For diseases of the respiratory system, accompanied by coughing attacks and fever, which may be signs of bronchitis, the doctor, along with other tests, prescribes an x-ray examination.
Often, x-rays for bronchitis are used in diagnosis as an addition to other methods.
The doctor first of all takes into account the results of laboratory tests of blood and sputum, the presence of noise in the lungs, and looks at the general condition of the patient.
An x-ray is necessary to rule out other respiratory diseases. This examination speeds up the process of making a correct diagnosis, which means it contributes to successful treatment.
The importance of bronchography in x-ray examination
X-ray examination for bronchitis is an auxiliary diagnostic method. With its help, you can identify or exclude obstruction, focal pneumonia, and also diagnose serious diseases, such as tuberculosis or lung cancer, which are often hidden behind the symptoms of bronchial inflammation. X-rays do not image the tissue and condition of these branches of the windpipe. It allows you to record only some deviations from the norm. In such cases, a doctor can confirm bronchitis only by excluding visible lung pathologies. If they are not there, then these are symptoms and manifestations of bronchitis.
On an x-ray, the image of healthy lung tissue has a uniform light tint. The presence of pathological processes, expressed in atypical shadows, may indicate incipient pulmonary edema and serious inflammation.
Fluorography for bronchitis is not effective, since its results cannot show the full picture of the disease. It can only be used to determine the condition of tissues that are affected by fibrosis or foreign agents. If we consider from the point of view of safety for the body, then fluorographic examination is a higher priority than x-rays. However, the lack of information about the course of the disease makes it useless against the background of a chest x-ray.
Fluorography
Fluorography is essentially not much different from conventional radiography. It is a chest X-ray, in which the image is transferred to a film measuring 5x5 cm, 7x7 cm or 10x10 cm. It is the size of the image that is the key difference between these two techniques , since with standard radiography, the image on the image corresponds to the real size of the chest. The technique for performing the procedure does not differ from conventional radiography, except that fluorography is performed only in a direct projection.
The method is specially designed for screening examinations for diseases such as tuberculosis and malignant neoplasms. Reducing the size of the images made it possible to make it much cheaper (6 times compared to the standard size), but at the same time significantly reduced the information content of the study.
For this reason, fluorography does not show bronchitis , with the exception of severe chronic forms with established COPD. On fluorography, simple bronchitis is not visible, since it is impossible to visualize the intensification of the vascular pattern in a small image.
Clinical picture of bronchitis
Bronchitis is an inflammatory process in the organs of the respiratory system that affects the lobar, segmental, interlobular, lobular and intralobular bronchi, and bronchioles. It can be observed as an independent process or as a complication against the background of viral or infectious colds.
Bronchitis is characterized by inflammation of the mucous tissues of the bronchial tree. In this case, the onset of the inflammatory process may be accompanied by swelling of the tissues, their compaction, and all this together leads to a narrowing of the respiratory lumen.
The course of bronchial disease can take different forms:
- acute inflammation – has obvious signs of a sharply onset disease, the total duration does not exceed 14 days. The disease manifests itself as a dry, irritating cough. After a couple of days, difficult to expectorate sputum appears. There is an increase in the patient's body temperature to 39 degrees;
- chronic inflammation - mild symptoms appear over a long period, which can last three weeks or more. The appearance of a wet cough with sputum is typical in the morning (immediately after waking up). The body temperature remains within the subfebrile range - no higher than 37.5 degrees;
- obstructive inflammation - a severe course of the disease is complicated by severe attacks of coughing and lack of oxygen (suffocation). The presence of obstruction can be determined by wheezing and changes in respiratory movements. Additionally, the muscles of the neck and abdominal muscles are involved.
Indications for a chest x-ray for suspected bronchitis
Drawing up a diagnostic picture of bronchial disease includes several activities.
- Questioning or collecting anamnesis of the disease. It is necessary to mention lifestyle, place of work, concomitant diseases and environment.
- Auscultation of breathing using a stethoscope. Allows you to identify extraneous noises, the presence of which may characterize a particular disease.
- Percussion of the respiratory system. Determines the presence of sputum in the bronchial body and serves to determine the severity of inflammation.
- A set of laboratory tests of biological materials (blood, urine, sputum). Allows you to identify the pathogen to determine the drugs active against it and prescribe a course of treatment.
In cases of a prolonged course of the inflammatory process, accompanied by a deterioration in the general condition and fever, as well as in case of unsatisfactory results of laboratory tests and insufficient effectiveness of previously prescribed treatment, the attending physician may prescribe an x-ray of the bronchi and lungs to exclude serious pathologies. For bronchitis, fluorography is not advisable due to the fact that its results have no diagnostic value.
Reasons for the development of the disease
The reasons that can provoke inflammation of the bronchi may include:
- development of complications of acute respiratory diseases or acute respiratory viral infections;
- entry into the body of various infectious agents in the form of fungi, chlamydia, mycoplasma and others. A common situation is when, after a purulent sore throat, bacteria and toxins accumulate in the bronchi (especially during sleep, when the cough effect is suppressed) and, multiplying on the lining of the respiratory organs, affect them;
- excessive addiction to bad habits (smoking);
- work in a production facility that produces harmful pollutant particles;
- one of the forms of allergy.
Correct diagnosis and identification of the causes of the disease make it possible to cure the onset of illness in a short time and with minimal consequences and prevent the transformation of acute bronchitis into chronic.
Indications for the study
X-ray diagnostics are prescribed:
- if you suspect a disease such as bronchitis;
- in order to distinguish it from pneumonia;
- to detect obstruction;
- in the absence of therapy effectiveness;
- to monitor the effectiveness of therapy and recovery.
Using X-rays, pathologies of the blood gas composition, as well as ventilation of the lungs, are detected.
Attention! X-rays are always performed for both obstructive and recurrent bronchitis.
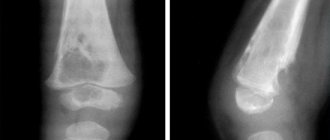
The photo clearly shows what chronic bronchitis looks like on film.
When any symptoms of bronchitis appear, the patient is referred for X-ray diagnostics
The patient's fever does not subside for a long time. The temperature usually rises in the evening. The patient suffers from symptoms of bronchitis such as chills, shortness of breath, sweating and cough.
When receiving blood tests from a patient, the doctor finds the following indicators in the results:
- acceleration of ESR;
- increased number of leukocytes.
Who should not conduct research
Prohibitions on performing lung X-rays include childhood patients (up to 15 years in accordance with the country’s legislation), severe conditions when the dose of X-ray radiation received can provoke the development of serious pathological processes or cause a decrease in the body’s immune defense. X-rays for bronchitis during pregnancy are also undesirable. It can cause disruption of the normal development of the fetus and cause pathologies, including the death of the fetus. The risk of complications must be weighed against the real threats to the mother's life.
Who is contraindicated for CT?
Contraindications to the study are:
- Pregnancy of any stage
- Lactation (CT is possible with weaning for at least a day)
- Children under 3 years of age (for children 3-10 years old, the procedure is performed only if there are serious indications)
- Weight more than 170-200 kg (relative contraindication, depends on the type of device)
- Claustrophobia, epilepsy, other mental disorders
CT angiography may be prohibited if you are allergic to the contrast agent. If it contains iodine, then tomography is contraindicated for hyperthyroidism, other pathologies of the thyroid gland, multiple myeloma, advanced stage of diabetes mellitus, heart failure, renal failure. You will have to reschedule the diagnosis if any studies using bismuth and barium have already been performed within a few days - they can negatively affect the interpretation of the tomography results.
What does bronchitis look like on an x-ray?
Bronchitis on x-ray demonstrates changes in the respiratory tract that begin during inflammation. The combination of colors in a picture of the respiratory organs should normally look like this:
- gray color – display of soft tissues;
- white color – visualization of bones absorbing radiation;
- black color - cavities with air that transmit rays through themselves.
In the presence of an inflammatory process, the density and structure of organ tissues change. These changes can determine the development of a serious disease.
X-rays do not show the inflammatory process during the development of bronchitis. However, with correct diagnosis and competent interpretation of the result, it will help to identify and show its indirect signs:
- lung tissue changes its structure;
- thickening of the bronchial walls occurs;
- changes manifested by the appearance of air cavities in the lower part of the lungs;
- the appearance of compactions formed due to the accumulation of fluid in the tissues of the respiratory system;
- increased manifestation of the bronchial tree pattern.
Main features
X-ray diagnostics when detecting bronchitis in the images can be manifested by the following main signs:
- tissue collapse appears, which appears in the form of lamellar lesions;
- infiltration of areas of adjacent tissues appears;
- the pattern of the bronchi changes, small vessels disappear and become invisible.
If the X-ray image shows the appearance of linear and ring-shaped shadows, which are a sign of proliferation of connective peribronchial tissue, it means that the patient has obvious signs of chronic bronchitis. The process of fibrosis formation occurs. Symptoms of pulmonary hypertension are also observed - the diaphragm changes its position, and large pulmonary vessels expand.
Obstructive bronchitis
Obstructive bronchitis on a standard radiograph is manifested by the main signs of bronchitis itself, along with acute and chronic. In this case, fuzzy contours and a greatly altered pulmonary pattern with thickening of the bronchial walls are observed. The transparency of the alveoli structure increases. The diaphragm thickens and shifts due to inflammation. Stagnation and disruption of the normal functioning of the pulmonary circulation occur. X-ray shows a decrease in the clarity and structure of the roots of the lung body, as well as a slight increase in size and blurred boundaries.
What are the differences in symptoms?
Bronchitis and pneumonia are related diseases. One often precedes the other. The respiratory tract consists of the nasopharynx, larynx, trachea, bronchi and lungs. If the trachea, bronchi and bronchioles are affected, then a diagnosis of bronchitis is made. If the pathological process has spread to the alveoli and further to the lung tissue, then a diagnosis of pneumonia is made. To better understand how bronchitis differs from pneumonia, let’s summarize the main points in a table.
| Sign | Bronchitis | Pneumonia |
| Pathogen | VirusBacteria predominates | Bacteria predominate Viruses Fungi |
| What is affected | TracheaBronchiBronchioles | AlveoliLung tissue |
| Peculiarities | The mucous membrane is affected, it swells, turns red, thickens | An infiltrate begins to form at the site of inflammation |
| Start | Slow | Acute |
| Temperature | 37-38оС | 38-40оС |
| Cough | Dry with gradual transition to wet | Wet |
| Sputum | White and yellowish, viscous | Yellow, greenish-brown, “rusty” |
| Chest pain | Rarely, with advanced forms | Often, occurs when inhaling or coughing, radiates to the side |
| Shortness of breath | Rarely, during physical activity | Eat both at rest and during physical activity |
| Violation of general condition | Moderate | Strong |
| Auscultation | Is it dry mixed wheezing? | Wet wheezing |
| Percussion | The sound is not changed | Muffled sound in the area of inflammation |
| X-ray | Strengthening the pulmonary pattern | Darkening in the area of inflammation |
| Blood analysis | Increase in leukocytes, ESR insignificant | A sharp increase in leukocytes, ESR, neutrophilia |
| Treatment | Outpatient, rarely in hospital | Only mild forms can be treated at home; inpatient treatment is recommended. |
The degree of manifestation of symptoms depends on what pathogen caused the disease and its severity. It is important to know how to distinguish bronchitis from pneumonia in an adult, but even more important in a child. The peculiarity of a child’s body is that inflammation from the bronchi very quickly (a day or several days) spreads to the lungs.
Intoxication increases, the condition worsens sharply. At the initial stage, it is difficult to both distinguish bronchitis from pneumonia and begin proper treatment. Even a doctor, when listening to breathing, cannot determine what exactly the patient’s diagnosis is.
Then only x-rays can provide complete information. If you have any suspicion, you should immediately go to the hospital.
Diagnosis of bronchitis in children
Bronchitis is often characterized by complications in children in the first three years of life. In infants up to one year old, when bronchitis develops, moderate shortness of breath may be present. When tapping, a boxy pulmonary sound appears. Dry and moist diffuse rales are heard. A whistling sound may occur when exhaling.
Acute (simple) bronchitis in the image obtained as a result of fluorography in children appears as changes in the form of an intensification of the pulmonary texture pattern, while the roots of the bronchial tree are significantly expanded. There may be an increase in the airiness of the lung tissue. There are no focal changes in the respiratory organs.
Contraindications
X-rays have no contraindications as such. There are isolated cases when a person is in serious condition. If the need for x-rays remains, the procedure is performed after stabilization of the patient's condition.
During pregnancy, in order not to irradiate the fetus, x-rays are not prescribed. But if the threat to the mother’s health is significant, the study is carried out by covering the abdomen with a special screen.
Many people are interested in how many safe radiation sessions can be performed annually. It depends on the doctor's indications and recommendations. Normal radiation exposure for humans is 100 roentgens per year.
If difficulties arise in diagnosing the disease, bronchography is performed. This procedure is performed extremely rarely, under local anesthesia. A warm contrast agent is injected into the patient's bronchi and, using an x-ray, the doctor can examine what is happening in the respiratory tract, what the severity of the pathology is, where it is localized and what changes have occurred.
Bronchography today provides the most accurate picture of pathologies in the respiratory organs. In addition, bronchoscopy is performed, which also allows you to study the bronchi from the inside. But all these measures are not very pleasant, so they are prescribed only in extreme cases.
If bronchitis has been diagnosed using X-ray studies, the doctor will prescribe treatment, which usually has a positive prognosis. The main thing is to contact the clinic in a timely manner.
Decoding the results
If an X-ray of the lungs in children does not reveal any changes during bronchitis, this is not evidence of the absence of serious diseases.
Bronchitis in childhood is manifested by an increase in the pulmonary pattern in the hilar region of the lungs. Moderate obstructive disorders may be recorded.
Interpretation of X-ray results in children should also be differentiated from pneumonia, the presence of a foreign body in the bronchi, bronchial asthma and other diseases.
Treatment of the disease
If bronchitis is detected on a FLG image or X-ray of the lungs, confirmed by laboratory tests, the doctor will immediately prescribe an effective course of treatment with medications.
Drugs are prescribed based on the main causes of the disease.
Bacterial bronchitis is treated by prescribing antibacterial agents. These drugs are: Azithromycin, Ceftriaxone, Augmentin. For viral cases, antiviral drugs are used: Grippferon, Kipferon, Arbidol. At high body temperatures, antipyretics are prescribed: Nurofen, Panadol, Paracetamol. In case of a strong wet cough, expectorants are used to facilitate the passage of bronchial secretions: ACC, Ambroxol, Ascoril. Inhalation with saline solution will help alleviate the condition of a severe dry cough. It is important to understand that inhalations are allowed only in the absence of elevated body temperature.
Manifestation of pneumonia
To understand the difference between bronchitis and pneumonia in adults, let us consider in detail the symptoms of pneumonia.
Pneumonia, or pneumonia, is an infectious disease of the lower respiratory tract that can be caused by viruses, bacteria or fungi. With it, intoxication quickly develops and respiratory failure increases. Only a mild form of the disease can be treated at home; for moderate and severe forms, therapy is carried out in a hospital.
The main symptoms of pneumonia are:
- A sharp increase in temperature to 38-40°C, which lasts for a long time and is poorly controlled by antipyretics.
- Severe weakness.
- Pain in muscles and joints.
- Shortness of breath at rest or with minimal physical activity.
- Headache
- Wet cough with copious discharge of purulent sputum, sometimes mixed with blood.
- Chest pain that gets worse with coughing or inhaling.
- Tachycardia.
Often the symptoms of the disease are vague, the cough may be absent or insignificant, the temperature does not rise to high levels, or the person takes antipyretics several times a day and cannot adequately assess the degree of fever. In this case, only instrumental diagnostic methods (x-rays) will help make the correct diagnosis.
Prevention of bronchitis
Strengthening the immune system is the main way to counteract various factors that can trigger the onset of the disease. Local immunity training should include the following:
- maintaining an active lifestyle with moderate physical activity in accordance with age;
- frequent walks in the fresh air, preferably in a forested area;
- eating only high-quality foods high in vitamins and minerals;
- compliance with air quality standards in the living room - it should be fresh, cool and moderate humidity;
- During the period of a cold, timely treatment and strict adherence to recommendations for taking medications are necessary.
Measures to prevent diseases of the respiratory system include regular screening fluorography of the chest organs. Annual radiography does not cause significant harm to the body, but helps to identify diseases such as bronchial asthma, tuberculosis, and oncological processes in the early stages.
Is pneumonia contagious?
Pneumonia can be caused by viruses, bacteria, fungi and other microorganisms. There are several types of pneumonia:
- Typical (symptoms of pneumonia in a child appeared as a result of hypothermia, ARVI).
- Aspiration (microbes enter the lungs along with mucus and vomit).
- Atypical. The causative agents are unusual forms of bacteria that live in the air of closed rooms with artificial ventilation. Depending on the type of pathogen, mycoplasma, chlamydial and other types of pneumonia are distinguished. They are difficult to diagnose using x-rays. The type of disease is established only using instrumental methods of analysis.
- Hospital infection, which occurs 2-3 days after the child is admitted to the hospital, and he initially does not have a pulmonary infection. It often appears after operations on the abdominal cavity, in the chest area, in patients with artificial ventilation. The causative agents of such pneumonia are not sensitive to the action of antibiotics.
Transmission of infection during pneumonia occurs mainly through airborne droplets. Viruses and bacteria from a sick child, when coughing and sneezing, enter the respiratory organs of surrounding people, causing the appearance of influenza or ARVI. But whether they later turn into pneumonia depends on the state of the immune system, the timeliness and correctness of treatment for these diseases. The risk of infection is especially high during asymptomatic pneumonia or during the incubation period when there are no manifestations. The most contagious and dangerous are atypical and hospital-acquired pneumonia, especially caseous (tuberculosis).
Note: After the baby shows signs of illness, there is no point in separating him from the rest of the family members who had contact with him before, since the infection has already entered their body. It is necessary to take measures (take vitamins, treat your throat, eat garlic, lemons). It is better for the baby to refrain from contact with strangers until the runny nose and cough go away.
The incubation period is 3-10 days. The acute stage of the disease lasts up to 6 weeks.
Traditional methods of treating bronchitis
In cases where it is impossible to use medications to treat bronchial inflammation, an effective alternative is recommended - traditional medicine recipes. The essence of the methods is to provide a local warming effect, which promotes the expansion of the bronchi and the discharge of sputum. The use of home medicine is permissible if you are confident that there is no allergic reaction to the incoming components.
Potato cake compress
To prepare a compress, boil a couple of medium-sized potatoes “in their jackets” until tender. In a bowl, mash the potatoes until smooth. The compress can be used in its pure form or with the addition of natural warming substances - honey, mustard powder and others. For plasticity, add a teaspoon of vegetable or olive oil to the potato mass. The compress is applied from the side of the bronchi, covered with film and wrapped in a warm blanket.
Lemon juice with glycerin and honey
The juice of lemon zest boiled for 10 minutes is squeezed out and mixed with 4 teaspoons of glycerin and natural honey. The resulting mixture is taken orally, ½ tablespoon throughout the day.