Almost every woman knows that breast health needs to be monitored especially carefully. The greatest attention should be paid to the breast in the postpartum period, at the onset of menopause, and also in case of an unfavorable prognosis for oncology. In addition to palpation and visual examination, as well as a number of tests, the doctor may prescribe you a type of examination such as mammography - this diagnosis is done using an X-ray, ultrasound or MR machine.
Indications and contraindications
Indications for prescribing breast x-rays for women:
- detection of lumps in the breast area during palpation (when visiting a gynecologist or on your own);
- complaints about changes in the shape of the glands - local protrusion, an increase in the size of one breast or both;
- the appearance of pain, inflammation, swelling, increased local temperature (the glands are hot to the touch);
- enlarged axillary and subclavian lymph nodes;
- discharge from the milk ducts;
- preoperative preparation;
- monitoring the effectiveness of the treatment course;
- screening examination (preventive).
Routine mammography is indicated for patients with the following conditions:
- excess body weight;
- infertility;
- previously diagnosed tumor – benign or malignant;
- local inflammatory process (for example, mastitis);
- undergone breast surgery.
Absolute contraindications are pregnancy and lactation, since mammography is a study in which the patient is exposed to ionizing radiation. And it has a detrimental effect on the fetus and changes the composition of breast milk.
The study is not recommended for women under 35-40 years of age. The tissue of the glands at a young age is still dense, which makes it difficult to assess its condition and does not allow differentiating pathological areas of the organ from normal structures. For young patients, X-rays are replaced by ultrasound. This method is more informative at their age.
Relative (temporary) contraindications - violation of the integrity of the skin in the chest area, burns, hematomas, infectious skin diseases. Mammograms are not performed on patients with breast implants. It is not recommended to undergo testing within six months after termination of pregnancy (this rule can be neglected if the expected diagnostic benefit is more significant than the potential harm).
Why do a mammogram
Regular mammography allows you to evaluate the dynamics of already identified diseases, timely diagnose and clarify the clinical picture of various pathological changes and neoplasms, including:
- calcifications (with an assessment of the size, nature, localization to determine the causes of the pathology),
- fibroadenomas (benign tumors), cysts, abnormal seals in the ducts of the mammary glands,
- all types of cancer (including tumors up to 5 mm in size), which is especially important when the first stages of oncology are asymptomatic.
Types of X-ray
X-ray mammography – viewing the structure of the breast using x-rays. For preventive purposes, it is performed for women after 40 years of age every 2 years, after 50 years of age - every year. Patients under 50 years of age, but at risk (primarily those whose close relatives have been diagnosed with carcinoma or sarcoma), are examined more often. Diagnostics is indicated for suspected tumors and other diseases. Information content is 90-95%. After additional tissue examination, false-positive results are detected in 25% of patients.
What does the methodology determine:
- infiltration (compaction) of different sizes and localization;
- calcifications – calcium deposits in the ducts and tissues of the gland;
- cystic formations;
- degree of patency of the milk ducts;
- detailed visualization of neoplasms.
Film X-ray mammography is a traditional diagnostic method. After Ro-rays pass through the breast tissue, an image is formed on film. This is the most accessible, cheapest, but also the least informative option, since the study is carried out on old-style devices. In addition, the radiation dose when performing classical mammography will be the highest compared to more advanced analogues.
Digital mammography is an examination performed on modern equipment using X-rays with minimal radiation exposure. The radiation dose is four times less than with traditional mammography. All information is transmitted in digital format, and not in black and white. It is possible to increase, detail, change the contrast, and clarity of the resulting image in 3D format. The doctor has the opportunity to work with images in electronic form; as a rule, there is no need for repeated examination.
Mammography with tomosynthesis is the use of X-rays to obtain a tomogram (layered sections with a three-dimensional image). The efficiency is close to 100%. Thanks to innovative automated equipment, diagnostics are painless and comfortable for the woman. Prescribed only if pathology is suspected; tomosynthesis is not performed as screening.
There are other types of mammography. They are not radiological, but are also informative.
Electrical impedance mammography is a technique based on the resistance of gland tissue to electrical impulses. The examination area is exposed to alternating current for half a minute. Healthy and altered tissues react to current differently, which determines the principle of obtaining a picture. The sensor displays the image on the monitor in real time. A complete breast examination takes 10-15 minutes. The technique is harmless for pregnant women and nursing mothers. It is recommended for young girls with symptoms of mastopathy.
MRI (magnetic resonance mammography) is a harmless way to diagnose breast diseases, based on the interaction of a magnetic field with biological fluids of the body. The examination does not use ionizing or radioactive radiation, so the method is absolutely safe. MRI is prescribed when mammography is insufficiently informative for the purpose of differential diagnosis.
Breast cancer treatment
The treatment strategy for breast cancer should be selected individually for each patient, taking into account factors such as tumor type, stage, and sensitivity of the tumor to hormonal therapy. The general condition of the patient is also taken into account. If the tumor is detected in the early stages and the correct patient management tactics are chosen, then the chance of completely curing breast cancer is very high.
Surgical method
The surgical method is the dominant one in the treatment of breast cancer. If the tumor is detected early, it is possible to perform an organ-preserving operation—sectoral resection. Performing such an intervention is accompanied by an increased risk of local recurrence, and therefore it is combined with other methods, for example, radiation therapy.
In later stages, breast cancer is treated with a mastectomy—removal of the entire breast along with nearby lymph nodes. The doctor may also decide to remove the second breast if there is a high risk of developing a malignant tumor in it.
A sentinel biopsy, or sentinel lymph node biopsy, may be performed to determine whether cancer cells have spread to the lymph nodes and to determine the extent of surgery . During surgery, a radiopharmaceutical or fluorescent dye is injected into the tumor to help visualize the lymph node that first receives lymph from the breast tissue. It is removed and histological examination is performed. If no tumor cells are found in the sentinel lymph node, you can limit yourself to removing the lesion in the mammary gland. Otherwise, excision of regional lymph nodes is indicated.
Radiation therapy
In order to improve the immediate and long-term results of surgery for breast cancer, radiation therapy is used as an auxiliary method. It can be used in the preoperative period to reduce the degree of malignancy of the tumor, damage and regression of micrometastases. However, more often radiation therapy is used after surgery, when it is necessary to destroy cancer cells that may have remained in the body.
Chemotherapy
To treat breast cancer, chemotherapy is used before or after surgery in order to completely cure the patient, to prolong life and improve its quality, or to reduce the volume of surgery. Each chemotherapy drug only affects cells in a specific phase of the cell cycle. Therefore, the most effective prescription is polychemotherapy - a combination of several drugs that have different effectiveness and mechanism of action.
The European Clinic uses the most modern, original European and American chemotherapy drugs for the treatment of breast cancer. We have the opportunity to create a “molecular fingerprint” of the tumor and, based on its analysis, select the most effective and safe combinations of drugs.
Drug therapy: hormonal and targeted drugs
A malignant breast tumor is recognized as hormone-sensitive if more than 10% of the cells in its composition have receptors for estrogen or progesterone. In this case, breast cancer should be treated using hormonal therapy. The more the tumor has hormonal receptors, the more effective such treatment will be.
This type of therapy includes several methods that stop the production of hormones and block their flow to the tumor. Today, drugs from the group of non-steroidal antihormones are increasingly used, which act only on the tumor and do not affect the mechanisms of hormone formation throughout the body. Therapy with hormonal drugs is prescribed both in the postoperative period to reduce the risk of recurrence, and as an independent treatment for inoperable breast tumors to control their growth.
Targeted therapy is also used to treat breast cancer—drugs that target specific target molecules in tumor cells and have minimal effects on healthy cells in the body. Targeted therapy is used either alone or in combination with other treatments.
Preparation and carrying out the procedure
X-rays do not require special preparation, diet, or medication. Points to consider:
- inform the gynecologist (radiologist) about the date of the last menstruation;
- before going to the clinic, do not apply deodorizing agents to the armpits;
- wear clothes that can be easily removed to quickly expose your torso to the waist;
- Before the examination itself, remove your watches and jewelry (chains, earrings, bracelets).
Diagnostics are carried out in an office with X-ray protection of walls, windows, floors, ceilings, and entrance doors. The room is equipped with an X-ray machine (stationary, mobile), and a digital radiovisiograph.
When is the best time to conduct research?
The most suitable time to obtain an accurate, informative result is from the 7th to the 12th day after the start of the menstrual cycle.
Before menstruation, most women's breasts swell slightly under the influence of the hormone (progesterone), which is normal. The condition is associated with increased blood circulation in the organ, accompanied by a feeling of fullness and pain when touched. This is a period of structural transformations in breast tissue. Therefore, it is not recommended to carry out diagnostics on the eve of menstruation.
When is the best time to conduct research?
As for the choice of time for conducting the examination, experts most often recommend scheduling it from the 5th to the 12th day of the menstrual cycle, because it is at this time that it is possible to achieve highly informative images. It is also noted that during this period of time the mammary glands are in a calm and unenlarged state. As for conducting the examination at other times, this is possible in critical situations, for example, when there is a threat to life or health, and on the initiative of a specialist.
How is the examination done?
The algorithm for conducting the survey is as follows.
- The procedure takes place in a sitting or standing position.
- The areas of the large and small pelvis are covered with a protective apron.
- The mammary gland is placed on a special platform, under which there is an emitter, and the breast is pressed on top with a plate. Thus, the examined area of the organ will increase.
- The image is displayed on x-ray film in several projections (as prescribed by the doctor).
- An x-ray of two glands takes on average 15-20 minutes. The conclusion is issued immediately after diagnosis.
Pictures are usually taken in several projections. The radiologist will help the patient take the correct position.
It is important to remain still while taking pictures, otherwise the picture will turn out blurry.
Is it harmful
The radiation dose for mammography is 0.4 mSv. To understand how big this value is, let’s compare it with other types of x-rays. During an extensive examination of the chest and lungs, a radiation dose of up to 0.8 mSv is administered. Residents of megacities annually receive radiation exposure from the atmosphere equal to 4 mSv. The dose leading to the death of body cells is 150 mSv.
How is mammography performed?
Before the examination in a specially equipped room, you must remove clothing and jewelry above the waist.
Next, the specialist will tell you how to position the breast between two mammograph plates, which will slightly compress it during the procedure (to increase image sharpness and reduce radiation exposure). The procedure lasts several minutes. If necessary, several targeted photographs are taken, which also does not take much time.
Mammography is performed for each breast separately, which is especially important for comparing the glands for the development of pathologies.
How is the image description protocol formulated?
The research protocol is carried out according to one of three options.
- The mammogram did not reveal any structural changes in the tissue.
- Most of the glandular tissue is without pathological changes. Minor destructive areas were identified. Recommendation: repeat x-ray in six months.
- The image revealed diffuse tissue changes and pockets of calcium accumulation (calcifications). Recommendation: biopsy to identify the pathological process.
If the image shows no signs of malignancy, it cannot be completely excluded. According to the findings of practicing oncologists, the tumor is clearly visible when it reaches a size of 1-1.5 cm.
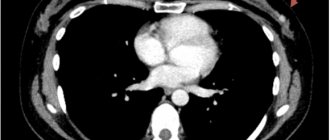
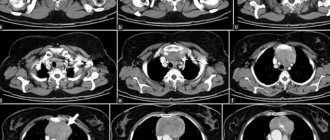
What does the radiologist see in the images?
In mastopathy with fibrous growths, heavy shadows are visible in the photo. The glandular tissue is enlarged, and isolated cysts are present.
Calcifications are detected during milk stagnation in lactating women. This is also a sign of the presence of a tumor. Therefore, an additional biopsy is performed, even if the image shows no signs of a neoplasm.
Fat involution is observed in women during menopause. On the mammogram there are no clear divisions between the structures of the gland. This is due to the replacement of glandular tissue with adipose tissue.
Signs of a benign tumor
A benign breast tumor is suspected based on the following signs:
- darkening in the image has a regular round shape;
- the boundaries of the tumor are clear;
- there is no reaction from surrounding tissues;
- in dynamics, non-infiltrative growth is observed (it moves apart healthy tissues, and does not penetrate them).
Signs of a malignant tumor
How to recognize breast cancer in mammography images:
- the shape of the tumor is irregular, asymmetrical;
- the edges are torn, the contours are blurred, the structure is heavy;
- a path stretches from the formation to the nipple;
- the presence of small calcifications in the milk ducts;
- there is no clear rim in the form of darkening around the tumor;
- increased proliferation of blood vessels;
- replacement of healthy connective tissue;
- thickening of the dermis in the area of the tumor;
- bulging or recessed nipple.
Symptoms of breast cancer
In the early stages, breast cancer usually does not manifest itself clinically. Most often, the tumor is discovered by the patients themselves or is detected accidentally during preventive studies.
Patients usually complain of the presence of a palpable formation and discharge from the nipple. Pain is a rare symptom of breast cancer, but the pain syndrome can come to the fore at the stage of generalization of the process, especially when metastases spread to the bones.
Quite often, signs of breast cancer are detected, such as the appearance of asymmetry due to changes in the size of the affected gland. Reduction, upward displacement, deformation and wrinkling of the mammary gland can be observed in the scirrhosis (fibrous) form of the tumor. On the contrary, the breast on the affected side becomes enlarged due to the rapid growth of the formation or due to edema, which forms due to impaired lymph outflow.
When the tumor spreads into the subcutaneous tissue, skin changes may be observed. The following symptoms of breast cancer are identified:
- “Platform” - the skin above the tumor becomes flattened; it is impossible to form a skin fold in this area.
- “Umbilization” - the skin over the lesion is wrinkled and retracted.
- “Lemon peel” is a characteristic appearance of the mammary gland due to lymphostasis.
Sometimes, when the tumor spreads to the surface of the skin, signs of breast cancer such as redness and ulceration may be observed. The presence of these symptoms indicates that the process is neglected.
Changes in the nipple can also be detected, but only in the later stages. In this case, the following symptoms of breast cancer occur:
- Forga's sign - on the affected side the nipple is higher than on the healthy side.
- Krause's sign - the nipple is thickened, the folds of the areola are noticeably pronounced.
Such a sign of breast cancer as pathological discharge is quite rare, but in some cases it may be the only symptom that is detected during examination. The discharge is often bloody in nature, serous and purulent are less common.
Depending on the manifestations of the disease, different clinical forms of breast cancer are distinguished. In 75–80% of cases, the nodular form occurs. In the early stages, the only symptom is usually a painless lump in the breast. If you divide the breast into four parts by horizontal and vertical lines, then in half of the cases the tumor will be located in the upper outer part.
Special forms of breast cancer have also been identified, which manifest themselves with typical symptoms. These include:
- An edematous-infiltrative form, which is characterized by enlargement and swelling of the gland, marbled skin color, and severe hyperemia.
- Mastitis-like. This type of breast cancer is manifested by hardening of the affected breast and increased body temperature.
- An erysipelas-like form, in which lesions are detected on the skin (sometimes ulcerations appear) that externally resemble erysipelas.
- The armored form is characterized by the presence of multiple nodes, due to which the gland shrinks and deforms.
- Paget's cancer affects the nipple and areola. With this type, thickening of the nipple, changes in the skin in the form of redness and thickening, and the formation of crusts and scales are observed.
Sometimes people, wondering what signs can be used to recognize the presence of a breast tumor, mistakenly look for symptoms of sternum cancer. This name is incorrect, since the sternum is the central flat bone of the chest and, even with metastasis of a malignant breast tumor, is almost never affected.
Where to get an x-ray and how much does it cost?
Breast X-rays are performed both in public clinics and private diagnostic centers and hospitals.
If you need a regular mammogram, with a referral from a gynecologist, it can be done free of charge at a public medical institution (at your place of residence). Such programs are funded by the Ministry of Health with the aim of timely detection of breast cancer in women.
If it is necessary to carry out detailed diagnostics using expensive equipment, the patient is sent to a private clinic.
The cost of mammography depends on the x-ray method (digital, CT, tomosynthesis), as well as the area being examined.
Advantages and disadvantages of the method
Breast X-ray is an accessible and informative method for diagnosing female diseases. Detects any changes - cysts, tumors, infiltration, inflammatory processes. The image visualizes small details, boundaries of formations, and tissue texture. It is used not only to detect pathology, but also as screening in women after 40 years.
The disadvantages of the method include radiation exposure to the body - receiving a dose of ionizing radiation. During the examination, some women experience discomfort and even pain. For girls of reproductive age, the technique is not very informative. It is difficult to diagnose women with small or excessively large breasts.
Is it harmful to do the procedure?
We receive a huge number of questions about the dangers of mammography for women, because in the process of conducting such a study, harmful ionizing radiation is still present. Fortunately, even for film diagnostics, the radiation dose is extremely small and relatively safe.
Important! In no case should you refuse such an examination, especially if it helps to make a correct diagnosis, due to unfounded fears about the development of malignant tumors due to X-rays. The chance of such consequences is extremely small.