Pregnancy-associated plasma protein-A (PAPP-A) is one of the largest associated enzymes produced by the embryo and placenta (syncytiocytotrophoblasts).
This protein is thought to have several different functions, including preventing fetal recognition by the maternal immune system, matrix mineralization, and angiogenesis. PAPP-A levels increase depending on the week of pregnancy when tested and analyzed in the 1st trimester, which is considered normal.
What is PAPP-A?
Plasma protein associated with pregnancy is what this abbreviation stands for. It plays a key role in complex biochemical processes that affect the growth and development of the fetus, placenta, and the development of immunity. The longer the period, the higher its level in the mother’s blood. A decrease in PAPP-A levels during pregnancy may indicate that the baby is at risk of developing Edwards or Down syndrome. This fact cannot but alarm and worry parents.
However, you should not rely only on the results of a blood test. Before making such a diagnosis, it is necessary to comprehensively evaluate other parameters that are obtained from ultrasound results. The optimal time to evaluate PAPP-A during pregnancy is 11-13 weeks, the first screening occurs at 10-14 weeks. This period was not chosen by chance. It is believed that at this time it is possible to obtain the most accurate information regarding the health status of the mother and fetus. After the 14th week, the results obtained, even if there are abnormalities in the child, will be the same as in a healthy one.
What does the analysis determine?
Studies conducted during biochemical screening are aimed at determining the likelihood of developing chromosomal pathologies in the fetus.
At the end of the first trimester of pregnancy, you can already find out the risk of such diseases as:
- Down syndrome;
- Anencephaly;
- Edwards syndrome;
- Spinal canal cleft.
Down syndrome or trisomy 21 pairs of chromosomes is a fairly common disease in the modern world. Thus, we get not two, but three chromosomes.
Children with this diagnosis have a characteristic appearance. With broad features, slanted eyes and a fairly short nose.
The disease is accompanied by mental retardation, cerebral palsy and other multiple pathologies of the development of internal organs.
Anencephaly or absence of a brain. This pathology can be determined by ultrasound. Such children are not viable.
As in the case of Down syndrome, an extra chromosome appears in the 18th pair.
This disease is accompanied by a large number of concomitant pathologies. Unfortunately, these babies usually do not survive birth.
Spinal bifida, or spina bifida, is a neural tube disorder that affects the spinal cord.
After birth, babies will not be able to fully move and will most likely be paralyzed.
If this pathology has accompanying deviations of internal organs, then the child is not viable.
Factors influencing the level
An experienced specialist should take into account that the following factors influence the level of PAPP-A during pregnancy:
- Method of conceiving a child.
- The presence of gestosis in a previous pregnancy and the weight of the newborn.
- Weight, height, presence of bad habits (in particular smoking).
- Having diabetes.
If a woman has at least one of the factors described above, then, most likely, in the first trimester the content of PAPP-A during pregnancy at 12 weeks will be low. In the second and third trimester, on the contrary, its level may increase. This is worth considering before paying attention to a specialist’s opinion.
Why low hCG on screening: reasons
Low hCG on screening , reasons:
- A pregnancy that develops outside the uterus, that is, in the fallopian tube
- The presence of pathology in the fetus. Indeed, with some chromosomal disorders, the concentration of hCG in the blood changes, and its norm significantly decreases from the permissible level.
- Diabetes. With this disease, hormonal abnormalities are possible.
- Taking certain medications or hormonal drugs.
In this case, an increase in hCG can also be quite informative. Usually it indicates a multiple pregnancy, an incorrect gestational age, as well as the presence of certain ailments, and hydatidiform mole.
Reasons for appointment
For each test during pregnancy there is a specific purpose or indication. Studies that should indicate the risk of developing a disorder (genetic or hereditary) are carried out during the next screening. At the end of the first trimester, a woman needs to undergo a series of tests. Along with the usual ones, such as a general blood test and urine test, PAPP and hCG are also included. During pregnancy, these indicators indicate a possible risk of having a child with Down syndrome. However, you should not rely only on blood results alone and get upset ahead of time if they differ from the norm.
Parents can undergo this test on their own, for example, if the pregnant woman is not registered or does not attend an antenatal clinic. This way they can make sure their baby is healthy or if there is a risk they should be aware of in advance.
Risk group
There is a certain risk group, which is conditionally such, according to medical practice, which includes women:
- Over 35 years of age and pregnant minors.
- Who had previously been diagnosed with a threatened miscarriage, regressing or frozen pregnancy.
- Drug or alcohol abusers.
- Having had an infectious disease or taking illicit, potent drugs at the beginning of pregnancy.
- Those living in unfavorable environmental conditions or working in hazardous industries.
- Having genetic or hereditary diseases in the family.
Do not forget that even if a pregnant woman is not at risk, there is still a possibility of having a child with genetic disorders.
PAPP-A and hCG. Necessary tests
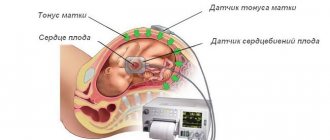
Along with the PAPP-A analysis during pregnancy, the level of AFP (alpha-fetoprotein), b-hCG and the content of free estradiol in the blood serum are necessarily measured. Additionally, ultrasound evaluates parameters such as:
- Coccygeal-parietal size (CTP).
- The thickness of the collar space (collar zone, or there is also such a term as the width of the neck fold).
- The presence or absence of a nasal bone.
If PAPP-A is normal during pregnancy at 12 weeks, then other indicators should not lag behind or exceed the established limits. From the first days of conception, special attention is paid to the level of hCG (human chorionic gonadotropin). It indicates existing defects in the development of the fetus and the nature of the pregnancy.
What do changes in protein levels indicate?
Deviations both upward and downward from the norm in hCG and PAPP-A levels indicate a risk of developmental abnormalities in the child.
A decrease in the amount of PAPP-A in a woman’s blood, together with an increase in hCG levels, signals a risk of Down syndrome.
Elevated hCG levels can occur in the presence of diabetes, multiple pregnancy, or severe toxicosis.
A low level may also indicate existing problems.
A decrease in the concentration of this protein is observed when:
- ectopic pregnancy;
- development of Edwards syndrome;
- threat of premature termination of pregnancy;
- placental insufficiency.
The reliability of deciphering the results of this test does not exceed 70%. Therefore, in addition to a blood test, it is necessary to undergo an ultrasound examination. It will help determine the diagnosis more accurately.
There are variants of false negative results. In this case, most likely, the diseases will be detected at the 2nd perinatal screening at 18-20 weeks.
Preparing for analysis
The blood level of PAPP-A during pregnancy is determined by taking a blood serum sample for analysis. Before taking biomaterial, a woman should prepare. It is worth refraining from eating 6 hours before the test; fatty and spicy foods are excluded from the diet. In the morning, you can drink clean water, no more than 100 ml, so that taking blood from a vein does not cause difficulties. Blood sampling should be done in the morning. It is advisable to be in a state of physical rest. For example, rest before donating blood, sit at the office for a few minutes.
You should also weigh yourself in advance and measure your height, as these indicators influence the interpretation of the results. It is recommended that all screening tests be carried out in one clinic or laboratory. This is due to the fact that the interpretation of data in each laboratory and the established standards are different.
Pregnancy - Prenatal screening for trisomy of the first trimester of pregnancy (Down syndrome), PRISCA
A non-invasive test that, based on certain laboratory markers and clinical data, allows a computer program to calculate the likely risk of developing chromosomal diseases or other congenital abnormalities of the fetus.
Due to limitations in the use of calculation methods for determining the risk of congenital fetal anomalies, it is impossible to calculate such risks in multiple pregnancies with 3 or more fetuses.
Synonyms Russian
Biochemical screening of the 1st trimester of pregnancy, “double test” of the 1st trimester.
English synonyms
Maternal Screen, First Trimester; Prenatal Screening I; PRISCA I (Prenatal Risk Calculation).
Research method
Solid-phase chemiluminescent enzyme-linked immunosorbent assay ("sandwich" method), chemiluminescent immunoassay.
Units
MME/ml (milli- international unit per milliliter), IU/L (international unit per liter).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Eliminate fatty foods from your diet 24 hours before the test.
- Avoid physical and emotional stress for 30 minutes before the test.
- Do not smoke for 30 minutes before the test.
General information about the study
Down's disease is a chromosomal disease associated with a disorder of cell division (meiosis) during the maturation of sperm and eggs, which leads to the formation of an additional 21st chromosome. The frequency in the population is 1 case in 600-800 births. The risk of chromosomal abnormality increases with the age of the mother and does not depend on the health status of the child’s mother or environmental factors. Edwards syndrome (trisomy 18) and Patau syndrome (trisomy 13) are less associated with maternal age, with a population incidence of 1 in 7000 births. Accurate prenatal diagnosis of genetic diseases requires invasive procedures that are associated with a high likelihood of complications, so mass screening uses safe research methods to identify low or high risk of chromosomal abnormalities and assess the feasibility of further examination.
Prenatal screening for trisomy in the first trimester of pregnancy is performed to determine the likely risk of chromosomal pathology of the fetus - trisomy 21 (Down syndrome), as well as trisomy 18 (Edwards syndrome) and trisomy 13 (Patau syndrome) between the 10th week and 13th week and 6 days of pregnancy. It is calculated using the PRISCA (Prenatal Risk Calculation) computer program developed by Typolog Software (Germany) and having an international certificate of conformity. For the study, the content of the free beta subunit of human chorionic gonadotropin (hCG) and pregnancy-associated plasma protein A (PAPP-A) in the blood of a pregnant woman is determined.
The PAPP-A enzyme ensures the full growth and development of the placenta. Its content in the blood increases as pregnancy progresses. The level of PAPP-A does not significantly depend on parameters such as the sex and weight of the child. In the presence of a chromosomal abnormality with fetal malformations, its concentration in the blood decreases significantly from the 8th to the 14th week of pregnancy. It decreases most sharply with trisomies on the 21st, 18th and 13th chromosomes. In Down syndrome, the PAPP-A level is an order of magnitude lower than in normal pregnancy. An even more dramatic decrease in the concentration of PAPP-A in the mother’s blood serum is observed when the fetus has a genetic pathology with multiple malformations – Cornelia de Lange syndrome. However, after 14 weeks of pregnancy, the value of determining PAPP-A as a risk marker for chromosomal abnormalities is lost, since its level is then normal even in the presence of pathology.
For screening, clinical data (pregnant woman’s age, body weight, number of fetuses, presence and characteristics of IVF, mother’s race, bad habits, presence of diabetes mellitus, medications taken), ultrasound data (coccygeal-parietal size (CPR) and nuchal translucency thickness) must be taken into account (TVP), nasal bone length). If ultrasound data is available, the gestational age is calculated based on the CTE value, and not on the date of the last menstruation.
After the study and risk calculation, a scheduled consultation with an obstetrician-gynecologist is carried out.
The results of a screening study cannot serve as criteria for making a diagnosis or as a reason for artificial termination of pregnancy. Based on them, a decision is made on the advisability of prescribing invasive methods of examining the fetus. If the risk is high, additional examinations are necessary, including chorionic villus puncture, amniocentesis with genetic testing of the material obtained.
What is the research used for?
- For screening examination of pregnant women to assess the risk of chromosomal pathology of the fetus - trisomy 21 (Down syndrome), Edwards syndrome.
When is the study scheduled?
- When examining pregnant women in the first trimester (analysis is recommended for pregnancy 10 weeks - 13 weeks 6 days), especially in the presence of risk factors for the development of pathology: age over 35 years;
- history of miscarriage and severe pregnancy complications;
- chromosomal pathologies, Down's disease or congenital malformations in previous pregnancies;
- hereditary diseases in the family;
- past infections, radiation exposure, taking medications that have a teratogenic effect in the early stages of pregnancy or shortly before it.
What do the results mean?
Reference values
- Pregnancy-associated plasma protein A (PAPP-A)
| Week of pregnancy | Reference values |
| 8-9th | 0.17 - 1.54 MME/ml |
| 9-10th | 0.32 - 2.42 MME/ml |
| 10-11th | 0.46 - 3.73 MME/ml |
| 11-12th | 0.79 - 4.76 MME/ml |
| 12-13th | 1.03 - 6.01 MME/ml |
| 13-14th | 1.47 - 8.54 MME/ml |
- Free beta subunit of human chorionic gonadotropin (beta-hCG free)
| Week of pregnancy | Reference values |
| 8-9th | 23.65 - 162.5 ng/ml |
| 9-10th | 23.58 - 193.13 ng/ml |
| 11-12th | 17.4 - 130.38 ng/ml |
| 12-13th | 13.43 - 128.5 ng/ml |
| 13-14th | 14.21 - 114.7 ng/ml |
| 14-15th | 8.91 - 79.44 ng/ml |
| 15-16th | 5.78 - 62.07 ng/ml |
| 16-17th | 4.67 - 50.05 ng/ml |
| 17-18th | 3.33 - 42.81 ng/ml |
| 18-19th | 3.84 - 33.3 ng/ml |
Based on the examination of the pregnant woman, the PRISCA program calculates the likelihood of developmental defects. For example, a ratio of 1:400 shows that, according to statistics, one out of 400 pregnant women with similar indicator values gives birth to a child with a corresponding malformation.
What can influence the result?
- The result is influenced by the accuracy of the information provided and the ultrasound diagnostic findings.
- A false positive result (high risk) in some cases may be associated with an increase in the beta subunit of human chorionic gonadotropin due to placental dysfunction and the threat of miscarriage.
Important Notes
- The laboratory must have accurate data on the gestational age and all factors necessary to calculate the indicators. Incomplete or inaccurate data provided may cause serious errors in risk calculations. The use of invasive diagnostic methods (chorionic villus biopsy, amniocentesis, cordocentesis) is not recommended if screening tests are normal and there are no changes on ultrasound.
- The results of prenatal screening, even with a high calculated risk, cannot serve as a basis for artificial termination of pregnancy.
Also recommended
- Pregnancy – 1st trimester
- Beta subunit of human chorionic gonadotropin (beta-hCG)
- Pregnancy-associated plasma protein A (PAPP-A)
- Alpha fetoprotein (alpha FP)
- Free estriol
- Placental lactogen
- Progesterone
- Cytological examination of hormonal levels (if there is a threat of miscarriage, cycle disorders)
Who orders the study?
Obstetrician-gynecologist, medical geneticist.
Literature
- Durkovic J., Andelic L., Mandic B., Lazar D. False Positive Values of Biomarkers of Prenatal Screening on Chromosomopathy as Indicators of a Risky Pregnancy. // Journal of Medical Biochemistry. – Volume 30, Issue 2, Pages 126–130.
- Muller F., Aegerter P., et al. Software for Prenatal Down Syndrome Risk Calculation: A Comparative Study of Six Software Packages. // Clinical Chemistry – August 1999 vol. 45 no. 8 – 1278-1280.
Decoding the testimony
When receiving the results, the woman tries to independently determine how much her numbers correspond to the PAPP-A norm during pregnancy. Each laboratory has its own equipment. In order for the doctor to determine whether the results obtained are within the time limit, it is necessary to find out in advance whether the laboratory can transfer them to the MoM. This is a special coefficient that eliminates errors in deciphering the results.
When assessing results, doctors usually pay attention to the cutoff values. Data obtained from a woman’s survey to identify factors that may influence deviation from the norm in one direction or another are also taken into account. The limit value for pregnancy-associated plasma protein-A (high molecular weight glycoprotein) is 0.5 to 2 MoM. In multiple pregnancies, the upper value can reach 3.5 MoM. This indicator is general for all laboratories and clinics. If the institution where the pregnant woman takes the test for prenatal screening immediately provides the results to the MoM, then it will be easier for the doctor to determine whether there are abnormalities or not.
How often should blood tests be done for adults and children?
There is no need for a general laboratory blood test, which reflects the main common abnormalities in the human body; it can be taken to check your health once every six months. A serious reason for going to the laboratory to check your blood is constant fatigue and drowsiness, frequent illnesses, rashes, and pregnancy. Women who are carrying a child should take special responsibility for carrying out blood tests, because the indicators obtained during the examination can diagnose serious pathologies of fetal development. Pregnant women should have a blood test every trimester.
Every year you should take a blood test for tumor markers; it is better to detect a malignant neoplasm at an early stage, when the tumor has not had time to harm all organ systems.
The doctor may also prescribe other blood tests for the patient if he is at risk for a particular disease.
Risk in decoding results
Some laboratories, in addition to numbers, also provide a comment regarding whether the test result is positive or not. If the result says “test positive,” it means the baby is at high risk of being born with Down syndrome. In order to make sure of this, parents may be asked to undergo a specific study. They involve the need to take a sample of amniotic fluid, umbilical cord blood or fetal chorionic villus sampling. Undoubtedly, such tests can harm the baby or lead to the threat of termination of pregnancy. However, doctors assure that modern technology can reduce this risk to a minimum.
A “negative” test, on the contrary, can reassure parents, since the risk of having a child with genetic abnormalities is minimal. During the second screening, the results obtained are compared with the first. This serves as a basis for canceling worries if deviations from the norm were identified at the first screening.
Normal during pregnancy by week
Since the expectant mother undergoes the first serious examination after the 10th week of pregnancy, it will be important to know what numbers will be considered normal at this stage. At the 10-11th week, the content of protein associated with pregnancy is within the normal range from 0.46 to 3.73 mU/l. It is this result that indicates that the fetus is not in danger. If we talk about the norm of PAPP-A during pregnancy, then at 11-13 weeks the numbers should be in the range of 0.79 - 6.01 mU/l, and at 13-14 weeks - already 1.47-8.54 honey/l.
Deviations may indicate not only pathologies associated with the genetics of the fetus, but also the risks of premature termination of pregnancy. This may be a threat of miscarriage or intrauterine fetal death. To eliminate the unreliability of the data obtained, it is recommended to conduct the study within a strictly established time period. That is why the first screening at this stage also includes an ultrasound examination, which helps determine the exact stage of pregnancy.
β-hCG – human chorionic gonadotropin
This hormone is produced by the chorion (“shell” of the fetus), thanks to this hormone it is possible to determine the presence of pregnancy in the early stages. The level of β-hCG gradually increases in the first months of pregnancy, its maximum level is observed at 11-12 weeks of pregnancy. Then the level of β-hCG gradually decreases, remaining unchanged throughout the second half of pregnancy.
| Normal levels of human chorionic gonadotropin, depending on the stage of pregnancy: | An increase in β-hCG levels is observed in the following cases: | A decrease in β-hCG levels is observed in the following cases: | |
| weeks | β-hCG, ng/ml |
|
|
| 10 | 25,80-181,60 | ||
| 11 | 17,4-130,3 | ||
| 12 | 13,4-128,5 | ||
| 13 | 14,2-114,8 | ||
Exceeding the norm: what to do?
If a pregnant woman has an increased protein associated with pregnancy, PAPP-A, and other indicators are normal, then it is necessary to find out how the woman feels during the entire first trimester. If you have severe toxicosis or diabetes, there is a risk of exceeding the indicators. Also, PAPP-A levels may be elevated during multiple pregnancies. Therefore, you should not immediately assume that the child will have genetic abnormalities.
It is important to understand that a deviation from the norm PAPP-A during pregnancy at 13 weeks can be caused by external factors that must be taken into account when taking the test. This could be stress, the mother being overweight, or conceiving a child using in vitro fertilization. To confirm or refute the diagnosis, repeated donation of blood serum may be required for testing. Alternative invasive methods may also be used. The advisability of their use can only be judged by a geneticist who studies all the data obtained as a result of screening.
Advantages and disadvantages of the method
Over the past 10 years, various screening and diagnostic tests have been developed to detect Down syndrome, and the use of combined ultrasound and serum markers has been evaluated.
Some doctors only offer these tests to women of a certain age, and the practice is controversial. ACOG has developed guidelines that evaluate the use of ultrasonography and serum markers for selective screening of aneuploidy in pregnant women.
Research has shown that in the 1st trimester there is an association between the size of the fluid collection at the back of the fetal neck (nuchal translucency) and the risk of trisomy 21.
Extensive assays have revealed that nuchal translucency can be combined with free beta-hCG and pregnancy-associated plasma protein A (PAPP-A) to screen for Down syndrome. PAPP-A and hCG measurements are effective for screening only in the 1st trimester, and alpha-fetoprotein, unconjugated estriol, and inhibin should only be performed in the 2nd trimester.
If PAPP-A is lowered, should you panic?
If the results are below normal, PAPP-A cannot be increased in any way during pregnancy at the 12th week. They may not be informative if the analysis did not take into account important parameters. For example, your weight and height were incorrectly indicated. When the level of pregnancy-associated protein is significantly reduced, this may indicate a possible genetic disorder. In particular, we are talking about:
- Trisomy 13 (Patau syndrome, the presence of the 13th chromosome).
- Trisomy 18 (Edwards syndrome, in which the fetus has abnormalities that are incompatible with life).
- Trisomy 21 (Down syndrome, in which the fetus is genetically endowed with 47 rather than 46 chromosomes; the extra chromosome can be passed on from both the father and mother).
- Monosomy on the X chromosome, triploidy (threatens short stature, mental retardation, infantilism in the fetus at birth).
If the functioning of the placenta is impaired, or there is a threat of miscarriage, a decrease in PAPP-A during pregnancy at the 13th week is a signal for taking urgent measures. Only after consultation with a geneticist can we talk about the advisability of performing a chorionic villus biopsy or amniocentesis.
When are plasma proteins A detected in a woman’s body?
PAPP-A during pregnancy, the norm at 8-12 weeks of which practically does not differ from the data in the 2nd trimester, can be estimated only approximately (with the exception of fibrinogen, when testing is carried out on condensed samples):
- With a typical reference range of 60–80 g/L, 1 plasma protein makes up about 7% of plasma by weight 2 and 0.5% of total body weight.
- Serum albumin makes up about 55% of plasma protein (typical reference range: 35–55 g/L), about 3.4. It maintains plasma osmotic pressure and is involved in the transport of calcium, lipids and steroid hormones.
- Globulins make up approximately 35% of plasma protein (typical reference range: 20–35 g/L) – 5.6 values. Globulins are involved in a number of processes, including the transport of ions, hormones and lipids, and acute phase reactions.
Globulins are divided into 4 subgroups:
- 2 alpha-1 (mainly alpha-1 antitrypsin);
- alpha 2 (including haptoglobin and ceruloplasmin);
- beta (contains transferrin and some complement components);
- gamma (includes mainly immunoglobulins and C-reactive protein).
Fibrinogen is a soluble protein that makes up about 6.5% of plasma protein. The conversion of fibrinogen to insoluble fibrin is a process that is critical for blood clotting.
The remaining plasma proteins contain hundreds of different protein molecules. Individually they are present in small quantities, but together they constitute approximately 1% of plasma protein and play important roles as regulatory proteins such as enzymes, proenzymes and hormones.
Plasma proteins are heterogeneous in nature and are involved in many complex body functions.
Abnormalities in plasma proteins can be:
- primary (cause of specific pathologies);
- secondary (the result of a wide range of disease processes).
Abnormal proteinuria can also result from various medical conditions.
Reasons why a gynecologist may perform plasma protein measurements include studies of symptoms, allergies, and immunity:
- Investigation of a specific symptom such as peripheral edema, diagnosis of an inflammatory process or autoimmune disorder: for example, testing of antinuclear antibodies in the evaluation of systemic lupus erythematosus.
- Diagnosis of bone marrow disorders, including multiple myeloma: assessment of allergies, testing for immunodeficiency in patients with recurrent infections, assessment of immunity to infections such as hepatitis B or rubella.
Specific antibody tests test for total immunoglobulin A (IgA) and tissue transglutaminase IgA antibodies.
Assessment of pregnancy-associated plasma protein A (PAPP-A) together with human chorionic gonadotropin (hCG) measurement and ultrasound are suggested for analysis in early pregnancy (10–14 weeks) when the fetus may be at risk for chromosomal abnormalities: Down syndrome (trisomy 21) or Edwards syndrome (trisomy 18).
A urine protein test is performed to diagnose urinary infection, primary kidney disease, including nephrotic syndrome, and secondary kidney disease.
Doctor's decisions
A competent obstetrician-gynecologist will not take responsibility for asserting that a deviation from the norm is a clear indication for termination of pregnancy. Even if the risk of having a child with a genetic disorder is very high, it is necessary to check this conclusion. The PAPP-A indicator alone cannot be a prerequisite for making a diagnosis.
There is a lot of evidence online that screening results with obvious deviations were erroneous and were not confirmed upon re-analysis. Moreover, no one can determine how a baby will be born with 100% probability. Experts can only prepare parents for the possibility that a special child will appear in their family. Moreover, if according to the ultrasound results the fetus is developing normally, and all parameters correspond to the gestational age, there are no neural tube defects, there should be no cause for concern.
Errors in results
During prenatal diagnostics, some indicators remain conditional. In particular, the level of PAPP-A may turn out to be unreliable in 5% of cases. Most often false positive, in only 2-4% of cases the diagnosis was confirmed, and a decision was required on which the fate of the unborn child depended. It is also worth understanding that some pathologies may not have any effect on the PAPP-A standards. It can be ideal, while the child is subsequently diagnosed with some kind of syndrome.
Pathologies with an extra chromosome
Of greatest interest at the 13th week of diagnosis are pathologies such as trisomies 13, 18 and 21. The numbers indicate a chromosome pair with an anomaly, namely the appearance of an extra chromosome of chromosome 47.
Naturally, this greatly affects the child’s appearance and his mental and physical development.
What are the features of these pathologies?