Laparoscopy is one of the most modern methods of diagnosis and treatment of gynecological pathologies. It is allowed to conduct a visual examination of the woman’s internal genital organs and, if necessary, carry out certain medical manipulations. The big advantage of using this method for treatment is minimal trauma to tissues and organs with high efficiency of the procedures performed.
What is laparoscopy?
Laparoscopy is a surgical procedure performed under anesthesia. In severe cases, artificial ventilation and total muscle relaxation are possible. The procedure requires careful preparation from patients, taking into account how it will be carried out: planned or emergency.
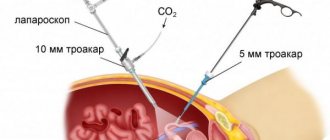
The meaning of the procedure is to make small incisions on the skin up to 10 mm, insert a short trocar with valves into the peritoneal cavity with carbon dioxide, and additionally a video camera with a color image. Such visualization makes it possible to control the lower lateral sections of the anterior abdominal wall.
In their work, doctors use manipulators—instruments (electrodes, scissors, clamps) to move the ovaries and fallopian tubes to the sides to give the desired position, move intestinal loops, coagulate bleeding vessels, and cut adhesions.
Main stages of laparoscopy
- General anesthesia is used to perform laparoscopy. Small incisions (about two centimeters long) are made on the skin, after which they are deepened using a blunt probe, thereby preventing damage to internal organs.
- One operation usually requires three or four holes. The introduction of sterile surgical instruments is carried out through special tubes inserted into the holes.
- To straighten the abdomen and provide maximum access to the internal organs, carbon dioxide is injected through one tube.
- A video camera and surgical instruments are inserted into other tubes.
- The video camera transmits the image of the operated organs to the monitor screen, which provides the doctor performing the operation with visual control over his actions.
- After all necessary actions have been completed, the instruments are removed and sutures are applied to the incision sites.
How are the fallopian tubes arranged?
The process of fusion of sperm with an egg occurs directly in the fallopian tubes. If some obstacle or condition arises along the way - obstruction due to clogged pipes, abnormal location, then childbearing in women may become questionable.
If a pathological process occurs in the fallopian tubes, we can talk about the development of infertility.
The fallopian tubes are a small and rather narrow paired organ, when blockage can lead to obstruction and problems with conception. An inflammatory process develops when it is no longer possible to do without surgery or laparoscopy, which is often used by surgeons today to solve problems with infertility in women.
Structure of the fallopian tubes:
- The fallopian tubes are a paired tubal organ. Length - 12 cm, width - 0.5 cm. Discharge begins from the lateral corners of the uterine cavity, then with a gradual divergence to the sides, adjacent to the walls of the pelvis. The main role of the pipes is transportation, through which sperm and eggs move. It is in the ampullary part that fertilization occurs.
- The structure of the tubes adjacent to the uterus is layered, consisting of 3 layers: internal mucous, middle muscular and external serous. Each of them plays a pushing role for the egg with advancement into the uterine cavity.
- At the end of the widest part of the tube there is a funnel containing many ISO fimbriae of varying lengths. The longest of them are in close contact with the ovaries, located on both sides of the uterus.
- Inside the ovaries there is a cavity designed for the maturation of germ cells, the production of progesterone and estrogen - as the main female hormones. 1 follicle with the release of a hollow mature egg matures in about 1 month. The fimbriae at the ends of the funnels help the egg to enter the fallopian tube. If she meets a sperm, then fertilization is quite possible.
REFERENCE! The sperm must penetrate each of the membranes of the egg for conception to occur. Only in this case a zygote is formed as the sperm penetrates. This is a fertilized egg with a gradual start of division into daughter cells, passing through the tube and producing a secretion. Due to the ciliated epithelium, it enters the uterine cavity, penetrates into the prepared endometrium and develops directly in the uterine cavity on the 7-8th day from the moment of fertilization.
Contraindications for salpingectomy
Surgical intervention for fallopian tubeectomy is carried out using two methods:
- Laparotomy . This technique involves abdominal dissection (up to 15 cm).
- Laparoscopy . The operation is carried out using an endoscope; three small incisions are made to carry out the instrumentation.
The laparoscopic method is very well tolerated, complications are rarely observed during its implementation, and it causes minimal trauma to the woman’s body. The recovery period does not take much time, and the woman very quickly returns to her usual lifestyle.
However, there are some contraindications that limit the use of this surgical technique.
These include:
- Increased risk of bleeding during surgery.
- Intolerance to general anesthesia.
- Inflammatory processes of an infectious nature.
- Nutritional obesity stage 2 or 3.
- Severe forms of adhesions and scar changes in the abdominal area.
- Skin diseases.
- Previous myocardial infarction or stroke.
- Malignant neoplasms.
- Severe diabetes mellitus.
- A large embryo that may threaten to rupture the fallopian tube.
If laparoscopic surgery is not possible, abdominal surgery (laparotomy) is used.
Preparing for surgery
Before surgical treatment for fallopian tubeectomy, a woman must undergo a comprehensive examination.
She is prescribed:
- X-ray of the lungs, with a detailed description of the result.
- Clinical and biochemical blood test.
- Urine examination.
- Laboratory tests for the presence of hepatitis, HIV infection, syphilis.
- Mandatory determination of blood group and Rh factor.
- An electrocardiogram is prescribed, followed by consultation with a therapist or cardiologist.
- Ultrasound examination of the pelvic organs.
- Gynecological smear for pathogenic microflora from the vagina.
- Before surgery, it is necessary to shave the groin area and perineum.
- One day before the operation, give a cleansing enema in the morning and evening.
- On the eve of the operation, do not eat food after 18 hours.
- Do not use oral contraceptives and aspirin during the day before surgery.
The essence and conduct of the operation
If there are no contraindications, preference is given to the laparoscopic method of surgical intervention. Such an operation is possible if the clinic has the necessary equipment and the gynecologist has the skills to use this technique.
But if a rupture of the fallopian tube occurs with subsequent hemorrhage into the retroperitoneal space, this poses a threat to the patient’s life (peritonitis develops). Then they resort to laparotomy. This condition requires urgent surgery.
Operation tactics:
- The operation takes place using anesthesia and is carried out in stages.
- To do this, an incision is made below the navel.
- The blood that spills into the peritoneal cavity is collected in a container (it is transfused after surgery).
- Eliminate bleeding using clamps.
- After this, the pipe is cut off.
- Carrying out measures to sanitize the abdominal cavity with subsequent suturing of the dissected tissues.
The same sequence is followed when performing laparoscopy, with the difference that the blood that accumulates in the peritoneal cavity is not collected and, as a result, is not transfused to the sick woman after the operation.
If we compare these two types of surgical treatment, it can be noted that laparoscopy has certain advantages:
- The operation is low-traumatic and does not cause psychological discomfort.
- After it is completed, there is a short period of rehabilitation (the woman is discharged from the hospital on the 5th day).
- After the operation there are no significant scars left on the skin.
Complications after tubal removal
Undesirable consequences sometimes occur after a fallopian tubeectomy. They help to increase the postoperative recovery period.
Typically this may occur:
- Attachment of a secondary infection. The patient's body temperature rises and symptoms of intoxication are observed.
- Internal hematomas may appear. They arise due to insufficient coagulation (cauterization) of blood vessels.
- Due to the use of anesthesia, vomiting may occur within 3 days. Sometimes it occurs as a result of intestinal irritation, because during laparoscopy carbon dioxide is introduced into the retroperitoneal space.
- After surgery, vaginal discharge in the form of blood clots may occur. This occurs due to the fact that blood entered the uterine cavity during surgery.
- There may be a sensation of pain due to the development of adhesions.
- Sometimes cystic growths appear.
Rehabilitation period after ectomy
After this operation, the main priority in the rehabilitation period is to prevent the appearance of adhesions and keloid scars.
To do this, a woman needs:
- Take a course of antibacterial therapy and, to prevent the development of an infectious, inflammatory process.
- At the end of the operation, special gels are introduced into the peritoneal cavity , which allow the internal organs not to touch, and to be located at some distance in relation to each other.
- The operated woman needs to get up the next day after surgery (move independently to the toilet, to the bathroom).
- On the second or third day, start taking walks , first around the ward, and then going outside. This will speed up the healing process while rehabilitation lasts.
- In the first days after surgery, completely eliminate heavy lifting and physical strain on the abdominal muscles. This may cause damage to the integrity of the seams.
- Mandatory prescription of physiotherapeutic procedures (iodine and zinc in combination with electrophoresis).
- In parallel with antibiotics, biostimulants (Aloe, Longidaza) are prescribed.
- For 6 months, oral contraceptives are prescribed to prevent pregnancy.
- If pain occurs, you can take medications from the analgesic group or antispasmodics (Baralgin, Analgin, Ketanov, Spazmalgon, Noshpa, Spazgan).
- Caring for postoperative sutures does not allow the use of a bath. Only showers are allowed. In this case, water should not be allowed to enter the area of the postoperative suture.
- cotton underwear
- You cannot have sex for a month after surgery.
- You need to follow a diet. The diet should not include foods that cause increased gas formation (flatulence ).
After surgical therapy, vaginal discharge usually occurs. This is a normal process if they do not contain purulent contents.
With rapid adaptation of the body, after several days the woman begins the menstrual cycle (it can have a longer duration). If its onset is accompanied by large blood losses, a blood transfusion and curettage of the uterine body may be prescribed. Early menstruation is not a sign of the development of a dangerous pathology.
Egg relocation after fallopian tubeectomy
Ovulation occurs in both the left and right ovaries. Afterwards, the egg penetrates into the peritoneal cavity, where it is captured by fimbriae within 2 days.
If one appendage is missing:
- Ovulation may be absent, resulting in the appearance of atretic follicles. They have the opposite development.
- The death of the egg occurs.
- Possible movement along the abdominal cavity in the opposite direction to another fallopian tube.
- If ovulation occurs on the other side where the operation was performed (salpingectomy), then the capture of the egg occurs much faster.
If surgery was performed to remove two pipes, only the first options may develop.
Onset of the menstrual cycle after surgery
If the surgical intervention was carried out efficiently, and the rehabilitation period passed without complications, then after a few days the next menstrual cycle may occur.
It can occur with a large amount of blood released and last for a long time.
In some cases, after salpingectomy, the first menstruation can lead to heavy blood loss. This gives grounds to perform curettage of the uterine body and prescribe a transfusion of blood and its components.
This development of menstruation is rare. Usually they come on time and occur in a normal rhythm. Very rarely, it takes a couple of months for them to recover. This should not cause a feeling of anxiety, because it is not a pathology.
It should be noted that if the menstrual cycle has not returned within 3 months, this is a serious reason to visit the doctor. Since the appearance of such a symptom may mean that surgical therapy has led to a failure of the proper functioning of the endocrine system.
Consequences of a fallopian tube ectomy
The body of the uterus and the fallopian tubes have a common innervation; their blood supply is carried out using the same vessels. Also, they are connected by one bra.
As a result, during a fallopian tubeectomy, the body’s hormonal levels are sometimes disrupted, and the normal functioning of the adrenal cortex and thyroid gland changes.
With hormonal imbalance, the following may appear:
- Migraine headaches.
- Violation of the psycho-emotional state, periods of irritability can be replaced by a decline in mood and the appearance of tearfulness.
- Pain and discomfort behind the sternum in the heart area.
- Increased sweating.
- Frequent flushing of blood to the face and upper parts of the body.
These symptoms may intensify before the onset of menstruation.
In some women, after surgery, after 3 months, the menstrual cycle may change. It may alternate with irregular periods.
The ovary, from the side of the removed fallopian tube, becomes sclerotic. This is clearly visible on ultrasound.
Some women may experience changes in the mammary glands:
- Their coarsening begins.
- Hypertrophy is noted.
- The thyroid gland enlarges.
- Sometimes weight gain occurs, and male-type hair growth occurs (hair grows on the face and body).
This clinical picture may be intensified if surgery was performed for an ectomy of two tubes.
Laparoscope - instruments
Laparoscopy is a modern surgical technique for intervention on the fallopian tubes. Small incisions are made in the front of the peritoneum, and a laparoscope is inserted to visualize the entire uterine cavity. In their work, doctors use 2 types of special instruments - an endoscope and a laparoscope.
The first group includes:
- monitor for regulating the operational process;
- laparoscope with a video camera to increase the size of the peritoneal cavity;
- insufflator by delivering a stream of gas into the peritoneum;
- irrigator-aspirator for the purpose of washing the operated area.
Laparoscopic instruments include:
- stylets for the purpose of spreading the dissected tissue to the sides;
- needles, needle holders for connecting (fastening) fabrics;
- electrodes for the purpose of cauterization of affected areas;
- clamps for clamping blood vessels;
- clip-like devices to stop bleeding;
- trocars in the form of special tubes to maintain tightness in the peritoneal cavity.
Laparoscopy is a low-traumatic technique and rarely leads to complications. The recovery period is no more than 3 hours. The very next day the woman can go about her daily activities.
Thanks to special instruments, doctors are able to examine not only the condition of the pelvic organs externally, but also the uterine cavity together with the appendages from the inside.
Possible causes of adhesions
Narrowing of the fallopian tubes does not occur on its own.
There are reasons why this pathological process develops:
- Constant inflammation in the uterus and appendages. Bactria, which spread after the occurrence of inflammation, penetrate the uterine cavity and invade the appendages. The inflammation becomes chronic, leading to tubal adhesions.
- Gonorrhea, trichomoniasis, ureplasmosis affect the fallopian tubes, causing them to narrow in several places. Urogenital infections do not go unnoticed, leading to the need to perform laparoscopy.
- Adhesions can occur after abortions or operations to remove an inflamed appendix. Surgical intervention in a woman’s reproductive organs entails the formation of adhesions.
Robot da Vinci
Previously, doctors restored the patency of the uterine uterus by cutting the anterior part of the peritoneum and performing techniques such as tubectomy, salpingectomy, which led to complications and the formation of a new adhesive process.
And today the operation is performed even with minor obstruction of the egg or minor damage to the fimbriae. Moreover, pregnancy after laparoscopy occurs in 60% of cases.
Today, doctors often resort to a surgical robot as a high-tech method with the presence of 4 robotic arms (3 – instruments, 4 – video camera) and displaying high-quality images on the monitor.
A device with a control unit makes it possible to control and control the robot as a whole. For doctors, this is assistance in carrying out surgical laparoscopic procedures to restore tubal obstruction.
The advantages of such a system:
- suppression of sudden movements of the surgeon’s hands during manipulations;
- carrying out extremely smooth movements (without jerking), since all the necessary actions will be performed only by the robotic arm;
- painlessness of the procedure;
- reduction of the temporary postoperative period;
- eliminating the risk of infection in the postoperative period
- minimizing possible complications;
- eliminating the risk of bleeding;
- minimizing the morbidity of the operation.
Features of nutrition during the recovery period
The first day after laparoscopy surgery, you are prohibited from eating. When the anesthesia wears off, you can drink clean, still water. You can eat after surgery on the second day. Food should be liquid in consistency and at room temperature. Low-fat broths, yoghurts, jelly, fruit drinks, compotes are allowed.
On the third day include:
- porridge with water;
- fermented milk products – kefir, cottage cheese, yogurt, low-fat cheeses;
- easily digestible fruits and berries without peel - apples, bananas, apricots, strawberries, melons and others;
- steamed vegetables - zucchini, peppers, carrots, eggplants, beets, tomatoes;
- seafood;
- boiled eggs;
- whole wheat bread;
- dietary meat and fish in the form of minced meat dishes.
By the end of the week, restrictions are reduced to a minimum. For a month, during the recovery period after laparoscopy, the following are excluded from the diet:
- Fatty, spicy, smoked food. The meat is baked, cooked in a double boiler or slow cooker. Soups are made without frying. Sausages, fatty fish, canned food, marinades, and pork are prohibited. Preference is given to chicken, rabbit, turkey, and veal.
- Products that cause gas formation. Exclude legumes (beans, peas, lentils), raw milk, baked goods (white bread, buns, any homemade pastries), and confectionery.
- Alcohol and carbonated drinks. It is allowed to drink weak tea, fruit drinks, compotes, and still mineral water. It is better to avoid juices, especially store-bought ones, as they contain citric acid and sugar. All alcoholic beverages are completely prohibited for a month. It is also advisable to avoid coffee after laparoscopy - starting from the second week, you can only drink weak coffee without cream.
Important! Doctors do not have a unanimous opinion about cigarettes. Some categorically prohibit smoking for 3–4 weeks, since nicotine and heavy metals slow down regeneration and provoke bleeding. Others believe that abruptly giving up a bad habit and the resulting withdrawal syndrome, on the contrary, can aggravate the patient’s condition.
Throughout the entire rehabilitation, especially in the first few days, meals should be fractional. You need to eat in small portions 6 – 7 times a day. It is necessary to monitor the regularity and consistency of stool. Make up a balanced and nutritious diet. Food products must contain all the necessary vitamins, minerals, and elements. The exact diet is selected by the attending physician, taking into account the specific disease and individual characteristics of the patient.
Indications for use
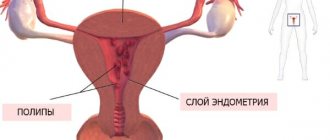
Laparoscopy on the tubes in the uterine cavity is prescribed when a preliminary diagnosis is made in women - infertility or of unknown origin, when it is necessary to establish an accurate diagnosis.
Main indications:
- development of inflammation in the appendages due to STIs, chlamydia;
- salpingitis;
- previous abdominal intervention in the pelvis, which led to an adhesive process;
- the presence of peritubar adhesions;
- infertility treatment;
- ectopic pregnancy;
- obstruction of pipes, blockage;
- hydrosalpinx, which prevents pregnancy;
- deterioration in quality, decrease in the thickness of the lining layer of the endometrium;
- sterilization to protect against unwanted pregnancy, method of contraception.
Adhesive process
In the pelvic area and tubes, adhesions can provoke:
- dense proliferation of pathological connective tissue;
- inflammatory process;
- surgery performed the day before on the genitals, abdominal peritoneum.
This leads to modifications in the structure of the uterus and the development of infertility. Connective tissue grows and lines the pipes from the inside. The adhesive process begins to develop, preventing sperm from meeting the egg.
Conception becomes almost impossible. In this case, the anatomical structure of the uterine cavity changes. Women develop infertility. The process leads to menstruation irregularities and pain in the lower abdomen.
Laparoscopy allows you to restore the correct anatomical location of the reproductive organs.
Ectopic pregnancy
The sperm helps fertilize the egg, but outside the fallopian tube. The embryo begins development outside the uterine cavity. Such pregnancy is precisely facilitated by pathology in the fallopian tubes, which is caused by the inflammatory process, adhesions or hormonal imbalance.
The main danger of developing such a pregnancy outside the uterine cavity is a possible rupture of the tube if the pathology is not detected in time and urgent measures are not taken. And only a timely operation will preserve the integrity of the fallopian tube.
The main signs of an ectopic pregnancy are pain in the lower abdomen, adhesions, weakness, spotting, difficulty urinating, and delayed menstruation. Only a timely ultrasound will reveal the diagnosis.
Laparoscopy may be prescribed as an urgent surgical intervention to remove residual pathological manifestations in the tubes. For women of this age group who do not plan to have children, it is possible to remove the uterus and underlying fallopian tubes.
Impaired patency
Blockage of the fallopian tubes near the ovary leads to a pronounced process of obstruction, when it is no longer possible to do without surgical intervention. Timely laparoscopy allows women to become pregnant in the near future in 35% of cases.
Hydrosalpinx
Pathology in the fallopian tube leads to the accumulation of serous fluid, since a favorable environment for the proliferation of microbes is created in the cavity. The fallopian tubes become clogged. Obstruction occurs.
The pathology requires urgent laparoscopy in combination with tubectomy, when the fallopian tube becomes inflamed and ceases to function. The quality of the endometrium deteriorates and infertility occurs.
Natural pregnancy is no longer possible due to disruption of the egg release process, blockage of the tube, and impossibility of natural fertilization.
Women are worried about high fever and pain in the lower abdomen. A timely surgical procedure will allow you to restore the patency of the tubes or remove them to avoid further development of the inflammatory process.
Sterilization
If a woman does not plan to have children, then laparoscopy will help as a reliable method by performing manipulations and cauterizing the fallopian tubes with an electrocoagulator. It is often prescribed in the form of sterilization to women over 35 years of age who have children in order to avoid the development of serious complications and inflammatory processes within the body.
Indications and contraindications for tubal laparoscopy
The reasons for laparoscopic intervention on tubes may be:
adhesive pelvic disease
Infertility (to diagnose causes and eliminate pathology);
- Adhesive disease of the pelvis with cicatricial adhesions around the appendages;
- Ectopic pregnancy in the tube;
- Sclerosis with lack of tubal patency;
- Hydrosalpinx, pyosalpinx and paratubar serous cysts, endometriosis;
- The desire to tie the tubes for the purpose of sterilization.
Infertility is one of the most common reasons leading a woman to undergo laparoscopy. In this case, it is of a diagnostic nature if the cause of infertility is not fully understood, but during the operation, obstacles to pregnancy (adhesions, for example) can also be eliminated, which will simultaneously serve as a treatment for the existing pathology.
Adhesive disease with the development of cicatricial adhesions around the fallopian tubes is another common pathology, the cause of which can be both infectious and inflammatory processes (banal infection, STIs, tuberculosis, chlamydia, cytomegalovirus, etc.) and previous abdominal surgeries in this area. In particular, appendectomy contributes to serious reproductive problems due to scarring, so laparoscopy of fallopian tube adhesions is a fairly common procedure for fertility problems.
ectopic pregnancy
Ectopic pregnancy, when the zygote attaches and begins to develop outside the uterus, most often occurs in the tube, from which, for one reason or another, a fertilized egg has not emerged. This pathology is classified as a surgical emergency, because a pregnancy growing in the tube is a direct path to organ rupture and fatal bleeding. With this pathology, laparoscopy is aimed at removing the affected tube along with the embryo.
Some experts propose methods of removing the embryo laparoscopically while preserving the organ, but experience shows that almost all tubes preserved in this way are difficult to pass in the future, and the risk of a repeat tubal pregnancy in them increases significantly. In this regard, most gynecologists insist on the need for complete excision of the tube laparoscopically.
Impaired patency of the tubes implies the need for diagnostic laparoscopy, during which the doctor determines the etiology of the obstruction, its prevalence, and also determines the possibilities of eliminating the pathology. This laparoscopy can be supplemented with chromotubation when the degree of obstruction is diagnosed using dye. A sterile dye is injected into the uterine cavity, and if the tube is not sclerotic, it exits into the abdominal cavity, which is recorded by the surgeon’s eye.
Laparoscopy for patency of the fallopian tubes is performed for a variety of pathologies lying outside the lumen of the organ - endometriosis, paratubar cysts, benign tumors. Disturbances in the tubes can be expressed in the accumulation of pus (pyosalpinx), serous fluid (hydrosalpinx), which also requires surgical treatment, preferably through laparoscopic technique. Usually, the affected tube is removed entirely during the operation, because it is no longer capable of performing its main function, and there will definitely be no benefit from its presence.
If in case of infertility the main goal of laparoscopy is to achieve pregnancy, then sterilization is the opposite situation. When there are already children, but there is no desire to have more, a woman may decide to undergo tubal ligation as a surgical method of contraception. This manipulation is also performed laparoscopically for patients who have reached the age of 35 and have at least two children. The result of laparoscopy will be irreversible, which the doctor must warn you about.
Before prescribing laparoscopic tubal intervention, the gynecologist determines the presence of obstacles, which can be absolute or relative.
Absolute contraindications to tubal laparoscopy are:
- Oncological diseases of the appendages and uterus, when intervention can aggravate the course of neoplasia and provoke metastasis (open surgery in an oncology hospital is indicated);
- Severe decompensated pathology of internal organs (failure of the liver, kidneys, heart, pulmonary system);
- Acute general infectious diseases - influenza, intestinal infections, etc. until they are cured;
- Severe pathology of hemostasis, when the risk of bleeding is extremely high;
- Diaphragmatic hernia, which creates certain risks when applying pneumoperitoneum;
- The patient is severely exhausted.
It is worth noting that some absolute contraindications can become relative when it comes to saving a life. For example, a tubal pregnancy in a woman with blood clotting disorders one way or another requires surgery, and in this case, laparoscopy is preferable, because the blood loss will be less than with conventional laparotomy.
Relative obstacles include severe obesity, diabetes, high blood pressure, and severe adhesive disease. For such patients, the possibility of intervention is determined individually based on the possible risk.
Benefits of laparoscopy
Today, such surgical intervention is widely applicable in surgery, since the positive aspects include:
- high information content of the technique with image magnification on optical equipment up to 10 times;
- ensuring diagnostic accuracy;
- painlessness of the procedure;
- low morbidity;
- loss of minor blood loss due to the absence of damage to healthy tissue;
- shortening the length of hospital stay (no more than 5 days);
- short duration of the rehabilitation period (only 10-15 days);
- preventing tubes from accidentally rupturing in the event of an ectopic pregnancy;
- maintaining the integrity of the organ with additional coagulation by applying sutures and plaster;
- no need to follow a strict diet in the postoperative period;
- reduction in the formation of the adhesive process again, which cannot be achieved through abdominal intervention;
- quick recovery after surgery;
- leaving minor scars up to 1.5 cm in diameter;
- high information content during endoscopic intervention due to video monitoring and full display of information on the screen.
Laparoscopy has proven its effectiveness as a gentle procedure without injury to neighboring organs.
Possible development of complications after laparoscopy
Laparoscopy is a method characterized by a minimal risk of developing dangerous complications. As a rule, this operation is easily tolerated, and recovery after laparoscopy is quick.
You should consult a doctor after discharge from the hospital as soon as possible if the following symptoms appear:
- high temperature, chills;
- fainting (loss of consciousness);
- increased pain in the abdominal area, nausea, vomiting that does not stop for several hours;
- swelling, suppuration or redness in the suture area;
- bleeding from wounds;
- urinary disorders
How is the operation performed?
The operation is performed under general anesthesia and requires careful preparation:
- taking tests, urine and blood;
- performing an ultrasound.
As a rule, it is carried out on days 8-10 of the menstrual cycle, until ovulation occurs.
The essence of the procedure is:
- supply of carbon dioxide to increase the size of the abdominal cavity;
- lifting the abdominal walls to gain maximum access to the internal organs;
- carrying out manipulations by a doctor in the form of several punctures with a diameter of up to 5 mm.
All manipulations are controlled and displayed on the monitor. This allows doctors to quickly identify the affected area with the presence of adhesions in the fallopian tube. A contrasting colored solution is injected and the doctor remains to dissect, remove adhesions, and restore the lumen in the fallopian tubes as far as possible.
Preparation
It is important to identify contraindications to surgery. The doctor carefully examines the patient’s medical history and performs a visual assessment to determine the possibility of emergency intervention.
Preparation is prescribed several months before the procedure, unless, of course, there is an emergency intervention.
In about 2 weeks, patients will have to take:
- blood test for coagulability, group and Rh factor;
- test for HIV, hepatitis;
- urine analysis to exclude or refute the inflammatory process in the body;
- flora smear;
- Ultrasound;
- Fluorography;
- ECG.
Only after receiving ready-made tests in hand, the doctor will decide to carry out surgical measures. In particular, certain contraindications are taken into account.
Laparoscopy is not performed if the body contains:
- acute infection;
- malignant neoplasm affecting the genital area;
- highly active endometriosis;
- poor blood clotting;
- cardiovascular pathology;
- diseases of the respiratory system;
- excessively short fallopian tubes (less than 4 cm) due to a previous operation;
- diseases of the kidneys, adrenal glands;
- operated hernia;
- state of shock.
On the eve of the operation, it is important for women to carry out a fasting diet for several days, excluding gas, drinks, vegetables, and fruits. Do not eat after 6 o'clock and give an enema at night.
REFERENCE! Analyzes are prepared for at least 10 days. The doctor must identify the possible chronic course of diseases in the body, when laparoscopy can be canceled and other therapeutic measures taken.
The day of the operation to remove the fallopian tubes is of no small importance. The procedure is not performed during the menstrual period. As a rule, it is recommended in the first half of the menstrual cycle to avoid and exclude the possibility of pregnancy.
Anesthesia
Anastasia is appointed as an anesthesiologist, since laparoscopy involves performing the operation under general anesthesia, when nerve impulses in the spinal cord and brain will still be involved. This can lead to partial loss of consciousness, increased pain as a reaction to external stimuli.
Before the operation, the patient’s blood pressure and the degree of oxygen saturation of the blood must be checked.
It is intended to administer (intravenous) solutions (sodium thiopental) to provide short-term anesthesia lasting up to 25 minutes. It is possible to use a mask or endotracheal method of anesthesia, in particular the administration of inhalation anesthetics together with gas (Halothane, Sevoflurane).
REFERENCE! Anesthesia is fraught with side effects (swelling of the larynx, respiratory failure, myocardial infarction, gagging). Only an experienced anesthesiologist will be able to determine the degree of administration of the necessary narcotic drugs and dosage, and control their intake into the body.
Operation stages
The operation is performed by a surgeon and gynecologist under sterile conditions. A woman needs to perform hygiene the day before, shave her pubic hair, and empty her bladder.
Anesthesia is administered immediately before the procedure, and the surgical area is treated with antiseptics.
Stages of implementation:
- placing the patient on the operating table;
- introduction of general endotracheal anesthesia;
- putting a woman to sleep;
- sanitizing the operated area with alcohol and antiseptics;
- making the first puncture of the navel with a Veress needle without injuring neighboring organs;
- supply of carbon dioxide and nitrous oxide into the cavity to artificially expand the space and free visualization for the doctor;
- insertion of a video camera through another puncture with a diameter of 10 mm;
- insertion of laparoscopic instruments through 3 punctures to examine the organ cavity and assess the situation;
- designation of the site of the adhesive process;
- carrying out manipulations to release tissue from adhesions, dissecting them;
- embryo removal during ectopic pregnancy;
- retrieving used tools;
- suturing;
- release of gases from the abdominal cavity.
The operation takes no more than 0.5 hours. The average duration is 40 minutes.
↑ Types of laparoscopic treatment on fallopian tubes
Depending on the purpose of the laparoscopic procedure, there are several types of operations on the fallopian tubes:
- with ectopic pregnancy:
- squeezing the fertilized egg out of the tube during tubal pregnancy (the operation is carried out using special clamps);
- removal of the fertilized egg attached outside the tube;
- salpingectomy (removal of the fallopian tube along with the fertilized egg);
- in the presence of adhesions in the pelvis:
- salpingo-ovariolysis (dissection of adhesions);
- fimbryolysis (disconnection of the cilia at the end of the fallopian tube);
- salpingostomy (removal of adhesions with restoration of the lumen of the fallopian tube or the formation of a new lumen - salpingoneostomy);
- for sterilization (blocking the lumen of the fallopian tubes by applying a clip, crossing or coagulation).
- The choice of drugs for anesthesia during laparoscopic surgery depends on the purpose and type of intervention, the complexity of its implementation and how long the operation lasts.
Consequences and complications
Possible complications:
- severe bleeding due to injury to nearby tissues and organs;
- development of a purulent-inflammatory course;
- the appearance of a repeated ectopic pregnancy;
- formation of adhesions in the pelvis;
- development of endometriosis.
Laparoscopy is popular today, although there are also disadvantages. It is possible to leave scars on the abdomen.
Rarely, a hernia or tubal adhesions form again. The risk of developing etopic pregnancy, stroke, myocarditis, thrombosis of the lower extremities, and pneumonia increases.
Trauma to the urinary tract, vascular damage, followed by embolism, which poses a deadly threat to women, can occur.
Consequences:
- infection of the retroperitoneal organs;
- seam divergence;
- violation of the structure of the reproductive organs, when it is impossible to do without a repeat emergency laparotomy with the involvement of cardiovascular surgeons.
Preventing possible complications
All pathological conditions that may arise in the period after surgery depend on the patient’s behavior.
General recommendations to prevent complications include:
- Increased activity and excessive physical exertion can provoke internal bleeding and suture dehiscence.
- Following a diet - carbon dioxide introduced before surgery will leave the abdominal cavity in a few days. During this period of time, it is advisable to adhere to an easily digestible diet, without overloading the body with difficult-to-digest foods and foods that cause flatulence. The recommended premium food intake is fractional, in small portions during the first month.
- Wearing elastic bandages on the lower extremities to normalize the circulatory system and prevent the appearance of venous enlargements.
Violation of the recommendations given by medical personnel will lead to a deterioration in the general condition of the operated patient and the development of pathological processes. Ignoring advice, going into difficult working conditions and refusing the recommended diet will return the patient to a hospital setting for treatment of emerging pathologies.
The worst option for ignoring the recommendations may be the need to remove both fallopian tubes or the body of the uterus itself. As a result, pregnancy is impossible - due to the absence of reproductive organs.
Rehabilitation after the study
Laparoscopy does not lead to serious consequences. Complications are extremely rare. The postoperative period is quick and easy due to low trauma and the absence of large incisions.
The rehabilitation course lasts no more than 3-4 days. Patients quickly recover and are discharged home. The sutures heal and intestinal function is restored.
Of course, in the first months you should take care and protect yourself from heavy physical labor and heavy lifting. You can't neglect your diet. It is worth excluding carbonated drinks and fried foods that increase gas formation. It’s better to sit for a while on light soups and porridges.
Women are not recommended to sit in one place for a long time. It is better to walk more often after the operation, which, on the contrary, will promote rapid tissue healing, eliminate intestinal problems, blood clots in the veins in the legs and other complications.
If there is no fallopian tube, where does the egg go?
When both fallopian tubes are in place, they use fimbriae to capture the egg released from the ovary into the abdominal cavity and gradually move it into the uterus. It is also possible for a sperm to meet an egg in the tube and fertilize it. In the peritoneal cavity, the egg can exist for two days, after which it dies.
When a woman has one tube missing, the following options are possible:
- Ovulation will not occur, the follicles will begin their reverse development. This situation is most often observed against the background of hormonal imbalance.
- The egg will be released into the abdominal cavity, and after 2 days it will die and be destroyed in it.
- The egg will float around the abdominal cavity, can reach the tube that remains intact, and pass through it to the uterus.
Of course, it is much easier for fimbriae to capture the egg that is released by the ovary from the side of the healthy tube. If a woman has both appendages removed, the ovaries either undergo reverse development, or the egg will constantly die in the peritoneal cavity.
Planning pregnancy after laparoscopy
After tubal laparoscopy, many women are concerned about pregnancy.
Of course, if there are complications, excessive blockage and obstruction of the fallopian tubes, pregnancy is unlikely to occur. If the situation is not advanced, then the probability of conception is highest in the first 2-3 months after the operation.
In the next 6 months it is already declining. If conception does not occur, then there is a high probability of adhesions forming again.
Experts do not advise postponing pregnancy for a long period, since after laparoscopy in the first 2-3 months the chances of pregnancy are high in 60% of cases.
Preliminary preparation for laparoscopy
Laparoscopy of the fallopian tube is carried out in the mode of preoperative preparation, which includes several successive stages:
- collection of complete anamnestic data, including all previously suffered diseases and the patient’s reaction to previously used anesthesia (anesthesia);
- medication preparation;
- laboratory and diagnostic tests.
Mandatory studies include:
- General blood test - to clarify the level of blood clotting and the content of components in it. It is used to identify possible hidden processes, inflammatory etiology, taking place at this moment in the body.
- General urine test - a sample is taken in the morning, immediately after a night's sleep. This sampling makes it possible to determine the normal functionality of the kidneys and other organs.
- Biochemical blood test - a sample is taken from a vein for a general assessment of the functioning of all organs and systems of the body being studied.
- Tests for HIV infection, syphilis and certain types of hepatitis.
- Determination of blood group and Rh factor - data is determined in advance, before the start of surgery. Necessary for possible blood transfusions.
- A smear from the urogenital area - to study the own microflora of the vagina, urethra and cervix.
- Fluorographic or x-ray examination of the pulmonary system.
- ECG - to determine the performance of the heart muscle.
- Ultrasound – study through ultrasound scanning of the pelvic organs.
- Consultation with a general practitioner.
After completion of all prescribed studies, data is examined to exclude possible pathological conditions. If there is a previously unknown disease, the woman is referred for consultation to a specialist. The latter must give an opinion whether surgical intervention can be performed.
If the result is positive and the exact time for the operation is assigned, the woman is recommended:
- for 2-3 days, follow a dietary diet based on easily digestible foods;
- before going to bed and in the morning immediately before the operation, perform a cleansing enema;
- refusal to eat, starting from six in the evening on the eve of the day of surgery.
If these tips are not followed, the operation will not be performed. Any operation that is performed under general anesthesia is prohibited by the presence of a full intestine (at the time of anesthesia sleep, involuntary vomiting will occur with the removal of masses through the nose and the patient may suffocate).
When can you plan to conceive after surgery?
After removal of one fallopian tube, a woman will be able to become pregnant on her own in 56-61% of cases. Moreover, this does not depend on the type of surgical intervention. Doctors indicate that you need to plan a pregnancy no earlier than six months after the operation. A number of experts recommend that a woman wait 1-2 years while taking oral contraceptives. During this time, it will be possible to normalize the functioning of the neuroendocrine system and the body will be ready to bear a child.
After removal of the fallopian tubes, 42% of patients develop infertility, and in 40% of cases, the ovaries stop working with their previous strength. Moreover, the risk of developing an ectopic pregnancy increases 10 times. Therefore, IVF is the only method that allows a woman to conceive a child after removal of the fallopian tubes.
Can tubal plastic surgery replace them?
Gynecologic surgeons may perform surgery to repair part of the fallopian tube, calling the procedure a fallopian tubeplasty. It is carried out after removal of the deformed area of the appendage.
As for the complete restoration of the fallopian tubes, this operation is not advisable. The fact is that a woman’s own appendages have the ability to contract so that the egg can move through them and reach the uterus. After plastic surgery, the tubes lose their ability to contract, which means fertilization will be impossible. Therefore, the operation is performed only when a small section of the appendage needs to be replaced.
Author of the article:
Lapikova Valentina Vladimirovna |
Gynecologist, reproductive specialist Education: Diploma in Obstetrics and Gynecology received from the Russian State Medical University of the Federal Agency for Health and Social Development (2010). In 2013, she completed her postgraduate studies at NIMU named after. N.I. Pirogova. Our authors