells of the mucous layer - the endometrium - grow beyond its boundaries). The image will show shadows behind the contour of the uterine cavity in the form of streaks, pockets, and lacunae.
- Changes in the shape of the uterus and filling defects may indicate synechiae - intrauterine adhesions.
Hysterosalpingography plays an important role in assessing tubal patency. Normally, the contrast, having filled the uterus and appendages, enters the abdominal cavity. If there is an obstacle, there are no signs of its spreading in the area of the ampullary part of the pipe.
Hysterosalpingograms
What does the contrast delay look like on an x-ray:
- Bonding of the ampulla facing the abdominal cavity as a result of inflammation or compression by adhesions is characterized by the accumulation of a contrast agent in the tube. The picture will show that the latter is flask-shaped expanded. The distal (ampullary) section is especially stretched. In this case, the contrast may partially flow into the abdominal cavity if the exit from the tube is not completely blocked.
- Blockage at the level of the intramural section, located in the thickness of the uterine wall, is characterized by its pronounced narrowing or complete absence of contrast staining of the rest of the tube.
- In tuberculosis, changes affect the ampullary and intramural sections. The first one usually undergoes obliteration, that is, it narrows, the second one expands. In the photograph, the fallopian tube takes the shape of a smoking pipe. Deformation of the uterine cavity due to tuberculous endometritis is often observed.
The reasons for the delay of contrast in the tube, therefore, may be the consequences of inflammation, some infections (tuberculosis), and adhesions in the pelvic cavity. The latter often occur after surgery.
HSG X-ray: how harmful is it?
Women are sometimes concerned about the consequences of metrosalpingography, since the X-ray examination involves exposure to radiation. The average dose for HSG is considered to be 2.8-4.6 mGy, which cannot cause serious harm to the patient. Only for pregnant women this is a dangerous dose that can cause mutation in the cells of the fetus, which is unacceptable. In general, hysterosalpingography is considered a safe procedure. It rarely leads to serious consequences associated with severe pain in the lower abdomen and allergies to contrast fluid.
The appearance of bloody discharge is considered a common occurrence after HSG, and patients are warned about this in advance. A similar symptom is associated with trauma to the epithelial tissues of the female organs during the session. The factor of bacterial infection and the occurrence of delayed menstruation cannot be excluded.
About alternative examination methods
Contrast ultrasound hysterosalpingography (ECHOGG) was mentioned above as a type of diagnosis carried out under the visual supervision of a doctor without pictures. The contrast agent in this case is a 0.9% sodium chloride solution and it appears black on the monitor.
Identification of formations in the uterus and tubes occurs on the principle of differences in the echogenic properties of different tissues and the contrast effect on the screen in gray shades. There is an echocardiography technique in which the drug “Ekhovist” is administered, which visualizes the MT without small pathological inclusions. This contrast produces a white image on the ultrasound machine monitor.
This examination is also performed using magnetic resonance imaging (MRI), which uses the properties of electromagnetic waves.
Considering the high cost of sessions and the complexity of MRI studies to identify the causes of lack of reproduction, it is rarely prescribed, for example, in cases of multiple uterine fibroids, agenesis (absence) of the ovaries.
An alternative is the chromosalpingoscopy technique, when the fallopian tubes are examined during laparoscopy using contrast.
Pregnancy after having your tubes checked
Doctors do not have an exact scientific basis for why pregnancy develops after HSG. Statistics indicate that this procedure actually increases the percentage of a woman’s ability to conceive a child. This happens especially often when testing for tubal patency is carried out using oil contrast agents. For this reason, some delay in menstruation after HSG may indicate not only the stress the woman has endured, but also a possible pregnancy, which you should definitely check.
What is hysterosalpingography (HSG) in gynecology
Hysterosalpingography (HSG) is an x-ray or ultrasound of the fallopian tubes and uterus, which allows you to assess their patency and identify the cause of the impossibility of conception. The procedure is carried out when pregnancy does not occur for a long time, and doctors do not detect objective factors for the occurrence of pathology when using other diagnostic procedures.
1-2% of modern women undergo such examination in gynecology, but there is a tendency to increase the rates.
Hysterosalpingography, an X-ray in which does not lead to a high radiation dose, is one of the best X-ray examinations for determining the patency of the uterus and tubes. The procedure raises many questions from patients: “HSG - what is it,” “HSG is painful,” “is it possible to get pregnant after hysterosalpingography.” You will find the answers to them below.
What does an x-ray show?
Hysterosalpingography is a research method that can be used to identify a number of diseases of the fallopian tubes and uterine cavity in the early stages.
X-rays visualize the female reproductive organs, with:
- If the patency is normal, the contrast liquid will spread throughout the abdominal cavity and will resemble cigarette smoke in the image.
- If patency is hampered by adhesions, scars or inflammation, then flasks will be clearly visible on the radiograph instead of tapes.
- When the tubes become obstructed, exudate accumulates in the oviducts—liquid that cannot escape due to impaired permeability of the vessel walls. The contrast mixes with it and shows that there is an enlargement of the ampullary portion of the fallopian tube.
What contraindications does the procedure have?
Due to the fact that this diagnostic method involves the introduction of a contrast agent or saline solution into the uterus and tubes, and the classical examination, moreover, is associated with X-ray irradiation, hysterosalpingography is not prescribed:
- at the slightest suspicion of pregnancy;
- with hypothyroidism;
- in the presence of diagnosed renal or liver failure, liver cirrhosis;
- for acute inflammatory processes in the genital organs, inflammation of the vagina and vulva;
- with uterine bleeding;
- if you are allergic to contrast agents;
- in the general serious condition of the patient;
- for infectious diseases of the genital organs;
- with thrombophlebitis and acute heart failure.
In what cases is a patient prescribed an examination?
The most common indication for hysterosalpingography is infertility. If a woman who does not have previously diagnosed reproductive health disorders cannot become pregnant within a year, with one regular sexual partner, without using contraceptive methods, a gynecologist or reproductive specialist can refer her to this type of study.
Other indications for the procedure:
- presence of previously diagnosed uterine pathologies;
- malformations of the uterus and fallopian tubes;
- suspicion of cancer;
- the likelihood of tuberculosis of the genital organs;
- a history of pregnancies that ended in miscarriage or fetal death.
The uterus and fallopian tubes: what they are responsible for in the body
The uterus is an unpaired hollow internal organ, one of the main functions of which is the development of the embryo and gestation of the fetus. Anatomically, the organ is represented by the bottom, body and neck, with the neck being at the bottom and representing a narrowing of the organ, and the bottom is located at the top. The place where the uterus meets the cervix is called the isthmus. The lower part of the cervix passes into the vagina, and the upper part lies above it. The body of the uterus has anterior and posterior surfaces. In front of it is the bladder, behind it is the rectum.
Content:
- The uterus and fallopian tubes: what they are responsible for in the body
- What is hysterosalpingography
- In what cases is a patient prescribed an examination?
- What contraindications does the procedure have?
- Preparation requirements for hysterosalpingography
- Examination technique
- Diagnostic results: what to do next
- Possible complications and consequences of the procedure
The size of the organ and its mass change throughout a woman’s life. The length of the uterus in an adult woman reaches 7-8 centimeters. The weight of a nulliparous woman does not exceed 50 grams, and that of a woman who has given birth does not exceed 80-80 grams.
Fixation in the pelvic area occurs due to the left and right broad ligaments, round ligament and cardinal ligaments of the uterus.
The organ, which has the shape and appearance of a pouch, is formed by three-layer walls. The inner layer is a mucous membrane covered with ciliated epithelium. From the outside, the organ is covered by a serous membrane, and in the middle the wall is formed by muscle tissue.
It’s not for nothing that the fallopian tubes got their name – these organs look like hollow tubes. There are two of them in a woman's body. The length of each tube ranges from 10 to 12 centimeters, the lumen diameter is up to 2-4 millimeters. The uterine, or fallopian, tubes are directly involved in the reproductive process - through them the egg from the ovary passes into the uterus, in it the moment of fertilization of the egg by the sperm occurs, and the embryo moves through the tubes to the uterus. The organs are located on the sides of the fundus of the uterus, their narrow end opens into its space, and their wide end opens into the abdominal cavity, that is, the tubes connect the abdominal cavity and the uterus.
Their structure is presented:
- funnel;
- ampoule;
- isthmus;
- uterine part.
The structure of the wall of the fallopian tube is similar to the wall of the uterus: it also contains three layers (serous, muscular, mucous).
The ability to diagnose tubal patency, as well as check the condition of the uterus, gives women who cannot conceive or carry a baby a chance to become pregnant and give birth to a healthy child.
Where can I get an X-ray of the pipes and how much does it cost?
Hysterosalpingography is a fairly common diagnostic method that is widely used both in public clinics (free of charge) and in private ones. The cost of HSG in private medical institutions, as a rule, ranges from 3,500 to 5,000 rubles. GHA using ultrasound examination will cost an order of magnitude more expensive – from 5,000 to 8,000 rubles.
The indicated prices can be considered only conditional, because the upper limit for the cost of the procedure can rise much higher. It all depends on the list of additional services that the clinic offers:
- consultation;
- anesthesia;
- presence of relatives at the procedure, etc.
Tubal obstruction is one of the seven most common causes of infertility. According to various sources, almost every fourth childless woman faces this diagnosis, but with timely diagnosis, it is not a death sentence. Doctors advise not to be afraid of pain and to decide on the procedure as early as possible. By choosing a clinic with precise modern equipment and qualified staff, you will learn everything about the condition of the organs of your reproductive system and will be able to choose the right treatment tactics.
What is the essence of the procedure?
To see the condition of the uterus and fallopian tubes on an x-ray, a special iodine-containing contrast agent is injected into their cavity through the vagina, which reflects x-rays. Then, using an x-ray, the doctor can see tumors, adhesions, inflammation - any pathology - in the image. Another goal is to determine whether the contrast that was infused through the vagina has exited through the fallopian tubes into the abdominal cavity. This will make it possible to judge the patency of the pipes.
In addition to HSG X-ray of the fallopian tubes, there is another type of hysterosalpingography - echo HSG, which is done using ultrasound. The meaning is the same. The only difference is that during an x-ray the doctor introduces contrast in portions to take several different pictures and track the dynamics, but during an ultrasound examination there is no such need - everything that happens in the pelvic and abdominal area is clearly visible on the ultrasound monitor. device in real time. Therefore, instead of contrast, saline is administered, and not gradually, but in one continuous stream.
Sometimes, this also has an additional therapeutic effect: under the pressure of a stream of saline solution, small adhesions can be smoothed out. Therefore, if only minor pathology interfered with conception, then it can easily be eliminated directly during HSG. It is not surprising that after such an ultrasound, many women finally become pregnant. Spontaneous conception also occurs after an x-ray, especially if an oil-based contrast agent was used during the procedure.
But doctors note: despite the possible beneficial therapeutic effects of echo-HSG, x-ray is still a more informative method and allows you to reproduce a more complete and accurate clinical picture. For example, if due to a spasm the walls of the tube are pressed against each other, on the ultrasound monitor it will look like a commissure and the doctor may misinterpret the result. It is not uncommon that after an ultrasound, the patient is again sent for an x-ray.
Consequences of hysterosalpingography
The consequences of x-ray of the fallopian tubes can be as follows:
- Temperature over 37.5 degrees requires immediate medical attention.
- Pain in the lower abdomen for more than 3 days. Occurs if the patient experienced inflammatory processes in the reproductive organs before the procedure.
- Bloody vaginal discharge for more than 3 days. In the vast majority of cases, they occur in patients with cervical erosion. Normally, discharge stops on the second day after the examination.
- Allergic reactions: dizziness, fainting, nausea, rashes and spots.
- The contrast agent itself can cause irritation when it enters the abdominal cavity. In this case, the pain is cramping in nature.
Most often, the procedure takes place without consequences or complications. The radiation dose received during an X-ray examination is negligible. It does not affect women's health in any way.
For three days after the procedure, doctors recommend refraining from visiting the sauna and having sexual intercourse.