Pleurisy: X-ray for diagnosing a dangerous disease
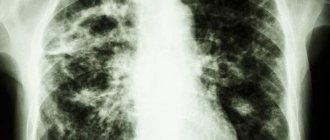
Inflammation of the pleural layers and loss of fibrin on their surface or accumulation of exudate in the pleural cavity of the lungs is diagnosed as pleurisy; X-rays are most appropriate in this case. It gives different results, the interpretation of which depends on the amount of fluid (exudative) or the size of the darkening (dry).
What affects the X-ray picture of pulmonary pleurisy?
The cause of the development of pleurisy can be either an infectious disease (syphilis, tuberculosis) or a non-infectious disease (wound, tumor).
If in the projection of the costophrenic sinus there are only small accumulations of exudate, then they may not be visible during an X-ray examination, so an ultrasound is also prescribed.
If dry pleurisy is diagnosed, then fibrin accumulates in places where the pleura is damaged. In this case, exudate is not expressed. In the early stages, the disease can be diagnosed only if the patient himself indicates the point where the pain is localized. Confirmation will be anamnesis of the course of the disease.
If the image shows a large darkened area with blurred contours, which tends to increase and progress, then doctors also identify a form of inflammation such as purulent (empyema). Adhesions and scars after this form of the disease are normal. An x-ray will always show them.
X-ray syndromes of pulmonary pleurisy
Symptoms and signs of identifying pleurisy in photographs:
- Complete or partial decrease in the transparency of the pulmonary field in the form of darkening in the chest area on both sides, having a homogeneous intense character.
- Displacement of the anatomical space in the middle parts of the sternum in the opposite direction.
- If, when the patient’s body position changes to horizontal or slightly inclined, the exudate spreads throughout the cavity, forming a darkening of the lungs of a homogeneous nature, then this phenomenon is called Lenk’s symptom.
- Even with a small accumulation of fluid in the sinus, a false sensation of a high standing diaphragmatic dome appears.
- An indirect sign of inflammation is a decrease in the mobility of the diaphragm during the examination.
- The increase between the pulmonary field and the gastric bladder reaches 2 or more centimeters (normally, no more than 0.5 cm).
- When taking an X-ray while lying on your side (laterography), fluid spreads across the lower part of the sternum.
Pathogenesis and classification
- Impact of microorganisms on the pleura. They get inside in the following ways:
- contact (cyst with suppuration, pneumonia, tuberculosis, abscess),
- lymphogenous (retrograde flow of tissue fluid),
- through direct infection due to disruption of tissue integrity (wounds, operations, injuries),
- hematogenous.
- Increased penetration of lymphatic and blood vessels due to the presence of vasculitis or due to the influence of toxic products (tumors, endotoxins), with enzymes that break down protein (acute pancreatitis).
- Blockage of lymph outflow pathways and disruption of its circulation.
- Allergies (local, general).
The disease is classified according to several indicators.
According to the etiology, pleurisy can be:
- Infectious.
- Non-infectious (injuries, tumors, autoimmune, etc.).
According to the nature of the exudate, they are distinguished:
- purulent,
- frail,
- putrefactive,
- cholesterol,
- fibrinous,
- serous,
- hemorrhagic,
- eosinophilic.
By phase:
- chronic,
- spicy,
- subacute
By prevalence:
- diffuse,
- encysted,
- costodiaphragmatic,
- interlobar,
- paramediastinal,
- paracostal,
- opical,
- diaphragmatic.
Exudative form
Exudative pleurisy is characterized by the following symptoms: shortness of breath, weakness, sweating, elevated body temperature, chills, poor appetite. Depending on the type of disease, swelling of the upper body, hoarseness, tachycardia, and muffled heart sounds may appear.
Diagnosis of pleurisy begins with an x-ray of the lungs. The X-ray image clearly shows a darkening with an uneven upper border and a shift of the mediastinum to the other side. If there are difficulties in making a diagnosis, additional tests are prescribed with preliminary pumping of the fluid.
Fibrinous form
It occurs as a result of the accumulation of a large amount of fibrin where there is damage to the pleura.
Its symptoms are pain in the chest area, which intensifies with breathing and coughing, general weakness, low-grade body temperature, lungs become less mobile, touching the pectoral muscles causes pain. With this disease, pain is concentrated in the upper abdomen or neck area.
In both forms, laboratory tests show an excess of ESR and leukocytes, low levels of iron (OAC), sialic acids, seromucoid and fibrin, and globulins (BAC). Analysis of the pleura will show a high protein content, density greater than 1.
018, the amount of lactate dehydrogenase is more than 1.6 mmol, a positive response to the Rivalta test, neutrophils in the remainder, empyema (accumulation of pus is characteristic of EF).
X-ray with pleurisy FF does not recognize it, but it will help to establish signs of the underlying disease (for example, tuberculosis, pneumonia or tumor).
How to describe pleurisy on an x-ray
The technique for describing pleurisy is unified, regardless of form. This approach helps the doctor make a diagnosis accurately and with minimal errors, and also makes it impossible to miss a single pathology when analyzing the image.
The general scheme drawn up by the radiologist is as follows:
- Shadows of the muscles of the sternum and sternoclavicular joints.
- Bone system.
- How are the diaphragm domes located?
- Sinuses.
- Root system of the lungs.
- Lung fields.
- Gaps between lobes.
- Mediastinum.
- Tomograms are additional.
General analysis of changes
The general analysis should be described according to the algorithm:
- position,
- number,
- form,
- sizes,
- intensity,
- drawing,
- contours,
- displacement.
Thanks to this description structure, the dynamics of the disease’s development can be easily tracked.
What does fluid accumulation in the pleura look like?
In the absence of inflammatory processes, the serous leaves are not visible in the image. If a patient has effusional pleurisy of the lungs, an x-ray will show an amount of fluid exceeding 200-250 ml (it is clearly visible on the pictures).
However, the doctor conducting the x-ray cannot indicate in the conclusion that he sees pleurisy on the x-ray, but can only write down symptoms indicating the presence of the disease. In this case, the main sign will be the presence of fluid.
The amount of fluid in the cavity and subjected to reverse absorption by the layers of the pleura makes up the picture of EF pleurisy. Even the smallest effusion can be suspected if there are indirect signs:
- The diaphragm is located high.
- Her mobility is poor.
- The space between the gas bubble and the pulmonary field increased sharply (up to 1.5 cm when the norm is no more than 0.5 cm).
The most indicative characteristic for a radiologist is the sinuses. Normally, these are free corners that are directed downwards. The accumulation of fluid in the lung image is visualized as darkening. Therefore, it is often confused with inflammation of lung tissue.
Another sign of the presence of fluid is darkening in the pleural fissures. This darkening is called mantle-shaped (covers the entire surface of the lungs).
Radiologists know that as the volume of fluid increases, the upper edge of the dark area on the image becomes smoother. The degree of hydrothorax (strong effusion into the pleural fissure of a different nature) is determined by the level and edges of this border. However, as practice shows, pleurisy on an x-ray rarely reaches such proportions, being limited to the sinuses.
Additional X-ray signs
Due to the accumulation of a large amount of fluid, the mediastinum shifts to the side opposite the affected one (one-sided). The degree of displacement depends on the following factors:
- Volume of liquid.
- Aperture level.
- Mobility of mediastinal structures.
- Pulmonary formations and their functional state.
In this case, Lenk phenomenon may be present and the lung tissue becomes less transparent.
If the liquid is not completely absorbed by the petals, and part of it is fenced off from the rest of the cavity, then this is an encysted form. The most common type is basal, when part of the encysted effusion is adjacent to the diaphragm with a wide base. The type of encysted type available depends on where the inflammation initially occurred and how it subsequently resolved:
- costal,
- supradiaphragmatic,
- interlobar,
- apical,
- mediastinal.
If the exudate does not resolve in a timely manner, there is a high risk of adhesions in the pleura, which will limit the respiratory capacity of the lungs.
As we see, there are quite a lot of methods for diagnosing pleural effusion, and each of them is important and informative in its own way.

Source: https://afrodita-spa.ru/diagnostika/ekssudativnyj-i-suhoj-plevrit-rentgen-kak-osnovnoj-metod-diagnostiki
Fibrinous form
In the fibrinous type of the disease, inflammation immediately takes on an acute form and is characterized by the formation of plaque on the membrane of the pleural layers. The patient is worried about weakness, chills, shallow breathing and limited mobility of the sore side of the chest, where pain is also noted when inhaling and coughing. This form of the disease is very dangerous and can permanently disrupt the breathing process.
The difficulty in determining the onset of fibrinous pleurisy lies in the absence of an exudative component. At the onset stage, the disease can be seen on an x-ray only if the patient points to a pain point in the chest. In the affected areas of the pleura, fibrin accumulates, then calcium, due to which strong darkening can be seen in the image. Such shadows remain with a person forever. In the passport for registration of dose loads in such patients there is a note about these shadows.
Pleurisy on X-ray: image analysis
Pleurisy on x-ray is visualized by infiltrative inflammation or fibrinous deposits on the pleural layers. Depending on the morphological features, the following types of pathology are distinguished:
- exudative (wet, effusion, free);
- fibrinous (dry);
- encysted.
X-ray syndromes of pulmonary pleurisy
Pulmonary pleurisy is determined on the image by the following x-ray symptoms:
- Subtotal or total decrease in pneumatization (transparency) of the pulmonary field - uniform intense darkening in the chest on the right or left with a superior oblique line (Damoiso-Sokolov-Ellis).
- Displacement of the mediastinal shadow in the opposite direction.
- Lenk's X-ray symptom - if you take a picture of the patient in a horizontal position or tilted to the side (Trendelenburg position), the liquid spreads throughout the pleural cavity, forming a uniform, uniform darkening.
- An imaginary sensation of a high standing dome of the diaphragm - with a slight accumulation of infiltrative fluid in the costophrenic sinus.
- A decrease in the mobility of the diaphragm during fluoroscopy (transmission with visualization on TV) is an indirect sign of inflammation of the pleura.
- Increasing the distance between the gastric bladder and the beginning of the pulmonary field on the left. The value should not exceed 0.5 cm, but if fluid is detected it increases to 2 cm or more.
- With laterography (taking an X-ray on the side), the fluid spreads across the lower part of the chest.
Scheme: radiological syndromes of exudative pleurisy
General analysis of changes on a radiograph with exudative pleurisy
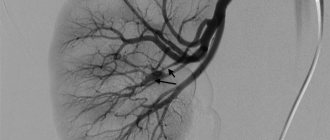
Exudative pleurisy is a common pathology that is detected when performing a chest x-ray. As a result, we present an analysis of the radiological report in the presence of pleural empyema on the right (see radiograph 3).
Photo description:
Paracostally on the right, a semi-fusiform shadow is identified, which with a wide base adjoins the anterior, outer and posterior edges of the ribs. The wide base of the formation faces the lung.
The shading contour is strongly emphasized and the shading structure is uniform. The greatest intensity of the shadow is in the center. In the peripheral zone, there is a smooth transition of darkening to adjacent zones with the formation of “obtuse” angles.
The parietal pleura is thickened over a large distance.
Conclusion:
X-ray signs of pleural empyema on the right.
Recommended:
X-ray monitoring in dynamics, since the tumor genesis of pleurisy cannot be excluded.
Analyzing the above detailed description of the image by a radiologist, the intensity and localization of the formation becomes clear, but the specialist did not indicate its size.
Of course, by planning for the patient to have subsequent X-rays performed by him, the doctor will be able to assess the dynamics, but the person can also go to another medical institution. Obviously, the “gold standard pulmonary analysis” should be followed.
Any shadow must be described using an algorithm, which when deciphered means:
- position;
- number;
- form;
- dimensions;
- intensity;
- drawing;
- contours;
- displacement.
If we analyze the x-ray, it is obvious that the shadow of the heart is slightly shifted to the left, and the right dome of the diaphragm is raised, which suggests the possibility of a tumor formation. Consequently, the patient needs additional studies: x-ray of the chest organs in the right lateral projection, tomography.
In conclusion, to “fill” the eye, we present a normal x-ray of the lungs for comparison.
Normal radiograph of the lungs without exudative pleurisy (given for comparison)
Despite the fact that exudative pleurisy is clearly visualized on an x-ray, one must not lose sight of the fact that it can be a consequence of other diseases (tumors, tuberculosis). The standard for identifying lung diseases is a chest x-ray in two projections, and it must be performed.
Source: https://x-raydoctor.ru/rentgen/grudnaja-kletka/plevrit-fibroznyj-ekssudativnyj.html
Dry pleurisy
Dry pleurisy is a pathology characterized by the presence of an inflammatory process in the serous membrane of the lung.
As a result, fibrinous edema forms on the surface of the pleural layers. Various other lung diseases can provoke this process, so most often dry pleurisy is a complication. It manifests itself as a rise in temperature and difficulty breathing.
Only complex therapy will help eliminate all the symptoms of the disease.
Reasons for development
Dry pleurisy has no independent meaning. Most cases of fibrinous pleurisy are etiologically associated with pulmonary tuberculosis or tuberculosis of the intrathoracic lymph nodes.
Dry pleurisy of tuberculous etiology occurs when the lesions are located subpleurally, break through into the pleural cavity with contamination of the latter, or as a result of hematogenous introduction of pathogens.
The causes of the development of dry pleurisy are also often nonspecific lung lesions: pneumonia, bronchiectasis, pulmonary infarction, lung abscess, lung cancer.
Among extrapulmonary processes, dry pleurisy can be complicated by diseases of the digestive system (cholecystitis, pancreatitis, subphrenic abscess), collagenosis (SLE, rheumatism, systemic vasculitis), infections (brucellosis, typhoid and typhus, whooping cough, measles, influenza). In some cases, dry pleurisy is accompanied by eating disorders (cachexia, scurvy), uremia.
The pathogenetic basis of dry pleurisy is the inflammatory reaction of the parietal and visceral pleura, which occurs with hyperemia, edema, and thickening of the pleural layers.
The amount of exudate is so insignificant that it is reabsorbed by the pleura with sedimentation of fibrin threads on the surface of the pleura in the form of pleural overlays, making it difficult for the sheets to slide.
In the future, this can lead to the formation of massive moorings and limitation of lung mobility.
In most cases, dry pleurisy turns into exudative, but it can resolve without the formation of pleural effusion.
Symptoms of dry pleurisy of the lungs
The main symptom of dry pleurisy should be considered acute painful sensations that have become stabbing in nature. They are localized in the side and are forced in the following cases:
- when trying to take deep breaths;
- short cough;
- sneezing.
When the pleural layers become inflamed, symptoms such as:
- chills;
- increased sweating at night;
- severe weakness;
- painful sensations.
- rarely - increased body temperature;
- swelling of the neck veins;
- sometimes - swelling of the skin in the lower parts of the chest may be swollen, its fold is thicker than on the healthy half of the chest.
In addition to pain, there are other manifestations of the disease. These include a dry cough, which occurs due to fibrin irritation of the cough pleural nerve endings, as well as an increase in body temperature.
Cough occurs reflexively, due to irritation of the pleura. But the patient tries to restrain coughing movements, as they increase pain in the chest.
In 80% of cases, patients with dry pleurisy indicate pain and discomfort in the lower and lateral sternum. Depending on which location is affected, other processes may be involved in the algorithm for the irradiation of symptoms. We are talking about the brachial plexus, the nerve trunks of the upper limbs and the diaphragm.
Typically, dry pleurisy lasts 1-3 weeks and ends with recovery. The transition of dry pleurisy to exudative pleurisy is possible; then the pain decreases and the pleural friction noise disappears. A prolonged or recurrent course indicates active pulmonary tuberculosis.
Left-sided diaphragmatic pleurisy should be differentiated from myocardial infarction. Indeed, in this situation the following symptom complex arises.
- pain in the chest, sometimes behind the sternum;
- dyspepsia;
- pain in the epigastric region;
- rhythm disturbance such as extrasystole or tachyarrhythmia;
- feeling of anxiety and fear.
There are a number of diseases that can occur with symptoms similar to pleurisy:
- intercostal neuralgia;
- intercostal neuromyositis;
- rib fracture;
- epidemic myalgia;
- fibrinous pericarditis;
- angina pectoris;
- myocardial infarction;
- spontaneous pneumothorax;
- peptic ulcer of the stomach and duodenum;
- acute cholecystitis;
- acute appendicitis;
- osteochondrosis of the intervertebral discs of the thoracic region.
A deep knowledge of their symptoms, as well as additional research methods, will help the doctor distinguish dry pleurisy from these diseases.
Diagnostics
Interpretations of complaints, visible manifestations, as well as data from additional examination methods will help the general practitioner establish the correct diagnosis.
Differential diagnosis with pericarditis, coronary insufficiency, intercostal neuralgia, and neuromyositis is necessary. For this purpose, consultations are necessary: with a cardiologist, neurologist, pulmonologist, and sometimes a thoracic surgeon.
Diagnostic methods include:
- Clinical blood test (increased erythrocyte sedimentation rate, neutrophilic leukocytosis with a shift to the left).
- Biochemical blood test (increased amount of seromucoids, fibrin, sialic acids and other acute-phase indicators).
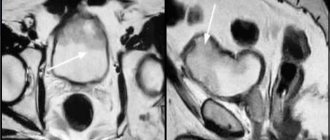
- X-ray examination of the thoracic organs (typical high location of the dome of the diaphragm on the affected side; decreased mobility of the lower edges of the organ during respiration and slight bulging of parts of the pulmonary field).
- Ultrasound (reveals the presence of deposited fibrin layers and thickening of the membrane walls).
A modern way to diagnose processes occurring in the pleural cavity is spiral computed tomography (SCT), as well as magnetic resonance imaging (MRI).
How to treat dry pleurisy?
Regardless of the origin of pleurisy, patients must adhere to medical prescriptions such as:
- bed or semi-bed rest;
- a balanced diet (it is especially important to consume enough proteins, but the consumption of carbohydrates, salts and liquids should be limited);
- anti-inflammatory drugs (in the acute period - intramuscular and intravenous, for residual effects - tablets);
- desensitizing agents;
- in case of severe pain, use painkillers;
- to increase the body's resistance - hyperimmune plasma, polyglobulin and their analogues.
Treatment for secondary pleurisy should be primarily aimed at eliminating the cause of inflammatory changes in the pleura - these are:
- cytostatics for cancer;
- anti-tuberculosis drugs for tuberculosis;
- antibiotics for pneumonia, taking into account the sensitivity of microorganisms;
and so on.
After consulting with your doctor, you can use old, but quite effective methods of traditional medicine:
- warm compress;
- tight bandaging of the lower chest;
- applying iodine strips to the skin of the chest
and so on.
In complex or advanced cases with a pronounced inflammatory process, as well as disturbances in protein and water-salt balance, the following is used:
- hormonal drugs;
- protein preparations;
- electrolyte solutions.
The introduction of antibacterial drugs into the pleural cavity is theoretically possible, but as a method for dry pleurisy it has not taken root.
Complications
As a rule, the outcome of the disease is always favorable, but if patients ignore medical prescriptions, it is possible:
- development of adhesive process in the pleural cavity,
- compaction of the pleura,
- education mooring,
- development of pneumosclerosis and subsequent respiratory failure.
A frequent complication of exudative pleurisy is suppuration of fluid in the pleural cavity.
Prevention
Of course, it is impossible to predict how the body will react to the action of a particular factor. However, anyone can follow simple recommendations for the prevention of pleurisy:
- First of all, complications should not be allowed during the development of acute respiratory infections. To prevent pathogenic microflora from penetrating the mucous membrane of the respiratory tract, and then into the pleural cavity, colds cannot be left to chance!
- If pneumonia is suspected, it is better to take a chest x-ray in a timely manner and begin adequate therapy. Improper treatment of the disease increases the risk of complications in the form of inflammation of the pleura.
- For frequent respiratory tract infections, it is good to change the climate for a while. Sea air is an excellent means of preventing respiratory tract infections, including pleurisy.
- Do breathing exercises. A couple of deep breaths after waking up will serve as an excellent prevention of the development of inflammatory diseases of the respiratory system.
- Try to strengthen your immune system. In the warm season, do hardening, spend more time in the fresh air.
- Stop smoking. Nicotine becomes the first cause of the development of pulmonary tuberculosis, which in turn can provoke inflammation of the pleura.
Source: https://doctor-365.net/suhoj-plevrit/
Etiology
For reference. In most cases, pleural empyema develops secondarily. It is preceded by bacterial diseases of the lung tissue. Most often - abscesses, bronchiectasis, pneumonia.
The disease may develop with gangrenous collapse of the lung and suppuration of a thin-walled air cyst. Less commonly, pyothorax develops with purulent bronchitis, when a bronchopleural fistula forms.
Primary pleural empyema occurs in cases where the main focus of inflammation in the lungs is not determined. In this case, bacteria immediately enter the pleural fissure and inflammation develops only in this place. Primary empyema is quite rare.
Injuries, especially open injuries with fractures of the ribs or sternum, can lead to purulent inflammation in the pleural cavity. Injuries that are not treated promptly pose a particular danger.
Sometimes empyema occurs after major thoracic surgery. In this case, microorganisms penetrate into the pleural gap through left drains or during surgery. Purulent inflammation in an organism weakened after surgery develops quite quickly.
Pleurisy on x-ray
The pleura is a thin serous covering that lines the inside of the lungs, diaphragm and chest. Inflammations to which the pleura is periodically exposed are called pleurisy. Back in the 19th century, the French clinician Lassegue noted that pleurisy “is not a disease of the pleura.”
Inflammation is indeed often a secondary process that develops after many dangerous diseases of pulmonary and extrapulmonary etiology: pneumonia, tuberculosis, pulmonary infarction and various neoplasms. Depending on the origin of the disease, pleurisy has several types: tuberculous, parasitic, tumor, post-traumatic, etc.
d.
And in terms of morphological features, pleurisy can be:
- Exudative (exudative)
- Fibrinous (dry).
Lungs in the picture - what determines the pathological picture
The most accurate picture of pleurisy is provided by an X-ray examination of the lungs. It allows you to identify the features of inflammation and determine how much fluid (exudate) has accumulated in the pleural area, and see the intensity of darkening of the lungs. Also, from an x-ray, the doctor can find out what pathology caused the development of pleurisy.
If pleurisy is of a dry (fibrinous) form, the following details are visible on the x-ray:
- The diaphragmatic dome of the affected area is located above normal
- The lung tissue is not transparent due to inflammation of the serous membrane.
Exudative (exudative) pleurisy is reflected in the following signs on the image:
- The diaphragmatic angle is flattened due to accumulated fluid
- The lower part of the lung field with a beveled border has uniform turbidity
- The mediastinum is shifted towards the healthy lung.
Pleural empyema - classification
Empyema is divided into types according to origin, amount of exudate, prevalence, and localization. Empyema is classified according to its origin:
- Primary – developing as an independent process.
- Secondary – resulting from another pathology. Most often it is pneumonic - developed as a result of a pathological process in the lungs. Pneumonic is divided into metapneumonic, which occurs in the process of resolving the pathology, and parapneumonic, which develops at the height of the underlying disease.
- Traumatic – occurring after a chest injury with disruption of the integrity of the pleura.
- Postoperative – which is a complication of operations on the lungs and mediastinum, it is also called iatrogenic.
Based on the amount of exudate, empyema can be:
- Small – up to half a liter of inflammatory fluid;
- Average - from half a liter to a liter of pus;
- Massive - more than one liter of exudate.
Empyema is classified according to its prevalence:
- Encapsulated - limited in a certain place of the pleural fissure by emerging adhesions;
- Non-encysted - unrestricted, in which the pus changes position under gravity.
According to localization, encysted empyema can be supradiaphragmatic, parietal, apical, interlobar, peri-mediastinal.
Attention. For non-bursal empyema, the latter classification does not apply, since the pus changes its location when the position of the body in space changes.