MRI of the head helps to identify pathological changes in the structure of the brain before symptoms of diseases appear, which allows the doctor to carry out therapy at an early stage. Magnetic resonance scanning is used to make an initial diagnosis, clarify it, and evaluate the results of a course of treatment or surgery.
MRI images of the brain
Content
- Can I eat/drink before an MRI?
- Can children have an MRI?
- Is it possible to do an MRI after surgery?
- Is it possible to do an MRI after an x-ray?
- Is it possible to do an MRI of the whole body?
- Is it possible to have an MRI during pregnancy?
- How often can an MRI be done?
- Is it possible to do an MRI during menstruation?
- Is it possible to have an MRI while breastfeeding?
- Is MRI possible for obese people (from 120-130 kg)?
- Is it possible to do an MRI without a referral?
- Is it possible to do an MRI while standing?
- Is it possible to do an MRI if there is presence in the body?
- Is it possible to have an MRI if you have been drinking alcohol?
- Do they do MRI of the heart?
- Do they do MRI of the lungs?
- Do they do MRI of the intestines?
- Comments.
Advantages and disadvantages of the technique
The main advantage of this method is the likelihood of access to the patient during the entire examination. Moreover, during diagnosis, a person has the opportunity to receive intravenous injections, which is of irreplaceable importance for seriously ill patients on life support. Until open-type equipment was invented, these patients did not have the opportunity to receive the necessary examination.
An open tomograph is indispensable for studying obese people
In addition, a big advantage is the likelihood of undergoing the study next to relatives, holding their hands, and talking to each other if possible. This is especially true for children or people suffering from mental disorders. Another advantage is the ability to diagnose in different body positions, since there are often situations when a patient cannot be examined lying down due to some disease.
This method has much fewer contraindications; it can be used to examine people with braces, dentures, artificial joints, and with fragments in the body.
Important! Open MRI produces much less noise than a traditional machine. Despite all the advantages, this equipment also has disadvantages, which include the longer time required for the examination. This diagnosis requires at least 1 hour, during which you should lie still. In addition, an open device has less voltage emitted by the magnetic field, which does not allow you to appreciate the smallest details.
Thus, this equipment does not provide the opportunity to obtain clear images necessary if there is a suspicion of severe brain pathology. With its help you can get a general picture of what is happening in the head cavity. That is, it is possible to detect neoplasms, cracks, and swelling, but it will not be possible to obtain exact coordinates and size.
The same applies to examination of cerebral vessels with the introduction of contrast. Open equipment will not allow you to obtain detailed images of brain structures and blood vessels, assess their diameter, and the elasticity of the walls. The doctor will receive only general information about the vascular network, and will see whether there are growths on the vessels or plaques.
Open MRI has both its advantages and disadvantages. If there is a need for more accurate research, then this equipment cannot compete with traditional tomography.
Magnetic resonance imaging (MRI) is one of the modern methods for diagnosing internal organs using electromagnetic waves. Today, there are different types of MRI scanners - open and closed devices. They have certain differences, and this concerns not only their appearance. So, open and closed MRI: which is better?
Closed-type MRI is the most commonly used. The device is a closed tube into which the patient “enters” while lying on the examination table. The chamber diameter of a closed tomograph is 60 cm with a length of 1.6...2 meters.
The duration of the procedure on average does not exceed half an hour. During this time, the patient is forced to remain completely still. Otherwise, the image of the organ being examined will be blurred, which will negatively affect the interpretation of the result.
The advantages of a closed tomograph include:
- high power. The magnetic field created by the equipment allows you to perform diagnostics of any complexity;
- image quality. The images obtained during the procedure are as clear as possible, which makes interpretation and diagnosis easier.
But at the same time, a closed magnetic resonance imaging scanner has a fairly large list of disadvantages. The disadvantages of classical diagnostic devices include:
- high noise level. The diagnosis is accompanied by various noises that can cause some discomfort to the person being examined. As a rule, the patient is given either special headphones or earplugs before the procedure begins;
- lack of visual contact with medical staff. The ability to communicate with medical workers while inside the tomograph exists, but it is represented only by audio communication;
- the impossibility of obtaining a diagnosis for people suffering from claustrophobia. A narrow tube can cause panic attacks in patients with a fear of closed spaces, so in many cases, before the start of the session, the patient is forced to receive sedatives or sedatives;
- the impossibility of performing a scan if there is an existing injury or a certain fixation of the human body. For example, a limb casted in a bent position will not allow the patient’s body to be brought into the tomograph chamber. Difficulty may also arise from injuries in which the patient cannot remain completely still for a long time;
- weight. At any stage of obesity, an MRI examination procedure is not available.
Doctors try not to use closed-type MTRs for examining small children. Enclosed spaces cause panic in children. In addition, the child cannot maintain long-term immobility, again, due to his age.
Unlike a classic device, an open-type tomograph does not have a closed scanning chamber. During the procedure, the person is placed in a special room in which magnets are located above and below. The space around the table on which the patient lies remains free. During the session, either a medical professional or a loved one may be near the person being examined.
Open MRI differs from classical equipment in the following ways:
- the ability to examine certain groups of patients. In particular, open-loop CT scanners can be used in critically ill and traumatized patients;
- scanning of young children. It is open type devices that are recommended for examining a child. The possibility of the baby and parents being together during the procedure helps him remain still and calm for a long time;
- reduced noise level. The examination takes place in more comfortable conditions, so it is recommended for people with unstable mental health and heightened emotional background.
But the open tomograph also has significant disadvantages. The first and most significant is the low magnetic field. It is impossible to create a strong magnetic field in an open and fairly large space, which affects the quality of the resulting images. It is much worse than when scanning on a classic (closed) tomograph.
In addition, open or semi-closed MRI does not allow obtaining images of:
- small parts of organs;
- vessels;
- organs that are in constant motion - the lungs and heart.
When using an open-type magnetic resonance imaging scanner, a person is forced to remain motionless for a longer time. The duration of the procedure is on average 30...40 minutes.
The main indications for the use of an open tomograph are confirmation of a previously established diagnosis.
Can I eat/drink before an MRI?
It is possible, with the exception of examining some organs.
No special preparation is required for MRI of the brain, spine or abdominal cavity.
Examination of the pelvic, intestinal and hepatobiliary system includes preparation several days in advance. You need to avoid gas-forming foods and foods that cause constipation. The day before the test, a laxative is taken to cleanse the intestines.
Immediately before an MRI of the abdominal cavity and retroperitoneal space, you need to take an antispasmodic drug (No-Shpa).
Scanning of the bladder and urinary tract is carried out no earlier than 3 hours after urination, therefore drinking before the procedure is not recommended only because of possible discomfort from bladder overflow.
What is cardiac stenting?
Stenting of the coronary arteries that supply the heart is a gentle intravascular surgical intervention with the expansion of stenotic or blocked areas of the arteries with a stent.
A stent is a special internal frame that prevents the vessel from narrowing again. This is an implant that is foreign to the body’s tissues, so it has a number of requirements. Stents for coronary vessels are made from cobalt and chromium - metals that are inert in relation to the internal environment of the human body and at the same time durable.
Externally, the stent resembles a vessel about a centimeter long and up to 6 mm wide with mesh walls. Basically, it's a balloon that you can inflate. The mesh structure makes it possible to deliver it to the installation site in a compressed state, and on site to expand it to the size required for the vessel.
The stents are coated on top with anticoagulating substances that prevent thrombus formation at the stenting site. Recently, absorbable implants have appeared, the validity period of which is calculated according to their metal counterparts.
The main reason for installing a stent in the heart is atherosclerosis, which narrows the coronary vessels, reducing blood flow to the myocardium, which is fraught with ischemia and hypoxia of the heart. The essence of stenting is to restore the original lumen of the coronary arteries, and therefore normal cardiac blood flow. The operation itself does not solve the problem of atherosclerosis, but it relieves its consequences for several years.
The operation is performed intravascularly, without incisions in the dermis. The stent does not remove the plaque, but presses it into the endothelium of the artery. During the intervention, several implants can be installed. Control over the localization of the lesion is carried out using radiocontrast.
Stenting of cardiac vessels is not the only method of restoring cardiac blood flow, but it has many advantages over other techniques (bypass surgery, angioplasty, medications), which ensure its effectiveness and safety for the patient. However, the method of correcting vascular pathology is chosen by the doctor for each patient individually, taking into account the physiological characteristics and severity of the disease.
Can children have an MRI?
Can. MRI has no age restrictions and can be performed from birth. During the examination, the child must remain motionless.
When this cannot be achieved, the examination is considered under anesthesia. During the MRI, parents can be with the child to reduce anxiety and fear. Diagnosis becomes more complicated if the child is hyperactive, which is why some clinics still have age restrictions, and you can undergo an MRI from 6-7 years old.
Flaws
Despite all the listed advantages, this tomograph also has some drawbacks. The most significant disadvantage is the low magnetic field. It is not possible to create a strong magnetic field on this device. This indicator affects the quality of the images obtained as a result of the study. They become much worse than during diagnostics on closed equipment.
Also, this view does not allow you to take a picture:
- the smallest parts of an organ;
- vessels;
- the exact size of the tumor location;
- heart and lung, since these organs are in constant motion.
Open MRI cannot clarify the nature of the tumor, whether it is malignant or benign. Important! When diagnosing using open-type equipment, the patient must remain motionless for a longer time, since the procedure lasts at least 40 minutes.
Is it possible to do an MRI after surgery?
The early postoperative period is a relative contraindication to MRI. The study is not carried out after surgery for stenting, coronary artery bypass grafting and gallbladder erosion. MRI is allowed one and a half months after surgical treatment.
There are restrictions on performing MRI after puncture biopsy of the mammary and prostate glands, as well as after their partial resection. The study is absolutely contraindicated after surgery for the installation of metal endoprostheses, stents, and plates.
Which doctor can order an MRI of the brain?
Patient at doctor's appointment
Magnetic resonance imaging of the brain can be prescribed by any specialist. Most often, this is a neurologist to whom the patient turns for headaches. Vascular surgeons, oncologists, and neurosurgeons refer for MRI diagnostics when surgery is planned and after surgery.
This examination method helps endocrinologists, otolaryngologists, ophthalmologists, therapists, traumatologists, dentists, psychotherapists and other specialists who believe that processes occurring in the structures of the skull can affect the patient’s condition.
The resulting images are analyzed by a radiologist. For further consultation with a conclusion and photographs, you must contact the attending physician who gave the referral for diagnosis.
Is it possible to do an MRI after an x-ray?
It is possible, but there are limitations to performing MRI with contrast.
Administration of the drug is contraindicated within 24 hours after any other study using a contrast agent, including radiography.
MRI without contrast can be performed at any time in the absence of contraindications. The study does not carry radiation exposure and can be performed as many times as required to make a diagnosis.
An MRI is often performed after an X-ray when a tumor is visible on the image. MRI will confirm the diagnosis and make it possible to evaluate the tumor.
Indications and contraindications for MRI of the head
MRI of the brain is recommended for people with complaints of:
- frequent headaches with an unknown cause;
- sudden deterioration in hearing or vision;
- periodic fainting and dizziness;
- nausea, vomiting, weakness, accompanied by headaches (including after traumatic brain injury);
- noises in the head;
- regular nosebleeds;
- increased body temperature in the absence of symptoms of a cold or viral disease;
- constant changes in blood pressure;
- seizures;
- spasms and partial loss of sensation in the tissues of the head and face;
- inhibition of reactions;
- spatial disorientation;
- deterioration of mental activity;
- speech disorders;
- memory loss or impairment.
An MRI of the head should be done if:
- increased intracranial pressure;
- presence of hematomas in the head area;
- diffuse axonal damage and other severe cranial injuries in the long-term period (to assess brain atrophy);
- chronic or acute sinusitis with the formation of pus;
- stroke;
- suspected accumulation of fluid in brain tissues and cavities;
- circulatory disorders;
- suspected edema, tumor, abnormalities of brain development;
- epilepsy and epileptic syndrome;
- inflammatory processes (meningitis, encephalitis, etc.).
This method is used to monitor the condition of patients with multiple sclerosis, Parkinson's disease, Alzheimer's disease, atherosclerosis, cardiac disorders, endocrine system disorder (pituitary dysfunction) and other pathologies.
Multiple foci of demyelination (indicated by arrows) on MRI scans: a) axial projection; b) sagittal projection
Magnetic resonance imaging has a number of contraindications for use. Before the procedure with enhancement, it is necessary to make sure that the patient is not allergic to the contrast agent and has no severe impairment of kidney or liver function.
It is prohibited to undergo an MRI if you have a pacemaker or other electronic devices (the device may malfunction or stop working), metal elements inside the body: implants, fragments, clips on blood vessels, etc. If the patient is not sure whether there are foreign objects in the body, it is worth taking an x-ray .
Relative contraindications are:
- tattoos based on metallic ink;
- pumps for administering medications;
- heart valve prostheses;
- neurostimulators.
The study is not recommended for acute heart failure, claustrophobia, tendency to panic attacks, in the first trimester of pregnancy (especially with contrast), if it is impossible to maintain a stationary position. Due to the design features of the devices, the procedure is not performed on people weighing more than 120 kg.
Is it possible to do an MRI of the whole body?
It is possible, but standard devices installed in diagnostic centers and clinics are not suitable for this.
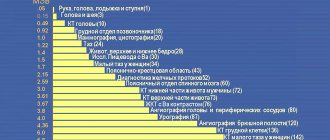
MRI diagnostics is designed to visualize individual anatomical areas. There are no indications for scanning the whole body. If you want to obtain such images, the study will have to be done several times, examining each anatomical zone in turn: the brain, chest, abdominal cavity and retroperitoneal space, pelvic organs and spine.
Preparing for an MRI of the brain
The head MRI procedure does not require any special preparation. A person does not need to change his usual diet, food intake or give up medications. The day before undergoing diagnostic tests with contrast, it is strictly forbidden to drink alcohol. Alcohol promotes vasospasm, as a result of which problem areas may not be sufficiently visualized during the examination.
If a nursing mother undergoes contrast tomography, it is necessary to prepare food for the baby for the day, since the dye penetrates into the milk.
Foci of gliosis in the white matter of the brain
Is it possible to have an MRI during pregnancy?
The first trimester of pregnancy is an absolute contraindication to MRI. Despite the absence of radiation exposure, it is not possible to study the effect of MRI on the fetus.
An MRI is considered only if absolutely necessary, when the pregnant woman is in danger. In this case, MRI is considered the safest examination option. Before prescribing an MRI, the doctor always clarifies the possibility of pregnancy, and if it is suspected, the study is not performed.
Stenting results, prognosis
No doctor will undertake to predict how long they will live after cardiac stenting surgery: the intervention restores cardiac blood flow, but does not eliminate the main cause of coronary stenosis - atherosclerosis, and does not remove the threat of AMI.
In 95%, the prognosis is favorable: on average, the stent provides 5 years of excellent vascular patency. But there are cases where the implant works for only a few days, and sometimes it lasts for more than 15 years. Symptoms of ischemia disappear in half of the cases after surgery, and in another half of the patients a persistent improvement in general well-being was noted. Unfortunately, the longer the stent is in place, the higher the risk of thrombosis with the development of complications and restenosis.
How often can an MRI be done?
MRI has no restrictions on the number of procedures performed over a certain period of time due to the absence of radiation exposure. The study is carried out as many times as necessary for the doctor to obtain a complete picture of the disease.
There are restrictions on contrast scanning. Frequent administration of a contrast agent may lead to the development of adverse reactions.
To perform MRI with contrast, safe gadolinium preparations are used, which eliminate the risk of an allergic reaction. The substance accumulates in tissues, after which it is completely eliminated from the body within 36 hours. Iodine-containing drugs are not used during MRI, therefore all risks are minimized.
Procedure for performing an MRI of the brain
Many patients are wary of magnetic resonance imaging, believing that their health condition may worsen after the procedure. Not everyone can easily tolerate a long stay in a confined space. The method is absolutely safe, you just need to strictly follow the doctor’s instructions.
When completing documents, you must indicate whether you have chronic diseases, allergies to medications, or metal objects in your body. Staff must be warned about pregnancy or claustrophobia.
Before entering the room where the tomograph is located, it is necessary to remove watches, glasses, dentures, jewelry, accessories and clothing with metal elements. Some medical institutions have disposable gowns and shirts - you should check what they are wearing for MRI of the brain when making an appointment. Phones and other electronic devices must not be brought into the examination room. Walkers, strollers and other devices for patients are left outside the door.
MRI of the brain
The procedure for magnetic scanning of the brain is as follows:
- a person lies on his back on a mobile table;
- to prevent accidental movements, the head is fixed with special bolsters, and the limbs are secured with straps;
- the conveyor is moved into the tunnel of the device, at this time the patient is left alone: the staff monitors what is happening from the next room;
- The tomograph switches to operating mode and takes images of the brain in three projections - axial, sagittal and coronal (the operation of the unit is accompanied by loud sounds, which headphones or earplugs help muffle);
- if contrast is provided, after the native part of the examination, a drug with a dye is injected into the vein and filming continues;
- When the diagnostic process is completed, the device is turned off and the patient can leave the table.
Having an MRI usually does not cause any discomfort. The only inconvenience is associated with the need to be in one position for a long time (from 30 minutes to an hour). Sometimes heat is felt in the area being examined due to the influence of the magnet. If it doesn't turn into a burning sensation, you don't have to worry.
MRI contrast agents have virtually no side effects. It is extremely rare that after administration of the substance, skin redness, swelling, hives, and itching are observed. To avoid such phenomena, people with a tendency to allergies need to do a test in advance.
Is it possible to do an MRI during menstruation?
The day of the menstrual cycle does not matter for the MRI and does not affect the result in any way.
An exception would be an examination of the pelvic organs and mammary glands, in which case the procedure is prescribed between days 6 and 12 of the cycle. Considering the need to remain in a horizontal position for a long time in a tomograph, women are advised to take care of reliable hygiene products in advance.
An obstacle can also be a woman’s increased nervousness during menstruation; in combination with physical discomfort, this can prevent her from remaining motionless in a closed tomograph for half an hour or more.
Features of Open Loop Equipment
An open-type device is used to examine overweight people.
The first open-type tomograph was designed for veterinary research. Devices created for diagnosing a particular disease using open MRI are based on the same properties of magnetic fields as classical models, differing only in the external features of the camera, its appearance, where the scanner is installed at the top with a side view.
The voltage on such a tomograph is not so great, especially when compared with closed circuit equipment. This is due to the very design of the device; in a closed type, the magnetic field spreads from all sides at once, and in a tomograph with an open circuit, it spreads from above and below.
Is it possible to do an MRI while standing?
Can. Vertical MRI is used to scan the lumbar spine.
This study is carried out in two stages. First, the lumbar spine is scanned in the supine position, then the mobile table is raised with the patient and a repeat series of images is taken. This diagnostic option is needed to assess the instability of the vertebrae, which are displaced under the influence of gravity. This allows you to choose the optimal treatment regimen and clearly visualize the herniated disc. Such a study is not available in every clinic.
Contraindications
Sometimes surgery with stent installation cannot be done for a number of reasons:
- unstable condition of the patient;
- severe general health: loss of consciousness, hypotension with risk of collapse, shock, multiple organ failure;
- allergy to iodine (contrast agent);
- hemophilia, other bleeding disorders;
- multiple atherosclerotic plaques over 1-2 cm in one or more cardiac arteries;
- capillary stenosis with a diameter of less than 3 mm;
- incurable malignant neoplasms.
Is it possible to do an MRI if there is presence in the body?
MRI has a number of limitations in the presence of endoprostheses, dental crowns and tattoos. The ability to undergo examination will depend on the material of the installed prosthesis. Any metal element will become an obstacle. Under the influence of a magnetic field, foreign iron-containing bodies can be displaced, damaging internal organs.
An MRI cannot be performed if the following elements are present in the body:
- dental implants – with the exception of metal-free ceramic structures;
- metal-ceramic crowns - with the exception of removable dentures;
- braces - all without exception (a metal-free brace system has not yet been developed);
- titanium plates on any bone;
- tattoo - large drawings can complicate the decoding of photographs.
An absolute contraindication is the presence of iron-containing bodies in the chest and brain. Under the influence of a magnetic field, an object may move with damage to blood vessels, which will lead to hemorrhage.
Why do they do MRI of the brain: what the study shows
On tomograms, head tissues have different color intensities (from white to black). The radiologist knows what shade is typical for each area and records all deviations. Based on the contrast of color, clarity of boundaries, shape and localization of the pathological focus, a diagnosis is subsequently made. Magnetic resonance technology makes it possible to assess the state of the blood supply, cerebrospinal fluid, nerve endings, and detect post-traumatic changes, tumors and metastases from other organs. The MRI procedure of the brain shows minute changes that are not available using other examination methods.
The arrow indicates a brain tumor on MRI scans.
Do they do MRI of the heart?
It is possible to conduct MRI of the heart using high-field devices from 1.5 Tesla, and for detailed visualization of the valves and vessels of the heart, 3 Tesla tomographs are required.
The difficulty of conducting research lies in the fact that such powerful devices are not installed in every clinic.
MRI of the heart with contrast may be prescribed to assess the condition of the myocardium after a heart attack. When it is necessary to assess the general condition of the heart muscle, alternative diagnostic methods are used.
Comparative characteristics and classification of equipment
Magnetic resonance imaging (MRI) of open and closed type is carried out using special devices - tomographs. Their main components are:
- The program receives, processes and transmits the necessary information;
- Magnet;
- Cooling system;
- Shimming, gradient, radio frequency coils;
- Protective screen.
The first open-type tomograph was designed for veterinary research.
And also cameras, for carrying out the described diagnostics based on the source of the main magnetic field, can be:
- Resistive;
- Permanent;
- Hybrid;
- Superconducting.
Cameras with a resistive system are almost never used in medical practice at this stage, due to the high energy consumption for their operation. Based on the intensity of the prevailing magnetic field, medical devices are:
- Ultra-high-field – over 2 Tesla;
- High-field – from 1 to 2 Tesla;
- Mid-field – approximately 0.5 Tesla;
- Low-field – from 0.1 to 0.4 Tesla;
- Ultra-low-field - less than 0.1 Tesla.
Ultra-high-field equipment is used only in research laboratories due to their excessive power of the main magnetic field.
Do they do MRI of the lungs?
MR imaging has low effectiveness in examining hollow organs. MRI of the lungs can be performed in combination with examination of the chest organs. MRI is also prescribed when a tumor is suspected.
But it makes no sense to use this method only for the purpose of examining the lungs. MRI does not show bronchoalveolar tissue or its changes. X-ray techniques are suitable for this purpose; CT is more often prescribed for targeted diagnostics.
What disorders in the body can the procedure reveal?
The body scan captures all tissues, from the brain to the proximal femur. In this case, it is possible to diagnose a minor pathology that does not affect the quality of life and is an accidental finding. Such pathological changes are not given any importance, since the main attention during the procedure is paid to life-threatening conditions.
When conducting a complete MRI examination of the whole body, the following structural changes are revealed:
- foci of myelomalacia in the brain;
- any violations of the bone structure of the skull;
- aneurysmal dilatation of blood vessels of any location;
- presence of infiltration in the lungs;
- any structural abnormalities of the lung tissue or bronchi;
- volumetric formations, including small ones, of any localization;
- the presence of plus tissue in the cavities of the heart or on the valves;
- structural features of the liver and pancreas;
- the process of stone formation in any area;
- the presence of purulent-inflammatory foci in any organ.
Pay attention to any extraneous space-occupying formations. They can be either a dense structure, such as a tumor, or a liquid structure, such as cysts or purulent contents.
Do they do MRI of the intestines?
An MRI of the intestine is performed, but in a slightly modified form. Hydro-MRI is prescribed to examine the large and small intestine. This method is based on the double contrast technique, when the patient drinks a solution of glucose or mannitol to straighten the bends of the intestine, and during the scanning process an intravenous administration of a contrast agent is carried out. This allows you to see the intestinal walls in detail without the need for a painful colonoscopy.
Before hydro-MRI, special preparation is needed, which includes following a diet several days before the examination and taking antispasmodics to reduce peristalsis. This method is of key importance in the diagnosis of colon cancer and acute diseases in which the introduction of endoscopic instruments is contraindicated.
How is the examination carried out?
All examinations using an open tomograph are carried out in three stages. The first stage is preparation for the procedure. The doctor collects a complete medical history and conducts a survey. Before the examination, the patient is asked to remove all metal accessories and jewelry that could harm the person being examined during the procedure.
This technique is most preferable for children
At the second stage, the diagnosis itself occurs, during which the patient is placed in a comfortable position on the table, which is very important. Because for a long time he will have to remain completely motionless. At the same time, a person can hear characteristic sounds, but he will not feel how the scanning proceeds. Usually the procedure lasts no more than 30 minutes; if the examination is carried out with contrast, the time increases to 60 minutes.
Typically, a contrast agent is injected after several CT scans. Then 10–20 ml of dye is injected into the vein, after which the study continues. The third stage involves decoding the results, and some data is sent to the attending physician immediately, the conclusion itself is sent the next day.