Advantages over open chest surgery
Lung thoracoscopy is a minimally invasive procedure that is gaining popularity in pulmonology and thoracic (chest) surgery. With the help of this examination, it is possible, without much harm or trauma to the patient, to visually assess the condition of the pleural cavity and the organs located in it.
Interesting! For the first time, the corresponding procedure was carried out by the Swedish physician Hans Christian Jacobeus in the pulmonology department. To assess the condition of the pleural cavity, the doctor used an endoscope to diagnose bladder pathology - a cystoscope. Over the next 100 years, the device was improved, the materials and dimensions of the device changed, however, the principle of operation remained the same.
The popularity of the technique is due to a number of advantages over traditional surgical interventions on the lungs. Every year the number of endoscopic procedures performed increases.
The main advantages of thoracoscopy over open chest surgery remain:
- Minimally invasive. Traditional interventions require the use of large skin incisions, which causes the formation of scars, difficulties for the patient, and trauma. The endoscopic procedure involves the use of 2-3 small incisions through which special instruments are inserted;
- Speed of the procedure. The use of small incisions (up to 3 cm) saves time on tissue dissection, stopping local bleeding, and suturing the wound;
- Better portability. 50% of patients who cannot undergo traditional surgery due to severe general condition respond well to treatment using minimally invasive technology;
- Fast rehabilitation. The recovery period after thoracoscopy is 2-3 times shorter compared to traditional surgical interventions;
- Low percentage of complications. A short postoperative period during pulmonary thoracoscopy reduces the risk of undesirable consequences;
- Reducing the amount of anesthetics used during treatment and diagnosis using thoracoscopy.
Another feature of the minimally invasive technique is the ability to enlarge the image obtained from the video camera. In traditional operations, the doctor assesses the condition of the pleura and lungs with his own eyes without auxiliary optical instruments.
How is thoracoscopy performed?
Thoracoscopy is a minimally invasive operation, so it is performed only in a hospital and in an operating room or other room that is equipped with the necessary equipment:
- Lighting equipment, monitor;
- Aspirator, trocars, clamps, coagulators and other instruments;
- Endoscope, endovideo camera;
- Sterile dressing material, napkins, gloves.
Sterile conditions are maintained in the room where the thoracoscopy will be performed. Middle and junior medical personnel monitor the cleanliness, timely processing and preparation of instruments, and assist the surgeon during the procedure.
The surgeon performing thoracoscopy requires extreme care, precision of movements and high skill, since when manipulating in a limited space he risks damaging nearby structures.
As a rule, thoracoscopic interventions are performed under general anesthesia due to the need for unilateral pulmonary ventilation and the rather long duration of the operation, during which the patient must remain motionless. In rare cases (pleural biopsy, for example, contraindications to general anesthesia), local anesthesia is possible.
The thoracoscopy operation takes place in several successive stages:
- The patient takes off clothes from the upper half of the body, lies down on his healthy side, under which a cushion is placed, raises his hand to his head, for men the nurse removes the hair in the area of the upcoming punctures;
- Local anesthesia is achieved by tissue infiltration with novocaine, lidocaine, trimecaine; if general anesthesia is necessary, appropriate drugs are administered intravenously, and an endotracheal tube is placed in the trachea to ensure ventilation of the lung on the side opposite the operation;
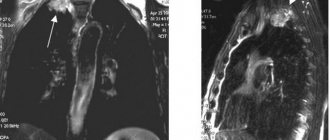
access points for thoracoscopy
Determining the puncture site of the chest wall where the thoracoscope will be inserted - usually at the level of the IV, V or VI intercostal spaces along the posterior axillary line, treating the puncture point with an antiseptic, limiting it with sterile napkins;- Ensuring ventilation of only one lung;
- When the organ has collapsed a little, the surgeon makes an incision in the skin and soft tissue of the intercostal space with a scalpel, and the puncture is made with a trocar;
- After removing the sharp rod from the trocar, a thoracoscope with a video camera is placed in it, which the surgeon will carefully rotate and move in the body cavity, examining those areas that are of most interest;
- If it is necessary to evacuate the contents of the chest cavity or perform some manipulations, the surgeon can make several more punctures through which additional instruments will be inserted (biopsy needles, scissors, forceps, etc.);
- Removing instruments, installing drainage tubes upon completion of thoracoscopy, suturing incisions, treating the skin with antiseptics, covering wounds with sterile napkins or plaster.
Diagnostic thoracoscopy can last up to 2 hours, and thoracoscopic surgery can last up to 2.5 - 3 hours. After the manipulation, the patient is left under observation for some time: for 1 hour - every 15 minutes, then every half hour, and 3 hours after the intervention - hourly. If severe pain occurs, painkillers will be administered. You will have to spend from several days to 2 weeks in the clinic.
Indications and contraindications
Thoracoscopy is a technique that allows, without traumatizing the patient, both diagnosis and treatment of the corresponding disease of the respiratory tract, which causes cough, pain, hemoptysis or other pathological conditions.
Indications for the technique:
- peripheral lung tumors of a benign nature;
- metastasis of the lung parenchyma, but in a single number;
- dissemination in the lungs of unknown origin. A tissue biopsy is performed followed by histological diagnosis;
- peripheral lung cancer;
- diagnostic puncture or resection (removal) of the thoracic lymph nodes;
- spontaneous pneumothorax;
- pleurisy of unknown origin.
Important! Diagnostic thoracoscopy differs from therapeutic thoracoscopy in the volume of intervention. In the first case, the procedure involves a visual assessment of the condition of the internal structures to confirm or refute a specific diagnosis with a possible biopsy.
In the second case, special surgical instruments are additionally used to excise non-viable tissue, remove lymph nodes, and stop bleeding.
Contraindications:
- acute vascular diseases with damage to vital organs - myocardial infarction, stroke;
- coagulation pathology, which may be accompanied by uncontrolled bleeding during manipulation;
- the patient’s inability to tolerate temporary breathing solely with one lung.
The issue of the scope of thoracoscopy and the need for it is decided solely by the doctor, depending on the characteristics of a particular clinical case.
Indications
Thoracoscopy is prescribed if the patient suffers from the following problems:
- Exudative pleurisy with unknown causes of development. Since this disease occurs as a result of metastasis of a cancer tumor, as a complication of tuberculosis or under the influence of malignant mesothelioma, pleuroscopy is used to collect biological material, which is examined histologically to establish an accurate diagnosis.
- Penetrating injury to the chest. In this case, videothoracoscopy reveals or excludes deformations of the pericardium and mediastinal sections.
- Peripheral malignant neoplasm of the lung. If cancer is suspected, then a diagnostic thoracoscopy is performed with a mandatory biopsy of the intrathoracic lymph nodes to establish the stage of the pathology.
- Benign tumors, cysts, lipomas of mediastinal organs.
- Lymphoma, characterized by enlargement of the mediastinal lymph nodes. In this case, pleuroscopy is the only diagnostic method with the ability to perform a biopsy of a morphological sample for subsequent immunohistochemical analysis. Thanks to the results of this examination, the lymphoproliferative process and its type are determined.
- Mediastinal lymphadenopathy with significant inflammation of the lymph nodes in the mediastinum. Here, manipulation determines the cause of the lesion, which can be tuberculosis, sarcoidosis, malignant lymphoma or lymphogranulomatosis. Only the study of the obtained tissue structures of the lymph nodes allows us to determine a preliminary diagnosis.
In addition to diagnosing pathologies of the pleura, which protects the lungs, diaphragm and mediastinum, biopsy of biological material for further histological examination, manipulation is used to eliminate cysts with liquid contents and air bubbles from the lung, remove exudate from the cavity of the serous membrane and perform marginal resection of the organ.
Patient preparation
Proper preparation of the patient for any instrumental examination or treatment procedure ensures an improvement in the achieved result and a reduction in the risk of complications in the postoperative period. Thoracoscopy is no exception.
Before conducting the appropriate examination, the doctor explains to the patient the features of the manipulation, possible risks and complications. Preparation includes the additional use of the following diagnostic measures:
- X-ray of the lungs;
- Ultrasound of the pleural cavity (according to indications);
- general and biochemical blood test;
- coagulogram;
- ECG.
If there are no contraindications to thoracoscopy, the patient is prohibited from eating food 12 hours before the examination to minimize the risk of aspiration (entry into the respiratory tract) of food. Additionally, a hygienic shower is recommended.
Immediately before the examination, the patient is prescribed premedication, which includes the injection of sedatives and, if necessary, muscle relaxants. The surgical site is treated, which may include shaving off chest hair if necessary.
Contraindications
Pleuroscopy is prohibited in the presence of a severe bleeding disorder, acute pulmonary failure with bilateral pneumonia, hemorrhagic diathesis, hemopericardium, characterized by hemorrhage due to rupture of the heart vessels, mechanical damage, or exposure to a neoplasm. Having only one lung in a healthy state also makes single-lung ventilation impossible.
The procedure cannot be performed if the patient suffers from arrhythmia or acute coronary insufficiency, since these pathologies cause disturbances in the functioning of the heart and blood vessels.
Diseases such as peritonitis and intra-abdominal bleeding with associated damage to the cavities, pustular lesions of the epithelium of the thoracic region, adhesions within the pleura, due to which artificial pneumothorax is not used, and acute deterioration of cerebral blood circulation are also considered contraindications to thoracoscopy.
This operation should not be used in severely ill patients with pathologies of internal organs.
Technique
The technique used depends on the volume of the procedure. The primary stages and insertion points of thoracoports (metal “tunnels” for instruments) are the same. The thoracoscopy scheme involves the use of incisions in the projection area of the pathological focus. Most often, tissue dissection is carried out at the level of the 5th and 6th intercostal space.
Algorithm for performing thoracoscopy:
- Premedication;
- Introducing the patient into anesthesia with “switching off” the lung ventilation on the affected side. The patient is transferred to artificial respiration using a specialized apparatus;
- Skin incision. The doctor mainly needs 2-3 holes for high-quality diagnostics using auxiliary instruments. The size of the incision does not exceed 2-3 cm;
- Insertion of a thoracoport into the pleural cavity. If there are adhesions inside the corresponding space, the path for instruments is cleared bluntly - using the surgeon’s finger or a non-sharp jaw of scissors;
- Insertion of a thoracoscope into the pleural cavity. The doctor assesses the condition of the space and the organs inside using an image broadcast on the screen in real time;
- Introduction (if necessary) of additional instruments for the purpose of collecting material for histological examination (biopsy), suturing a vessel, removing pathological tissue, etc.;
- Removing instruments and thoracoscope;
- Installation of drainages;
- Stitching wounds.
The described scheme remains universal. Depending on the current situation, the stages of the procedure may vary. In some cases, conversion from thoracoscopy to open lung surgery is permitted due to the severity and severity of the situation.
Benefits of Thoracoscopy
Among all the positive aspects of thoracoscopy, it is worth noting that after the procedure there are practically no scars left (only a small one from a puncture), the duration of rehabilitation is minimal, and there is no need to transfer the patient to the intensive care unit. In addition, the patient's hospitalization period is reduced, as the likelihood of postoperative complications is reduced.
The procedure does not take much time and requires a minimal amount of anesthesia. And thanks to modern methods and technologies, it is performed as accurately as possible.
The procedure is intended for:
- performing atypical pulmonary marginal resection;
- pumping out fluid from the pleural cavity;
- removal of subpleural cysts from the lungs;
- performing a biopsy;
- diagnosing pleural diseases.
How long does a thoracoscopy take?
Thoracoscopy is a method for diagnosing and treating diseases of the respiratory tract, requiring a doctor to penetrate the pleural cavity using special equipment.
The duration of the corresponding procedure directly depends on:
- severity of the pathological process;
- doctor's skill;
- individual characteristics of each clinical case;
- volume of thoracoscopy.
If the doctor’s goal remains purely diagnostic without additional surgical intervention, then the procedure takes an average of 30-40 minutes. If it is necessary to carry out certain surgical procedures, thoracoscopy can last 90-100 minutes.
What it is
Thoracoscopy is an endoscopic method for examining the patient’s pleural cavity. The manipulation method involves inserting a special instrument through a puncture in the chest wall.
Clear color visualization on the screen allows the doctor to assess the condition of the lungs, mediastinal organs and pericardium located in the cavity of the serous membrane. The procedure, performed only in a hospital setting, is used both to establish an accurate diagnosis and for therapeutic purposes.
Advantages
Often, surgeons use pleuroscopy instead of standard thoracotomy to avoid opening the chest. This is explained by the fact that thoracoscopy has a number of significant advantages. The manipulation allows for multiple magnification of the image of specific structures on the monitor using optical instruments.
In addition, unlike thoracotomy, pleuroscopy is considered a less traumatic and painful operation, with a lower risk of developing negative consequences. During the rehabilitation period, sometimes narcotic painkillers may not even be used.
Thoracoscopy also takes much less time than opening the chest, has a shorter hospitalization time for the patient, is characterized by the absence of large scars and accelerated recovery.
Is thoracoscopy possible during pregnancy?
Thoracoscopy is a minimally invasive intervention that carries a certain threat to the patient. The risk of complications is lower compared to traditional operations, but the danger remains.
During pregnancy, the advisability of carrying out an appropriate procedure depends on the gestation period of the child. In the third trimester, thoracoscopy is prohibited. At earlier stages, the question of the need for a specific examination is decided only by a council of doctors after carefully weighing all the risks and potential benefits of the event for a particular woman. In 75% of cases, doctors try to avoid this diagnostic method.
Causes:
- negative impact of anesthesia on the fetus;
- temporary “switching off” of one lung, which can lead to a decrease in the child’s oxygenation;
- risk of complications.
Important! However, if thoracoscopy remains the only justified method of diagnosis or treatment, then an appropriate examination of the pleural cavity is carried out, but only after obtaining written consent from the woman.
Concept of diagnostics
Thoracoscopy (synonymous names - pleuroscopy or videothoracoscopy) is an endoscopic examination technique designed to examine the pleural cavity of a sick person by introducing a special device - a thoracoscope - through a puncture made in the chest wall.
Thanks to a clear color image displayed on the screen, the specialist performing the procedure has the opportunity to assess the condition of the organs located in the pleural cavity: the lungs, the mediastinum and the outer connective tissue membrane of the heart - the pericardium.
Performed only in medical institutions - clinics and hospitals - the thoracoscopy procedure can have both therapeutic and diagnostic significance: with its help, the doctor can establish an accurate diagnosis.
Modern surgeons often use it instead of traditional thoracotomy, a surgical operation that involves opening the chest.
This is due to a number of advantages characteristic of thoracoscopy, since it:
- makes it possible to repeatedly enlarge the image of individual structures on the monitor screen thanks to the use of modern optical technology;
- is less traumatic;
- not so painful;
- requires less narcotic analgesic drugs during the postoperative period (sometimes there may be no need to prescribe them at all);
- completed in a shorter period of time;
- gives fewer postoperative complications (usually pneumonia and heart rhythm disturbances);
- significantly reduces the length of hospitalization of the patient;
- eliminates the need to place the patient in the intensive care unit;
- does not require a long period of rehabilitation: after it, patients recover faster;
- does not leave large scars on the patient’s body.
The thoracoscopy procedure is intended for:
- Accurate diagnosis of diseases of the pleura - the serous membrane that lines the chest from the inside and protects the surface of the lungs, diaphragm, and mediastinum.
- Obtaining samples of tissue under study (biopsies) for the purpose of their further laboratory study.
- Removing subpleural cysts (fluid-filled cavities) and bullae (air bubbles) from the lungs.
- Evacuation of excess fluid from the pleural cavity.
- Performing atypical marginal lung resection.
Results of diagnostic thoracoscopy
Thoracoscopy is a procedure that allows the doctor to visually determine the localization of the pathological process in the pleural cavity. Using a video camera, the doctor examines all areas of the relevant space step by step and records any changes.
Depending on the picture he sees, the doctor forms a conclusion in which he describes all the deviations and sums up the results of the examination. It is worth considering that the final results of the procedure sometimes differ from the expected diagnosis.
General information
Today, thoracoscopy (TS) or videothoracoscopy (VTS) can be considered one of the common methods of endoscopic examination used to study and treat the organs of the thoracic cavity. The thoracoscope used for research has undergone many evolutionary changes.
If at the beginning of the 20th century it was a device equipped with a system of mirrors, allowing for examination of the pleural cavity and minimal surgical interventions (cauterization, biopsy, cutting of adhesions), then the design of the thoracoscope of the 21st century includes all modern technical achievements (fiber optic technologies, video equipment with high resolution).
Such changes made it possible to use the technique not only for diagnostics, but also for full-fledged surgical procedures. Since thoracoscopic intervention is carried out by introducing a thoracoscope and other necessary equipment through a puncture in the chest, it is possible to avoid large blood losses that usually accompany open operations, as well as cosmetic defects caused by postoperative scars.
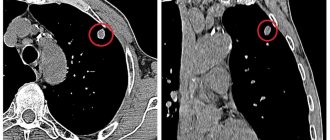
High quality visualization using video monitors and the possibility of multiple magnification successfully compensated for the lack of tactile sensations of the surgeon, and made it possible to accurately determine the localization of pathological foci (for example, bronchopleural fistulas or metastases), which is especially important when taking material for histological analysis.
Important! Often, to perform a biopsy, instead of a thoracoscope, a fibrobronchoscope is used, equipped with an intense lighting source and a convenient control system; it has a built-in device for taking a histological sample.
Rigid operating thoracoscope with a channel for inserting biopsy forceps
Complications
The described examination is minimally invasive. The low invasiveness of the event ensures rapid recovery of the patient without the risk of complications. According to reviews of pulmonary thoracoscopy from patients and doctors, the incidence of undesirable consequences is 50-60% lower compared to traditional open operations.
Possible complications:
- pain at the incision sites;
- wound infection with increased body temperature and general deterioration of the patient’s condition;
- bleeding.
The chance of developing relevant undesirable consequences depends on the specific situation and the skill of the doctor.
Indications for thoracoscopy
The basis for prescribing pulmonary thoracoscopy is the presence of:
- Exudative pleurisy of unknown etiology. Since pleurisy can develop due to various reasons (for example, under the influence of malignant mesothelioma, tuberculosis or the spread of a cancerous tumor in the pleura), a thoracoscopy procedure is necessary to obtain informative biopsy material, the study of which will make it possible to establish an accurate diagnosis.
- Penetrating chest wounds. Thoracoscopy will reveal or exclude damage to the pericardium or mediastinal organs.
- Peripheral lung cancer. If cancer is suspected, conducting a diagnostic study (with the obligatory taking of a biopsy of the intrathoracic lymph nodes) will give an idea of the extent of the oncological process and will allow us to determine its stage.
- Benign neoplasms of the mediastinum.
- Mediastinal lymphadenopathy is a condition accompanied by a significant increase in lymph nodes localized in the mediastinum. Thoracoscopy will determine the type of lesion (it may be a consequence of tuberculosis, lymphogranulomatosis, sarcoidosis or malignant lymphoma). Only analysis (immunohistochemical or histological) of the tissues of the affected lymph nodes can clarify the preliminary diagnosis.
- Lymphoma accompanied by damage to the mediastinal lymph nodes. Thoracoscopy is the only diagnostic method that makes it possible to take morphological samples to perform an immunohistochemical study, the results of which will allow us to establish the type of lymphoproliferative process occurring in each specific case.
Features of preparation
The patient is allowed to undergo surgery only after passing all the necessary tests. Based on these tests, the doctor determines the possibility of performing thoracoscopy. The patient should undergo the following tests:
- electrocardiogram;
- chest x-ray;
- spirometry;
- coagulogram;
- blood tests: general, coagulability and group.
Based on these tests, the doctor is convinced that the patient has no contraindications and can therefore be allowed to undergo surgery.
It is important to know! At the preparation stage, it is necessary to determine the presence of allergies in the patient. If the patient knows what he is allergic to, then he must immediately inform the doctor about it.
Before the patient lies on the operating table, he will be required to sign a document outlining the risks and confirming consent to undergo the operation.
The preparation stage includes the following actions:
- 8-10 hours before surgery it is forbidden to eat;
- you should not drink alcohol 2-3 days before thoracoscopy;
- inform the doctor about taking medications (if the patient is taking medications);
- take your relatives and necessary things and items with you on the day of the operation.
Carrying out thoracoscopy
Videothoracoscopy and conventional thoracoscopy are carried out using special instruments - thoracoscopes, which include a light source and a video camera. There are a large number of their varieties, allowing you to adapt the procedure to each specific patient.
After administering general anesthesia and tracheal intubation, one lung collapses (from the examination side). A trocar is carefully inserted through a small incision in the intercostal space to prepare an opening for the thoracoscope. After this, a trocar is inserted directly, allowing a visual assessment of the condition of the pleural cavity. As a rule, several aspirators are additionally introduced, used to suck out excess fluid.
At the end of thoracoscopy, the instruments are removed from the pleural cavity, and the incisions are sutured and covered with aseptic dressings. During the day after the procedure, it is necessary to carefully monitor the patient's vital signs.
In addition to diagnostic purposes, thoracoscopy can also be therapeutic. In this case, accumulated pathological fluid can be removed from the pleural cavity, obscure neoplasms can be removed, or pieces of them can be taken for subsequent morphological diagnosis.
The technique is performed in a medical facility, due to the risk of severe complications.
The average duration of thoracoscopy is 1-2 hours, depending on its purpose. As a rule, no serious complications are observed if the procedure technique is followed.
Preparation for thoracoscopy
Before the procedure, the patient signs a voluntary informed consent for the study.
The most important stage in preparing the patient is a thorough explanation of the procedure, the purpose of its implementation, as well as informing the patient about possible complications. As a rule, for adequate pain relief, general anesthesia is used to minimize the risk of developing pain.
10-12 hours before the procedure, the patient should refuse to eat to empty the upper gastrointestinal tract. This allows you to avoid the development of a number of complications associated with aspiration of food.
It is necessary to consult with your doctor before the procedure to find out the specifics of preparation, the progress of thoracoscopy and obtain information about the recovery period.
Before the examination, all patients are required to undergo an electrocardiogram, assessment of respiratory functions, determination of blood coagulation status, and chest x-rays. Such a preliminary study is aimed at identifying risk factors that can lead to complications of the main procedure. For example, poor blood clotting can cause prolonged bleeding during thoracoscopy.