The body's reaction to external irritants is swelling of the mucous membrane, redness and rashes on the skin. Immunoglobulin E is responsible for this.
The production of these antibodies in response to the appearance of foreign cells (including bacteria, fungi) occurs in the submucosal layers of the digestive system, skin, tonsils, adenoids, and respiratory tract.
The immunoglobulin E level in bronchial asthma is important for diagnosis. This disease is associated with suffocation, shortness of breath and cough caused by inflammation and the reaction of the bronchi to irritants.
What is the disease: briefly about the main thing
Bronchial asthma is a pathological condition that is inflammatory and immunoallergic in nature, occurs in a chronic form, exacerbations occur under the influence of allergens.
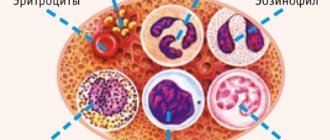
As a result of sensitization (hypersensitivity) of the body, an immunoallergic reaction begins, which is accompanied by the active release of eosinophils, lymphocytes and inflammatory mediators (prostaglandins, leukotrienes, histamine, heparin). These substances increase the permeability of the vascular wall, which leads to swelling and spasm of the bronchioles. The secretion of mucus in the bronchi also increases, it becomes more viscous (this is due to the action of prostaglandin F2a).
Most often, bronchospasm is caused by inhaled agents - allergens that enter the body through the mucous membrane of the respiratory tract. This could be dust, fluff, pet hair, or pollen from some plants. Approximately 20-23% of people suffering from the disease are hypersensitive to food allergens (chocolate, citrus fruits, seafood), and 2-5% are allergic to medications (antibiotics, non-steroidal anti-inflammatory drugs, local anesthetics).
Despite the fact that this pathological condition is characterized by a severe and long-term course, today there are many treatment methods that make it possible to transfer the disease to a stage of stable remission. But in order to correctly prescribe treatment, the doctor must conduct a multi-stage diagnosis.
Condition of the small airways
It is generally accepted that measuring the midpoint on the expiratory curve of forced expiration or the average volumetric flow rate is a functional test of small bronchi, and the total forced expiratory volume indicates the performance of large highways. But studies of structure-function relationships have shown that the conclusions are incorrect. After all, the alveoli are part of the small respiratory tract and small bronchi, and therefore flow into the general system. The entire expiratory airflow then finally reaches the spirometer. Therefore, all factors are interrelated, and not a single isolated indicator on the curve reveals differences in the elements of the system.
Isolated diseases of the small respiratory tract also exist. For example, with bronchiolitis obliterans, expiratory airflow is disrupted in the same way as with asthma or chronic obstructive pulmonary disease. Therefore, spirometry is not able to provide a differential diagnosis between asthma and COPD.
Stepwise approach to diagnosis and treatment
The method of a stepwise approach in the diagnosis and treatment of bronchial asthma is that the more severe the disease, the more examinations and medications the doctor prescribes. At the initial appointment with the doctor, the patient is questioned, his complaints are found out, his life history, illnesses are clarified, and allergy and family history is collected. Then they conduct an examination: count the pulse and respiration rates, note whether auxiliary muscles (for example, abdominal muscles, intercostal muscles) are involved in the breathing process. Based on the data obtained, it is possible to make a primary diagnosis and prescribe certain medications.
However, if a person experiences frequent paroxysms of bronchial asthma, but pocket inhalers with bronchodilators do not help stop them, then additional instrumental and laboratory research methods are also needed. They will help to find out the nature of the disease and prescribe the correct treatment.
A stepwise approach to treatment begins with prescribing the simplest treatment methods: anti-inflammatory drugs, pocket inhalers, physiotherapeutic procedures and breathing exercises. If the first “step” is not effective enough, then stronger drugs for inhalation are prescribed, for example, bronchodilators (M-anticholinergics and 2-adrenergic agonists). If these remedies are not enough, then local and systemic glucocorticoids, slow sensitization with allergens and other treatment methods are added to these treatment methods.
It is believed that a stepwise approach to the diagnosis and treatment of pathology is the most correct today. It allows not only to assess the severity of the pathology, but also to save the patient from unnecessary research and prescription of medications that are not indicated at this stage.
But, despite the fact that there are many diagnostic methods that make it possible to determine this disease, often (especially in the first stages) the disease is expressed only in the form of a cough without sputum production. Therefore, patients turn to a specialist only when the first paroxysm of bronchial asthma occurs.
Assessing a Patient with Asthma Using a Spirogram
Physical assessment of patients with asthma is not accurate, therefore, in the remission stage, breathing volumes normalize.
The presence of bronchial obstruction during status asthmaticus is also beyond doubt. However, spirometry makes it possible to assess the severity of bronchial asthma. Since the level of gases in the blood changes only during attacks, and x-rays do not determine pulmonary function in order to track the development of the disease.
The goal of treatment is to achieve an asymptomatic state with a maximum increase in FEV1 and FVC values. It is on the basis of these indicators that powerful inhaled bronchodilators and glucocorticosteroids should be prescribed.
Spirometry allows you to evaluate which doses provide the maximum therapeutic effect.
If asthma is left untreated, changes in the alveoli become irreversible, resembling COPD. There will be a decrease in FEV1, which is a powerful indicator of asthma prognosis.
Author of the publication: Inna Kailin
Remember!
Self-medication can cause irreparable consequences for your health! At the first symptoms of the disease, we recommend immediately contacting a specialist!
Key diagnostic methods
The detection and treatment of the disease is carried out by pulmonologists, as well as allergists, therapists, and immunologists. Sometimes it is also necessary to consult a neurologist, cardiologist and other specialists who diagnose concomitant diseases.
Sometimes it can be difficult to distinguish the symptoms of bronchial asthma from other diseases, for example, cardiac asthma, pulmonary embolism, chronic bronchitis, pneumonia, lung tumors. That is why differential diagnosis must be carried out by a qualified and experienced specialist.
There are a number of important methods for diagnosing the disease:
- Physical examination (assessment of heart rate and respiratory movements).
- Auscultation (listening for wheezing in the lower parts of the lungs).
- Percussion (tapping the chest).
- Functional examination of external respiration (assessment of vital capacity of the lungs, tidal volume, forced expiratory volume).
- General blood analysis.
- Biochemical blood test.
- Immunological blood test.
But this pathological condition may also be similar to other ailments of the respiratory and cardiovascular systems, therefore, only an initial examination and examination is not enough: it is necessary to make sure that there are no chronic pathologies.
What indications can be identified?
The deciphering of the spirogram is carried out taking into account the personal characteristics of the patient (gender, age, weight, height).
The norms for patients who belong to different groups are not the same. Without taking this fact into account, it will not be possible to establish the correct cause of the disease. The list of indicators that were obtained when reviewing the results includes:
- the amount of air entering the body per minute;
- breathing density;
- vital capacity of the lungs;
- tidal volume.
These indicators are established at the very beginning of the procedure. For the purpose of a more in-depth study of the functioning of the lungs, additional studies are prescribed.
To establish the reactivity of the bronchi, provocative tests are done. The test is also indicated in the following cases:
- the clinical picture is unclear;
- have chronic diseases;
- the etiology of the disease is unknown.
Attention! Provocative tests are taken under the supervision of a doctor
Additional instrumental diagnostic methods
It is not always possible to make a diagnosis based on the examinations described above. The next “step” in diagnosing bronchial asthma is conducting additional instrumental and laboratory studies. Based on them, it is possible to exclude concomitant chronic diseases of the respiratory and cardiovascular systems, and also more accurately determine when the disease began, at what stage it is and what provokes its exacerbations.
Additional examination methods include:
- Sputum analysis (allows you to determine the nature of inflammation).
- Spirometry (helps assess the degree of obstruction of the bronchial tree).
- Peak flowmetry (assess peak expiratory flow in the evening and morning, draw up a schedule for 2-4 weeks). If PEF begins to decrease, then we can say that there is a risk of the disease moving into the exacerbation phase - you need to urgently consult your doctor.
- Assessment of blood gas composition (determine the amount of oxygen, carbon dioxide).
- ECG (performed to exclude cardiac asthma).
- Plain radiography (performed to exclude pneumonia).
- Bronchoscopy (helps identify possible tumors).
- Allergy tests (prick test, skin prick test, patch test).
- Radiography of the lungs.
- Computed tomography (CT) - allows you to exclude circulatory disorders in the pulmonary circulation, lung tumors and other concomitant diseases.
After carrying out a full range of diagnostic measures, it is possible to determine not only the form and extent of the disease, but also to select the most suitable medications.
How the research is carried out
The correct actions of the staff and the patient during a spirogram for bronchial asthma allow you to obtain the most accurate result.
If all the doctor’s requirements are met, the procedure does not cause any unpleasant emotions or sensations in the patient.
It is important to ensure that the patient does not experience anxiety or agitation during operation of the spirometer.
The main purpose of the study is to assess the working volume of the lungs. In this case, it is necessary to exclude or confirm the presence of certain pathological processes.
To obtain the most accurate result, the procedure is carried out in a dimly lit room. It is advisable to exclude loud sounds and other irritating factors. Recommended air temperature is from 18 to 24C.
During the study, different models of devices are used to measure breathing parameters, ranging from a purely mechanical device to a modern computer spirometer.
The study is carried out according to the following methodology:
- A patient suffering from bronchial asthma needs to be seated. Carrying out the examination while standing can greatly distort the main indicators of spirography, which will be significantly higher than normal.
- A special clip is placed on the patient's nose.
- The patient is given a special sterile mouthpiece. Several calm inhalations and exhalations are performed through it.
- After this, a series of inhalations and exhalations is performed with maximum amplitude.
- Pause 20 seconds.
- Inhale and exhale again at a normal pace.
- The last breathing cycle is performed at the maximum possible pace.
If necessary, the doctor may ask the patient to take as deep breaths as possible for 20 seconds.
The whole procedure takes no more than 15 minutes. After this, the patient needs to rest for some time.
Additionally, a test with bronchodilators may be prescribed. In this case, there are a number of differences from the standard procedure.
At first, everything is done as in a normal study. The patient is then given a bronchodilator, most often by inhalation. After a short period of time, the procedure is repeated.
This study allows you to choose the right medicine that has the greatest therapeutic effect. It is also possible to identify spasms in the bronchi and understand whether the obstruction processes are reversible.
Interpretation of examination results
To determine the presence of pathology in a patient, it is necessary to be able to correctly decipher the results of instrumental and laboratory tests.
At the initial examination, you may notice some deviations from normal indicators:
- Physical examination: possible tachycardia (heart rate over 90 beats per minute), as well as tachypnea (respiratory rate over 16 per minute).
- Auscultation: rough breathing is heard, whistling dry rales, intensifying with exhalation.
- Percussion: box sound, the lower border of the lungs is lowered, almost motionless.
- Functional examination of external respiration: increased vital capacity (VC) and tidal volume (TI), decreased forced (accelerated) expiratory volume (FEV).
If a patient goes to emergency medical care or to a family doctor during a paroxysm of the disease, a characteristic posture (orthopnea) will be noticeable: the patient is sitting, his back is bent, his hands are resting on the edge of a chair or bed. You can also experience a dry cough, as well as wheezing, severe shortness of breath, and the jugular veins (in the neck) swell. Possible tachycardia. The paroxysm can last from 5-10 minutes to 3-6 hours, and it usually ends with the release of colorless sputum. The danger of this condition lies in the threat of the formation of status asthmaticus - a sequence of attacks that cannot be stopped with the help of bronchodilators.
Laboratory results and their meanings
Laboratory research methods can also provide a wealth of information about the disease.
- Complete blood count : increased number of eosinophils (more than 5%), ESR (over 15 mm/minute), neutrophils (more than 48-50%).
- Biochemical blood test : increase in the concentration of gamma globulins and alpha-2-globulins and fibrinogen.
- Immunological blood test : a significant increase in the concentration of immunoglobulins of class E and G and typical immunoglobulins E to the identified allergen.
- Sputum analysis : an increased number of Kurshman spirals, as well as Charcot-Leyden crystals - these are fibers of small bronchioles and dead neutrophils that were on the mucous membrane. The sputum is usually colorless, viscous, two-layered, and difficult to separate.
- Blood test to determine gas composition : gas alkalosis (increased pH), increased amount of carbon dioxide, decreased oxygen content.
Decoding the results of instrumental studies
Instrumental diagnostic methods help to exclude concomitant diseases, assess the function of external and internal respiration, and determine the allergen that causes paroxysms of the disease:
- Spirometry : decrease in vital capacity of the lungs (less than 90), expiratory reserve volume (less than 70% vital capacity), forced expiratory volume per second (less than 80). After the introduction of bronchodilators, the above-described indicators sharply increase, which indicates the allergic nature of this disease.
- Peak flowmetry : peak expiratory flow decreases to 60-70% of the normal (or individual) value, the difference between the evening and morning PEF is more than 25%.
- ECG : respiratory dysfunction is visible, which manifests itself in a high P wave, heart rate is increased, the rhythm is rarely disturbed.
- Survey radiography : the borders of the lungs are unclear, the lower border is sharply lowered, the roots of the lungs are narrowed, full of blood. The chest is barrel-shaped.
- Bronchoscopy : the bronchial mucosa is inflamed, hyperemic (there is redness), the bronchial lumen is greatly narrowed, there is a large amount of viscous, uncolored sputum on the walls.
- Allergy tests : at the site of application (injection) of the allergen that causes paroxysms, redness, swelling, burning and itching are noted. When performing scratch tests and prick tests, these symptoms are observed after 15-25 minutes. The patch test makes it possible to detect the provoking factor that causes an allergic reaction of the delayed hypersensitivity type. When conducting a patch test, the result is assessed after 24, 48 and 72 hours.
- Radiography of lung tissue : an increase in the density of lung tissue is a sign of pneumosclerosis against the background of prolonged infectious-allergic bronchial asthma.
- Computed tomography (CT) : narrowing of the bronchi, local dilatation of blood vessels.
Based on the results of laboratory and instrumental studies, the stage of the disease can be determined and adequate treatment can be prescribed.
What is spirometry procedure? a brief description of
diagnostics
brainrehabilitation of anesthesiaCOBLastmaemphysemabronchitissymptomsshortness of breathcough
- Obstructive type
, caused by a violation of the passage of air through the bronchi (for example, with spasm, swelling or inflammatory infiltration of the bronchi, with a large amount of viscous sputum in the bronchi, with deformation of the bronchi, with collapse of the bronchi on exhalation); - Restrictive type
, caused by a decrease in the area of the alveoli of the lungs or low extensibility of the lung tissue (for example, against the background of pneumosclerosis, removal of part of the lung during surgery, atelectasis, diseases of the pleura, abnormal shape of the chest, disruption of the respiratory muscles, heart failure, etc.) ; - Mixed type
, when there is a combination of both obstructive and restrictive changes in the tissues of the respiratory organs.
The essence of spirometry
The term is formed from two words: spiro - breathing and metria - measurements, measurements.
Spirometry is a diagnostic examination of the function of external respiration with the establishment of characteristic speed and volume indicators.
The method is widely used in medicine: it allows you to identify pathologies that cause low levels of gas exchange.
The procedure is carried out with a special digital device - a spirometer. Their mechanism is quite simple: an air flow sensor and a computing part that converts information into numerical values.
The readings are calculated automatically. There are computer modifications of the device.
The first examinations were carried out with mechanical (most often water) spirometers. All indicators were calculated manually. The procedure was long and laborious.
If constant monitoring is necessary, you can use a modern portable spirometer, which is applicable both at home and when traveling.
Consultations with your attending physician and a medical specialist who sells similar equipment will help you choose the right device. A spirometer is selected taking into account functional requirements and personal preferences.
The most accurate measurements are obtained by a special camera with sensors - a plethysmograph. The results of the study, presented graphically in the form of spirography, help to clearly illustrate modifications in human lung volume during normal and forced breathing. What is spirography and what it looks like can be clearly seen in the figure:
Through the procedure:
- diagnose pathological abnormalities (foci of gas exchange disturbances, level of bronchial obstruction);
- assess the patient’s condition during treatment and the effectiveness of therapy;
- teach various breathing techniques.
Measurements are carried out on an outpatient basis with immediate results.
Causes
It is not known for certain why the disease occurs. It is believed that its appearance is due to a complex interaction of various factors. Apparently, the key mechanism is the release of biologically active substances (inflammatory mediators) from the cells of the bronchial mucosa in response to various stimulants or triggers. The trigger for bronchospasm can be:
- Allergens - contact with antigens that cause an allergic reaction in patients sensitive to them, and, accordingly, bronchospasm. This could be animal hair, plant pollen, household dust, food.
- Non-allergic triggers are substances contained in detergents, or used in perfumes, epoxy adhesives, smoke, chemicals.
- Physical exercises (bronchial asthma of physical exertion).
- Stress and strong emotional reactions.
- Exposure to cold air.
- Medicines such as beta blockers and aspirin.
Identifying and avoiding exposure to the trigger can help prevent asthma attacks. Allergists and immunologists are doctors who specialize in helping patients identify allergens. It may cause an exacerbation of the disease. These doctors can help with allergic bronchial asthma.
Analysis of bronchoalveolar lavage and arterial blood gases
When analyzing bronchoalveolar lavage, a significant number of different leukocytes will be detected in the analyzed material. This analysis shows a paucity of alveolar macrophage (basophil) volume and a slight increase in the number of lymphocytes and neutrophils. Eosinophilia is particularly pronounced.
Changing the level of gas pressure in arterial blood is of great importance, because the gas composition contributes to the correct determination of the severity of the disease. In bronchial asthma, these blood components vary in direct proportion to the severity of the disease. Thus, in severe cases of the disease, the volume of oxygen decreases, and the volume of carbon dioxide increases. With this picture, the patient needs oxygen inhalation.
Bronchial asthma is an intractable disease with recurrent attacks, the specificity of which is an individual treatment regimen and constant monitoring of the course. To do this, you need to visit your doctor on a schedule, strengthen the body’s immune functions and eliminate allergens. The absence of attacks and a healthy lifestyle with asthma is easy!