Limitations of magnetic resonance cholangiopancreatography
MRCP has a number of significant advantages over other diagnostic methods:
- Non-invasive. The procedure is as comfortable as possible for the patient without tissue injury or mechanical impact.
- Visualization accuracy. MR cholangiopancreatography allows the doctor to obtain a whole series of high-quality images, thereby increasing the accuracy of diagnosis.
- Versatility. Through MRCP, the doctor can not only assess the condition, size and shape of the bile ducts, but also analyze the possibilities of their functioning.
- No complications after the procedure. Unlike endoscopic retrograde cholangiopancreatography (ERCP), with MR examination there is no risk of developing pancreatitis, pancreatic perforation, etc.
- Safety. MR cholangiopancreatography takes place without ionizing radiation.
Important! MR cholangiopancreatography provides results comparable in quality to images obtained during the ERCP procedure, but without risk to the patient’s health.
https://www.youtube.com/watch?v=https:www.googleadservices.compageadaclk
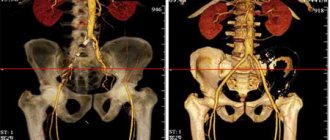
Magnetic resonance cholangiopancreatography (MRCP) is a special type of magnetic resonance imaging that creates detailed images of the hepatobiliary and pancreatic systems, which include the liver, gallbladder, bile ducts, pancreas and its duct.
Magnetic resonance imaging (MRI) is a non-invasive test that helps doctors diagnose and treat diseases.
MRI involves the use of powerful magnetic fields, high-frequency pulses and a computer system that allows you to obtain a detailed image of organs: soft tissues, bones and almost all structures inside the human body. The resulting images can be studied on a computer monitor, transmitted electronically, printed or copied to storage media. Ionizing (X-ray) radiation is not used in MRI.
Detailed images allow doctors to accurately assess the condition of various organs and systems and identify certain diseases that may be indistinguishable when using other examination methods, for example, X-ray, ultrasound or computed tomography.
The only way to ensure that high-quality images are obtained is by keeping the patient completely still during the examination and, if necessary, holding your breath at the time the image is taken. Anxiety, severe fear, or pain may prevent the patient from lying still during the procedure.
It can be difficult for overweight patients to fit adequately into a traditional MRI scanner.
Obtaining clear images may be difficult if there is an implant or other metal object in or on the patient's body. Patient movement has a similar effect.
Generally, MRI is not recommended immediately after acute trauma or injury. However, this issue remains at the discretion of the doctor. This is due to the fact that during MRI it is necessary to remove all fixation devices or life support devices from the patient’s body, which is not always possible in such situations.
Although there is no evidence that MRI is harmful to the developing fetus, the test is generally not recommended for pregnant women unless medically necessary.
MRI does not always allow one to determine the exact cause of swelling: inflammation, infection or malignancy. In addition, this study is not able to detect calcifications (calcium accumulation) in soft tissue formations such as tumors.
When is MRCP required?
A non-invasive diagnostic technique helps ICLINIC doctors find the most minimal deviations from the norm, identify developmental anomalies or acquired pathologies. MR cholangiopancreatography is indicated in cases where:
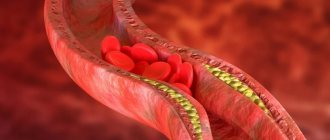
- symptoms of bile duct obstruction were identified;
- cholelithiasis occurs;
- there is a suspicion of the formation of sclerosing cholangitis;
- it is necessary to differentiate the causes of different genesis of biliary dilatation;
- there is a risk of developing cholangiocarcinoma;
- there is a need to assess the consistency of anastomoses and the functioning of the bile ducts after surgery;
- jaundice of unknown origin.
Important! MR cholangiopancreatography is mandatory in situations where it was not possible to identify the cause of abdominal pain using other diagnostic methods.
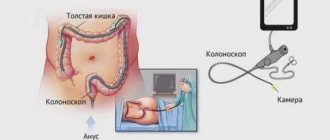
Endoscopic retrograde cholangiopancreatography (ERCP)
Indications:
- Determination of the causes of obstructive jaundice (cholangiography).
- Identification of the causes of postcholecystectomy syndrome (cholangiography).
- Clarification of indications for EPST in cases of identified diseases of the major duodenal papilla and distal common bile duct (cholangiography).
- Suspicion of pancreatic cancer (pancreatography) with insufficient information content of other research methods (ultrasound, CT, laparoscopy, tumor markers, etc.).
- A pronounced clinical picture of chronic pancreatitis with the presence of pancreatic ductal hypertension syndrome (according to ultrasound, CT), pancreatography, to clarify the indications for surgical treatment and select the volume and nature of the surgical intervention.
- Persistent pancreatic fistulas, especially post-traumatic ones (pancreatography + fistulography) - to select the optimal treatment tactics (conservative treatment, fistula occlusion, surgery, EPST, etc.).
- Recurrence of the cyst with a previously performed pancreatodigestive anastomosis; multiple pancreatic cysts.
Contraindications:
Absolute
- Acute pancreatitis.
- High probability of developing acute pancreatitis against the background of factors aggravating the prognosis.
- Acute cholecystitis and (or) purulent cholangitis.
- Pancreatic cysts complicated by perforation, bleeding, suppuration.
- Acute infectious hepatitis.
Relative
- Most cases of pancreatic cysts and verified chronic pancreatitis.
- Some cases of pancreatic cancer (verification using other diagnostic methods), and peripapillary diverticula (anatomical relationship with the papilla).
- Stenosis of the major duodenal papilla (technical impossibility without prior dissection).
- Severe concomitant diseases and functional intolerance to the study.
Areas of application of the study
MRCP is used in the following cases:
- When examining the liver, gall bladder and bile ducts, pancreas and its duct. The test can help detect growths, inflammation, infection, or calcifications (stones).
- When examining patients with pancreatitis to identify the cause of the disease.
- For abdominal pain of unknown etiology: easier diagnosis.
- It is a less traumatic alternative to endoscopic retrograde cholangiopancreatography (ERCP). ERCP is a diagnostic procedure that combines endoscopy (using an optical instrument to view internal structures of the body) and radiography.
Who should not undergo ERCP?
The procedure has a fairly large number of contraindications, among which acute inflammatory processes in the organs of the hepatobiliary system occupy a leading position. Endoscopic examination of the bile and pancreatic ducts using radiopaque agents is strictly contraindicated in cases of acute hepatitis, pancreatitis or inflammation of the bile ducts. In case of viral liver damage, the study should be postponed until recovery and completion of basic therapy.
Contraindications for ERCP
Contraindications for prescribing and performing ERCP are also:
- pancreatic cysts;
- pregnancy (regardless of gestational age);
- bronchial asthma;
- severe heart disease (heart disease, acute heart failure, history of myocardial infarction);
- allergies to drugs used for anesthesia or taking x-rays (if replacement therapy is not possible).
Important! Patients taking insulin or medications that prevent blood clotting are allowed to undergo the procedure only after adjusting the dosage regimen.
Normal criteria for ERCP
How should you prepare for research?
The nurse may ask the patient to wear a hospital gown during the examination. If the patient's own clothing is loose, comfortable and does not have metal elements, then it is allowed to wear it.
Recommendations regarding food and fluid intake before an MRI depend on the rules established by the diagnostic center. It is usually recommended that you avoid eating or drinking liquids for several hours before the test.
Because an MRI may require contrast material to be injected into the bloodstream or stomach, the radiologist or nurse always asks the patient about any allergies, including to medications or food, as well as the presence of allergic rhinitis, urticaria, or asthma. .
In addition, the radiologist needs to know about any serious diseases of the patient, as well as about the operations he has undergone. Some medical conditions, such as kidney disease or sickle cell disease, preclude the use of contrast in MRI.
A woman should always warn the radiologist about the possibility of pregnancy. MRI has been used to evaluate patients since the 1980s. twentieth century, and there are no reports of negative effects on the body of pregnant women or their children. However, during the study, the woman's body, along with the fetus, is placed inside a strong magnet.
Therefore, MRI should be performed in pregnant women only in cases where the possible benefits of the study outweigh the possible risks. In addition, the administration of contrast material is contraindicated for pregnant women. If you have claustrophobia (fear of closed spaces) or severe anxiety, the patient may ask the doctor for a mild sedative before the test.
It is advisable to leave all jewelry and other decorations at home or remove them before the examination. Metallic and electronic objects are not allowed in the treatment room as they may affect the operation of the magnet. Such objects include:
- Jewelry, watches, credit cards and hearing aids that may be damaged during the examination.
- Pins, hair clips, metal lighters and similar metal objects that cause deformation of the MR image.
- Removable dentures.
- Pens, folding knives and glasses.
- Piercing.
In most cases, MRI is safe for patients who have metal implants in their bodies, with the exception of certain types. Persons with the following devices are prohibited from undergoing an MRI or being in the examination area, unless specifically authorized by a radiologist aware of the presence of the implant:
- Built-in pacemaker
- Cochlear implant
- Some types of clips that are used for cerebral aneurysms
- Some types of metal devices (stents) that are placed inside blood vessels
https://www.youtube.com/watch?v=ytadvertiseru
The presence of medical or electronic devices in the body must be reported to the radiologist, since these devices can interfere with the examination and carry a risk that depends on their type and the strength of the magnet. Examples of such devices include, but are not limited to:
- Artificial heart valves
- Installed ports for drug administration
- Installed electronic devices, including heart pacemaker
- Limb prostheses or metal joint prostheses
- Installed neurostimulator
- Metal plates, screws, pins, stents, or surgical staples
In general, metal objects used in orthopedic surgery do not pose any risk during MRI. However, recent joint replacement may require a different study. If the doctor doubts the presence of metal objects in the patient's body, then diagnostic radiography may be performed.
X-ray examination before MRI is also required for all patients with metal objects in certain parts of the body or organs. It is important to notify the radiologist or technologist if there are any bullets, shrapnel, or other metal that may have entered the body as a result of the accident.
The inks used in tattoos may contain iron and become hot during an MRI. However, this rarely poses a serious difficulty. Fillings and braces are usually not affected by the magnetic field, but these elements can distort images during MRI of the head and face, so they should always be reported to the radiologist.
Performing an MRI on a child, especially a young child, requires sedation, that is, the administration of sedatives, which ensures immobility during the procedure. When using sedatives, parents are advised not to feed or water their child for several hours before the test.
Keeping your child safe during an MRI with sedation requires parents to fully understand and follow all instructions received from the physician. After the examination, some time must pass before the child comes to his senses. The doctor or nurse gives permission to take the child home only after making sure that consciousness is fully restored and that it is safe.
Features of preparation for the procedure
Preparing the patient for the examination is short. Before an MRI, the patient is advised to abstain from food and liquids for 8 hours before the diagnosis.
Two days before the procedure, the patient should exclude from the diet foods that stimulate flatulence (legumes, white cabbage, black bread, etc.).
The doctor recommends giving up fatty foods, coffee, strong tea, and alcoholic beverages.
Immediately before the magnetic tomography scan, you can take an anti-gas medicine and do an enema.
The described recommendations should be followed to obtain reliable diagnostic data.
Diagnostic examination is the right choice!
A standard MRI machine is a large cylindrical tube surrounded by a magnet. The patient sits on a movable examination table that slides inside a magnet.
Some CT scanners (called short-tunnel systems) are designed so that the magnet does not completely surround the patient's table. Some devices are open on the sides. Such tomographs are especially suitable for examining obese patients and people who suffer from a fear of closed spaces.
Modern open MRI scanners make it possible to obtain very high-quality images for various examinations. However, if an open type machine uses an old magnet, the image quality may be reduced. Some studies cannot be performed on an open tomograph. For more information, consult a specialist.
The computer working system that processes the images is located in the room next to the scanner.
MRI is performed on an outpatient basis. Initially, the patient removes any metal jewelry and accessories. Next, the patient must be placed on the movable panel of the device. The assistant fixes the position of the body using bolsters and belts, which ensures immobility during the examination.
After preparation, the table will be moved to the tomograph. During the procedure, the patient remains alone in the manipulation room; medical personnel are located in the adjacent room. Communication is provided through an intercom and a signal bulb.
A series of photographs are taken while holding your breath, as well as while breathing freely.
MR cholangiopancreatography lasts for 15-20 minutes. Often, diagnosis is accompanied by a standard MRI of the abdominal organs, which increases the procedure time. Therefore, in total, the examination can take about 30 minutes.
https://www.youtube.com/watch?v=ytdevru
No referral for examination? Don't know where to turn for help? Leave a request on our website using the online form right now. Administrators of the medical institution will call you back at the appropriate time.
The ICLINIC clinic has expert level tomographs with a magnetic field strength of 1.5 T, thanks to which the doctor visualizes pathological foci of minimal size. The decryption of the received images is carried out within a couple of hours, after which the conclusion along with the images is transferred to the client.
MRI examinations are carried out by qualified specialists who practice in the best European and American clinics. If it is difficult to decipher tomorgammas, it is possible. An expert radiologist reviews the results and provides his description, which either confirms the presence of pathology or makes a refutation. Thanks to this, the chance of medical error is reduced to zero.
Benefits and risks of the study
If safety rules are followed during scanning, there are no health risks. Vital signs are constantly monitored by an assistant.
Important! MRI has a number of significant contraindications, the presence of which should be reported to the doctor before the actual examination. Pregnancy is not an absolute contraindication for tomography, but in such situations contrast is strictly prohibited.
Advantages:
- MRI is a non-invasive imaging technique in which the patient's body is not exposed to ionizing radiation.
- MRI, compared to other imaging methods, allows you to obtain clearer and more detailed images of soft tissue formations such as the heart, liver and other organs. This property makes MRI an invaluable tool for early diagnosis of cancer and assessment of tumor properties.
- MRI has proven diagnostic value for a wide range of diseases, including cardiovascular pathology and stroke, diseases of the joints and muscular system.
- MRI helps doctors evaluate both the structure of an organ and its functioning.
- MRI can detect pathological lesions hidden by bone formations and therefore invisible to other imaging methods.
- The contrast material used in MRI is much less likely to cause allergic reactions than the iodine-based contrast used in traditional x-rays and CT scans.
- The information content of MRCP images is comparable to those obtained during a more traumatic test called endoscopic retrograde cholangiopancreatography (ERCP). In contrast to this study, MRCP does not have the risk of pancreatitis (inflammation of the pancreas), perforation of the pancreas and bile ducts, and the possible complications of intravenous sedation required for ERCP.
Risks:
- If appropriate safety guidelines are followed, MRI carries virtually no risks for the average patient.
- When using sedatives, there is a risk of overdose. This is why the radiologist assistant carefully monitors the patient's vital signs.
- Despite the fact that the powerful magnet in the scanner itself is harmless, problems during MRI can arise if there are devices implanted into the patient's body that contain metals.
- When contrast material is injected, there is a very small risk of developing an allergic reaction. Such reactions are usually very mild and go away quickly when appropriate medications are prescribed. If allergy symptoms occur, a radiologist or nurse will immediately provide the necessary assistance.
- One recently described, but extremely rare, complication of MRI is nephrogenic systemic fibrosis, which develops when large doses of gadolinium-based contrast material are administered to patients with impaired renal function.
What is the basis for the research?
A special probe for ERCP is inserted through the oral cavity, esophagus and stomach into the duodenum - the patient turns to a position lying on his left side. Retrograde cholangiopancreatography is performed in several stages - first, an inspection of the intestinal mucosa and the surface of the major (Papilla of Vater) is carried out to assess its condition.
At the next stage of RCP, the papilla is cannulated by introducing a probe into its lumen, and the depth of insertion depends on the purpose of the study. If it is necessary to study all the ducts of the hepatobiliary tree and pancreas, a relatively shallow penetration is sufficient; in a selective procedure, the probe is inserted up to the area being examined.
Unlike traditional X-rays and computed tomography (CT), MRI does not require the use of ionizing radiation. Instead, the radio waves generated by the magnet change the direction of rotation in a powerful magnetic field of protons, which are the nuclei of hydrogen atoms.
In most MRI machines, a magnetic field is generated when an electric current passes through coils. Other wires located in the machine, and in some cases placed on the area of the patient's body that needs to be examined, send and receive radio waves. This generates signals that are picked up by sensors.
The signals are processed by a computer program, resulting in a series of images, each showing a thin section of tissue. The resulting images can be examined from a variety of angles by a radiologist. Often, MRI is the best way to distinguish pathologically altered, diseased tissue from healthy tissue than other imaging techniques, such as radiography, CT or ultrasound.
How the procedure is carried out in clinics in Belgium
The key to successful ERCP and the absence of complications is complete relaxation of the walls of the duodenum and duct walls, as well as suppression of the secretion of bile and pancreatic juice.
In clinics in Belgium, a complex of drugs is used to ensure that the desired effect is achieved.
It includes:
- sedatives and hypnotics;
- myotropic antispasmodics;
- m-anticholinergics;
- blockers of H₂-histamine receptors and proton pumps.
Some of these drugs may be administered directly during the procedure through an endoscope.
Anesthesia of the pharynx is carried out using modern anesthetics such as Ultracaine or Bupivacaine.
An endoscope with lateral optics under the visual supervision of an endoscopist is passed through the esophagus and stomach into the duodenum. A thin Teflon probe is then passed through the endoscope and its end is inserted into the common outlet of the gallbladder and pancreatic ducts (the Vater nipple).
After this, a water-soluble radiopaque substance is injected through a probe into the main pancreatic duct and common bile duct. On the monitor, the endoscopist sees in real time how the ducts are filled with contrast agent.
This makes it possible to see not only organic, but also functional disorders in the examined organs.
Abroad, due to the fact that during ERCP different tasks can be solved, as well as due to differences in the anatomical structure of the Vater nipple in different people, different types of catheters are used. The type of catheter used is selected individually in each specific case. This leads to better results in difficult cases and further reduces the risk of complications.
How is the research conducted?
MRI can be performed either on an outpatient basis or during the patient’s hospitalization. The radiologist's assistant places the patient on a moving table. The body position is secured using belts and special bolsters that help the patient lie still.
Devices containing wires that send and receive radio waves are placed around the area of the body being examined.
If it is necessary to use contrast material during the test, the nurse inserts a catheter into a vein in the arm. A bottle of saline solution may be connected to the catheter. The solution provides continuous flushing of the system, which prevents it from clogging before contrast material is injected.
After all preparations, the patient’s table moves inside the magnet, and the radiologist and nursing staff leave the treatment room for the period of the study.
If contrast material is needed, it is administered intravenously after the initial series of images. During or after the injection, the doctor receives an additional series of images.
The MRCP procedure itself takes about 10 minutes. However, the test is usually combined with a standard abdominal MRI, which takes about 30 minutes and requires the use of contrast. In such a situation, the study takes an average of 45 minutes.
How to prepare properly
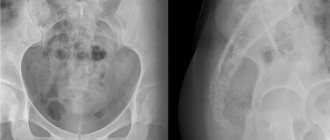
Before starting the ERCP procedure, the doctor prescribes a preparatory examination in a hospital setting, which includes laboratory tests, chest X-ray, electrocardiogram and abdominal ultrasound.
Before ERCP, the patient will need to undergo a contrast agent and local anesthetic tolerance test. To relieve anxiety, the doctor conducts explanatory conversations. If the anxiety is too strong, sedatives are prescribed a few days before the examination.
The day before the procedure
The day before the start of ERCP, the patient is contraindicated for any overexertion or excitement. Particular attention should be paid to nutrition. Food should be light and nutritious enough. The diet should be dominated by vegetable purees, pasta, white chicken meat, light broths, and cereals. The last meal should take place no later than 18:00 on the evening before the examination day. A cleansing enema or taking a laxative is recommended 2 hours before bedtime.
On the day of the study
You should not eat or drink water on the day of ERCP. To relax the papilla of Vater and duodenum and slow down peristalsis, premedication is used using Atropine, No-Shpa, Promedol or other drugs that are selected by the doctor based on the condition of the patient’s body. To reduce the sensitivity of the oropharynx, immediately before the examination, it is irrigated with Lidocaine or Dicaine, or a small amount of their solution is taken orally.
Duration of the study
Interesting facts about MRI
The word “nuclear”, which is in the full name of the physical phenomenon (NMR), explains that the magnetic field interacts with the nuclei of hydrogen atoms in the human body. It does not change their work and does not cause any negative impact.
The average duration of one “MR-cholangiopancreatography” study in our center is up to 20 minutes (less than with conventional studies due to the modification of the “SQ Engine” tomograph), however, it all depends on the detected changes: sometimes, to clarify the disease, the radiologist can expand study protocol and resort to the use of contrast enhancement. In such cases, the research time increases.
What should you expect during and after the study?
In most cases, an MRI is completely painless. However, some patients experience discomfort due to the need to lie still during the test. Other patients may experience an attack of claustrophobia (fear of closed spaces). This is why doctors offer sedatives for anxious patients, but in reality only 1 in 20 people need them.
If it is necessary to use contrast material, slight discomfort may occur during placement of the intravenous catheter.
During the study, a local increase in the temperature of the body area being examined is possible, and this is normal. However, if this phenomenon greatly bothers the patient, it is important to inform the doctor about it. It is extremely important that the patient lie absolutely still while the images are being taken (from several seconds to several minutes at a time).
https://www.youtube.com/watch?v=ytcreatorsru
During some tests, the doctor asks the patient to hold their breath. The tapping or clicking sounds that the magnet makes as it produces high-frequency pulses help you know when image capture has begun. You can relax a little between series of shots, but you should still try to maintain your body position, without moving if possible.
Typically, the patient is alone in the treatment room during the examination. However, the radiologist can see, hear and talk to the patient at all times via a two-way communication system. Staff at many diagnostic centers allow relatives or friends of the patient to remain in the room until the test begins. However, they then need to go out to avoid exposure to the magnetic field.
The patient may be given headphones or earplugs to help suppress the loud knocking and humming of the scanner while images are taken. The patient has the right to ask for headphones himself. Children must be provided with headphones or earplugs of the appropriate size. The MRI scanner is air conditioned and well lit. Some centers play soft music during the examination.
When a contrast material is injected, there is normally a feeling of coolness or a rush of blood that lasts a couple of minutes. The patient experiences some discomfort when inserting and removing an intravenous catheter, which can leave hemorrhage under the skin. It is extremely rare that irritation occurs on the skin at the site of needle insertion. Some patients experience a metallic taste in their mouth after receiving contrast material.
If the procedure was not accompanied by the use of sedatives, then a recovery period after it is not required. A return to normal activities and normal nutrition is possible immediately after the study. Some patients experience side effects when contrast is administered, such as nausea and local pain.
Manufacturers of contrast materials do not recommend breastfeeding for 24-48 hours after intravenous administration of contrast to the mother. However, experts from the American College of Radiology and the European Society of Urogenital Radiology report that research suggests that it is safe to continue breastfeeding after the use of intravenous contrast materials.
The American College of Radiology guidelines on the use of contrast materials state: “A review of the published literature indicates that oral administration by infants of small amounts of gadolinium-based contrast material that is excreted in breast milk does not cause any toxic effects.
Therefore, we believe that after the introduction of such materials, continued breastfeeding is safe for both mother and baby. If the mother is concerned about the development of any unwanted effects, she should be given the opportunity to either continue breastfeeding after administration of gadolinium contrast or temporarily discontinue it.
If the mother decides to stop breastfeeding for 24 hours after administration of the drug, then active expression of milk from both breasts is recommended during this period. Alternatively, a breast pump may be used before an examination using a contrast agent, which allows for enough milk to be fed to the baby for 24 hours after the procedure.”
Possible complications
Pancreatitis
One of the most common complications of ERCP is pancreatitis. According to statistics, it develops in 1.3-5.4% of patients and can be provoked by a number of factors accompanying such a study.
The development of pancreatitis after ERCP can be facilitated by the patient’s history of this disease, long and complex cannulation of the papilla of Vater, sphincterotomy, the need to re-introduce contrast into the ducts, etc.
Bleeding
In more rare cases, ERCP is complicated by clinically significant bleeding. The frequency of such an undesirable consequence of the study is 0.76-1.13%.
Bleeding often appears after additional surgical procedures are performed. Predisposing factors to its occurrence may be pathologies of the blood coagulation system and the small size of the mouth of the large duodenal papilla.
What is the difference between tomographs?
The key to correct diagnosis differentiation is reliable images, which are created only through the full interaction of medical personnel and diagnostic equipment. But at the same time, one should take into account the fact that, despite the enormous practical experience of a radiologist, it is impossible to achieve high-quality visualization of pathologies on tomographs with low magnetic field induction (up to 0.5 Tesla). Thus, diseases of the brain are not displayed due to the complex structure of the organ and the lack of accuracy and clarity of the images. Read more…