The essence of diagnosis
Magnetic resonance imaging is a method of studying internal organs and tissues using nuclear magnetic resonance. In essence, a magnetic storm is created, as a result of which special devices pick up signals and transmit the image to the monitor. The response occurs due to hydrogen atoms, which are arranged in a certain sequence. Examination of the bile ducts using MRI is called cholangiography.
For humans, the procedure is painless, but may seem unpleasant. With high sensitivity to magnetic vibrations, dizziness, headache, and weakness appear. It goes away a few hours after the examination is completed. MRI is used as an independent procedure or as an additional procedure to clarify the diagnosis and obtain more accurate data.
The tomograph can be of open or closed type. Standard equipment is a large pipe with a magnet inside. During the examination, the person is placed inside. In the old devices there was much less space, the confined space put pressure on the psyche. In new equipment, the cylinder is expanded on the sides and is perceived more easily and calmly. Open type tomographs are used less frequently because they provide insufficiently accurate images. For people with claustrophobia they are an alternative option.
Prevention of consequences
It should be understood that any surgical intervention is traumatic for the body, and it needs time to adapt and recover. Therefore, you should follow the recommendations of doctors.
- You should not adhere to any long-term diet after removal of the gallbladder in the absence of problems with stool and abdominal pain: a varied healthy diet is necessary.
- If you have diarrhea or bloating, you should limit your intake of fatty, spicy foods, drinks containing caffeine, and the consumption of dairy products, as well as treating bile outflow dysfunction.
- It is necessary to control weight and hormonal levels in the presence of relevant diseases.
An expert on the site Pokhmelye.rf, gastroenterologist Daniela Purgina, refutes the typical misconception regarding cholecystectomy.
It is a very common belief that after removal of the gallbladder, you need to constantly take some kind of medication to drain bile. In fact, there is no need for this. Taking choleretic drugs is completely unjustified, since the bladder has been removed and there is nowhere to drive the bile from; it will go from the liver through the ducts to the intestine. Ursodeoxycholic acid drugs are prescribed only if there is a risk or stones have been identified in the bile ducts.
What is postcholecystectomy syndrome
The operation to remove the gallbladder is scientifically called cholecystectomy. Such a surgical intervention can go without problems, but it can cause some complications.
If, after cholecystectomy, problems with the outflow of bile occur, accompanied by characteristic symptoms, doctors call this postcholecystectomy syndrome (PCES). Symptoms may occur immediately after surgery or some time later.
This pathological condition is most often associated with dysfunction of the sphincter of Oddi, which plays a key role in the normal outflow of bile and pancreatic juices. The fact is that the contractility of this sphincter of the duodenum is impaired. According to studies, the disease is diagnosed in approximately 10–15% of patients after gallbladder removal. Manifestations may vary from person to person, but in any case you will need to see a doctor and begin treatment to avoid more serious complications.
What causes PCES to develop?
The development of postcholecystectomy syndrome is associated with various problems that arise in the gastrointestinal tract after removal of the gallbladder. One of the most common causes is disruption of the normal functioning of the sphincter of Oddi, which is located on the wall of the duodenum. This structural element of the digestive system is a circular muscle responsible for the supply of bile and pancreatic enzymes to the intestinal cavity. Upon a signal, the sphincter of Oddi opens, which is accompanied by the outflow of bile and pancreatic juices into the intestines, and also closes upon a signal.
Pathological changes in the sphincter of Oddi develop in most patients precisely after surgery to remove the gallbladder. As doctors explain, the mechanism of the disease works like this:
- In the absence of a bladder, signals about its filling do not arrive to the sphincter, which leads to the formation of constant tension in the orbicularis muscle and the development of congestion in the pancreatic gland and hepatic ducts.
- An uneven outflow of bile leads to a decrease in its bactericidal effect in the small intestine, and bacteria begin to multiply excessively in it. These microbes are opportunistic, that is, they should even be present in small quantities in the intestines, but when there are a lot of them, problems arise (gas formation, pain in the navel).
Among the most common causes of symptoms of PCES are also:
- the presence of residual calculi (stones) in the bile ducts after surgery;
- progressive bile duct cyst;
- biliary dyskinesia;
- stone formation as a result of obesity or diabetes.
Sometimes the cause of this pathological symptom complex may be severe postoperative pain, which is not relieved by non-narcotic analgesics, and the accumulation of effusion (fluid) in the area of the surgical intervention.
Rarely (about 5% of clinical cases) the true reasons for the development of changes in the functionality of the sphincter of Oddi remain unknown to doctors.
How does PCES manifest itself?
As already mentioned, the symptoms of postcholecystectomy syndrome can vary. Just in case, after surgery to remove the gallbladder, listen to your body - and if alarming phenomena occur, consult a doctor. Bad signs can appear either a few days or several weeks after surgery.
The most common manifestations of PCES include:
- dyspeptic symptoms, which are manifested by a feeling of bitterness in the mouth, nausea, flatulence;
- diarrhea or constipation;
- aching, cramping pain of varying intensity in the right hypochondrium, which radiates to the right shoulder and collarbone;
- bloating, excess gas formation;
- hypovitaminosis conditions associated with insufficient absorption in the intestine;
- jaundice and chills with an increase in body temperature of 38°C and above (if stones remain in the bile ducts after surgery).
The disease can take various clinical forms. Sometimes after removal of the gallbladder the following consequences occur:
- relapses of stone formation in the biliary tract;
- strictures (narrowing of the lumen) of the common bile duct;
- papillitis (inflammation of the papilla of the excretory duct in the duodenum;
- the formation of adhesions that disrupt the outflow of bile fluid in the subhepatic space;
- inflammation of the pancreas;
- ulceration of the gastroduodenal digestive tract.
Pain in this area can occur not only after surgery, but also with the entire organ. Read the article about how to identify the disease by the nature of the pain and how to treat pain in the gallbladder.
A case from the practice of gastroenterologist Daniela Purgina, an expert on the website Pokhmelye.rf.
I rather remember a whole group of cases where a patient with asymptomatic cholelithiasis had his gallbladder removed, and after the operation, postcholecystectomy syndrome developed or, even worse, hologenic diarrhea (that is, diarrhea with bile). So the tactics should be in the maximum effort to preserve the organ.
Modern diagnostics
To confirm postcholecystectomy syndrome, the patient needs a series of examinations. As a result, the doctor will be able to determine the main causes of the development of the pathological condition and the degree of functional disorders of the digestive system. Unfortunately, most patients do not immediately turn to specialists.
Diagnostics usually includes the following steps:
- Conversation with the patient, detailed discussion of complaints, study of the medical history and life of the patient, identification of the leading pathological signs from all complaints.
- Clinical examination of a person, allowing to determine the localization of the source of the disease and assess the extent of the disorders.
- A set of laboratory tests, which includes general and biochemical blood tests with assessment of the functioning of the liver and pancreas, analysis of thyroid hormones, tests for viral hepatitis.
- Ultrasound examination of the organs of the hepatobiliary zone (standardly includes the liver, gall bladder and bile ducts. Since the gall bladder has already been removed, only the ducts and liver are examined).
- Esophagogastroduodenoscopy.
- If necessary, endoscopic examination of the bile ducts (endosonography, endoscopic retrograde cholangiopancreatography), manometry of the sphincter of Oddi, MRI and abdominal organs is also performed.
A complete and detailed diagnosis of suspected PCES allows the doctor to draw conclusions about why the disorders began, how far they have gone, whether there are any serious complications, and what therapy is suitable for treatment. Read on to learn how to treat post-operative problems.
How to be treated
The main thing in the treatment of PCES is to eliminate the factors that triggered the development of symptoms. The main principles of such therapy are:
- eliminating the influence of factors contributing to the occurrence of pathological manifestations;
- symptomatic treatment of dysfunctions of the organs of the hepatobiliary region;
- prevention of possible complications.
As a rule, in addition to drug intervention, doctors recommend in the first stages an increase in the frequency of food intake to 5–7 times a day to normalize the outflow of bile. Any strict diet is usually not required; this is discussed individually.
In order to eliminate the symptoms of the disease, the patient may be prescribed:
- analgesics and antispasmodics, since inflammation is accompanied by pain and spasm of the sphincter of Oddi;
- proton pump inhibitors to reduce acidity in the upper gastrointestinal tract if there is inflammation there;
- drugs to normalize the flow of bile;
- antacids to combat high acidity;
- non-absorbable antibiotics to eliminate bacterial overgrowth in the small intestine.
Sometimes medications cannot correct the problem, in which case surgery is indicated. Surgical treatment methods are aimed at restoring the patency of the bile ducts and normalizing the functioning of the sphincter of Oddi.
How to avoid complications after gallbladder removal
Doctors are well aware that postcholecystectomy syndrome is a common occurrence. However, today there are no special measures to prevent it. When you have your gallbladder removed, you must remember that PHES may not catch up with you months later.
In order to reduce the risk of its occurrence, you should follow the principles of a healthy lifestyle: a balanced diet, giving up bad habits, adequate sleep and moderate physical activity. People with high cholesterol levels and endocrine system disorders should be regularly examined by doctors.
The prognosis for cure for PCES directly depends on how effectively the problem that caused its development was dealt with.
Indications
The diagnostic method is prescribed to determine neoplasms, their shape, size, location, and nature. MRI is performed after an ultrasound examination of the abdominal organs in order to clarify the diagnosis. The indication for use of the method is suspicion of the following pathologies:
- Sclerosing cholangitis is inflammation that causes narrowing of the bile ducts;
- Concretions – stones;
- Congenital anomalies;
- Traumatic injuries to the liver, gall bladder;
- Polyps and other neoplasms.
MRI is prescribed to identify pathologies, monitor the development of the disease, and evaluate the effectiveness of therapy.
Types of cholecystectomy
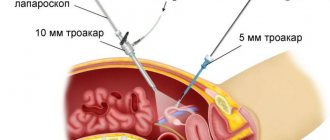
The classic method of removing the gallbladder involves creating an access through the anterior abdominal wall.
This is an open operation, accompanied by significant trauma and an increased risk of infectious and inflammatory complications. An incision in the muscles of the abdominal wall prolongs the rehabilitation period and introduces significant restrictions on the patient’s lifestyle. Laparoscopic cholecystectomy is considered optimal for the patient. The method involves performing an operation using endoscopic equipment, which is inserted into the abdominal cavity through small punctures. Modern operating techniques make it possible to minimize injuries, avoid discomfort in the postoperative period and reduce rehabilitation time to several days.
Contraindications
The procedure has contraindications, but there are not many of them:
- Fear of confined spaces, mental disorders;
- Metal plates;
- Dentures;
- Hearing implants;
- Metal objects remaining in the body after injury - bullets, fragments;
- Pacemaker;
- Alcohol intoxication.
MRI of the gallbladder is not performed in the presence of infectious or viral diseases in the acute stage, when a person feels unwell, or an increase in temperature is observed. The study should not be started if the patient is in a state of severe depression or nervous exhaustion. In this case, during the study, panic attacks may occur with various consequences, including loss of consciousness. Weight restrictions – 120 kg.
What are the absolute contraindications for abdominal MRI?
The method of performing abdominal MRI is based on capturing resonant vibrations from organs and tissues of the human body in a magnetic field.
Although it is considered the safest of diagnostic tests, there are contraindications for its use. The magnetic field that is created around the patient affects materials that have ferromagnetic or paramagnetic properties. It is capable of attracting and moving ferromagnetic objects, increasing their temperature, and influencing the operation of electrical appliances.
Therefore, an absolute contraindication for abdominal MRI is the presence of metal objects or electronic devices inside or on the human body:
- electrical stimulators. This is a pacemaker, external pacemaker, neurostimulator, defibrillator;
- electronic inner ear prosthesis (cochlear implant). A hearing aid is not a contraindication if it can be removed before the procedure;
- vascular clips. They are used to clip brain aneurysms, blood vessels during surgery, and are also applied to vessels to restrict blood flow - for example, to treat uterine fibroids to cause their reverse development. Titanium clips on the ducts and vessels of the gallbladder after laparoscopic cholecystectomy are a relative contraindication;
- insulin infusion pumps;
- artificial heart valves if they contain ferromagnetic materials. Biological implants are not considered a contraindication;
- artificial joint prostheses, plates, pins. Most of them are diamagnetic, but they can distort the image. This group also includes dental implants and crowns. In such cases, an individual approach is required;
- Ilizarov apparatus or metal osteosynthesis;
- shrapnel wounds; if you are not sure that all the fragments have been removed, you must first take an x-ray;
- stents. These are mesh tubes that are used to restore stenotic vessels; they do not interfere with MRI, but it can only be done 2-3 months after surgery;
- vena cava filters, metal meshes in the inferior vena cava, for catching blood clots;
- piercings or tattoos made with inks containing metal.
If you are indicated for an MRI of the abdominal cavity, do not forget to warn your doctor about the presence of such inclusions; this may be a contraindication to the procedure.
Preparation
The procedure does not require special preparation, but must be performed on an empty stomach. The last meal should be at least 5 hours before the examination. For convenience, it is prescribed in the morning. If a person smokes, one should abstain from this habit for a day to keep the gallbladder full. A specialist may recommend, a couple of days before the examination, to exclude from the diet foods that cause flatulence and increased gas formation.
Other preparatory procedures are carried out immediately before the study. Remove chains, hairpins, rings, belts with a metal buckle, and other items containing it. In some cases, experts allow you to leave earrings or a chain, since the magnetic field will be directed to the stomach and not the head, but it is better to remove everything or not put it on when going for an examination.
Conducting research
The device is located in a special room where no one except the patient should be present during operation. The person lies down on the couch, relaxes, and needs to remain in this position for 5 to 30 minutes. A special lid is closed over him, and the device moves around the person, examining the necessary organs.
During operation of the tomograph, noise is felt, so the person wears headphones. Inside such a “spacesuit,” air circulates freely, it is light, and if necessary, you can contact a specialist through a loudspeaker. Moving is prohibited, as this leads to a distortion of the result. If a person cannot lie still, anesthesia is administered. If you have a disease such as claustrophobia, it is possible to carry out the procedure in an open room.
Cholelithiasis
It occurs with the formation of stones and crystalline deposits in the gallbladder and ducts. More often, pathology develops in overweight people, in the presence of chronic pathologies of the liver, pancreas, and stomach. The process of stone formation proceeds unnoticed by the person himself, and has a stage of active growth and decay. In the gallbladder, a neoplasm is easily detected using ultrasound; MRI does not make sense.
At a certain point, the stones begin to come out into the ducts, causing a sharp, severe, sharp pain in the upper abdomen, under the shoulder blade on the right side. A bitter taste appears in the mouth, nausea, vomiting, diarrhea. In this case, a conventional ultrasound examination will not be able to show neoplasms in the ducts; an MRI is prescribed. Timely diagnosis and qualified treatment help prevent obstructive jaundice, pancreatitis, obstruction, and cancer.
Technique of the operation
The intervention is performed under general anesthesia. Anesthesia is selected on an individual basis. For pain relief, modern drugs are used that do not have an adverse effect on the patient’s body. Cholecystectomy can be performed using various techniques:
- Classic.
The surgeon makes 3-4 punctures in the abdominal wall and hypochondrium, through which he inserts trocars with endoscopic instruments. Carbon dioxide is injected into the abdominal cavity to improve visualization. The doctor dissects the artery that feeds the cystic duct, then removes the gallbladder. The organ is removed using a special basket through one of the holes. The punctures are sutured and a bandage is applied. - Minilaparoscopic.
The operation is performed using miniature instruments (3.5 mm in diameter), which makes it possible to reduce the size of the entrance holes and provide a better cosmetic effect. The technique for removing the gallbladder corresponds to classical laparoscopic cholecystectomy. - Single-puncture.
The method involves creating access to internal organs through one incision in the navel area with a diameter of 2.5 cm. Through it, a SILS port with endoscopic instruments is inserted into the abdominal cavity. The surgical scar in the navel area is almost invisible.
The appropriate cholecystectomy technique is selected for each patient individually. If complications develop, perforation of the bladder walls and the need for an abdominal cavity revision, they always resort to an open (laparotomy) technique.
Cholecystitis
Inflammation of the gallbladder develops as a complication of gallstone disease or for other reasons. In the absence of timely treatment, it becomes chronic. Inflammatory processes lead to thickening of the walls, disruption of the outflow of bile, and the appearance of stones.
MRI is performed at any stage of the disease, at the first signs. Allows you to identify pathology at the initial stage, which prevents complications and transition to a chronic form. Signs: aching pain under the right rib, nausea, vomiting, bitter taste in the mouth, diarrhea after eating, increased gas formation, bloating.
In case of exacerbation of cholecystitis, an MRI with the introduction of a contrast agent is prescribed. This technique gives a clearer picture.
Indications for gallbladder removal
Cholecystectomy is performed to treat recurrent cholecystitis and complications of cholelithiasis. The reasons for the operation are the following conditions:
- progressive acute inflammation of the bladder;
- stagnation of bile in the liver ducts with the formation of stones;
- persistent pain syndrome due to cholelithiasis;
- formation of large gallstones (2.5 cm or more);
- deposition of calcium salts in the walls of the organ;
- stones in the common channel.
The need for surgery is determined individually, taking into account the medical history and characteristics of the development of the disease.
Polyps
Neoplasms appear due to the proliferation of cells in one or more places under the influence of provoking factors. New growths form that protrude into the gallbladder, disrupting its normal functioning.
Polyps are often diagnosed using ultrasound, but in this case it is impossible to determine the nature of the tumor and its structure. Endoscopic examination through the small intestine makes it possible to assess the structure of polyps, size, and exact location. MRI does all this with high accuracy in a few minutes, avoiding any unpleasant sensations.
In addition, computer diagnostics evaluates the condition of the gallbladder and ducts, studies the histological structure of tumors, and identifies concomitant diseases. The method gives a clearer, more multifaceted picture. The study also determines the narrowing of the lumen, the presence of an inflammatory process, changes in tone, tissue structure, stones, and tumor.
Dyskinesia
The pathology is associated with a change in the contractility of the gallbladder muscles, which leads to disruption of the outflow of bile. Stagnant processes persist in the case of involuntary muscle contraction and in the complete absence of motor ability of the organ. Diagnosing pathology is quite difficult. A comprehensive examination is prescribed. MRI is performed in case of a controversial diagnosis or unclear clinical picture.
The provoking factors of primary dyskinesia are pathologies of the endocrine system, dysfunction of the sweat glands, and menopause. Gastrointestinal diseases, hepatitis, giardiasis, intestinal infections, and hormonal imbalance lead to stagnant processes.
Features of MRI with contrast
It differs from a regular MRI only in that immediately before the procedure a special substance is injected through a vein or mouth. This procedure is prescribed in case of detection and examination of neoplasms, to determine the nature, tissue structure, exact location, size.
The special substance is called gadolinium. The drug rarely provokes the development of an allergic reaction and does not cause side effects. Makes it possible to accurately determine the nature and structure of anomalies and pathologies.
Initially, MRI is performed in the usual way, then gadolinium is administered. This is done intravenously or by drip during the procedure. In the first case, the person needs to lie down for about an hour, after which the study continues. No more than 10 ml of the product is administered at a time. The solution enters the altered cells, making them visible and their outlines clear.
Indications for MRI with contrast:
- Malignant neoplasms;
- Unknown infection;
- Detailed diagnostics in case of doubtful diagnosis.
Contraindications to the use of the method are individual intolerance to gadolinium and renal failure. When it is difficult to remove the active component of the contrast agent from the body, toxicosis occurs.
Indications and contraindications for examination
Tomography is necessary to determine the location of the gallbladder, identify changes, pathologies, and stones in it. Main indications for MRI of the gallbladder:
- abdominal trauma;
- foreign bodies or parasites in the organ, ducts;
- abnormal development;
- suspicion of an infectious process;
- pain in the right hypochondrium that appears for an unknown reason;
- symptoms of cholecystitis and cholangitis (inflammation of the bladder and its ducts);
- hepatitis;
- poor laboratory tests (high concentration of liver enzymes, bilirubin, etc.);
- damage to the gallbladder or liver;
- various neoplasms (including suspicion of malignancy or metastasis);
- stones;
- abnormal liver development;
- duct obstruction.
MRI of the gallbladder is performed before surgery, during the rehabilitation period to monitor the dynamics of recovery. In other cases, tomography can be performed as a preventative measure or to clarify a previously made diagnosis using other diagnostic methods (for example, after ultrasound).
Conducting a survey
The patient is placed on the retractable couch of the device. The legs, arms and head are secured with soft straps to eliminate involuntary movements that could distort the image. If an MRI is performed with contrast, it is administered intravenously, with a syringe or through a catheter.
If the patient has cardiovascular pathologies or diseases of the respiratory system, but devices are attached to the body to monitor the rhythm of the heart and breathing.
After all the preparations, the doctor goes into the next room and turns on the tomograph. The couch slides into the tunnel and scanning begins. During this, the device makes a slight noise and clicking noise.
The tomograph has a built-in intercom through which the doctor communicates with patients (he may ask them to hold their breath, take a deep exhale or inhale). When the scan is completed, the couch moves out of the tunnel. The duration of the procedure is from 30 minutes to an hour (this depends on whether a contrast agent is used - it will take longer with it).
Benefits of MRI
At the moment, magnetic resonance imaging is one of the best diagnostic methods. Allows you to examine any tissues, organs in the human body, obtain a three-dimensional image, and a quick result. On the screen you can get a picture in any projection, despite the fact that the person is in the same position.
The procedure is absolutely painless, so absolutely everyone agrees to it. With high accuracy it makes it possible to determine the nature of the pathology, associated anomalies, and inflammatory processes at the initial stage. MRI does not cause side effects, and you will not have to recover as much as after an endoscopy. The result is accurate and fast. You can hear the verdict within an hour. The procedure itself lasts from 5 minutes to 60.
5. Contraindications to MRI of the biliary tract
Doctors do not recommend cholangiopancreatography (MRCP) and cholangiography for lactating and pregnant women.
People suffering from claustrophobia and epilepsy should decide to undergo research only after consultation with their doctor or a competent healthcare professional with the necessary qualifications and specialization.
In acute and chronic forms of renal failure, as well as previously identified allergic reactions, the use of magnetic resonance imaging using a contrast agent is contraindicated.
It is strictly prohibited to conduct an MRI examination if the following is present in the body:
- Magnetic and electromagnetic devices (insulin secretion stimulants, pacemakers, hearing aids).
- Foreign bodies made of metal containing metal shavings or metal coating (shot, bullets).
- Surgical staples.
We recommend reading: Do allergies protect against cancer?
Which is better MRI or CT
Computed tomography is performed using x-rays. A three-dimensional image appears on the monitor screen, which allows you to assess the condition of the organ from different angles. The capabilities of CT and MRI are somewhat different, therefore the indications are different. Computed tomography is more informative when examining hard tissues. Accurately detects stones, cysts, tumors, polyps. To obtain a more accurate result, a contrast agent is used.
Computed tomography is often prescribed for injuries, bleeding, and to examine internal organs. As for MRI, this is like the final stage of diagnosis with a complete, comprehensive picture. Each method is informative and is used in different cases. The doctor can tell you which one will best display the picture, based on the clinical picture, complaints, and preliminary research using other methods.
CT has more contraindications:
- Pregnancy;
- Lactation;
- Diabetes;
- Kidney failure;
- Thyroid diseases.
It is prescribed to children if other methods are not very informative. There is a weight limit; it is impossible to diagnose a person weighing more than 200 kg. The procedure takes on average 15 minutes. Before the test, you are prohibited from eating for 5 hours. It is recommended to come to the examination in loose clothing.
It is impossible to answer unequivocally the question of which is better. Because each method is informative in different cases. You can argue about safety for a long time. In general, both methods do not pose a threat to health or well-being. The cost of the procedures also differs little. The average price for research of one organ is 4 thousand rubles.
CT examination of the gallbladder and ducts
Similar to magnetic resonance imaging, CT cannot diagnose stones in the bladder. This study is also carried out in conjunction with ultrasound to establish an accurate diagnosis. X-ray examination is indicated for patients with excess body weight (but not more than 150 kg), with an anatomically elevated location of the liver.
When is the procedure indicated, what are the contraindications?
A CT scan is performed when an atypical clinical picture is detected in a patient or to monitor the dynamics of an already diagnosed disease. The list of indications for this procedure is:
- cholecystitis;
- cholelithiasis;
- violation of the patency of the ducts;
- bleeding of unknown nature;
- suspicion of oncology;
- preoperative preparation.
A detailed examination of the gallbladder requires the introduction of contrast into the body. The use of this substance is unacceptable if the patient is individually intolerant to iodine or has thyroid and kidney diseases.
Stages of CT, features of the study with contrast
It is recommended to prepare in advance for a CT examination of the gallbladder. A few days before the procedure, foods that stimulate excessive gas formation are excluded from the patient’s diet: baked goods, dairy products, vegetables with fiber. It is recommended to drink 2-3 glasses of water a couple of hours before the procedure.
Before a computed tomography scan of the gallbladder, the patient removes metal jewelry and takes a stationary position on the machine table. A CT scan of the gallbladder lasts several minutes, during which the table moves through the ring. During the procedure, the patient is alone in the office, but can contact the doctor via feedback.
CT scans of the gallbladder are often performed using contrast, which fills the tissue and improves their visualization in the image. The component does not harm the patient’s health and is eliminated from the body 24 hours after administration. So that the drug has time to spread through the blood vessels and fill the organs, it is consumed in the evening, before computer diagnostics.
What does the photo show?
A peculiarity of studying an organ using X-rays is the impossibility of detecting stones at the initial stage. Using computed tomography, solid formations requiring surgical intervention are diagnosed. When using a contrast agent, neoplasms may appear larger due to the simultaneous visualization of gases and blockage of ducts, and therefore the decision on surgical intervention is made by the doctor based on a comprehensive study of the pathological process.
MRI and CT are effective methods for diagnosing diseases of the gallbladder and ducts. The effect of a magnetic field on the body provokes response impulses from particles of the tissues being examined, which are transmitted to the tomograph for processing and transformation into three-plane images. To make an accurate diagnosis, the body is examined using X-rays and a contrast agent.
Cost of MRI procedure
The examination can be done in specialized public and private clinics, but in any case, the procedure is paid.
- MRI of the gallbladder – 4000 – 5000 rubles;
- Study with contrast – 5,700 rubles;
- Recording a photo to disk – 500 rubles;
- Recording on a flash card – 1000 rubles.
Consultation with a specialist costs about 1000 rubles. Comprehensive examination of the whole body - 100,000 rubles, search for oncology - 20,000 rubles. Prices may vary slightly between clinics. Discounts and promotions are offered periodically. You can find the addresses of the centers via the Internet or make an appointment by phone. Or all the information will be provided by the attending physician, who will give a referral for the procedure.
What diseases can be diagnosed using MRI of the gallbladder?
MRI of the gallbladder and ducts can detect various diseases.
Gallstone disease
This disease is one of the most common. More often it affects women from 20 to 40 years old. The causes that lead to the formation of stones are stress, poor diet, and pregnancy. Stones can be either passive or active - move through the bladder, enter the duct with bile, block it, and cause damage. Gallstone disease is accompanied by pain, heartburn, loss of appetite, and in advanced cases, jaundice. For a detailed examination in this case, MRI of the gallbladder with contrast is used. A contrast agent stains the bile ducts, making them more visible and clear.
Cholecystitis
Inflammatory process in the gallbladder. It can be either acute or chronic. It is often hereditary.
Polyps
Neoplasms on the walls of the gallbladder. The disease is rare compared to others. If the polyps do not cause discomfort to the patient and do not lead to bladder dysfunction, they are not removed.
Dyskinesia
Impaired contractility of the bile ducts. Accompanied by stagnation or excess bile with corresponding symptoms.